Abstract
This paper describes the opportunities and challenges in building ST-elevation acute myocardial infarction (STEMI) systems of care in Stent for Life affiliated and collaborating so-called emerging countries, namely India, China, South Africa and Mexico, where CAD mortality is increasing and becoming a significant healthcare problem. The Stent for Life model supports the implementation of ESC STEMI Guidelines in Europe and endeavours to impact on morbidity and mortality by improving services and developing regional STEMI systems of care, whereby STEMI patients’ timely access to a primary percutaneous coronary intervention (PPCI) is assured. In India, the STEMI India model incorporates a dual approach of combining PPCI with a pharmacoinvasive strategy of reperfusion. The architecture of the system is based on a hub and spoke model with each unit called a STEMI cluster. The project is driven by a private non-profit organisation. In China, the STEMI PCI programme is led by the Chinese College of Cardiovascular Physicians and supported by the national government. Although primary PCI is performed nationwide, a thrombolytic treatment strategy is still the first option in many rural areas because of logistic considerations. Establishing local STEMI transfer networks and then implementing a pharmacoinvasive strategy of reperfusion are being considered and promoted currently. In South Africa, the pharmacoinvasive approach currently dominates as STEMI treatment option in many areas. A pilot study shows that low symptom awareness leads to long patient delays. The education of all role players, from patients to healthcare professionals and including institutions and governmental structures, is needed to achieve prompt diagnosis and treatment. In Mexico, improving the treatment of STEMI requires considering myocardial infarction to be an emergency that must be treated by an entire system and not just by a particular service. Patients need to receive quick treatment from clinical and interventional cardiologists, and the emergency medical system (EMS) must understand the importance of early reperfusion therapy when appropriate. Mexican health authorities have used registries as their main strategy for improving the use of health resources for ACS patients. In general, building regional STEMI systems of care and an EMS system infrastructure are critical success factors in the stepwise development of STEMI systems of care at a national level in emerging countries as they are in Europe. An in-depth understanding of healthcare system-level barriers to timely and appropriate reperfusion therapy facilitates the development of more effective strategies for improving the quality of STEMI care in each region and country.
Introduction
Stent for Life (SFL), an EAPCI and EuroPCR coalition, was established in 2008 as a non-profit international network of national cardiac societies and partnering organisations to address inequalities in ST-elevation acute myocardial infarction (STEMI) patients’ access to a life-saving revascularisation treatment. SFL supports the implementation of European Clinical Practice Guidelines (Guidelines) at national and regional levels through the formulation of strategies, the creation and implementation of educational programmes, and through advocacy activities and awareness campaigns. Currently 18 national cardiac societies and partnering organisations are actively participating in the SFL Initiative.
The SFL model activates all stakeholders interested in the treatment of STEMI patients, from emergency medical service (EMS) providers to cardiologists, from STEMI-referral hospitals (non-PCI-capable) to STEMI-receiving hospitals (PCI-capable), from payers to policy makers, from patients to public.
The goal is to improve STEMI patients’ timely access to appropriate treatment at a national level by establishing effective regional STEMI systems of care.
SFL countries’ geographic mapping and situational analyses have shown that adherence to the ESC STEMI Guidelines is influenced by many factors and varies from country to country, from region to region, and one model does not fit all. An in-depth understanding of system-level barriers and unique challenges in the regional context facilitates the development of more effective strategies for improving the quality of the STEMI system of care in a particular country.
In this paper we describe the opportunities and challenges in building the STEMI systems of care in SFL affiliated and collaborating countries, namely India, China, South Africa and Mexico, where coronary artery disease (CAD) mortality is increasing and becoming a significant healthcare problem. These four emerging countries represent almost three billion people, e.g., 40% of the world population.
By 2020, 60% of the world’s heart disease is expected to occur in India
CAD is a significant healthcare problem in India. By the year 2015 an estimated 65 million people will be affected by CAD1. Coronary artery disease causes three million deaths/year, accounting for 25% of all mortality in India. By 2020, 60% of the world’s heart disease is expected to occur in India. CAD is affecting Indians 5-10 years earlier than other communities: in some studies from South India, the percentage of patients below 45 years suffering from acute myocardial infarction (AMI) is reported to be as high as 25-40%. Asian Indians have a 40% higher mortality rate from CAD than their white counterparts.
The CREATE registry gives the clearest contemporary statistics regarding ST-elevation myocardial infarction (STEMI) cases in India. This study showed that in India a higher percentage of patients with acute coronary syndromes (ACS) present with STEMI than in North America and Europe. In addition, the patients are younger, belong to a lower socioeconomic group and have limited access to adequate treatment. Patients with STEMI took much longer to reach hospital (median 300 minutes) than did patients in developed countries (range from 140 to 170 minutes). The study suggested that the reasons patients reached hospital late included the lack of ambulance services, traffic congestion, long distances and consultation with family physicians2.
The Kovai Erode Pilot STEMI Study3 was the first attempt to develop a system of care combining primary percutaneous coronary intervention (PCI) with the pharmacoinvasive strategy of reperfusion. This was important since cathlabs are located in urban areas, where primary PCI is feasible, while more than 70% of STEMI cases are in rural and semi-urban areas where only thrombolysis is possible. This study showed that: (1) it is possible to develop a hub and spoke model combining primary PCI with a pharmacoinvasive approach, (2) awareness and reasonably early access to medical care are possible even in rural communities, and (3) a good ambulance system significantly reduces travel times (median time from symptom onset to presentation was 165 minutes compared to 360 minutes in CREATE).
The pilot study indicated multiple issues that needed to be addressed. Guidelines on STEMI management need to be developed, accepted and given wide publicity especially in smaller and rural hospitals. Building partnerships between hospitals is critical in developing the pharmacoinvasive strategy and a mechanism for inter-hospital transfer of patients is required. Financial mechanisms are needed to enable patients from lower socioeconomic levels to access STEMI care. Audit and quality control issues need to be addressed at every level.
The role of STEMI INDIA in STEMI system of care development in the country
Based on the experience from the Kovai Erode Pilot STEMI Study, STEMI INDIA –a non-profit organisation working to develop STEMI systems of care– has proposed a model known as the STEMI INDIA model. STEMI management in India will adopt the dual approach of combining primary PCI with a pharmacoinvasive strategy of reperfusion to produce a coherent framework for developing a system of care (Figure 1)4.
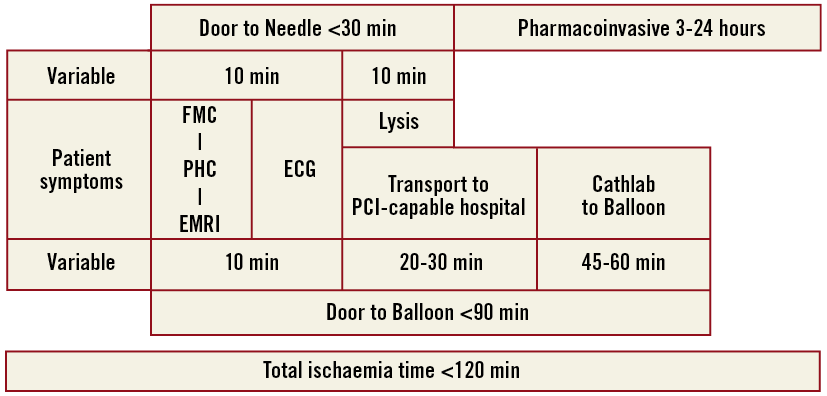
Figure 1. STEMI INDIA reperfusion model.
Primary PCI will be available primarily for patients located close to catheterisation laboratories in urban areas with presumed short transportation time to hospitals equipped with 24/7 primary PCI capabilities. Patients in rural areas, with suspected long transportation time to PCI-capable hospitals, would utilise the pharmacoinvasive strategy with thrombolytic therapy followed by catheterisation and PCI if indicated within 3-24 hours of thrombolysis. The architecture of this system is based on a hub and spoke model with each unit called a STEMI cluster (Figure 2)4.
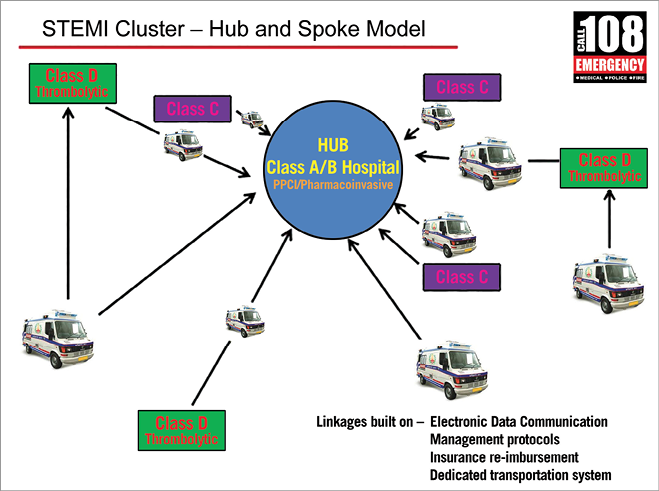
Figure 2. Architecture of ST-elevation myocardial infarction cluster.
Based on this architecture, a four-cluster programme was launched in the south Indian state of Tamil Nadu. Two of the main challenges of the programme have been infrastructure for managing medical emergencies at the population level and manpower constraints. These have been partly overcome with the use of technology. STEMI INDIA has developed a multifunctional device that can be used in the spoke hospitals. These devices have 3G transmission capabilities and can function as an ECG device, monitoring device and a data entry device. ECGs can be transmitted to an “on call” cardiologist in the hub hospital for appropriate action.
Despite the fact that overall healthcare spending in India is significantly lower than in developed countries, and that public and private health insurance programmes are inadequate and disparities in access to healthcare persist between urban and rural India, the STEMI system of care infrastructure is developing rapidly. One of the key partners in this programme has been the GVK EMRI ambulance system, a free service that operates as a public-private partnership. The government pays for services while the overall operation is carried out by a private organisation. The organisation has pioneered the development of emergency medical services (EMS) in India, including training paramedics, technicians, nurses and physicians in emergency care. It is now available in 15 states and union territories of the country.
STEMI INDIA serves as a best practice example to other country states, where situational (facility and manpower) mapping and geographic planning will be performed to outline the STEMI systems of care development at a national level in the near future.
National PCI registry led by the Chinese Government shows a rapid increase in PPCI in China
The disease spectrum in China is changing. The rapid rise of non-communicable diseases driven by urbanisation, rising incomes, and ageing poses major challenges for China’s health system. The leading causes of death were stroke and ischaemic heart disease in China in 20105. It is estimated that the number of myocardial infarction (MI) patients will increase to 23 million in China by 20306. This is partly because of a worsening profile of risk factors, such as an increased prevalence of hypertension, hyperlipidaemia, overweight and obesity, diabetes, and partly because of an increase in the aged population.
PCI started in 1984 in China and uptake has increased rapidly, especially in the last decade. The national online PCI registry was set up by the Ministry of Health of China in 2009 for the purposes of PCI quality improvement, including certification of institutions and individuals as well as quality control of diagnostic and therapeutic interventions. China’s 2010 ST-segment elevation myocardial infarction (STEMI) guidelines recommend (Class I, Level of Evidence A) that primary PCI should be conducted by experienced operators who independently perform at least 50 elective PCI procedures per year. In addition, primary PCI should be performed in qualified catheter labs conducting at least 100 procedures per year.
The overall reperfusion ratio is about 55% and did not change significantly from 2001 to 2011. However, the ratio of primary PCI increased from 10.2% to 27.6%, while the ratio of thrombolysis concurrently decreased from 45.0% to 27.4%7. Published data show that a total of 175,591 cases were performed by 4,389 physicians in 1,015 online registered hospitals from July 2009 to February 20108. Primary PCI only accounted for about 30% of STEMI patients undergoing PCI in 2009 and 20108,9. The median time between MI symptom onset and hospital admission was 14, 15 and 13 hours in China in 2001, 2006 and 2011, respectively7. Treatment delays result both from the healthcare system and from patients. Several system-level barriers affect the efficacy of STEMI care in China including: (1) leadership, capacity, ability, and collaboration of emergency medical services (EMS) and hospitals, and (2) healthcare funding constraints and high out-of-pocket expenses10. Delays attributed to patients are mainly due to poor knowledge and an inharmonious relationship between doctors and patients. An inability to recognise ischaemia symptoms, failure to call an ambulance when symptoms occur, and prolonged discussions for obtaining consent lead to delays in medical assistance for suspected MI.
To improve upon the gaps between practice and evidence, such as low reperfusion ratio, non-standardised treatment, as well as economic burden, the prospective observational China STEMI PCI programme was initiated in 2011. A pilot study focused on improving the in-hospital green channel was performed in 53 tertiary hospitals qualified for primary PCI and data analysis has just been completed. The data are not yet available for publishing. The study will be expanded to around 200 primary PCI-capable hospitals together with hundreds of adjacent non-primary PCI-capable hospitals in 2014.
Several key issues will be addressed at this stage, including: (1) conducting public education and physician training continuously, (2) setting up a local STEMI network focusing on pre-hospital alert by EMS, inter-hospital transfer, and/or bypassing the emergency department in hospital, (3) promoting chest pain centre (CPC) construction as well as improving standards of independent CPC accreditation in China, and (4) increasing the overall reperfusion ratio of STEMI.
Of note, a thrombolytic treatment strategy is still useful in China especially in many rural areas because of logistic issues. Since EMS and hospitals are relatively independent in China, the government plays a very important role in enhancing collaborations between EMS and PCI-capable hospitals, and non-PCI-capable hospitals and PCI-capable hospitals. A pharmacoinvasive reperfusion strategy is being considered and will be promoted with the local STEMI transfer network support.
Barriers and opportunities for early reperfusion in South Africa: a pilot study in a metropolitan area in the City of Tshwane
Results from the ACCESS survey (Acute Coronary Events – a Multinational Survey of Current Management Strategies), with specific reference to South Africa11, show that thrombolytic therapy was used in only 36% of STEMI patients and primary PCI in 59.7%, with a delay from onset of symptoms to arrival in hospital of a median (Q1; Q3) of 3.6 (1.6; 9.5) hours, which is well beyond the 120-minute cut-off for primary PCI. This study was conducted during 2007-2008. Currently, the pharmacoinvasive strategy appears to be fundamental to patient management in South Africa although in many areas pharmacotherapy is the only treatment option (and probably will be for years to come - personal observation).
Pre-hospital early diagnosis and immediate transport are of vital importance12,13, and barriers to timely and appropriate intervention need to be identified and specifically targeted in order to impact on change. A prerequisite for effective STEMI management is education. The South African Heart Association has embarked on an educational project which aims to improve the quality of acute myocardial infarction (AMI) care, to improve the network of care to give more patients access to reperfusion therapy, and to decrease AMI mortality. The Tshwane metropolitan area was deemed suitable for the pilot study for reasons of convenience and representation of near optimal conditions. The South African Heart Association performed a pilot study in the Tshwane metropolitan area which has a total population of approximately 2.9 million14 within an area of 6,368 square km15. There are seven PCI-capable hospitals in this region –not all of which deliver a 24/7 service– and one public and 14 private emergency medical service (EMS) providers.
The aim of the study was to investigate whether primary PCI is performed in a timely way in this region, and to identify barriers to effective STEMI management with the purpose of forming training programmes and South African STEMI treatment guidelines. A cross-sectional observational study was performed in a convenience sample of 21 “inter-facility- transfer” (IFT) and 21 “direct access to cathlab” (DA) consecutive cases in the City of Tshwane. EMS were poorly solicited and time lapses along the referral pathway and arrival-in-cathlab intervals (ACI) were considerably shorter in the DA patients compared with the IFT patients, with mean cathlab activation times of 9 hrs 20 min vs. 20 hrs 11 min.
EMS development is vital in South Africa
In terms of the Constitution of South Africa, access to emergency medical services (EMS) is a right. When a call for EMS is registered with the communication centre, the appropriate service must be dispatched. The evolution of EMS is a national priority, and the government has created a National Emergency Medical Service Strategic Framework, complete with goals and timelines. A national emergency telephone number for EMS has been established. The communication centres in EMS have been modernised, a significant number of the ambulance fleet has been replaced, and the staff complement has been expanded and strengthened.
The key findings of the interviews with the EMS providers were inadequate facilities to record and transmit ECGs, and problems with admitting patients to hospitals due to a shortage of beds or medical aid issues, e.g., the PCI-capable hospital is not the preferential provider of the medical aid. Although the EMS appear quite capable and are relatively well equipped to transfer patients, their services were poorly solicited in this pilot study. There is an obvious need to ensure that paramedics are adequately trained to diagnose and triage STEMI patients successfully as this will impact positively on patient outcome.
Healthcare professional education supports early diagnosis of STEMI
The first educational initiative, as implemented in the pilot, was to educate healthcare professionals at cathlab hospitals to ensure that an ECG is done on all patients with chest pain within 10 minutes of arrival and that they are then transferred to the cathlab with minimal delay. This educational programme was then extended to healthcare professionals working in hospitals without cathlabs. As the network of referring healthcare professionals is large and facilities are based in outlying areas, the education of these individuals continues to pose a challenge.
The project requires involvement of all key system stakeholders
Apart from the need for education, fragmentation of the healthcare sector is a major obstacle as there is no effectively functioning central hub. Communication among the different groups of stakeholders (private hospital groups, public hospitals, ambulance services and cardiologists) to work together to improve STEMI care has been challenging. This obstacle is, however, not insurmountable. Furthermore, it is noteworthy that in the South Africa setting 75% of cathlabs are found in the private healthcare system and these cathlabs only service 25% of the population, whereas in the public sector five of the eleven provinces have no specialist cardiac care available, leaving the public patient severely disadvantaged.
In South Africa the education of all role players, from patients to healthcare workers and including institutions and governmental structures, is still a burning issue. Patient awareness programmes will be developed with the assistance of the SA Heart and Stroke Foundation. In conclusion, the experience gained through the pilot project in the City of Tshwane may pave the way for national rollout of the STEMI Early Reperfusion Project with the ultimate aim of improving outcomes for all patients.
Access to reperfusion therapy in Latin America is improving
Community incidence rates for STEMI have declined over the past decade, whereas those for non-ST-elevation ACS have increased. At present, STEMI comprises approximately 25-40% of MI presentations16. Cardiovascular mortality and MI have declined in some Latin American countries in recent years. Data show that the rates of total deaths from these causes have decreased in Argentina and Brazil17-19.
In some of the many multicentre clinical trials on patients with acute AMI, those randomised in Latin America had a slightly higher mortality compared to patients in North America and Europe20. However, trends in Latin America are similar to other parts of the world: there is an increasing use of angioplasty instead of thrombolysis, and a significant number of patients do not undergo reperfusion for a range of reasons, one of the most important being treatment delay21.
Numerous trials have been conducted on pre-hospital thrombolysis22-24. While Latin American trials have not been published in this area, Brazilian authors suggest the strategy could be cost-effective in terms of reducing mortality25.
Centres without facilities for coronary angiography use thrombolysis as their primary approach. In these situations the need to transfer patients for angioplasty is evaluated on a case-by-case basis, taking into account the cost benefit and risk benefit of a transfer21. Patients need to receive quick treatment from clinical and interventional cardiologists and the emergency medical system (EMS) who must understand the importance of early reperfusion therapy when appropriate. Improving the treatment of STEMI requires considering MI to be an emergency that must be managed by an entire system and not just a particular service.
The prevalence of cardiovascular risk factors is increasing in the Mexican population
Cardiovascular diseases are the main cause of death and disability in Mexico17. Ischaemic heart disease is the most prevalent cardiovascular disease and the second cause of overall mortality after diabetes mellitus. It is estimated that cardiovascular diseases decrease life expectancy in Mexico by seven years26. In Mexico, 25% of deaths under 60 years of age are related to chronic degenerative diseases27. It is well known that the development and progression of chronic degenerative diseases are related to lifestyle, and recent studies revealed that 80% of coronary heart disease and 90% of diabetes mellitus can be avoided by adopting a healthier lifestyle28,29.
The prevalence of risk factors is increasing not only in the adult population but also in children and young people. In emerging countries people develop chronic degenerative diseases at younger ages, live with them for longer periods of time and often have complications that could be avoided26. In Mexico there are more than 17 million hypertensives, more than 14 million dyslipidaemias, and more than six million diabetics30. The high level of risk factors in the Mexican population led to an evaluation of the need for research in this area.
The National Registry of Acute Ischemic Coronary Syndromes (RENASICA)
To improve understanding of the profile and treatment of cardiovascular patients in Mexico, in 1998 the National Registry of Acute Ischemic Coronary Syndromes (RENASICA) was initiated31. The registry assessed current practices in relation to coronary risk factors, therapy and outcomes in patients with ACS with and without ST-segment elevation. Data were collected in 18 secondary and tertiary hospitals, of which 79.6% were in the public healthcare system and 14% were private institutions. A total of 4,253 patients were enrolled, including 2,773 (65.2%) without ST-segment elevation and 1,480 (34.8%) with STEMI. The main characteristics of the study are summarised in Table 1.
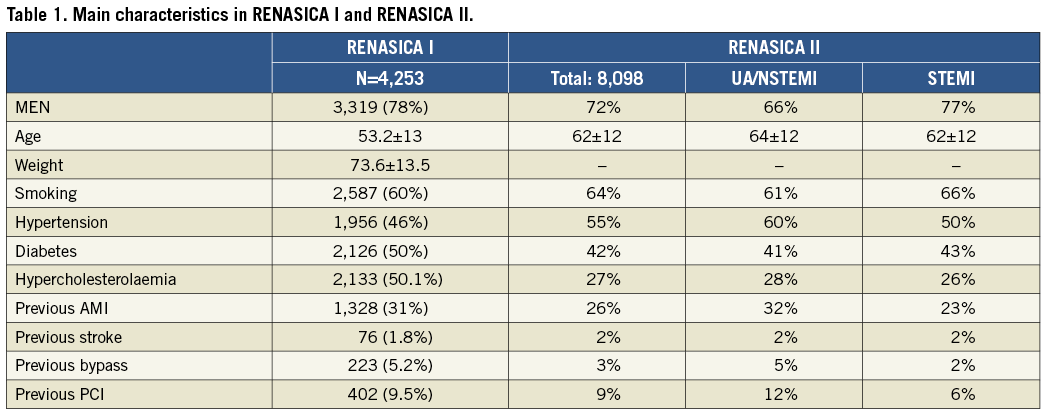
One of the primary objectives was to assess the therapeutic management of these patients. Of the eligible cohort of ACS patients, only 58% (n=2,448) patients had haemodynamic measurements performed. More than half of the patients (55%, n=1,354) received PCI (Figure 3), while coronary bypass surgery was performed in 10.2% (n=435) of patients. Just half (50.4%) of the patients with ACS and STEMI who were eligible for thrombolytic therapy received it.
To extend the knowledge gained in the registry, RENASICA II was launched in 200232. This registry included 8,098 patients with a final diagnosis of ACS. Of these, 3,543 patients had unstable angina or non-ST-elevation myocardial infarction (UA/NSTEMI) and 4,555 had STEMI. Coronary angiography, angioplasty and coronary bypass surgery were performed in 62%, 30% and 8% of UA/NSTEMI patients, respectively, with corresponding rates of 44%, 27% and 4% for the STEMI group (Figure 4). Among patients with STEMI, 37% (n=1,685) had thrombolytic therapy and 15% received primary or facilitated angioplasty.
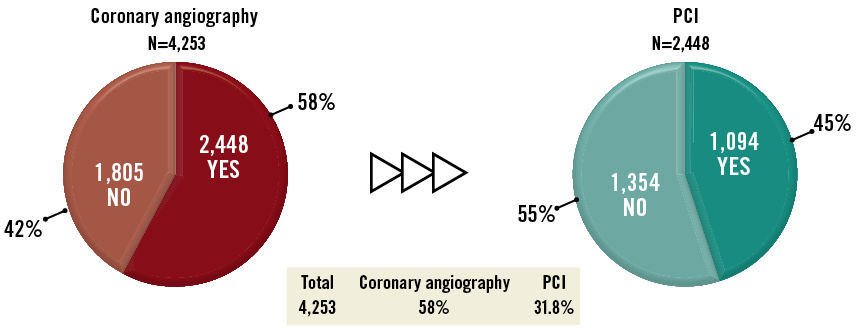
Figure 3. Distribution of patients receiving coronary angiography and PCI in RENASICA I.
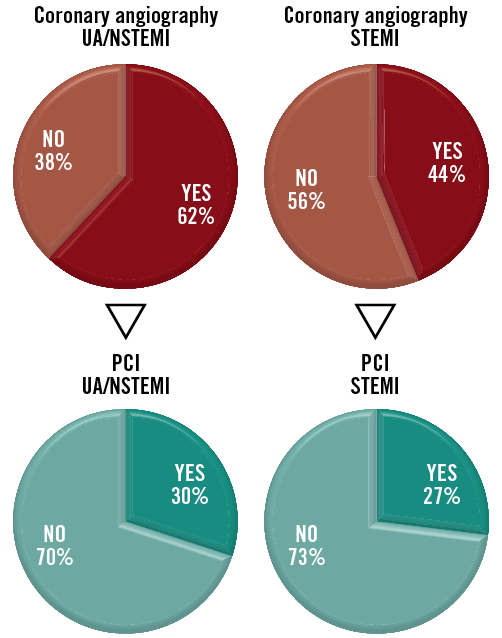
Figure 4. Distribution of patients receiving coronary angiography and PCI in RENASICA II.
The SOCIME registry for national coronary interventions
Following this approach, the Mexican Society of Interventional Cardiology (SOCIME) designed a registry for national coronary interventions. The registry includes data from 250 haemodynamic facilities representing 95% of centres in Mexico. The aim of the registry is to understand the evolution of strategies used during interventions. Information is provided on risk factors, pharmacologic therapy, type of access, types of stent, treatment at discharge and other characteristics of patients receiving PCI.
Preliminary analysis shows that 68% of PCI patients were hypertensive, 62% dyslipidaemic and 42% diabetic. In 80% of PCI patients the final diagnosis was ACS and in 20% it was ischaemic heart disease. Most PCI patients (81%) received drug-eluting stents, and radial access was the primary approach33,34.
Registries have been the main strategy used by the Mexican health authorities for obtaining information about ACS patients that will help them improve the use of health resources to treat this patient group.
Barriers in access to reperfusion therapy in Mexico
CAD awareness is limited in Mexico and many people do not recognise the symptoms of a heart attack. RENASICA II showed that, in 31% of STEMI patients who receive reperfusion therapy, the time between symptom onset and initiation of therapy was less than two hours. This delay was 2 to 4 hours in 36% of patients, 4 to 6 hours in 19% of patients and more than six hours in 15% of patients32.
Just 41% of the Mexican population has social security, while 54% are not covered by any medical service and 5% have private insurance33. Not all STEMI patients are entitled to stents and catheters, and only a few public hospitals have facilities for cardiovascular interventions. Approximately 28% of haemodynamic facilities are public. Public-private partnerships have been established to provide optimal care for every STEMI patient. Some private sponsors donate cathlab materials for people not covered by public insurance.
Mexico has both public and private EMS. The government is updating ambulances and training all staff. A programme called “Codigo Infarto” (Infarction Code) is being introduced in which patients bypass the emergency room and are taken from the ambulance directly to the cathlab for primary PCI. The programme began two years ago in Puebla and is being rolled out across Mexico. The 10 states with the largest populations are currently running Infarction Code. For every 10 ambulances there are three high-technology ambulances. These have wireless communication for transmitting 12-lead ECG results to cathlabs and medical staff. Protocols include helicopter transportation for ACS patients more than two to three hours’ drive from a cathlab. Last year air transportation was used for 30 patients in different states.
The management of cardiovascular patients requires a complex approach which includes genetic, geodemographic, clinical and socioeconomic aspects. In Mexico, epidemiological surveillance systems for chronic degenerative diseases are used by the national health system to define the population at high risk of ischaemic heart disease and encourage first contact physicians to identify patients and provide early treatment. A programme has been established to detect obesity, diabetes mellitus, hypertension, dyslipidaemia and metabolic syndrome by screening all adults over 20 years of age every six months. The need for early interventions to change lifestyle is an urgent priority in emerging countries. Healthy young people without evidence of cardiovascular disease but with one or more risk factors may be predisposed to clinical events that could be prevented.
Conclusion
To build an effective STEMI system of care, partnerships between STEMI-referral hospitals, primary PCI hospitals and EMS teams are critical. An in-depth understanding of healthcare system-level barriers to timely and appropriate reperfusion therapy facilitates the development of more effective strategies for improving the quality of STEMI care in a particular region or country.
The results from reviewed pilot studies in emerging countries revealed that building and integrating regional EMS infrastructures in a stepwise development of STEMI systems of care at a national level is a key prerequisite to support access to a pharmacoinvasive strategy in those areas where primary PCI is not accessible in a given time frame, and a mechanism for inter-hospital transfer of patients is required.
Primary PCI should be a preferred treatment available primarily for patients located close to catheterisation laboratories in urban areas with presumed short transportation time to hospitals equipped with 24/7 primary PCI capabilities. Patients in rural areas, with suspected long transportation time to PCI-capable hospitals, would utilise the pharmacoinvasive strategy with thrombolytic therapy followed by catheterisation and PCI if indicated within three to 24 hours of thrombolysis. It has been observed that a level of lay public education and patient literacy influences the access of STEMI patients to a reperfusion therapy.
Audit and quality control issues need to be addressed at every level. Inspired by the Stent for Life model, by building STEMI systems of care region by region, a majority of patients will have access to a reperfusion therapy in emerging countries in the near future. The model can be applied only by close and enthusiastic collaboration of all stakeholders, respecting the local circumstances.
Conflict of interest statement
The authors have no conflicts of interest to declare.