Abstract
Clinical scenario
At a routine medical examination a 44 year-old bricklayer who has smoked 20 cigarettes a day since his mid-teens admits that recently he has been more breathless than usual on heavy work. After an episode of bronchitis last winter he attended for spirometry which confirmed moderate COPD with an FEV1/FVC ratio of 0.65 and a post-bronchodilator FEV1 of 78% predicted. He was offered smoking cessation advice but did not attend the follow-up appointments offered. He is on no medication.
Similar content being viewed by others
Assessment
My initial priority would be engaging this patient in further assessment and management of his COPD. He is presenting for a routine medical, but it is likely he is worried about his health; like many male patients he may be inclined to hide from health care and be reluctant to return for further visits. It is vital that the general practitioner (GP) be patient-centred,1 communicate that he or she is there to work with the patient, and acknowledge that change, particularly smoking cessation, can be challenging.
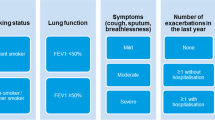
Assessment involves history, examination and investigations. In the history I would ask about respiratory symptoms such as cough (including sputum production), dyspnoea, wheeze and frequency of chest infections. It is also important to ask about possible cardiac symptoms such as chest pain and features that may suggest malignancy such as weight loss. The GOLD guidelines now encourage systematic assessment of the impact of the disease and risk of future events.2 The former is assessed with tools (modified Medical Research Council Dyspnoea Scale and COPD Assessment Tool (CAT)) and the latter by exacerbation history and degree of airflow limitation. Incorporating questionnaires, even brief ones, is challenging given time pressures and the fact that these instruments are not yet incorporated into GP clinical software, so I am yet to start using this approach in my practice.
The smoking history is vitally important. As well as discussing quantity and duration of tobacco use, I would explore the stage of change by asking a non-judgmental question such as, “How do you feel about your smoking at the moment?”.3 I would assess nicotine dependence by asking about time to first cigarette and number of cigarettes per day.4 Although tobacco smoking is the likely cause of his COPD it is important to ask also about occupational dust exposure. His level of family support and whether he lives with a smoker is important. I would ask about his mood and level of interest, as depression is another common co-morbidity.
Alpha-1 antitrypsin deficiency
A family history of respiratory disease could suggest alpha-1 antitrypsin deficiency. This is a genetic disorder most common in northern Europeans and those of Iberian descent where there is an abnormality of production of the protease inhibitor alpha-1 antitrypsin. The degree of deficiency and clinical symptoms vary, but those affected can develop COPD before the age of 40, as proteases damage the alveoli, especially if they are also smokers. Liver disease is another feature of the condition.
Examination
Physical examination is likely to be normal but I would check his body mass index (BMI) and look for general features of chronic lung disease as well as specific respiratory examination. It is also important to examine the cardiovascular system and look for evidence of muscle wasting. Spirometry (pre- and post-bronchodilator) needs to be repeated to see if there is evidence of disease progression since the last visit. Given the young age of onset of COPD in this patient, measuring the serum alpha-1 antitrypsin and liver function is indicated. One of the most common co-morbidities in people with COPD is cardiovascular disease and this patient needs cardiovascular risk assessment and testing for diabetes. An electrocardiogram is often part of a routine medical and can help exclude left ventricular hypertrophy and previous infarction. Chest X-ray has value in excluding other pathology and in revealing lower lobe emphysematous changes which may indicate alpha-1 antitrypsin deficiency.
Smoking cessation support
Smoking cessation support is the key intervention as it is the most effective measure to reduce progression of the disease.6 There is evidence that the effect may be greater in patients with mild and moderate disease than in patients with severe disease.7 Motivational interviewing can help the patient progress towards a quit attempt.8 Smokers who are told their “lung age” may be more likely to quit, so I would consider using this as a tool to enhance motivation.9 If he is willing to try to quit then I would offer professional support and follow-up and encourage him to use smoking cessation pharmacotherapy. The choice of medication is based on clinical suitability and patient preference.4
He should be encouraged to exercise regularly, and referral to pulmonary rehabilitation will be indicated if his condition deteriorates.10 Pharmacotherapy for COPD will improve lung function and reduce symptoms but will not prevent long term decline in FEV1. Options are short-acting bronchodilators on an ‘as required’ basis, or (if this does not control symptoms) regular long-acting antimuscarinics or long-acting β2-agonists.2 It is important to educate about device technique and review this together with adherence at follow-up visits. Annual influenza vaccination is important. Pneumococcal vaccination — given as one dose followed by a single booster dose five years later — is also indicated, though there is less evidence of benefit.
Education is important to help him understand and come to terms with the diagnosis. Although currently his risk of exacerbations is low, he should be advised on what to do if his symptoms increase. Specialist referral in my view is not needed unless he has alpha-1 antitrypsin deficiency. Management in the context of alpha-1 antitrypsin deficiency follows the same principles but may also include replacement of the protein. Engaging him in regular follow-up (for example six-monthly) is very important, and use of a disease register with recall and reminder can help facilitate this.
References
Stewart M, Belle Brown J, Weston WW, McWhinney IR, McWilliam CL, Freeman TR . Patient centered medicine: transforming the clinical method. Radcliff Medical Press: Oxford, 2003.
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of COPD. Updated December 2011 Available from: http://www.goldcopd.org/. (Accessed August 2012)
Richmond RL, Austin A, Webster IW . Three year evaluation of a programme by general practitioners to help patients to stop smoking. BMJ 1986;292:803. http://dx.doi.org/10.1136/bmj.292.6523.803
Zwar N, Richmond R, Borland R, et al. Supporting smoking cessation: a guide for health professionals. The Royal Australian College of General Practitioners: Melbourne, 2011
Gruffydd-Jones K . GOLD guidelines 2011: what are the implications for primary care? Prim Care Respir J 2012;21(4):437–41. http://dx.doi.org/10.4104/pcrj.2012.00058
Anthonisen NR, Connett JE, Kiley JP, et al. Effects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEV1. The Lung Health Study. JAMA 1994;272:1497–1505. http://dx.doi.org/10.1001/jama.1994.03520190043033
Kanner RE, Connett JE, Williams DE, Buist AS . Effects of randomized assignment to a smoking cessation intervention and changes in smoking habits on respiratory symptoms in smokers with early chronic obstructive pulmonary disease: the Lung Health Study. Am J Med 1999;106:410–16. http://dx.doi.org/10.1016/S0002-9343(99)00056-X
van Schayck CPO, Pinnock H, Østrem A, et al. IPCRG Consensus statement: Tackling the smoking epidemic — practical guidance for primary care. Prim Care Respir J 2008;17:185–93. http://dx.doi.org/10.3132/pcrj.2008.00060
Parkes G, Greenhalgh T, Griffin M, Dent R . Effect on smoking quit rate of telling patients their lung age: the Step2quit randomised controlled trial. BMJ 2008;336: 598–600. http://dx.doi.org/10.1136/bmj.39503.582396.25
Maltais F, Bourbeau J, Shapiro S, et al. Effects of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med 2008;149:869–78.
Acknowledgements
Handling editor Hilary Pinnock
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
NZ has provided expert advice on smoking cessation education programmes to Pfizer Pty Ltd and GlaxoSmithKline Australia and has received support to attend smoking cessation conferences.
Rights and permissions
About this article
Cite this article
Zwar, N. How I would manage a man with COPD who has few symptoms and is at low risk of an exacerbation: a primary care perspective from Australia. Prim Care Respir J 21, 442–443 (2012). https://doi.org/10.4104/pcrj.2012.00097
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.4104/pcrj.2012.00097