- radial
- femoral
- complications
- bleeding
- outcomes
Abstract
Aims: The aim of the present study was to examine the impact of the transradial approach (TRA), in comparison to the transfemoral approach (TFA), on PCI-related bleeding and patient outcomes in acute coronary syndrome patients who underwent PCI in the OASIS-5 trial.
Methods and results: The primary outcome (death, myocardial infarction, refractory ischaemia) at nine days was similar in both groups (7.1% in 872 TRA and 7.7% in 7,013 TFA). Major bleeding was significantly lower in patients who underwent PCI with TRA by comparison to TFA (1.6% vs 3.5%, p<0.003, respectively). No difference between patients treated by fondaparinux or enoxaparin was noted for ischaemic events at nine days according to the access site. The rate of major bleeding at nine days was markedly reduced with fondaparinux when compared to enoxaparin for both access sites (from 4.8% to 2.3%, HR 0.48 [0.37-0.62], p< 0.0001 for TFA and from 2.4 to 0.9%, HR 0.36 [0.11- 1.16], p<0.08 for TRA).
Conclusions: TRA is associated with substantial decrease of PCI-related bleeding in current contemporary pharmacological environment in comparison to TFA. Even in the context of low access site complication rate provided by TRA, fondaparinux was effective in reducing major bleeding.
Introduction
The use of combined antithrombotic therapies over the last two decades has substantially decreased the risk of ischaemic complications after percutaneous coronary intervention (PCI), but it has also been associated with a substantial bleeding risk1. Therefore, strategies that maintain the benefits seen with currently available antithrombotic therapies but with lower bleeding risk are attractive. Indeed, major bleeding is currently the most common non cardiac complication for ACS patients who have undergone an invasive strategy and PCI1,2.
PCI-related bleeding in the setting of acute coronary syndromes occurs frequently at the arterial puncture site and is consistently associated with subsequent poor patient outcomes, as reported in many contemporary pharmaco-invasive trials and registries3-8. In the OASIS-5 trial, fondaparinux was shown to be non-inferior to enoxaparin for the primary ischaemic composite endpoint. Furthermore, by reducing major bleeding, fondaparinux was associated with better net adverse clinical events and a mortality reduction at one month, sustained significantly at six months9. The OASIS 5 trial provides an opportunity to evaluate the impact of a radial approach compared to the more conventional femoral approach in a large cohort of ACS patients treated with a contemporary pharmacological regimen and an early invasive strategy. To minimise access-site bleeding and other vascular complications, the radial approach is increasingly recognised as an alternative to the routine use of the femoral approach10-13. Therefore, to determine the impact of the access site on efficacy and safety endpoints in ACS patients, we performed a post hoc analysis of patients who were enrolled in the OASIS 5 trial, and underwent an early invasive strategy with systematic coronary angiography.
Materials and methods
Study population
The design of the OASIS 5 trial has been previously published in detail9. Briefly, 20,078 patients with ACS (high-risk patients with unstable angina or myocardial infarction without ST-segment elevation) were enrolled from 576 centres in 41 countries and were randomly and blindly assigned to enoxaparin or fondaparinux (2.5mg once daily plus placebo enoxaparin twice daily by subcutaneous injection or enoxaparin at a dose of 1mg per kilogram of body weight twice daily plus placebo fondaparinux once daily by subcutaneous injection). Angiography was performed at the investigating physician’s discretion, as well as triage to PCI, CABG or medical treatment after angiography.
Interventions
The choice of the arterial access site was left to the discretion of the investigating physician. Patients with a brachial access were excluded from this analysis. A study population of 14,159 catheterised patients was available and 7,885 who underwent PCI either by radial or femoral access at time of initial catheterisation were included in the present analysis.
If PCI was to be considered, use of clopidogrel and aspirin was recommended at least six hours before the procedure.
Endpoints
The composite ischaemia (death from any cause, MI or refractory ischaemia) and major bleeding endpoints were compared between patients treated by radial and femoral approaches at nine days, 30days and six months follow-up. The incidence of stroke was also compared in the two groups. Combining the composite ischaemia (triple efficacy) endpoint and major bleeding (primary safety) endpoint a quadruple endpoint named “net adverse clinical events” was also used to compare the access site strategies. In the OASIS 5 trial, major bleeding was defined as clinically overt bleeding that is either fatal, symptomatic intracranial, retroperitoneal, intraocular, adecrease in haemoglobin of at least 3.0 g/dL (with each blood transfusion unit counting for 1.0 g/dL of haemoglobin), or requiring transfusion of ≥2 U of red blood cells.
Statistical analysis
Comparisons of baseline, angiographic and procedural characteristics were carried out according to access site (femoral or radial). Continuous variables were summarised by means and SD and categorical variables were summarised as percentages. P values were calculated comparing femoral and radial access. Categorical variables were compared by Chi-square and continuous variables were compared by the non-parametric Wilcoxon rank sum test. The hazard ratio (for radial vs. femoral) and two-sided 95% confidence interval were calculated with the use of a Cox proportional-hazards model, with the access site as the only covariate. Time-to-event data are displayed using Kaplan-Meier methodology. A propensity score was developed for the use of the radial approach and included variables that influenced the use of the radial approach such as age, sex, diabetes, ST-segment deviation, prior MI, GPI use and elevated cardiac enzymes and other baseline variables listed in Table 1. The propensity score was used to adjust the Cox proportional hazards model to compare outcomes in the radial versus the femoral groups.
Results
Baseline characteristics of THE study population
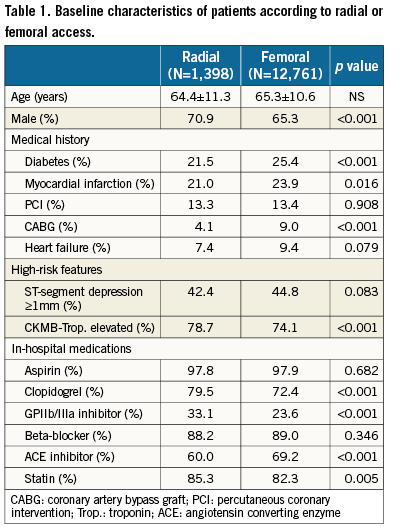
The femoral approach was used in 90% (n=12,761) of cases while the radial approach was used in 10% (n=1,398). As described in Table 1 –and related to the huge difference between the sample size between the two groups and the post hoc analysis design– significant differences were found in baseline characteristics between patients treated by the radial approach and those treated by the femoral approach. While most of the cardiovascular risk factors were more frequent in the femoral group, patients treated by the radial approach more frequently had positive biomarkers. No significant difference for the presence of ST depression was observed between the two groups. Subtle differences were also observed in medical treatment between the two groups of patients with GPIIb/IIIa inhibitors more frequently administered in patients catheterised by radial approach. The procedural details (such as frequency of thrombus-containing lesions) and procedure success rates were similar in both groups.
Clinical outcomes and bleeding complications by access site in PCI patients
Major bleeding and bleeding complications by access site are shown in Table 2 at day nine.
Net adverse clinical events at day nine were lower with the radial approach, with 10.5% versus 11.1% for radial and femoral approach, respectively (adjusted OR = 0.83 95% CI [0.62-0.99], p=0.03). The composite ischaemic endpoint at day nine –including death, MI and refractory ischaemia– was identical between the two strategies, and significant reduction of major bleeding at day nine was observed with the radial approach cases compared to the femoral approach cases (adjusted OR=0.45 95% CI [0.26-0.77], p=0.003).
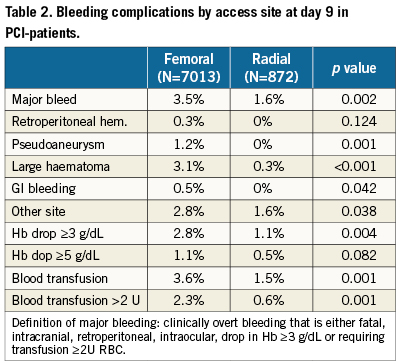
At one month, net adverse clinical events was still in favour of the radial approach with no significant difference for composite ischaemia and a 50% lower major bleeding with the radial approach (Figure 1).
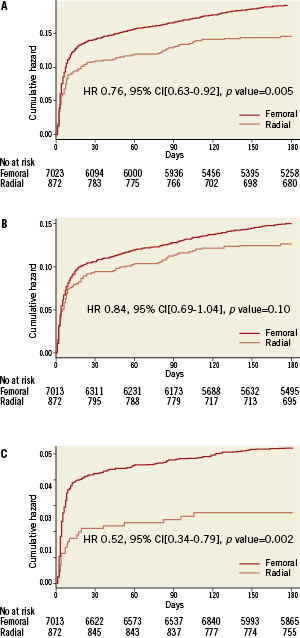
Figure 1. Kaplan-Meier curves for 180 days net adverse clinical events (Panel A), composite ischaemia (Panel B) and major bleeding (Panel C).
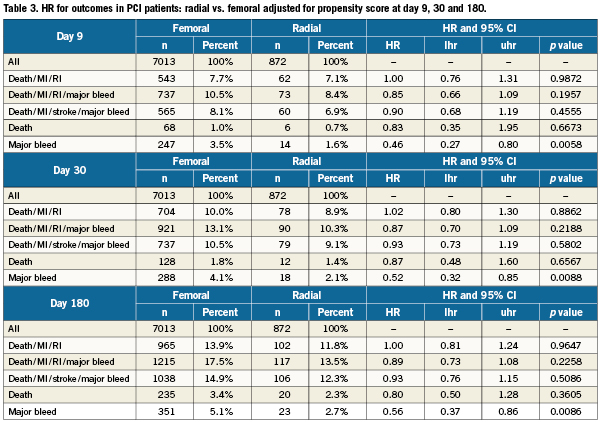
At six months follow-up, net adverse clinical events were now highly significantly in favour of the radial approach strategy, with a similar trend for composite ischaemia and still with a 50% reduction for major bleeding in favour of the radial access. As shown in the Kaplan-Meier curves, the trend of composite ischaemia reduction was driven by a similar trend to mortality reduction at six months in patients treated by the radial approach (Figure 2). All Hazard ratios and 95% CI are given after propensity adjustment for outcomes in PCI patients in Table 3 at day nine, 30 and 180.
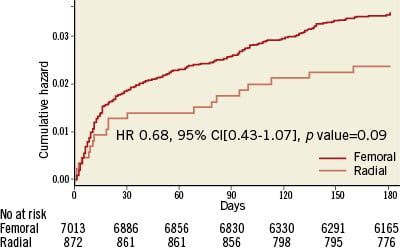
Figure 2. Mortality at six months comparing Kaplan-Meier curves of patients initially treated by radial or femoral access.
Bleeding and transfusions by access site and treatment group
Major bleeding at day nine as well as subsequent haemoglobin drop or blood transfusions were likely to be driven by access site complications more frequently encountered when the femoral approach was used. In Figure 3, the impact of the radial approach on major bleeding overall and during blind study drug administration is shown in the two arms of the trial. Significant reduction of major bleeding is observed in the same range when patients are treated either by enoxaparin or by fondaparinux. In Figure 4 major bleeding by access-site according to the anticoagulation regimen received indicates a homogeneous bleeding reduction in favour of fondaparinux, even in patients catheterised by the radial approach (P for interaction NS).
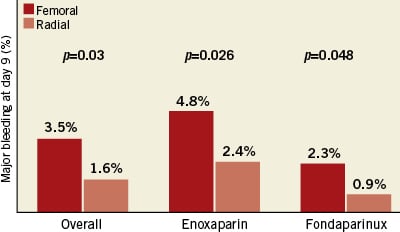
Figure 3. Major bleeding in PCI patients at day nine during blinded study drug administration.
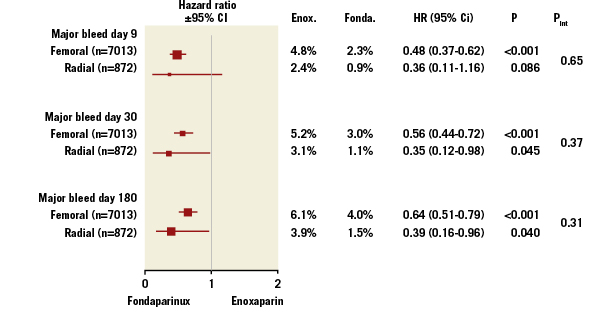
Figure 4. Major bleeding according to anticoagulation regimen in access site subgroups.
Discussion
In ACS patients undergoing an early invasive strategy, the radial access was associated with similar rates of composite ischaemic outcome and significantly reduced major bleeding when compared with the femoral access using a contemporary pharmacological regimen. This reduction of major bleeding was translated in better net adverse clinical events when patients were explored by a radial approach. A fondaparinux based-strategy was also associated, even in the context of transradial access, with a reduction of major bleeding. However, as recently outlined, an additional bolus of unfractionated heparin is needed in case of PCI to avoid catheter thrombosis in patients who received fondaparinux pretreatment14.
The combination of antithrombotic therapies used in the last two decades has decreased the risk of heart attacks after PCI procedures substantially, but has also been associated with a significant increase in bleeding risk1-8. Bleeding in patients with acute coronary syndromes (ACS) is associated with an increased risk of long-term mortality and morbidity, and this relationship may be causal. Clearly then, it would be important that future therapies or strategies are able to maintain the benefits of currently available antithrombotic therapies and also lower the bleeding risk. Bleeding complications in the setting of ACS management are partly in relation to femoral access-site complications and are responsible for a non-negligible rate of patient complaints11-13. Routinely, percutaneous arterial access is achieved by means of fluoroscopic visualisation of bony landmarks or guided by palpation of the femoral pulse. Thus, femoral arterial access is largely a blind procedure with a success rate influenced by anatomical variation, obesity, and incorrect needle puncture, all of which can lead to local complications such as groin haematoma, arteriovenous fistula, arterial pseudoaneurysm and retroperitoneal haemorrhage. In addition, systemic aggressive antithrombotic regimens used in the past few years further increase the risks of perivascular and systemic bleeding.
These bleeding complications and the transfusions that they make necessary are identified as independent predictors of poor outcome and may be primary influences on the quadruple endpoint, including both efficacy and safety endpoints, as was recently pointed out in the OASIS 5 trial9.
The available evidence, supported by several randomised studies, suggests that radial access is associated with fewer bleeding events and transfusions, as compared to the femoral approach11-13. With radial access, bleeding and vascular access site complications are virtually eliminated, essentially because radial artery is superficial and easily compressible. This is a major advantage in the current era of intensive anticoagulant and antiplatelet therapy. Patient comfort is increased, nursing staff workload is reduced, and outpatient treatment has already been set up by some pioneers15. This drastic reduction of the complication rate from the vascular access site is immediately associated with a significantly shorter hospital stay and financial savings. It remains to be seen whether the reduction in access-site complications observed with radial access and confirmed in the present analysis can be translated into a long-term mortality reduction as suggested by 6-months follow-up. In fact, because the radial approach can reduce major bleeding by ~50%, it would be not surprising that mortality might be reduced, if the association observed between bleeding and death is causal16. In keeping with this hypothesis, we can mention the reductions in all cause mortality and cardiovascular mortality observed in Horizons-AMI trial when patients are treated with bivalirudin associated with lower rates of major bleeding compared to the conventional use of unfractionated heparin and a glycoprotein IIb-IIIa inhibitor17. However, after adjustment for the propensity to use radial access, a significant reduction in mortality was not observed with radial compared to femoral access in the present study, despite a clear reduction in access-site bleeding. Large randomised trials are thus required to address this question definitively, such as the recently completed RIVAL trial18.
The relative disadvantage of radial access relates to the operator’s learning curve, and therefore only experienced operators should attempt it. Clearly, materials and procedures were not well standardised in the beginning, and the rate of failure related to radial spasm, arterial puncture failure or failure to reach the ascending aorta were obstacles that made operators reluctant to use this approach. However, dedicated materials and diffusion of the technique reduced these limitations, and success rates are now equivalent in both access sites11. Still, as shown in the present analysis, less than 10% of radial access is currently reported in contemporary trials indicating that some dedicated and sustained educational actions must be pursued to teach this safer access route for performing PCI.
Limitations
This is a post hoc analysis without randomisation between the femoral and the radial approach. Although procedural antithrombotic treatment of the patients was similar in both radial and femoral groups, the patients in the radial group were more likely to present with different baseline characteristics. However, some high risk features as indicated by elevation of biological markers were more frequent in patients undergoing the radial approach. Another limitation of this analysis is the lack of post-procedural radial patency assessment. Indeed, radial occlusion of 1-6%, even when asymptomatic, can be considered by some physicians as a significant complication19. In addition, several important variables that may affect PCI outcomes and bleeding were not collected in this study, and thus were not available when adjusting for the hazard in clinical outcomes, including hypertension, hyperlipidaemia, body mass index, renal function, haematocrit and white blood cell count, left ventricular ejection fraction, the number of diseased vessels, and the number of lesions and vessels undergoing PCI. Furthermore, the present analysis was not by intention to treat; i.e., patients in whom radial or femoral access was unsuccessful who then “crossed-over” were analysed according to the access site actually used, which may have introduced a bias. The frequency of this occurrence was not collected.
Conclusions
In ACS patients undergoing an early invasive strategy, radial access is associated with similar rates of composite ischaemic outcome and is associated with a substantial decrease of major bleeding in comparison to conventional femoral access leading to a better clinical outcome. A fondaparinux based-strategy, which provides anti-ischaemic protection not inferior to enoxaparin, can be favourably associated with radial access to optimise patient outcome. Whether radial access, which is able to reduce bleeding complications, is also able to impact on long-term patient mortality remains to be proved in an adequately powered randomised trial18.
Conflict of interest statement
Martial Hamon has received in the last two years research grants from Glaxo Smith Kline, The Medicines Company and Lilly. OASIS 5 was supported by Sanofi-Aventis, Organon and Glaxo Smith Kline.The other authors have no conflict of interest to declare.