Published online Oct 27, 2013. doi: 10.4240/wjgs.v5.i10.268
Revised: September 15, 2013
Accepted: October 16, 2013
Published online: October 27, 2013
A 40-year-old male underwent tube placement surgery for continuous ambulatory peritoneal dialysis (CAPD). A 2-cm skin incision was made, and the peritoneum was reflected enough to perform secure fixation. A swan-necked, double-felted silicone CAPD catheter was inserted, and the felt cuff was sutured to the peritoneum to avoid postoperative leakage. An adequate gradient for tube fixation to the abdominal wall was confirmed. The CAPD tube was passed through a subcutaneous tunnel. Aeroperitoneum was induced to confirm that there was no air leakage from the sites of CAPD insertion. Two trocars were placed, and we confirmed that the CAPD tube led to the rectovesical pouch. Tip position was reliably observed laparoscopically. Optimal patency of the CAPD tube was confirmed during surgery. Placement of CAPD catheters by laparoscopic-assisted surgery has clear advantages in simplicity, safety, flexibility, and certainty. Laparoscopic technique should be considered the first choice for CAPD tube insertion.
Core tip: Continuous ambulatory peritoneal dialysis (CAPD) is currently considered the preferred choice for dialytic treatment, based on improved quality of life and patient survival. The open surgical technique for tube placement is easy, though a painful large incision is needed and unexpected tube dislocation may occur. Minimally invasive technique and optimal tube position should be guaranteed in the placement of CAPD catheters. We suggested that placement of CAPD catheters by laparoscopic-assisted surgery has clear advantages in simplicity, safety, flexibility, and certainty. Here, we present our surgical procedures and discuss key techniques and pitfalls with literature review.
- Citation: Hori T, Nakauchi M, Nagao K, Oike F, Tanaka T, Gunji D, Okada N. Laparoscopic-assisted catheter insertion for continuous ambulatory peritoneal dialysis: A case report of simple technique for optimal placement. World J Gastrointest Surg 2013; 5(10): 268-271
- URL: https://www.wjgnet.com/1948-9366/full/v5/i10/268.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v5.i10.268
Peritoneal dialysis (PD) is considered the first choice for dialytic treatment because it offers improved quality of life and patient survival compared with hemodialysis. PD, including continuous ambulatory peritoneal dialysis (CAPD), is widely used in the treatment of end-stage renal failure[1-3]. The most frequent complications of PD are peritonitis[4-6], infection of the catheter exit site[7-9], mechanical complications[2,10,11], and dialysate leakage[12-14].
CAPD catheter insertion by the open method is easy, though a painful large incision is needed and unexpected tube dislocation may occur. With open surgery, minimally invasive technique and optimal tube position should be assured. Recent surgical innovations and technological improvements have been made, mainly in laparoscopic and laparoscopic-assisted surgery and advanced devices[2,10,11,13,15-19]. We present a case of laparoscopic-assisted catheter placement for CAPD induction in detail, and discuss key techniques and pitfalls for this minimally-invasive surgery.
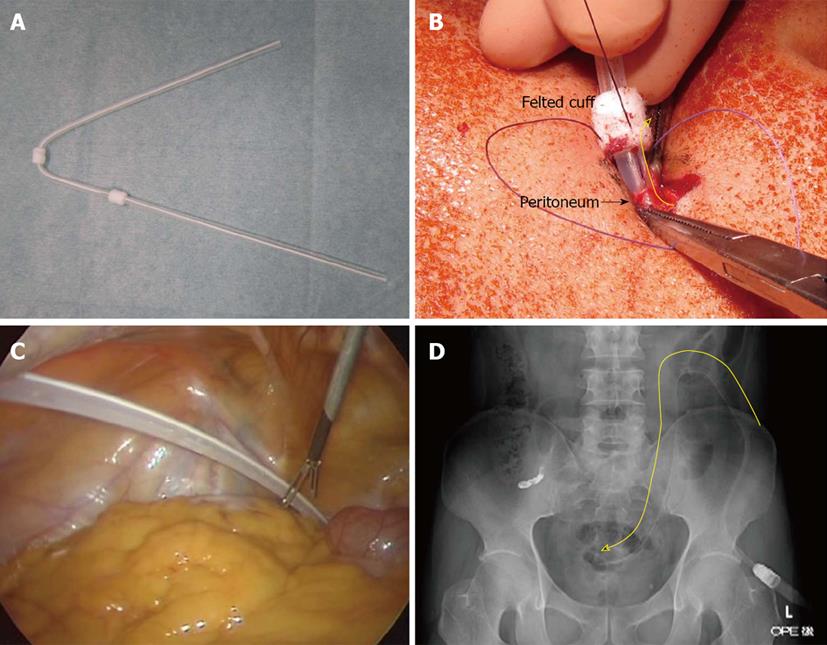
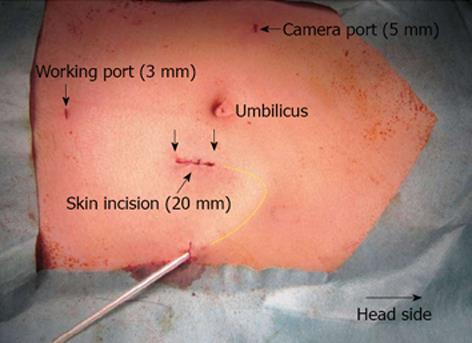
A 40-year-old male suffered from renal failure due to immunoglobulin a nephropathy, and CAPD was introduced using a swan-necked, double-felted silicone catheter (JB-5; JMS Co. Ltd., Osaka, Japan; Figure 1A). Site marking was performed before surgery. After induction of general anesthesia, a urethral catheter was inserted to avoid bladder injury during surgery. A 2-cm skin incision was made, and the peritoneum was opened at the most caudal point to insert the CAPD tube (Figure 2). The abdominal wall was lifted with Kocher’s forceps, and a 5-mm trocar for a camera was placed opposite the site of subcutaneous tube fixation after confirmation of intra-peritoneal adhesion (Figure 2). The peritoneum was reflected enough to perform secure fixation. The CAPD tube was inserted, and the felt cuff was sutured to the peritoneum with a tight running pattern to avoid postoperative leakage, using absorbable, atraumatic suture material (Figure 1B). The CAPD tube passed under the fascia, and the fascia was tightly closed from the caudal end with interrupted sutures. Hence the CAPD tube passed through the fascia at the most cranial aspect (Figure 2). An adequate gradient for tube fixation to the abdominal wall for a well-orientated catheter was confirmed. Subcutaneous tunneling was performed to accommodate the shape of the swan neck. The CAPD tube was passed through this tunnel, and the second felt was placed subcutaneously (Figure 2). Buried absorbable sutures were used for skin closure.
Aeroperitoneum was induced to confirm that there was no air leakage from the sites of CAPD insertion. A 5-mm laparoscope was inserted. No adhesions or ascites were observed. A 3-mm trocar was placed in the lower abdominal wall near the pubic bone as a working port, without bladder injury. The catheter had already been directed by the fixation to the abdominal wall. The CAPD tube was grasped with 3-mm laparoscopic forceps (Figure 1C). We confirmed by laparoscopy that the CAPD tube led to the rectovesical pouch (Figure 1C), and no stylet was required for tube placement. Tip position was reliably observed laparoscopically. Enough carbon dioxide gas was removed from the trocar wound to prevent iatrogenic eosinophilic peritonitis, and the stab wounds for trocar placement were closed with buried absorbable sutures. The CAPD tube had a radiodense line, and intraoperative radiographs revealed optimal and reasonable curve of the CAPD tube (Figure 1D). Intentional discrepancy between the preperitoneal fixation points in the peritoneum and fascia as described above resulted in an adequate curve without any distortions (Figure 1D). Optimal patency of the CAPD tube should be confirmed during surgery. Normal saline (100 mL) was injected through the CAPD tube, and then a total of 79 mL was retrieved (79% retrieval rate). Total operative time for all procedures was 45 min.
The patient received a second-generation cephem antibiotic intravenously until postoperative day 3, and the postoperative course was uneventful. CAPD was introduced during the early postoperative period without obstruction, leakage, or infection.
PD including CAPD is currently considered the preferred choice for dialytic treatment, based on improved quality of life and patient survival. The open surgical technique for tube placement is easy, though a painful large incision is needed and unexpected tube dislocation may occur. Minimally invasive technique and optimal tube position should be guaranteed in the placement of CAPD catheters, and many physicians have established excellent laparoscopic techniques and advanced devices[2,10,11,13,15-19]. Patients in renal failure may have concurrent peritonitis, and peritonitis can also occur after CAPD induction[20-22]. In patients with mild ascites, sampling for culture or neutrophil counts is very easy with laparoscopy. Even though CAPD tubes are specially-designed devices, an artificial catheter is a foreign body. We suggest that bacteriological and microbiological assessments should be routinely performed during laparoscopic surgery if mild ascites is present.
Complications of CAPD include peritonitis, infection of the catheter exit site, mechanical obstruction, and dialysate leakage[2,4-14]. Many surgeons have previously demonstrated that laparoscopic surgery reduced these complications[2,10,11,15,17,23]. Omental wrap or plugging is one cause of mechanical obstruction[24,25]. Fibroadhesion and sclerosing peritonitis also decrease tube efficiency[26,27]. These mechanical obstructions require omentopexy, omentectomy, and other additional surgeries[22,23]. So-called ‘‘abdominal cocoon syndrome’’ can result in death and requires removal or reinsertion of the catheter[26,27]. Laparoscopic surgery has the advantage of flexible catheter placement according to intra-abdominal findings to prevent these complications[16].
Laparoscopic surgery results in less pain, shortened convalescence, improved cosmesis, and absence of wound complications[15,19,28]. A simple question arises: Is pure laparoscopic surgery better than laparoscopically-assisted surgery? Pure laparoscopic surgery has been documented to be an ideal technique for the placement of CAPD catheters[10,19]. Reports suggest that pure laparoscopic surgery has the advantage of preventing major complications in CAPD[10,19]. We agree that laparoscopic surgery offers many advantages in CAPD tube placement, but suggest that pure laparoscopic surgery requires more advanced techniques and involves technical difficulties because of the tangential view and access, especially in securely fixing the catheter to the peritoneum. We agree that pure laparoscopic surgery is ideal, but only in the hands of experienced surgeons. Laparoscopic surgery using single and two-port methods have been reported[17,18]. We employed two ports because it allowed greater flexibility for intraoperative procedures and required only a negligible second stab wound for a 3-mm port.
It has been reported that a pure laparoscopic intra-peritoneal approach has the advantage of ensuring adequate insertion, which prevents mechanical obstruction and allows secure fixation to the peritoneum, preventing intractable leakage[10]. However, we found a 2-cm incision to be large enough for an optimal lead and secure catheter fixation. Mechanical obstruction[2,10,11] and dialysate leakage[12-14] are still the most serious complications in CAPD, and reasonable tube placement with secure fixation to the peritoneum are extremely important during surgery. We performed laparoscopic-assisted surgery with a minimally open method to create an adequate preperitoneal tube curve with secure fixation to the peritoneum. An adequate gradient for tube fixation to the abdominal wall can be made even with a 2-cm incision.
Image studies are important in CAPD tube placement[12,29]. Intraoperative radiographs revealed that our intentional discrepancy between the peritoneal and fascial fixation points worked well to create an optimal tube curve without any distortions and with a secure tip position.
Placement of CAPD catheters by laparoscopic-assisted surgery has clear advantages for simplicity, safety, flexibility, and certainty. Laparoscopic technique should be considered the first choice for CAPD tube insertion. In conclusion, laparoscopic approach is a very useful tool in the induction of PD programs.
P- Reviewers Ker CG, Hori T S- Editor Zhai HH L- Editor A E- Editor Lu YJ
| 1. | Mirković TD. Peritoneal dialysis--experiences. Med Pregl. 2010;63:753-757. [PubMed] [Cited in This Article: ] |
| 2. | Gultekin FA, Cakmak GK, Karakaya K, Emre AU, Tascilar O, Oner MO, Comert M, Kulah E. Our long-term results of Tenckhoff peritoneal dialysis catheters placement via laparoscopic preperitoneal tunneling technique. Semin Dial. 2013;26:349-354. [PubMed] [Cited in This Article: ] |
| 3. | Wyld M, Morton RL, Hayen A, Howard K, Webster AC. A systematic review and meta-analysis of utility-based quality of life in chronic kidney disease treatments. PLoS Med. 2012;9:e1001307. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 306] [Cited by in F6Publishing: 318] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 4. | Vikrant S, Guleria RC, Kanga A, Verma BS, Singh D, Dheer SK. Microbiological aspects of peritonitis in patients on continuous ambulatory peritoneal dialysis. Indian J Nephrol. 2013;23:12-17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Barone RJ, Cámpora MI, Gimenez NS, Ramirez L, Panese SA, Santopietro M. Continuous ambulatory peritoneal dialysis versus automated peritoneal dialysis and peritonitis in the short and very long term at risk. Adv Perit Dial. 2012;28:44-49. [PubMed] [Cited in This Article: ] |
| 6. | Gardenier JC, Sawyer RG, Sifri CD, Brayman K, Wispelway B, Bonatti H. Peritonitis caused by Haemophilus parainfluenzae, Leifsonia aquatica, and Gordonia spp. in a patient undergoing continuous ambulatory peritoneal dialysis. Surg Infect (Larchmt). 2012;13:409-412. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Lo MW, Mak SK, Wong YY, Lo KC, Chan SF, Tong GM, Lo KY, Wong PN, Tse CW, Kam KM. Atypical mycobacterial exit-site infection and peritonitis in peritoneal dialysis patients on prophylactic exit-site gentamicin cream. Perit Dial Int. 2013;33:267-272. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 8. | Cho KH, DO JY, Park JW, Yoon KW. Catheter revision for the treatment of intractable exit site infection/tunnel infection in peritoneal dialysis patients: a single centre experience. Nephrology (Carlton). 2012;17:760-766. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Koch LD, Knoll F, Hartmann G, Lhotta K. Recurrent exit-site infection due to Staphylococcus lugdunensis--a virulent coagulase-negative Staphylococcus. Perit Dial Int. 2011;31:372-373. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Bae IE, Chung WK, Choi ST, Kang J. Laparoscopic internal fixation is a viable alternative option for continuous ambulatory peritoneal dialysis catheter insertion. J Korean Surg Soc. 2012;83:381-387. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Zakaria HM. Laparoscopic management of malfunctioning peritoneal dialysis catheters. Oman Med J. 2011;26:171-174. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Markić D, Zivcić-Cosić S, Valencić M, Miletić D, Rahelić D, Krpina K, Maricić A, Pavlović I, Racki S, Fuckar Z. [The role of CT peritoneography as diagnostic tool in patient on peritoneal dialysis with dialysate leakage]. Acta Med Croatica. 2011;65 Suppl 3:95-98. [PubMed] [Cited in This Article: ] |
| 13. | Pantea S, Pantea C, Lazăr F, Bordoş D, Păpurică M, Bălaşa-Guragata C, Nicoară S, Mateş A. [Laparoscopic placement of Tenchkhoff catheter for peritoneal dialysis--surgical technique]. Chirurgia (Bucur). 2008;103:591-593. [PubMed] [Cited in This Article: ] |
| 14. | Lin MY, Wu CC. Hydrocele in a peritoneal dialysis patient: hernia or leakage. Intern Med. 2011;50:3047-3048. [PubMed] [Cited in This Article: ] |
| 15. | Permpongkosol S, Nontakaew K. Laparoendoscopic single-site nephrectomy for patients with dialysis-dependent end stage renal disease. J Med Assoc Thai. 2012;95:607-613. [PubMed] [Cited in This Article: ] |
| 16. | Kazemzadeh G, Modaghegh MH, Tavassoli A. Laparoscopic correction of peritoneal catheter dysfunction. Indian J Surg. 2008;70:227-230. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Blessing WD, Ross JM, Kennedy CI, Richardson WS. Laparoscopic-assisted peritoneal dialysis catheter placement, an improvement on the single trocar technique. Am Surg. 2005;71:1042-1046. [PubMed] [Cited in This Article: ] |
| 18. | Caliskan K, Nursal TZ, Tarim AM, Noyan T, Moray G, Haberal M. The adequacy of laparoscopy for continuous ambulatory peritoneal dialysis procedures. Transplant Proc. 2007;39:1359-1361. [PubMed] [Cited in This Article: ] |
| 19. | Attaluri V, Lebeis C, Brethauer S, Rosenblatt S. Advanced laparoscopic techniques significantly improve function of peritoneal dialysis catheters. J Am Coll Surg. 2010;211:699-704. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 20. | Solak Y, Biyik Z, Demircioglu S, Polat I, Genc N, Turkmen K, Turk S. Brucella peritonitis in peritoneal dialysis: a case report and review of the literature. Perit Dial Int. 2012;32:126-130. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Li PK, Chow KM. Infectious complications in dialysis--epidemiology and outcomes. Nat Rev Nephrol. 2012;8:77-88. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 56] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 22. | Sinnakirouchenan R, Holley JL. Peritoneal dialysis versus hemodialysis: risks, benefits, and access issues. Adv Chronic Kidney Dis. 2011;18:428-432. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 94] [Cited by in F6Publishing: 113] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 23. | Vagefi PA, Freise CE. Fibrin plug. Kidney Int. 2010;78:942. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Kavalakkat JP, Kumar S, Aswathaman K, Kekre NS. Continuous ambulatory peritoneal dialysis catheter placement: Is omentectomy necessary? Urol Ann. 2010;2:107-109. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Goh YH. Omental folding: a novel laparoscopic technique for salvaging peritoneal dialysis catheters. Perit Dial Int. 2008;28:626-631. [PubMed] [Cited in This Article: ] |
| 26. | Tseng WC, Tarng DC. Cocoon-like fibroadhesive tuberculous peritonitis in a peritoneal dialysis patient. Chin J Physiol. 2012;55:361-365. [PubMed] [Cited in This Article: ] |
| 27. | Noormohamed MS, Kadi N. Abdominal cocoon in peritoneal dialysis--a fatal outcome. BMJ Case Rep. 2012;2012. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 28. | Varela JE, Elli EF, Vanuno D, Horgan S. Mini-laparoscopic placement of a peritoneal dialysis catheter. Surg Endosc. 2003;17:2025-2027. [PubMed] [Cited in This Article: ] |
| 29. | Goldstein M, Carrillo M, Ghai S. Continuous ambulatory peritoneal dialysis-a guide to imaging appearances and complications. Insights Imaging. 2013;4:85-92. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |