Published online Oct 15, 2022. doi: 10.4239/wjd.v13.i10.809
Peer-review started: May 13, 2022
First decision: August 1, 2022
Revised: August 6, 2022
Accepted: September 8, 2022
Article in press: September 8, 2022
Published online: October 15, 2022
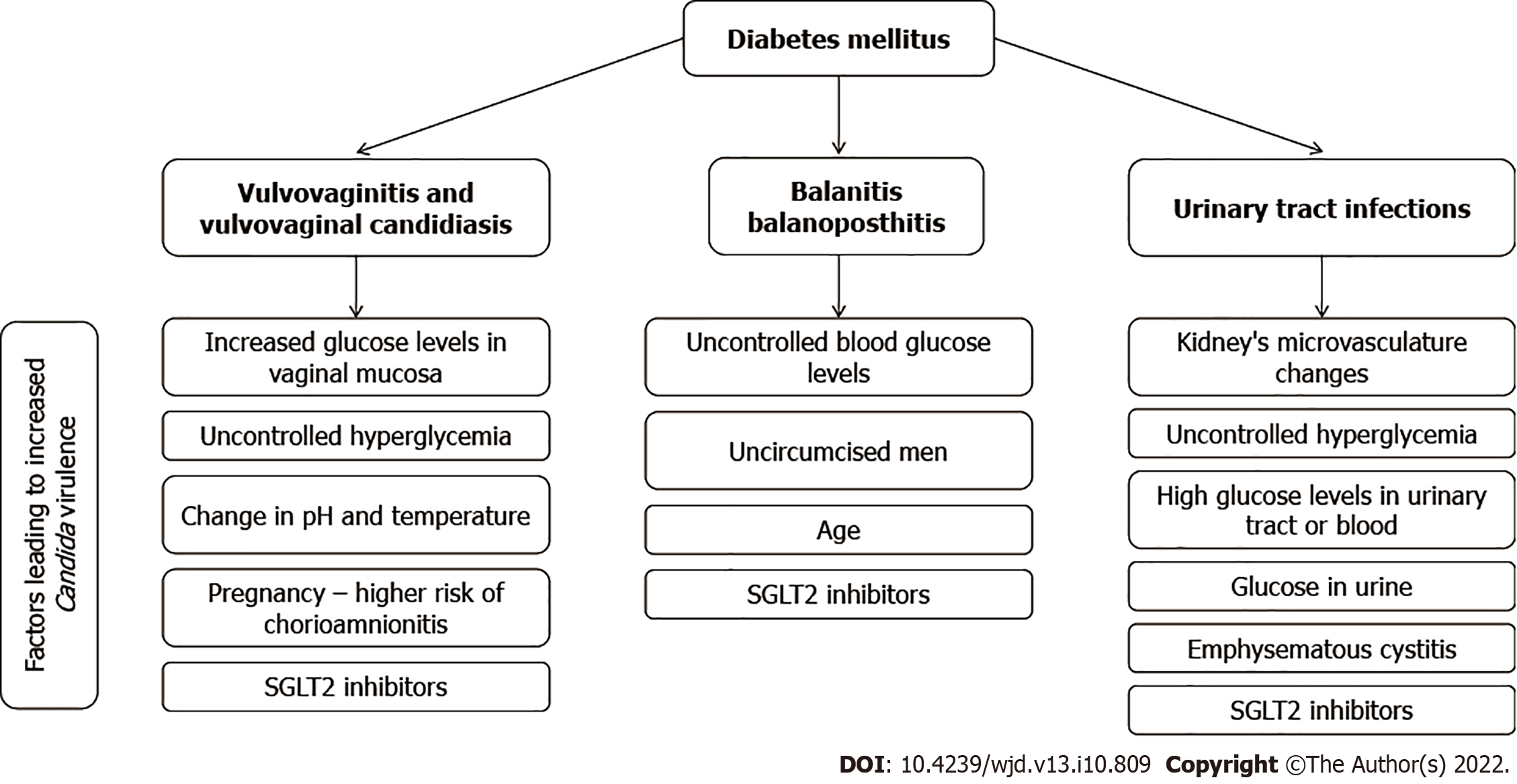
Both diabetes and fungal infections contribute significantly to the global disease burden, with increasing trends seen in most developed and developing countries during recent decades. This is reflected in urogenital infections caused by Candida species that are becoming ever more pervasive in diabetic patients, particularly those that present with unsatisfactory glycemic control. In addition, a relatively new group of anti-hyperglycemic drugs, known as sodium glucose cotransporter 2 inhibitors, has been linked with an increased risk for colonization of the urogenital region with Candida spp., which can subsequently lead to an infectious process. In this review paper, we have highlighted notable virulence factors of Candida species (with an emphasis on Candida albicans) and shown how the interplay of many pathophysiological factors can give rise to vulvovaginal candidiasis, potentially complicated with recurrences and dire pregnancy outcomes. We have also addressed an increased risk of candiduria and urinary tract infections caused by species of Candida in females and males with diabetes, further highlighting possible complications such as emphysematous cystitis as well as the risk for the development of balanitis and balanoposthitis in (primarily uncircumcised) males. With a steadily increasing global burden of diabetes, urogenital mycotic infections will undoubtedly become more prevalent in the future; hence, there is a need for an evidence-based approach from both clinical and public health perspectives.
Core Tip: The global health burden of both diabetes and Candida spp. infections is on the rise, and these two clinical entities can have a compounding effect on the development of different urogenital diseases and syndromes. Pathophysiological changes observed in diabetes mellitus can predispose individuals to Candida colonization, increased virulence of this fungus, and subsequent infection. Diabetic females are more prone to recurrent vulvovaginal candidiasis that can endanger the pregnancy, while diabetic males have higher rates of balanitis/balanoposthitis. In both females and males, there is an increased risk of candiduria and urinary tract infections, with complications such as emphysematous cystitis.
- Citation: Talapko J, Meštrović T, Škrlec I. Growing importance of urogenital candidiasis in individuals with diabetes: A narrative review. World J Diabetes 2022; 13(10): 809-821
- URL: https://www.wjgnet.com/1948-9358/full/v13/i10/809.htm
- DOI: https://dx.doi.org/10.4239/wjd.v13.i10.809
Diabetes is a salient global health issue, with an enormous disease burden that has increased substantially in recent decades for the majority of developed and developing countries. The estimations from the International Diabetes Federation reveal that 537 million adults are living with diabetes around the world, with a projected growth to 693 million or more by 2045 without effective preventative methods[1,2]. On the other hand, the estimates from the Global Action Fund for Fungal Infections show that every year there are over 300 million individuals of all ages suffering from a fungal infection that can seriously impact their health[3], which also includes urogenital infections caused by yeasts belonging to the genus Candida.
Taking into account such considerable global prevalence of these two frequently coexistent clinical conditions, it is of no wonder that diabetic patients with genitourinary candidiasis are currently pervasive not only in primary practice but also in secondary and tertiary care facilities. In addition, a relatively new group of anti-hyperglycemic drugs known as sodium glucose cotransporter 2 (SGLT2) inhibitors made both females and males more prone to Candida colonization of the urogenital region as well as for subsequent infection[4-6]. All of this means urogenital Candida infections may become even more ubiquitous among diabetic patients in the future. Therefore, given the scarcity of recent and comprehensive sources that provide an integrative and critical overview of the available literature on this topic (Table 1), in this review we aimed to summarize microbiological, pathophysiological, and clinical facets of urogenital infections with Candida species in both females and males with diabetes.
| Keywords | MeSH term | Database |
| Balanitis | Balanitis | PubMed, Scopus, RCA |
| Balanoposthitis | - | PubMed, Scopus, RCA |
| Vulvovaginitis | Vulvovaginitis | PubMed, Scopus, RCA |
| Urogenital infections | Urogenital system; infections; pathogenicity | PubMed, Scopus, RCA |
| Pregnancy | Pregnancy | PubMed, Scopus, RCA |
| Candida | Candida | PubMed, Scopus, RCA |
| Candidiasis | Candidiasis | PubMed, Scopus, RCA |
| Diabetes | Diabetes mellitus; diabetes insipidus | PubMed, Scopus, RCA |
According to the classification published by the American Diabetes Association, diabetes occurs in four basic forms, of which diabetes mellitus type 1 and diabetes mellitus type 2 are the most common forms of the disease[7]. In the quotidian clinical approach, fasting blood glucose levels up to 5.6 mmol/L are normal. When these values are above 7 mmol/L, this represents a key criterion for diagnosing diabetes mellitus, while values between 5.6 mmol/L and 6.9 mmol/L indicate prediabetes[8]. Therefore, it is always necessary to perform two glucose measurements: the first one on an empty stomach; and the second 1-2 h after a meal. Glucose values 2 h after a meal should fall below 7.8 mmol/L; if these values are still above 11 mmol/L, then we can diagnose diabetes mellitus with a substantial amount of certainty. If these values are between 7.8 to 11 mmol/L, we consider prediabetes or glucose intolerance[9]. The vital difference between prediabetes and diabetes is that prediabetes can be reversed. Of course, the most crucial factors are lifestyle changes, but there are also several viable pharmacological approaches.
Type 1 diabetes mellitus is caused by an absolute (or almost absolute) lack of insulin due to autoimmune destruction of pancreatic β-cells, which leads to insulin insufficiency and hyperglycemia[10]. Conversely, type 2 diabetes mellitus is characterized by insulin resistance with an inadequately compensatory increase in insulin secretion[11]. Gestational diabetes occurs in pregnancy, most often during the second trimester of pregnancy. Insulin resistance is potentiated by hormones produced by the placenta[12]; therefore, it occurs in females whose pancreatic function does not overcome pregnancy-related insulin resistance. The main consequences are increased risks of preeclampsia, macrosomia, as well as Cesarean delivery and their associated morbidities[13].
Diabetes mellitus is one of the most common endocrine disorders characterized by a disorder in insulin secretion and its action. Due to its frequency, it is currently a global health problem[14]. The prevalence of diabetes mellitus is constantly increasing in developed and developing countries alike. According to the data from 2017, its prevalence is around 8.8% worldwide[15]. In addition to a myriad of co-occurring problems characteristic of patients with diabetes mellitus, a particular issue is immune system dysfunction resulting from complex interactions between the endocrine and immune systems[16]. Immune dysfunction occurs due to elevated insulin levels (hyperglycemia) and leptin present in affected individuals, resulting in an increased risk of various organ damage[17].
Decreased immunity is manifested in decreased T lymphocyte count, reduced cytokine release, increased programmed leukocyte cell death, reduced neutrophil function, impaired ability to fight infectious agents, and increased susceptibility to infection[14]. The increased risk of opportunistic infections is a particular problem due to the weakened ability to fight invasive pathogens[18]. In patients with diabetes mellitus, the recovery time after infection is significantly prolonged compared to individuals without it[19]. One of the salient indicators that should raise a suspicion of underlying diabetes is a propensity for recurrent infections caused by opportunistic pathogenic fungal species belonging to the genus Candida[20]. The pathogenic abilities of Candida species and their colonization factors depend on host-related immune factors due to the intricate homeostatic relationship of fungi with the host’s current immune status, a key determinant of commensalism or parasitism[21]. From a pathophysiological perspective, we find a suitable environment in diabetic patients for Candida multiplication and proliferation due to alteration of gut microbiota, dietary changes, reduced intestinal secretions and altered liver function, continued usage of antimicrobial agents (and other drugs), coexisting diseases, as well as the pervasive deficiency of key nutrients, as demonstrated in the literature[21].
Fungal infections caused by Candida species lead to a significant health burden, causing high mortality rates, hospitalizations, and increased treatment costs[22]. Lethal outcomes are most commonly seen as a result of sepsis and invasive systemic candidiasis[23].
Candida albicans was the most widespread fungal pathogen isolated during episodes of candidiasis for a long time. Still, recent literature reports reveal an increasingly important role of other non-albicans species such as Candida glabrata (C. glabrata), Candida parapsilosis (C. parapsilosis), Candida krusei (C. krusei), Candida tropicalis (C. tropicalis), and more recently Candida auris (C. auris)[24]. However, the most commonly isolated Candida spp. from clinical specimens are non-albicans species. These other non-albicans Candida species are becoming more noticeable due to the production of virulence factors that were once attributed exclusively to C. albicans; furthermore, they are also characterized by reduced sensitivity to the most commonly used antifungal drugs[25]. The prevalence and virulence of non-albicans Candida species show varied geographical distribution, but more importantly many non-albicans Candida species cause more frequent fungal infections in patients with diabetes. That is especially pertinent for patients with type 1 and 2 diabetes mellitus with foot ulcers and skin and nail lesions[6]. Considering all of the above, species-level identification of Candida spp. should be introduced into routine laboratory work-up[26].
But notwithstanding such global prominence of non-albicans candida, C. albicans is still the most common cause of candidiasis[27]. It can be a colonizer of skin and many mucosal surfaces and can thus easily act as an opportunistic pathogen in the genitourinary system[28]. Approximately 75% of females have at least one episode of vulvovaginal candidiasis during their lifetime, and the most common cause (i.e. in 90% of cases) the putative species is C. albicans[29]. According to available data, in females with diabetes mellitus who presented with a vulvovaginal infection caused by Candida, C. albicans is the most prevalent fungus in over 50% of cases, while different non-albicans Candida species are present in about 40% of cases[30].
Candida is a polymorphic fungus that, contingent on the environment in which it is located, can alter its morphology from yeast form (blastoconidia) to pseudohyphae and hyphae[31]. Indeed, this is one of the most important differences from other Candida species because it can create true hyphae in vivo when met with favorable conditions[32]. Two serotypes of C. albicans have been identified, namely type A and type B[33], and numerous factors contribute to the noticeable increase in invasive fungal infections, including hyperglycemia[19].
Virulence represents the ability of a microorganism to damage a host[34], and C. albicans possesses a panoply of virulence factors[35]. One of the most important factors is dimorphism (already mentioned), which represents the ability of C. albicans to change its shape from yeast to mold, with subsequent formation of true hyphae under favorable conditions. The latter trait significantly increases its invasiveness and proteolytic activity; however, in yeast form, it shows the propensity for greater dissemination[36]. Genes that are important for these activities are ALS3, SAP4-6, HWP1, HYR1, and ECE1, and their expression can be variable[37], while SAP1 and SAP3 and SAP8 genes have been correlated with vaginal infections[38].
In the first phase of the infection, which is the adhesion phase, adhesins and invasins allow C. albicans cells to adhere to the substrate, forming a basal layer of cells[39]. Adhesins are glycoproteins that enable yeast to adhere to epithelial and endothelial cells[40]. Invasins are specialized proteins by which C. albicans stimulates host cells towards endocytosis by binding to host cell ligands[41]. The target ligands are E-cadherin on epithelial cells and N-cadherin on endothelial cells[42]. Numerous genes are involved in adhesion to epithelial cells, and the large cell surface area of the glycoprotein encodes eight genes belonging to the C. albicans agglutinin-like sequence family[43].
Biofilm production is recognized as a crucial virulence factor (Table 2)[44]. In the proliferation stage of C. albicans cells, filaments are formed, in which yeast cells begin to develop filamentous hyphae. That is the most critical step in which cells can change their morphology, facilitating in turn biofilm formation on the mucosal surfaces of the host[45,46]. The biofilm formation process is controlled by six genes (EFG1, BCR1, BRG1, NDT80, TEC1, and ROB1) that belong to the transcriptional regulatory network[47,48].
| Phase | Phase name | Description |
| 1 | Adherence | In the first 3 h, individual C. albicans cells adhere to the substrate, which forms the basal layer of the biofilm |
| 2 | Intermediate phase | In 11-14 h, biofilm is shaped during this phase of cell proliferation and filamentation, in which the formation of hyphae occurs, marking the beginning of true biofilm formation |
| 3 | Maturation phase | In 20-48 h, there is a complete penetration of all layers of cells attached to the surface; extracellular polysaccharide matrix accumulates at this stage of maturation |
| 4 | Dispersion | After 24 h, the final phase involves separation of non-adherent cells from the biofilm, resulting in possible development of new biofilms and dissemination in the tissue |
Alongside the aforementioned virulence factors, it is also becoming clear that C. albicans isolated from patients with diabetes mellitus has more pronounced pathogenic properties[49]. Namely, the hyp-erglycemic environment, rich in carbohydrates, serves as a source of energy indispensable for producing biofilms and matrices that protect fungal cells from external influences[6]. Most pathological conditions caused by C. albicans are associated with biofilm formation on abiotic surfaces or host surfaces[50]. Yeast cells dispersed from mature biofilm are more virulent and have a more remarkable ability to adhere to surfaces to form new biofilms than planktonic ones[51]. Biofilm production also complicates treatment and contributes to high morbidity and mortality rates[52].
C. albicans can produce the cytolytic enzyme known as candidalizine, and hyphae are responsible for its secretion[44]. This enzyme plays a vital role in developing vaginal mucosal infections[53]. More specifically, candidalizine has immunomodulatory properties critical in host cell damage[54] and plays a role in neutrophil recruitment during disseminated systemic fungal infections[55].
A direct contribution to the virulence of C. albicans is the secretion of hydrolytic enzymes aspartyl proteinase and phospholipase as well as hemolysin, which all enhance pathogenic effects such as binding to host tissue and rupture of the cell membrane. As a result of their activity, the invasion of the mucosal surface is facilitated, and they are also responsible for avoiding the host’s immune response[46,56,57]. In C. albicans, at least ten members of the aspartyl proteinase gene family are present, while phospholipase has been reported in four families[58].
Finally, one of the essential contributors to C. albicans virulence is thigmotropism (contact sensing), which is regulated by extracellular calcium intake and aids significantly in spreading into host tissues and biofilm development[44].
Several important pathophysiological mechanisms are involved in the occurrence of vulvovaginitis and vulvovaginal candidiasis (VVC) in individuals with uncontrolled hyperglycemia, leading to increased glucose levels in vaginal mucosa[6]. First of all, yeasts can utilize the glucose found in secretions as a viable nutrient, and additional influence of the overall change in pH and temperature can result in increased Candida spp. virulence[59]. Furthermore, the binding of Candida spp. to epithelial cells on the vaginal surface represents a pivotal initial step in colonization and ensuing infection with yeasts[60], with an indispensable role of intercellular adhesion molecule 1 expression for facilitating adhesion after the episodes of hyperglycemia[61]. Recurrent episodes of VVC are more frequent in diabetic patients due to immune suppression, altered leukocyte function, and a myriad of other factors[21].
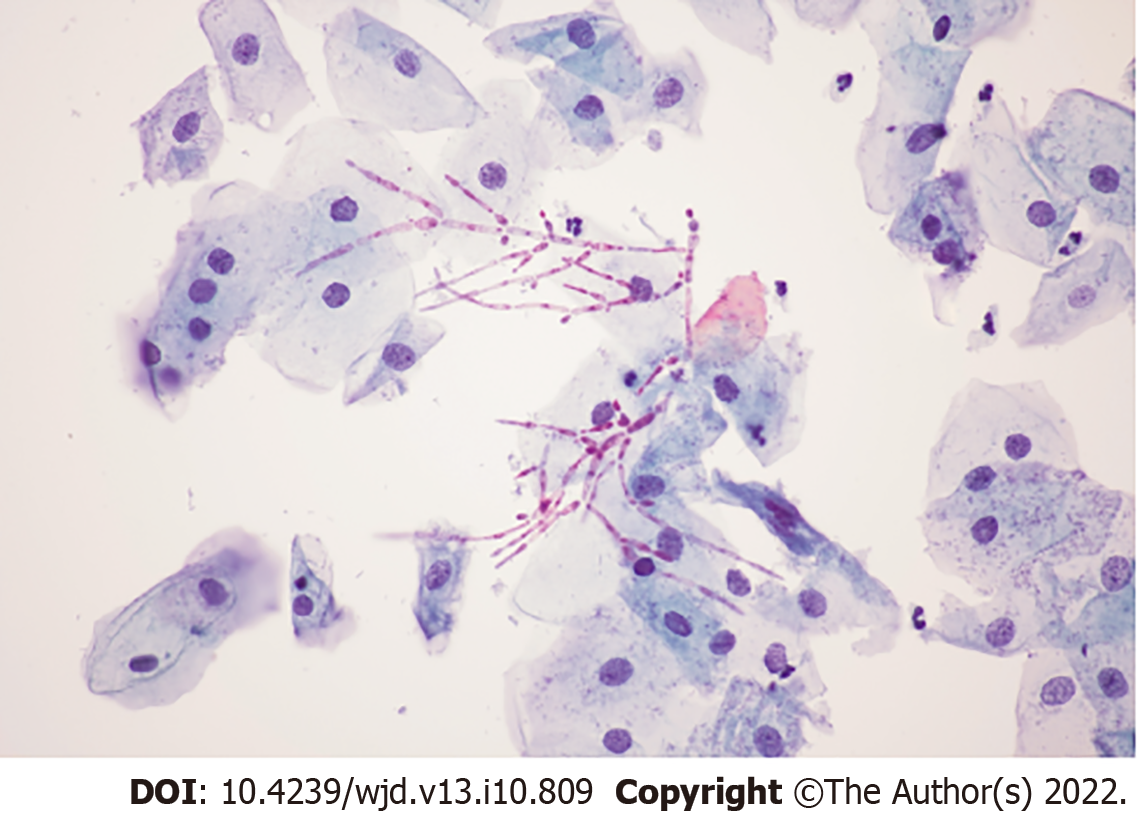
Several different author groups appraised the association between VVC and diabetes mellitus. For example, Gunther et al[30] studied females with diabetes from Brazil and found that Candida species were more frequently isolated in them than in those without it (18.8% vs 11.8%); likewise, the development of VVC (both isolated and recurrent forms) has been more frequently observed in the diabetic group of patients, together with lower cure rates. In a study on postmenopausal females with diabetes and symptoms of VVC, Candida spp. were isolated in 15.6% of involved patients using culturing techniques and molecular confirmation with C. albicans leading the way in frequency (59.30%), followed by C. glabrata (24.41%) and C. krusei (16.27%)[62]. These studies also showed different antifungal susceptibilities of isolated species, which is why mycological culture is often endorsed, even though microscopy is often sufficient for visualizing recognizable fungal elements such as pseudohyphae of C. albicans (Figure 1).
However, non-albicans Candida species are increasingly implicated in VVC in cases of patients with diabetes. In a research endeavor by Ray et al[63], which explored cure rates of different treatment modalities, C. glabrata has been cultured in 61.3% and C. albicans in 28.8% of 111 female individuals with VVC and diabetes. A study by Goswami et al[64], conducted on diabetic females from India, showed a relatively high prevalence (46%) of VVC with a relative risk of 2.45 and a predominance of C. glabrata and C. tropicalis. Such dominance of C. glabrata in the same context was confirmed by another study from India[65], showing that all therapeutic considerations have to consider country- and region-specific pathogen distribution (Table 3).
| Ref. | Yr | Study population | Study outcome |
| Goswami et al[64] | 2000 | n = 78 diabetics, n = 88 non-diabetics | A total of 46% of diabetic patients showed vaginal Candida sp. and 23% healthy subjects demonstrated Candida spp. |
| Goswami et al[65] | 2006 | n = 85 diabetics, n = 62 non-diabetics | A total of 67.1% of diabetic patients showed vaginal Candida spp. and 47.3% healthy subjects demonstrated Candida spp. following fluconazole treatment |
| Gunther et al[30] | 2014 | n = 48 diabetics; n = 669 non-diabetics | A total of 18.8% of diabetics showed vaginal Candida spp. and 11.8% healthy subjects demonstrated Candida spp. |
| Yokoyama et al[5] | 2019 | 65 diabetic patients | A total of 36.9% of diabetic patients converted to a positive vaginal Candida spp. |
| Halteet et al[62] | 2020 | 550 diabetic patients | A total of 15.6% of diabetics showed vaginal Candida spp. |
| Lisboa et al[71] | 2010 | n = 38 diabetics; n = 440 non-diabetics | A total of 26.2% of males had Candida spp. and 18% of males had balanitis; 13.8% of diabetic patients had balanitis |
| Kofteridis et al[84] | 2009 | n = 88 diabetics; n = 118 non-diabetics | A total of 12.7% of diabetic patients showed urinary tract Candida spp. and 1.7% healthy subjects demonstrated Candida spp. |
| Yismaw et al[90] | 2013 | 422 diabetic patients; n = 387 with asymptomatic UTI; n = 35 with symptomatic UTI | A total of 17.1% of symptomatic diabetic patients showed significant candiduria and 7.5% of asymptomatic diabetic patients |
| Falahati et al[91] | 2016 | 305 diabetic patients | A total of 12.5% of diabetic patients were positive for candiduria |
| Esmailzadeh et al[89] | 2018 | 400 diabetic patients | A total of 10% of diabetic patients showed Candida spp. in the urinary tract |
| Gharanfoli et al[92] | 2019 | 500 patients with UTI; n = 106 diabetics; n = 394 non-diabetics | A total of 21.1% of diabetic patients showed Candida sp. in urinary tract and 4.2% of UTI patients were positive for Candida spp. |
The problem is further aggravated with the use of relatively novel hypoglycemic agents that are known to induce glycosuria, and this specifically pertains to SGLT2 inhibitors. More specifically, the colonization rate with Candida spp. (and subsequently the risk of VVC) can increase substantially with the use of these agents, reaching up to 37%[4,5]. Another important issue is selecting the optimal treatment approach in females with recurrent VVC and diabetes, especially since many author groups recommend routine prophylactic administration of antimicrobial drugs in preventing candidiasis when faced with uncontrolled diabetes[6,21]. The best approach is still a matter of debate, as even a recent and comprehensive Cochrane review on different pharmacological and non-pharmacological treatment modalities highlighted that more research is necessary to ascertain the optimal medication choices as well as dose and frequency for females with diabetes[66].
The influence of diabetes on the development of balanitis/balanoposthitis caused by Candida spp. is well known due to the well-established association of uncontrolled blood glucose levels and the proliferation of Candida beneath the prepuce[67]. While Candida is a causative agent of less than 20% of all balanoposthitis cases, it is the most commonly observed pathogen in males with diabetes, habitually presenting as a pruritic rash with sores, erosions, or papules (with possible sub-preputial discharge)[68]. In addition, coinfection with other pathogens can worsen the clinical presentation in males with diabetes (not only with common sexually transmitted infections but also pathogens such as Streptococcus pyogenes[69]).
The aforementioned connection between diabetes and penile infection is reflected in population studies as well; for example, the appraisal of all male patients with balanoposthitis from the Longitudinal Health Insurance Database in Taiwan revealed that the incidence of type 2 diabetes mellitus was higher in the balanoposthitis cohort than those without it, with a hazard ratio of 2.55 after age and comorbidity adjustments[70]. Furthermore, a large study from Portugal demonstrated that diabetes mellitus was significantly more prevalent in patients with clinically frank balanitis when compared to the asymptomatic group, and there was also higher colonization with Candida species[71]. In addition, an extensive survey of dermatology specialists from across India, with more than 60000 outpatients in their care, showed that up to 75% of individuals with Candida balanoposthitis were known cases of diabetes mellitus[72].
Even novel hypoglycemic agents that can induce glycosuria, most notably already mentioned SGLT2 inhibitors, can also increase the risk of genital candidiasis in males (Figure 2). For example, a recent report by Bartolo et al[73] showed the development of balanitis due to C. albicans and subsequent candidemia but also the potential role of other species such as C. glabrata. A severe form of balanoposthitis caused by C. albicans after treatment with SGLT2 was also described in a 57-year-old with type 2 diabetes coupled with oral candidiasis[74]. Of note, balanitis is rarely seen in circumcised males, as the moist space beneath the foreskin represents an ideal environment for facilitated yeast proliferation[4].
The observed incidence of VVC during pregnancy is approximately 15%[75], but this percentage is even higher in pregnant females with either type 1/type 2 diabetes mellitus or gestational diabetes[76]. This means both pregnancy as a physiological process and diabetes as a pathological condition may have a compounding effect in the development of VVC (Figure 2). In a study on 251 pregnant females from Poland, Nowakowska et al[77] demonstrated a four times increased risk of developing vaginal mycosis in those with type 1 diabetes mellitus as well as a two times increased risk in those with gestational diabetes in comparison with healthy controls. A study on pregnant females from a Malaysian tertiary-care hospital showed that the first and second trimester of pregnancy and diabetes mellitus are significant risk factors for developing VVC[78]. A prospective study from China showed a significantly higher frequency of VVC in females with gestational diabetes (22.6% vs 9.7%)[76].
This is important due to the possible development of candida chorioamnionitis in diabetic pregnant females stemming from VVC, with potentially detrimental consequences for the unborn child. Although this clinical entity is relatively uncommon, it was repeatedly described in the medical literature. One of the gravest examples is a case reported by Obermair et al[79] on Candida chorioamnionitis that successively led to a late stillbirth in a pregnant woman with gestational diabetes mellitus. Unfortunately, there were no prior obstetrics procedures in this case, and infection with C. albicans triggered an inflammatory cascade that resulted in the occlusion of umbilical cord blood vessels, ultimately resulting in fetal death[79].
Recently, Shazniza Shaaya et al[80] reported 2 cases of Candida chorioamnionitis linked to gestational diabetes and originating from VVC where manifold red and yellowish spots were observed during pathohistological observation on the superficial area of the umbilical cord. Microscopically, these spots were microabscesses laden with yeasts and pseudohyphae, while peripheral funisitis was highlighted as a prominent feature of such Candida chorioamnionitis. Other reported cases of Candida chorioamnionitis associated with diabetes mellitus also led to adverse perinatal outcomes such as preterm birth, neonatal sepsis due to C. tropicalis, and the death of one twin as an unfortunate outcome of twin pregnancy[81-83]. The imputable role of diabetes mellitus in the development of Candida chorioamnionitis after VVC (with potentially serious sequelae for the fetus) cannot be overstated.
Urinary tract infections (UTI) are much more common in individuals with diabetes, and this is also valid for potential complications such as emphysematous cystitis, pyelonephritis, and kidney abscesses[84,85]. Furthermore, type 2 diabetes mellitus is a well-recognized risk factor for both community- and healthcare-associated acquired UTIs, but UTIs are linked to catheterization and following renal transplantation. In all of these scenarios, different Candida species have a prominent role[6,86]. In addition, in patients with diabetes, the duration of disease and poor glycoregulation in the long run lead to changes in the kidney’s microvasculature and frequent polyuria/glycosuria, which can predispose them to more frequent urinary tract infections[87].
Delineating candiduria from frank UTI is still a controversial topic, as there are no steadfast laboratory criteria. Furthermore, Candida is a recognized commensal of the urogenital tract. Therefore, its presence in the urine sample adds ambiguity to making a definitive diagnosis of Candida UTI[88]. A further issue is that candiduria by itself may be the sole indicator of invasive candidiasis, with potentially serious outcomes (particularly in immunocompromised patients)[88]. In any case, the prevalence of candiduria in individuals with type 2 diabetes mellitus ranges between 2.27% and 30.00% in studies conducted worldwide, with notably higher rates in females[89] (Table 3).
A study from Ethiopia found significant candiduria in 7.5% of asymptomatic and 17.1% of symptomatic patients presenting with diabetes, with C. albicans, C. glabrata, and C. tropicalis being the most commonly implicated species[90]. In one study by Falahati et al[91] from Iran, uncontrolled diabetes, increased fasting blood sugar levels, and glucose in urine were all significantly related with candiduria, with the most frequent species being C. glabrata and C. albicans in 50.0% and 31.6% of cases, respectively, followed by C. krusei, C. tropicalis, and C. kefyr. This was corroborated by another study from Iran, where the candiduria rate was also high in individuals with type 2 diabetes mellitus that presented with inadequate blood glucose control[89]. The most frequently isolated species in the latter study was C. albicans (47.5%), followed by C. glabrata (37.5%), C. kefyr (10.0%), and C. krusei (5.0%)[89]. A recent study from Iran on 1450 urine samples highlighted diabetes as the most frequent risk factor for the development of candiduria and the three most common species as C. albicans, C. glabrata, and C. tropicalis[92].
Emphysematous cystitis is a rare complication that is almost exclusively seen in diabetic patients, while fungal microorganisms are seldom implicated in its pathogenesis[6]. Still, uncontrolled diabetes is viewed as a major risk factor for an increasing role of Candida species (especially non-albicans species) in this specific pathology. Wang et al[93] described the case of a 53-year-old man with diabetes from China who presented with two rare and concomitant complications of C. tropicalis infection in the urinary tract: a discrete mass known as a fungus ball and emphysematous cystitis. Another study from the United States presented a case of a 49-year-old male with diabetes and emphysematous pyelitis caused by C. tropicalis, where early diagnosis and treatment led to a favorable outcome[94].
Antifungal therapy is often not justified, even in UTIs caused by different types of Candida[95]. The assumption is that people with predisposing factors (e.g., diabetes) should first be treated, which may in turn resolve the infection[96]. For individuals who have symptomatic UTIs caused by Candida spp. and when it is assumed that predisposing factors have been eliminated or at least kept to a minimum, the use of fluconazole is recommended due to the possibility of achieving high concentrations in urine. It can be administered orally, 200-400 mg daily, in a single dose for 14 d. Exceptions are infections caused by C. krusei and C. glabrata, where amphotericin B deoxycholate is often used (due to inadequate urine concentrations of other azole antifungals and echinocandins)[95]. In instances of resistant Candida spp. or in high-risk patients, amphotericin B is given intravenously at a dose of 0.3 to 0.6 mg/kg per day in the case of cystitis and given intravenously in a dose of 0.5 -0.7 mg/kg in the case of pyelonephritis[97]. In the case of resistant pyelonephritis, 25 mg/kg of flucytosine is added orally four times a day. The standard treatment regimen is 2 wk. The patient’s kidney function should be taken into account[98]. The use of flucytosine, although very effective in the eradication of Candida spp., requires extra caution due to the toxicity it possesses[98]. If used alone, resistance to it occurs very quickly, and therefore therapy is not carried out longer than 7-10 d. Also, the drug is administered every 6 h at a dose of 25 mg/kg[99]. It is important to note that the recurrences of infections caused by Candida spp. are very common[100].
In conclusion, there is an increasing body of evidence that shows how patients with diabetes (particularly those characterized by unsatisfactorily controlled glycemia) are vulnerable to urogenital mycotic infections with C. albicans and other non-albicans Candida species of increasing importance. We have highlighted virulence factors of C. albicans and shown how the interplay of many pathophysiological factors can give rise to VVC with increased risk of recurrent episodes and dire pregnancy outcomes. There is also an increased risk of candiduria and UTI development caused by species of Candida in females and males alike (with the possibility of further complications such as emphysematous cystitis) as well as balanitis and balanoposthitis in (primarily uncircumcised) males. With a steadily increasing global burden of diabetes, these clinical conditions will undoubtedly become more prevalent in the future. All of this underscores the importance of establishing and preserving euglycemia, alongside any introduced antifungal treatment approaches, if our end-goal is to successfully manage urogenital candidiasis in affected individuals with diabetes. Moreover, in order to minimize this high burden of yeast infections in individuals with diabetes, it is pivotal to identify those at high risk for developing type 2 diabetes mellitus and forestall the rise of complications; consequently, many lifestyle interventions (such as dietary changes, exercise, and weight reduction) have a much better impact than pharmacologic treatment. If the condition arises and the patient is faced with urogenital Candida infections, an early and appropriate treatment regimen should be introduced, especially to avoid several complicated conditions, which we have described.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Mycology
Country/Territory of origin: Croatia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Rwegerera GM, Botswana; Tu WJ, China S-Editor: Wu YXJ L-Editor: Filipodia P-Editor: Wu YXJ
| 1. | Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X, Song X, Ren Y, Shan PF. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep. 2020;10:14790. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 695] [Cited by in F6Publishing: 669] [Article Influence: 167.3] [Reference Citation Analysis (1)] |
| 2. | International Diabetes Federation. IDF Diabetes Atlas. 10th ed. Brussels; Belgium: 2021.. [Cited in This Article: ] |
| 3. | SAGE knowledge. Global Action Fund for Fungal Infections (GAFFI) Priority Fungal Infections [Internet].. [DOI] [Cited in This Article: ] |
| 4. | Nyirjesy P, Sobel JD. Genital mycotic infections in patients with diabetes. Postgrad Med. 2013;125:33-46. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 54] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 5. | Yokoyama H, Nagao A, Watanabe S, Honjo J. Incidence and risk of vaginal candidiasis associated with sodium-glucose cotransporter 2 inhibitors in real-world practice for women with type 2 diabetes. J Diabetes Investig. 2019;10:439-445. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | Rodrigues CF, Rodrigues ME, Henriques M. Candida sp. Infections in Patients with Diabetes Mellitus. J Clin Med. 2019;8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 92] [Cited by in F6Publishing: 98] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 7. | American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2012;35 Suppl 1:S64-S71. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1005] [Cited by in F6Publishing: 1083] [Article Influence: 90.3] [Reference Citation Analysis (0)] |
| 8. | Sinnott M, Kinsley BT, Jackson AD, Walsh C, O'Grady T, Nolan JJ, Gaffney P, Boran G, Kelleher C, Carr B. Fasting plasma glucose as initial screening for diabetes and prediabetes in irish adults: The Diabetes Mellitus and Vascular health initiative (DMVhi). PLoS One. 2015;10:e0122704. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Mathew TK, Tadi P. Blood Glucose Monitoring. Med Devices Syst [Internet] 2021.. [DOI] [Cited in This Article: ] |
| 10. | Toren E, Burnette KS, Banerjee RR, Hunter CS, Tse HM. Partners in Crime: Beta-Cells and Autoimmune Responses Complicit in Type 1 Diabetes Pathogenesis. Front Immunol. 2021;12:756548. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 26] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 11. | Galicia-Garcia U, Benito-Vicente A, Jebari S, Larrea-Sebal A, Siddiqi H, Uribe KB, Ostolaza H, Martín C. Pathophysiology of Type 2 Diabetes Mellitus. Int J Mol Sci. 2020;21. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 278] [Cited by in F6Publishing: 753] [Article Influence: 188.3] [Reference Citation Analysis (0)] |
| 12. | Moyce BL, Dolinsky VW. Maternal β-Cell Adaptations in Pregnancy and Placental Signalling: Implications for Gestational Diabetes. Int J Mol Sci. 2018;19. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 66] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 13. | Choudhury AA, Devi Rajeswari V. Gestational diabetes mellitus - A metabolic and reproductive disorder. Biomed Pharmacother. 2021;143:112183. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 71] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 14. | Reed J, Bain S, Kanamarlapudi V. A Review of Current Trends with Type 2 Diabetes Epidemiology, Aetiology, Pathogenesis, Treatments and Future Perspectives. Diabetes Metab Syndr Obes. 2021;14:3567-3602. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 142] [Cited by in F6Publishing: 102] [Article Influence: 34.0] [Reference Citation Analysis (0)] |
| 15. | Standl E, Khunti K, Hansen TB, Schnell O. The global epidemics of diabetes in the 21st century: Current situation and perspectives. Eur J Prev Cardiol. 2019;26:7-14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 81] [Cited by in F6Publishing: 126] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 16. | Berbudi A, Rahmadika N, Tjahjadi AI, Ruslami R. Type 2 Diabetes and its Impact on the Immune System. Curr Diabetes Rev. 2020;16:442-449. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 241] [Cited by in F6Publishing: 355] [Article Influence: 88.8] [Reference Citation Analysis (0)] |
| 17. | Giri B, Dey S, Das T, Sarkar M, Banerjee J, Dash SK. Chronic hyperglycemia mediated physiological alteration and metabolic distortion leads to organ dysfunction, infection, cancer progression and other pathophysiological consequences: An update on glucose toxicity. Biomed Pharmacother. 2018;107:306-328. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 167] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 18. | Daryabor G, Atashzar MR, Kabelitz D, Meri S, Kalantar K. The Effects of Type 2 Diabetes Mellitus on Organ Metabolism and the Immune System. Front Immunol. 2020;11:1582. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 181] [Article Influence: 45.3] [Reference Citation Analysis (0)] |
| 19. | Lao M, Li C, Li J, Chen D, Ding M, Gong Y. Opportunistic invasive fungal disease in patients with type 2 diabetes mellitus from Southern China: Clinical features and associated factors. J Diabetes Investig. 2020;11:731-744. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 20. | Lim S, Bae JH, Kwon HS, Nauck MA. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol. 2021;17:11-30. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 472] [Cited by in F6Publishing: 500] [Article Influence: 166.7] [Reference Citation Analysis (0)] |
| 21. | Mohammed L, Jha G, Malasevskaia I, Goud HK, Hassan A. The Interplay Between Sugar and Yeast Infections: Do Diabetics Have a Greater Predisposition to Develop Oral and Vulvovaginal Candidiasis? Cureus. 2021;13:e13407. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Pappas PG, Lionakis MS, Arendrup MC, Ostrosky-Zeichner L, Kullberg BJ. Invasive candidiasis. Nat Rev Dis Primers. 2018;4:18026. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 545] [Cited by in F6Publishing: 676] [Article Influence: 112.7] [Reference Citation Analysis (0)] |
| 23. | Zhang Z, Zhu R, Luan Z, Ma X. Risk of invasive candidiasis with prolonged duration of ICU stay: a systematic review and meta-analysis. BMJ Open. 2020;10:e036452. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 24. | Seyoum E, Bitew A, Mihret A. Distribution of Candida albicans and non-albicans Candida species isolated in different clinical samples and their in vitro antifungal suscetibity profile in Ethiopia. BMC Infect Dis. 2020;20:231. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 25. | Deorukhkar SC, Saini S, Mathew S. Non-albicans Candida Infection: An Emerging Threat. Interdiscip Perspect Infect Dis. 2014;2014:615958. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 98] [Cited by in F6Publishing: 112] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 26. | Singh DP, Kumar Verma R, Sarswat S, Saraswat S. Non-Candida albicans Candida species: virulence factors and species identification in India. Curr Med Mycol. 2021;7:8-13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 27. | Quindós G. Epidemiology of candidaemia and invasive candidiasis. A changing face. Rev Iberoam Micol. 2014;31:42-48. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 122] [Cited by in F6Publishing: 125] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 28. | Dias V. Candida species in the urinary tract: is it a fungal infection or not? Future Microbiol. 2020;15:81-83. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 29. | Sustr V, Foessleitner P, Kiss H, Farr A. Vulvovaginal Candidosis: Current Concepts, Challenges and Perspectives. J Fungi (Basel). 2020;6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 30. | Gunther LS, Martins HP, Gimenes F, Abreu AL, Consolaro ME, Svidzinski TI. Prevalence of Candida albicans and non-albicans isolates from vaginal secretions: comparative evaluation of colonization, vaginal candidiasis and recurrent vaginal candidiasis in diabetic and non-diabetic women. Sao Paulo Med J. 2014;132:116-120. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 31. | Ciurea CN, Kosovski IB, Mare AD, Toma F, Pintea-Simon IA, Man A. Candida and Candidiasis-Opportunism Versus Pathogenicity: A Review of the Virulence Traits. Microorganisms. 2020;8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 50] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 32. | Das S, Bhuyan R, Bagchi A, Saha T. Network analysis of hyphae forming proteins in Candida albicans identifies important proteins responsible for pathovirulence in the organism. Heliyon. 2019;5:e01916. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 33. | Grainha T, Jorge P, Alves D, Lopes SP, Pereira MO. Unraveling Pseudomonas aeruginosa and Candida albicans Communication in Coinfection Scenarios: Insights Through Network Analysis. Front Cell Infect Microbiol. 2020;10:550505. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 34. | Staniszewska M. Virulence Factors in Candida species. Curr Protein Pept Sci. 2020;21:313-323. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 50] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 35. | Martin H, Kavanagh K, Velasco-Torrijos T. Targeting adhesion in fungal pathogen Candida albicans. Future Med Chem. 2021;13:313-334. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 36. | Mukaremera L, Lee KK, Mora-Montes HM, Gow NAR. Candida albicans Yeast, Pseudohyphal, and Hyphal Morphogenesis Differentially Affects Immune Recognition. Front Immunol. 2017;8:629. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 87] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 37. | Tsang PW, Bandara HM, Fong WP. Purpurin suppresses Candida albicans biofilm formation and hyphal development. PLoS One. 2012;7:e50866. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 95] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 38. | Taylor BN, Staib P, Binder A, Biesemeier A, Sehnal M, Röllinghoff M, Morschhäuser J, Schröppel K. Profile of Candida albicans-secreted aspartic proteinase elicited during vaginal infection. Infect Immun. 2005;73:1828-1835. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 48] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 39. | Nikou SA, Kichik N, Brown R, Ponde NO, Ho J, Naglik JR, Richardson JP. Candida albicans Interactions with Mucosal Surfaces during Health and Disease. Pathogens. 2019;8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 40. | Willaert RG. Adhesins of Yeasts: Protein Structure and Interactions. J Fungi (Basel). 2018;4. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 41. | Pellon A, Begum N, Sadeghi Nasab SD, Harzandi A, Shoaie S, Moyes DL. Role of Cellular Metabolism during Candida-Host Interactions. Pathogens. 2022;11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 13] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 42. | Loh CY, Chai JY, Tang TF, Wong WF, Sethi G, Shanmugam MK, Chong PP, Looi CY. The E-Cadherin and N-Cadherin Switch in Epithelial-to-Mesenchymal Transition: Signaling, Therapeutic Implications, and Challenges. Cells. 2019;8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 361] [Cited by in F6Publishing: 637] [Article Influence: 127.4] [Reference Citation Analysis (0)] |
| 43. | Hoyer LL, Green CB, Oh SH, Zhao X. Discovering the secrets of the Candida albicans agglutinin-like sequence (ALS) gene family--a sticky pursuit. Med Mycol. 2008;46:1-15. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 249] [Cited by in F6Publishing: 236] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 44. | Talapko J, Juzbašić M, Matijević T, Pustijanac E, Bekić S, Kotris I, Škrlec I. Candida albicans-The Virulence Factors and Clinical Manifestations of Infection. J Fungi (Basel). 2021;7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 178] [Cited by in F6Publishing: 145] [Article Influence: 48.3] [Reference Citation Analysis (0)] |
| 45. | Pereira R, Dos Santos Fontenelle RO, de Brito EHS, de Morais SM. Biofilm of Candida albicans: formation, regulation and resistance. J Appl Microbiol. 2021;131:11-22. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 105] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 46. | Talapko J, Škrlec I. The Principles, Mechanisms, and Benefits of Unconventional Agents in the Treatment of Biofilm Infection. Pharmaceuticals (Basel). 2020;13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 47. | Tseng YK, Chen YC, Hou CJ, Deng FS, Liang SH, Hoo SY, Hsu CC, Ke CL, Lin CH. Evaluation of Biofilm Formation in Candida tropicalis Using a Silicone-Based Platform with Synthetic Urine Medium. Microorganisms. 2020;8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 48. | Mancera E, Nocedal I, Hammel S, Gulati M, Mitchell KF, Andes DR, Nobile CJ, Butler G, Johnson AD. Evolution of the complex transcription network controlling biofilm formation in Candida species. Elife. 2021;10. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 17] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 49. | Harpf V, Kenno S, Rambach G, Fleischer V, Parth N, Weichenberger CX, Garred P, Huber S, Lass-Flörl C, Speth C, Würzner R. Influence of Glucose on Candida albicans and the Relevance of the Complement FH-Binding Molecule Hgt1 in a Murine Model of Candidiasis. Antibiotics (Basel). 2022;11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 50. | Peng Z, Tang J. Intestinal Infection of Candida albicans: Preventing the Formation of Biofilm by C. albicans and Protecting the Intestinal Epithelial Barrier. Front Microbiol. 2021;12:783010. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 51. | Rumbaugh KP, Sauer K. Biofilm dispersion. Nat Rev Microbiol. 2020;18:571-586. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 434] [Cited by in F6Publishing: 326] [Article Influence: 81.5] [Reference Citation Analysis (0)] |
| 52. | Tulasidas S, Rao P, Bhat S, Manipura R. A study on biofilm production and antifungal drug resistance among Candida species from vulvovaginal and bloodstream infections. Infect Drug Resist. 2018;11:2443-2448. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 53. | König A, Hube B, Kasper L. The Dual Function of the Fungal Toxin Candidalysin during Candida albicans-Macrophage Interaction and Virulence. Toxins (Basel). 2020;12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 54. | Brown R, Priest E, Naglik JR, Richardson JP. Fungal Toxins and Host Immune Responses. Front Microbiol. 2021;12:643639. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 28] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 55. | Desai JV, Lionakis MS. The role of neutrophils in host defense against invasive fungal infections. Curr Clin Microbiol Rep. 2018;5:181-189. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 50] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 56. | Qiu S, Wu T, Wang P, Li J, Li Q, Du J. The Association between VEGFR Gene Polymorphisms and Stroke: A Meta-Analysis. PLoS One. 2016;11:e0151371. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 57. | El-Houssaini HH, Elnabawy OM, Nasser HA, Elkhatib WF. Influence of subinhibitory antifungal concentrations on extracellular hydrolases and biofilm production by Candida albicans recovered from Egyptian patients. BMC Infect Dis. 2019;19:54. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 58. | Schaller M, Borelli C, Korting HC, Hube B. Hydrolytic enzymes as virulence factors of Candida albicans. Mycoses. 2005;48:365-377. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 327] [Cited by in F6Publishing: 322] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 59. | Van Ende M, Wijnants S, Van Dijck P. Sugar Sensing and Signaling in Candida albicans and Candida glabrata. Front Microbiol. 2019;10:99. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 48] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 60. | d'Enfert C, Kaune AK, Alaban LR, Chakraborty S, Cole N, Delavy M, Kosmala D, Marsaux B, Fróis-Martins R, Morelli M, Rosati D, Valentine M, Xie Z, Emritloll Y, Warn PA, Bequet F, Bougnoux ME, Bornes S, Gresnigt MS, Hube B, Jacobsen ID, Legrand M, Leibundgut-Landmann S, Manichanh C, Munro CA, Netea MG, Queiroz K, Roget K, Thomas V, Thoral C, Van den Abbeele P, Walker AW, Brown AJP. The impact of the Fungus-Host-Microbiota interplay upon Candida albicans infections: current knowledge and new perspectives. FEMS Microbiol Rev. 2021;45. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 127] [Cited by in F6Publishing: 113] [Article Influence: 37.7] [Reference Citation Analysis (0)] |
| 61. | Mikamo H, Yamagishi Y, Sugiyama H, Sadakata H, Miyazaki S, Sano T, Tomita T. High glucose-mediated overexpression of ICAM-1 in human vaginal epithelial cells increases adhesion of Candida albicans. J Obstet Gynaecol. 2018;38:226-230. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 62. | Al Halteet S, Abdel-Hadi A, Hassan M, Awad M. Prevalence and Antifungal Susceptibility Profile of Clinically Relevant Candida Species in Postmenopausal Women with Diabetes. Biomed Res Int. 2020;2020:7042490. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 63. | Ray D, Goswami R, Banerjee U, Dadhwal V, Goswami D, Mandal P, Sreenivas V, Kochupillai N. Prevalence of Candida glabrata and its response to boric acid vaginal suppositories in comparison with oral fluconazole in patients with diabetes and vulvovaginal candidiasis. Diabetes Care. 2007;30:312-317. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 69] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 64. | Goswami R, Dadhwal V, Tejaswi S, Datta K, Paul A, Haricharan RN, Banerjee U, Kochupillai NP. Species-specific prevalence of vaginal candidiasis among patients with diabetes mellitus and its relation to their glycaemic status. J Infect. 2000;41:162-166. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 78] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 65. | Goswami D, Goswami R, Banerjee U, Dadhwal V, Miglani S, Lattif AA, Kochupillai N. Pattern of Candida species isolated from patients with diabetes mellitus and vulvovaginal candidiasis and their response to single dose oral fluconazole therapy. J Infect. 2006;52:111-117. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 66] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 66. | Cooke G, Watson C, Deckx L, Pirotta M, Smith J, van Driel ML. Treatment for recurrent vulvovaginal candidiasis (thrush). Cochrane Database Syst Rev. 2022;1:CD009151. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 67. | Cold CJ, Taylor JR. The prepuce. BJU Int. 1999;83 Suppl 1:34-44. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 116] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 68. | Kalra S, Chawla A. Diabetes and balanoposthitis. J Pak Med Assoc. 2016;66:1039-1041. [PubMed] [Cited in This Article: ] |
| 69. | Maatouk I, Hajjar MA, Moutran R. Candida albicans and Streptococcus pyogenes balanitis: diabetes or STI? Int J STD AIDS. 2015;26:755-756. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 70. | Lien CS, Lee SW, Chang CH, Chung CJ, Lin CL, Huang CP. Adult balanoposthitis patients have a higher risk of type 2 diabetes mellitus: A nationwide population-based cohort study. Urol Sci. 2017;. [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 71. | Lisboa C, Santos A, Dias C, Azevedo F, Pina-Vaz C, Rodrigues A. Candida balanitis: risk factors. J Eur Acad Dermatol Venereol. 2010;24:820-826. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 72. | Verma SB, Wollina U. Looking through the cracks of diabetic candidal balanoposthitis! Int J Gen Med. 2011;4:511-513. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 73. | Bartolo C, Hall V, Friedman ND, Lanyon C, Fuller A, Morrissey CO, Athan E. Bittersweet: infective complications of drug-induced glycosuria in patients with diabetes mellitus on SGLT2-inhibitors: two case reports. BMC Infect Dis. 2021;21:284. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 74. | Moldenhauer I, Pliquett RU, Kreft B, Sunderkötter C. Severe candidal balanoposthitis on concurrent treatment with secukinumab and the antidiabetic agent empagliflozin (sodium-glucose cotransporter 2 inhibitor - SGLT2-inhibitor). J Dtsch Dermatol Ges. 2019;17:456-458. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 75. | Roberts CL, Rickard K, Kotsiou G, Morris JM. Treatment of asymptomatic vaginal candidiasis in pregnancy to prevent preterm birth: an open-label pilot randomized controlled trial. BMC Pregnancy Childbirth. 2011;11:18. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 62] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 76. | Zhang X, Liao Q, Wang F, Li D. Association of gestational diabetes mellitus and abnormal vaginal flora with adverse pregnancy outcomes. Medicine (Baltimore). 2018;97:e11891. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 77. | Nowakowska D, Kurnatowska A, Stray-Pedersen B, Wilczynski J. Prevalence of fungi in the vagina, rectum and oral cavity in pregnant diabetic women: relation to gestational age and symptoms. Acta Obstet Gynecol Scand. 2004;83:251-256. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 78. | Masri SN, Noor SM, Nor LA, Osman M, Rahman MM. Candida isolates from pregnant women and their antifungal susceptibility in a Malaysian tertiary-care hospital. Pak J Med Sci. 2015;31:658-661. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 79. | Obermair HM, Bhagwanani G, Caldas R, Doyle H, Smoleniec J, Adno A. Candida chorioamnionitis associated with late stillbirth: A case report. Case Rep Womens Health. 2020;27:e00239. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 80. | Shazniza Shaaya E, Halim SAA, Leong KW, Ku KBP, Lim PS, Tan GC, Wong YP. Candida Chorioamnionitis in Mothers with Gestational Diabetes Mellitus: A Report of Two Cases. Int J Environ Res Public Health. 2021;18. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 81. | Friebe-Hoffmann U, Bender DP, Sims CJ, Rauk PN. Candida albicans chorioamnionitis associated with preterm labor and sudden intrauterine demise of one twin. A case report. J Reprod Med. 2000;45:354-356. [PubMed] [Cited in This Article: ] |
| 82. | Canpolat FE, Çekmez F, Tezer H. Chorioamnionitis and neonatal sepsis due to Candida tropicalis. Arch Gynecol Obstet. 2011;283:919-920. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 83. | Maki Y, Fujisaki M, Sato Y, Sameshima H. Candida Chorioamnionitis Leads to Preterm Birth and Adverse Fetal-Neonatal Outcome. Infect Dis Obstet Gynecol. 2017;2017:9060138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 84. | Kofteridis DP, Papadimitraki E, Mantadakis E, Maraki S, Papadakis JA, Tzifa G, Samonis G. Effect of diabetes mellitus on the clinical and microbiological features of hospitalized elderly patients with acute pyelonephritis. J Am Geriatr Soc. 2009;57:2125-2128. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 85. | Mnif MF, Kamoun M, Kacem FH, Bouaziz Z, Charfi N, Mnif F, Naceur BB, Rekik N, Abid M. Complicated urinary tract infections associated with diabetes mellitus: Pathogenesis, diagnosis and management. Indian J Endocrinol Metab. 2013;17:442-445. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 86. | Nitzan O, Elias M, Chazan B, Saliba W. Urinary tract infections in patients with type 2 diabetes mellitus: review of prevalence, diagnosis, and management. Diabetes Metab Syndr Obes. 2015;8:129-136. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 105] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 87. | Burekovic A, Haskovic E, Ceric F, Halilovic D. Correlation Between Inflammatory and Biochemical Parameters in Patients with Diabetes and Urinary Tract Infection. Mater Sociomed. 2021;33:240-243. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 88. | Alfouzan WA, Dhar R. Candiduria: Evidence-based approach to management, are we there yet? J Mycol Med. 2017;27:293-302. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 89. | Esmailzadeh A, Zarrinfar H, Fata A, Sen T. High prevalence of candiduria due to non-albicans Candida species among diabetic patients: A matter of concern? J Clin Lab Anal. 2018;32:e22343. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 90. | Yismaw G, Asrat D, Woldeamanuel Y, Unakal C. Prevalence of candiduria in diabetic patients attending Gondar University Hospital, Gondar, Ethiopia. Iran J Kidney Dis. 2013;7:102-107. [PubMed] [Cited in This Article: ] |
| 91. | Falahati M, Farahyar S, Akhlaghi L, Mahmoudi S, Sabzian K, Yarahmadi M, Aslani R. Characterization and identification of candiduria due to Candida species in diabetic patients. Curr Med Mycol. 2016;2:10-14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 92. | Gharanfoli A, Mahmoudi E, Torabizadeh R, Katiraee F, Faraji S. Isolation, characterization, and molecular identification of Candida species from urinary tract infections. Curr Med Mycol. 2019;5:33-36. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 2.2] [Reference Citation Analysis (1)] |
| 93. | Wang L, Ji X, Sun GF, Qin YC, Gong MZ, Zhang JX, Li NC, Na YQ. Fungus ball and emphysematous cystitis secondary to Candida tropicalis: A case report. Can Urol Assoc J. 2015;9:E683-E686. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 94. | Alansari A, Borras MD, Boma N. "I have chicken fat in my urine! Med Mycol Case Rep. 2015;10:27-28. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 95. | Odabasi Z, Mert A. Candida urinary tract infections in adults. World J Urol. 2020;38:2699-2707. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 96. | Muskett H, Shahin J, Eyres G, Harvey S, Rowan K, Harrison D. Risk factors for invasive fungal disease in critically ill adult patients: a systematic review. Crit Care. 2011;15:R287. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 94] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 97. | Ross J, Hickling D. Medical Treatment for Urinary Tract Infections. Urol Clin North Am. 2022;49:283-297. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 98. | Bellmann R, Smuszkiewicz P. Pharmacokinetics of antifungal drugs: practical implications for optimized treatment of patients. Infection. 2017;45:737-779. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 153] [Cited by in F6Publishing: 194] [Article Influence: 27.7] [Reference Citation Analysis (0)] |
| 99. | Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner L, Reboli AC, Schuster MG, Vazquez JA, Walsh TJ, Zaoutis TE, Sobel JD. Executive Summary: Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62:409-417. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1076] [Cited by in F6Publishing: 1001] [Article Influence: 125.1] [Reference Citation Analysis (0)] |
| 100. | Lai MY, Hsu JF, Chu SM, Wu IH, Huang HR, Chiang MC, Fu RH, Tsai MH. Risk Factors and Outcomes of Recurrent Candidemia in Children: Relapse or Re-Infection? J Clin Med. 2019;8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |