Abstract
Background
Arthroscopic cuff repair is a highly successful technique, but postoperative rehabilitation is complex and the rate of tear recurrence is not negligible. Biological augmentations have been proposed to overcome these drawbacks. The platelet-rich plasma (PRP) is a platelet-rich blood fraction that is applied on the repair site to enhance tendon healing. This study evaluates the effectiveness of PRP application in arthroscopic cuff repair.
Materials and Methods
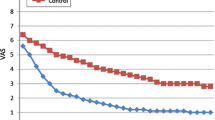
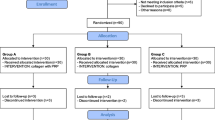
A prospective nonrandomized study was carried out on 22 patients undergoing arthroscopic rotator cuff repair. Only patients with isolated and repairable supraspinatus tears were included and divided into two groups: 11 patients (Group A) received intraoperative PRP and 11 patients (Group B) did not. All patients had the same rehabilitation and followup protocol. Clinical–functional parameters (visual analog score, active range of motion, University of California at Los Angeles - UCLA, Constant) were recorded at predefined intervals, and magnetic resonance imaging (MRI) was performed 1 year postoperative.
Results
Only one patient of Group B did not complete the study protocol. No intraoperative or postoperative complications were observed. No differences were found in the clinical–functional parameters during the entire study. At 1 year, MRI showed 1 retear in Group A and 2 retears in Group B, but the difference was not significant.
Conclusions
The role of PRP as an adjuvant for surgical repair of rotator cuff tears is controversial. In this study, we could not demonstrate significant advantages of PRP for arthroscopic repair of isolated supraspinatus tears. The potential improvement in the structural outcome should be evaluated in the long term to justify the additional costs related to PRP application.
Similar content being viewed by others

References
Gumina S, Carbone S, Campagna V, Candela V, Sacchetti FM, Giannicola G, et al. The impact of aging on rotator cuff tear size. Musculoskelet Surg 2013;97 Suppl 1:69–72.
Walch G, Noel E, Boulahia A. Rotator cuff tears: Epidemiology, differentiation, clinical presentation and natural history. Rheum Eur 1999;28:129–33.
Burkhart SS. A stepwise approach to arthroscopic rotator cuff repair based on biomechanical principles. Arthroscopy 2000;16:82–90.
Yadav H, Nho S, Romeo A, MacGillivray JD. Rotator cuff tears: Pathology and repair. Knee Surg Sports Traumatol Arthrosc 2009;17:409–21.
Alsousou J, Thompson M, Hulley P, Noble A, Willett K. The biology of platelet-rich plasma and its application in trauma and orthopaedic surgery: A review of the literature. J Bone Joint Surg Br 2009;91:987–96.
Dohan Ehrenfest DM, Rasmusson L, Albrektsson T. Classification of platelet concentrates: From pure platelet-rich plasma (P-PRP) to leucocyte- and platelet-rich fibrin (L-PRF). Trends Biotechnol 2009;27:158–67.
Barber FA, Hrnack SA, Snyder SJ, Hapa O. Rotator cuff repair healing Influenced by platelet-rich plasma construct augmentation. Arthroscopy 2011;27:1029–35.
Rodeo SA, Delos D, Williams RJ, Adler RS, Pearle A, Warren RF, et al. The effect of platelet-rich fibrin matrix on rotator cuff tendon healing: A prospective, randomized clinical study. Am J Sports Med 2012;40:1234–41.
Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res 1990;254:81–6.
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 1994;304:78–83.
Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: Assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg 1999;8:599–605.
Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 1987;214:160–4.
Romeo AA, Mazzocca A, Hang DW, Shott S, Bach BR Jr. Shoulder scoring scales for the evaluation of rotator cuff repair. Clin Orthop Relat Res 2004;427:107–14.
Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am 2007;89:953–60.
Randelli P, Randelli F, Ragone V, Menon A, D’Ambrosi R, Cucchi D, et al. Regenerative medicine in rotator cuff injuries. Biomed Res Int 2014;2014:129515.
Chahal J, Van Thiel GS, Mall N, Heard W, Bach BR, Cole BJ, et al. The role of platelet-rich plasma in arthroscopic rotator cuff repair: A systematic review with quantitative synthesis. Arthroscopy 2012;28:1718–27.
Le BT, Wu XL, Lam PH, Murrell GA. Factors predicting rotator cuff retears: An analysis of 1000 consecutive rotator cuff repairs. Am J Sports Med 2014;42:1134–42.
Eppley BL, Woodell JE, Higgins J. Platelet quantification and growth factor analysis from platelet-rich plasma: Implications for wound healing. Plast Reconstr Surg 2004;114:1502–8.
Riboh JC, Saltzman BM, Yanke AB, Fortier L, Cole BJ. Effect of leukocyte concentration on the efficacy of platelet-rich plasma in the treatment of knee osteoarthritis. Am J Sports Med 2016;44:792–800.
Zumstein MA, Berger S, Schober M, Boileau P, Nyffeler RW, Horn M, et al. Leukocyte- and platelet-rich fibrin (L-PRF) for long term delivery of growth factor in rotator cuff repair: Review, preliminary results and future directions. Curr Pharm Biotechnol 2012;13:1196–206.
Vavken P, Sadoghi P, Palmer M, Rosso C, Mueller AM, Szoelloesy G, et al. Platelet-rich plasma reduces retear rates after arthroscopic repair of small- and medium-sized rotator cuff tears but is not cost-effective. Am J Sports Med 2015;43:3071–6.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Martinelli, D., Fornara, P., Stecco, A. et al. Does Intraoperative Platelet-rich Plasma Improve Clinical and Structural Outcomes after Arthroscopic Repair of Isolated Tears of the Supraspinatus Tendon?. JOIO 53, 77–81 (2019). https://doi.org/10.4103/ortho.IJOrtho_35_17
Published:
Issue Date:
DOI: https://doi.org/10.4103/ortho.IJOrtho_35_17