Published online Feb 7, 2015. doi: 10.3748/wjg.v21.i5.1573
Peer-review started: July 9, 2014
First decision: August 6, 2014
Revised: August 27, 2014
Accepted: October 15, 2014
Article in press: October 15, 2014
Published online: February 7, 2015
AIM: To evaluate the effect of computed tomography (CT) attenuation values of ascites on gastrointestinal (GI) perforation site prediction.
METHODS: The CT attenuation values of the ascites from 51 patients with GI perforations were measured by volume rendering to calculate the mean values. The effect of the CT attenuation values of the ascites on perforation site prediction and postoperative complications was evaluated.
RESULTS: Of 24 patients with colorectal perforations, the CT attenuation values of ascites were significantly higher than those in patients with perforations at other sites [22.5 Hounsfield units (HU) vs 16.5 HU, respectively, P = 0.006]. Colorectal perforation was significantly associated with postoperative complications (P = 0.038). The prediction rate of colorectal perforation using attenuation values as an auxiliary diagnosis improved by 9.8% compared to that of CT findings alone (92.2% vs 82.4%).
CONCLUSION: The CT attenuation values of ascites could facilitate the prediction of perforation sites and postoperative complications in GI perforations, particularly in cases in which the perforation sites are difficult to predict by CT findings alone.
Core tip: In gastrointestinal (GI) perforations, the prediction of perforation sites is important for surgeons in planning for intensive perioperative care of fatally ill patients. Although multi-detector row computed tomography (CT) continues to gain further acceptance as a diagnostic tool, more precise identification of the perforation site is required in clinical practice. We show that the CT attenuation values of ascites in patients with GI perforations could simply and objectively predict perforation sites and are useful in predicting postoperative complications, particularly in cases in which perforation sites are difficult to predict by CT findings alone.
- Citation: Seishima R, Okabayashi K, Hasegawa H, Tsuruta M, Hoshino H, Yamada T, Kitagawa Y. Computed tomography attenuation values of ascites are helpful to predict perforation site. World J Gastroenterol 2015; 21(5): 1573-1579
- URL: https://www.wjgnet.com/1007-9327/full/v21/i5/1573.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i5.1573
A delay in acute abdomen diagnoses is reported to markedly influence morbidity and mortality and is associated with a lengthened hospital stay[1,2]. Computed tomography (CT) has gained acceptance as a fast and accurate diagnostic method for acute abdomen cases and has become a vital imaging technique in emergency departments, which increases the level of diagnostic certainty. A randomized controlled clinical trial conducted in the United Kingdom reported that early CT (within 24 h of presentation) reduced serious diagnostic errors by 17% and decreased the hospital stay and mortality rate[2].
Gastrointestinal (GI) perforation is one of the most life-threatening conditions in acute abdomen cases. Despite recent advances in imaging techniques, surgical treatment, and intensive medical care, peritonitis caused by GI perforation is associated with various complications[3] and is linked with a mortality rate of 5%-30%[4-8]. Among various GI perforation sites, colorectal perforation has the highest complication rate and approaches 55%[9]. To prevent postoperative complications, the prediction of perforation sites is important for surgeons in planning intensive perioperative care of fatally ill patients.
The use of multi-detector row CT (MDCT) has led to improvements in the diagnosis of GI perforation and the prediction of perforation sites. Retrospective studies have reported that the sensitivity of MDCT for perforation site prediction is approximately 80%-85%[10-12], whereas that of conventional CT is 36%[13]. A previous prospective study reported that the concentration of extraluminal air bubbles, segmental bowel wall thickening, and focal defects of the bowel wall were the three most significant specific signs for predicting perforation sites using CT[14]; however, these signs might be subtle or only indirectly related to the site or etiology of perforation, and some patients exhibit none of these signs. In an emergent situation, the precise identification of the perforation site is important for surgeons for appropriate and immediate patient management[15]. Although the use of laparoscopic surgery has been increasing, even for colorectal perforations, it is limited to elective cases[16,17]. Open surgery is required for patients with colorectal perforations. Although MDCT continues to gain further acceptance as a diagnostic tool, a simplified and objective method to increase its reliability in clinical practice is required.
CT images of a GI perforation are characterized by free intraperitoneal gas, ascites and abscesses in the peritoneal cavity[14,18]. Ascites relevant to GI perforation might contain GI contents as well as exudates or blood that might influence CT attenuation values. We hypothesized that CT attenuation values most likely reflect the degree of ascites contamination, which could help to predict GI perforation sites. To verify this hypothesis, we compared the CT attenuation values of ascites in patients with GI perforation sites. The objectives of this study were to assess the sensitivity and specificity of CT attenuation values to predict GI perforation sites and evaluate their usefulness in clinical practice.
A total of 61 consecutive GI perforation patients with detectable ascites by abdominal CT on admission underwent surgery at Keio University Hospital (Tokyo, Japan) between 2006 and 2012. The data were obtained from our surgical database. All the patients were intraoperatively diagnosed with GI perforations. To exclude the influence of bowel preparation, 10 patients with iatrogenic perforations were excluded from this analysis including seven with anastomotic leakage after GI surgery, two with intraoperative injuries, and one with a perforation after an endoscopic submucosal dissection, whereas those with perforations resulting from chemotherapy or radiotherapy were included. A total of 51 patients were included in our analyses. The patient data were obtained from a prospectively maintained registry of surgery records and reviewed retrospectively. For our analysis, the patients were divided into the following two groups: a colorectal perforation group and a group with perforations at other sites, including the upper GI and small intestine. The postoperative complications were categorized as systematic (including pneumonia, pulmonary embolism, and deep vein thrombosis) or surgical site infections (SSIs). The study protocol was approved by the institutional ethics committee of Keio University Hospital.
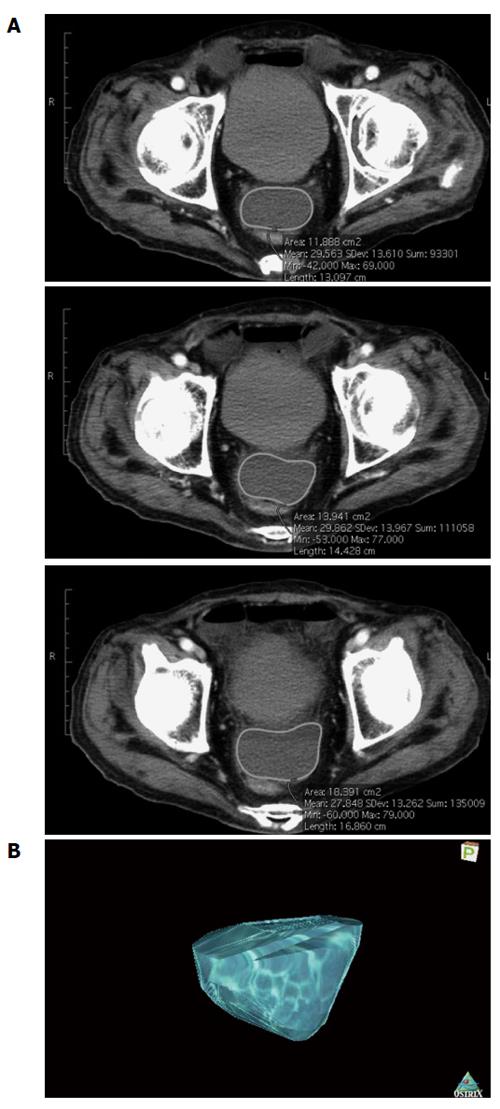
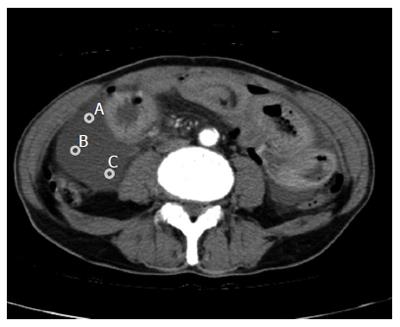
All the CT scans were performed using a BrightSpeed scanner (General Electric Medical Systems, Milwaukee, WI, United States) with 5-mm slices. Each enhanced CT was performed with an intravenous injection of iohexol (Omnipaque; Daiichi-Sankyo Co., Tokyo, Japan) as the contrast agent at a dose of 300 mgI/kg and scanned at the late phase. No oral contrast agent was used. The ascites sites revealed by CT were categorized into the following five sites: perihepatic, perisplenic, paracolic gutters, pelvis, or Douglas pouch. The ascitic fluid volume at each site was quantified by three-dimensional (3D)-CT volumetry (a volume rendering method) using OsiriX computational open source Digital Imaging and Communication in Medicine imaging software (v.3.7.1; OsiriX Foundation, Geneva, Switzerland) (Figure 1). The average CT attenuation values were calculated from the 3D constructions of where the greatest fluid accumulations were found. All the measured ascites fluid volumes were at least 5 cm3. All the measurements were performed in a similar manner, using a single CT slice image (2D method). Of the slices showing the greatest fluid accumulation, a region of interest of approximately 5 mm2 was selected, and three arbitrary points of the ascites were measured (Figure 2). The average of the three points was calculated. All the measurements were made retrospectively and independently by two investigators who were blinded to patient complaints, specific medical histories, physical examination findings, surgery data, laboratory evaluations, and imaging results. The data are presented as the average measurements of two investigators and expressed as Hounsfield units. The patients with any of the three specific findings of perforation site prediction by CT (concentration of extraluminal air bubbles, segmental bowel wall thickening, and focal defect of the bowel wall) were defined as predicted cases.
The median values with interquartile ranges (IQR) are presented for the continuous variables. The comparisons between the two groups were made using the Mann-Whitney U test or Fisher’s exact test. Univariate and multivariate linear regression analyses were used to evaluate the influence of the covariates on the measurement of the CT attenuation values of the ascites. Logistic regression analysis was used to evaluate the risk factors of postoperative complications. The covariates with a P value of ≤ 0.10 in the univariate analysis were included in the multivariate analysis. The interclass correlation coefficient was calculated to evaluate the reliability of the data obtained from different measuring methods or investigators. The ability of the CT attenuation values to predict colorectal perforation or perforations of other sites was assessed using receiver operating characteristic (ROC) curves, and the cut-off point was determined using the ROC curve closest to (0, 1) to the point at which the sensitivity and specificity were maximized. All the statistical tests were two-sided, and the significance level was set at 0.05. All the statistical analyses were performed using SPSS version 21 statistical software (IBM Japan, Tokyo, Japan).
Of the 51 patients, 24 (47.1%) had colorectal perforations and 27 (52.9%) had perforations at other sites (17 in the small intestine and 10 in the upper GI tract). The patient characteristics are presented in Table 1. The patients with colorectal perforations were significantly older (P = 0.015) and had a smaller amount of ascites (P = 0.018) than those with perforations at other sites. The patients with colorectal perforations had significantly higher CT attenuation values using volume rendering [colorectal vs other sites, 22.5 Hounsfield unit (HU) (IQR = 15.9) vs 16.5 HU (IQR = 9.8), respectively, P = 0.006].
| Colorectum(n = 24) | Other sites(n = 27) | P value | |
| Age (yr) | 70 (44-91)1 | 61 (24-84)1 | 0.0152 |
| Gender (male) | 14 (58.3) | 15 (55.6) | 1.0003 |
| Reason of perforation | 0.8803 | ||
| Malignancy | 5 (20.8) | 6 (22.2) | |
| Benign | 14 (58.3) | 16 (59.3) | |
| Chemo and/or radiotherapy | 2 (8.3) | 3 (11.1) | |
| Idiopathic | 3 (12.5) | 2 (7.4) | |
| Ascites accumulated site | 0.5943 | ||
| Douglas’s pouch | 12 (50.0) | 13 (48.1) | |
| Perihepatic | 7 (29.2) | 10 (37.0) | |
| Paracolic gutter | 5 (20.8) | 3 (11.1) | |
| Intrapelvic | 0 | 1 (3.7) | |
| Amount of ascites (cm3) | 17.3 | 55.4 | 0.0182 |
| (5.1-736.3)1 | (9.3-494.1)1 | ||
| Intravenous contrast (no) | 5 (23.8) | 4 (15.4) | 0.4863 |
| Time from onset (hours) | 25.5 (6-144)1 | 17.7 (4-192)1 | 0.3402 |
| CT attenuation values of ascites | 22.5 | 16.5 | 0.0062 |
| (11.2-66.9) | (2.5-63.1) |
The univariate and multivariate analysis results of the factors influencing the CT attenuation values of ascites are shown in Table 2. The univariate analysis showed that the perforation site (coefficient = 8.86, 95%CI: 1.49-16.24; P = 0.020) was significantly associated with the CT attenuation values. Additionally, the multivariate analysis showed that the perforation site (coefficient = 7.39, 95%CI: 1.60-13.19; P = 0.014) was identified as a significant independent factor that influenced the CT attenuation values of ascites.
| Univariate | Multivariate | |||
| Coefficient (95%CI) | P value | Coefficient (95%CI) | P value | |
| Perforation site | 8.86 (1.49-16.24) | 0.020 | 7.39 (1.60-13.19) | 0.014 |
| Amount of ascites | -0.09 (-0.04-0.02) | 0.513 | ||
| Reason of perforation | 1.57 (-4.64-7.77) | 0.614 | ||
| Ascites accumulated site | 1.48 (-2.01-4.97) | 0.397 | ||
| Intravenous contrast | 5.10 (-4.61-14.80) | 0.296 | ||
| Time from onset | -0.03 (-0.14-0.09) | 0.656 | ||
Further analysis was performed to clarify the association between postoperative complications and the CT attenuation values of ascites. The logistic regression analysis results are shown in Table 3. An analysis of postoperative complications demonstrated that the perforation site (coefficient = 3.40, 95%CI: 1.07-10.78; P = 0.038) and age (coefficient = 1.04, 95%CI: 1.01-1.08; P = 0.026) were significant risk factors for postoperative complications. The influences of the CT attenuation values of ascites on SSIs and systemic infections were separately evaluated using logistic regression analysis. Colorectal perforation was significantly associated with SSIs (coefficient = 2.52, 95%CI: 1.06-5.98; P = 0.036) and not systemic complications (coefficient = 2.10, 95%CI: 0.62-7.17; P = 0.236).
| Coefficient (95%CI) | P value | |
| Age | 1.04 (1.01-1.08) | 0.026 |
| Reason of perforation | 1.50 (0.61-3.67) | 0.374 |
| Perforation site | 3.40 (1.07-10.78) | 0.038 |
| CT attenuation values of ascites | 1.03 (0.98-1.07) | 0.247 |
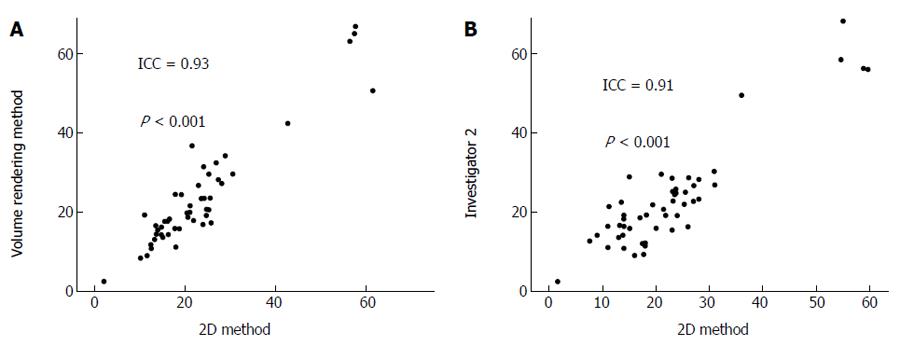
These results suggested that the volume rendering system was useful for predicting perforation sites; however, it might be too complicated to perform on an emergency basis. Therefore, we evaluated whether measurements of the CT attenuation values of ascites using one-slice CT images (2D method) provided similar results. As shown in Figure 3A, there was a significant correlation between the CT attenuation values of ascites gained by volume rendering and the 2D method (ICC = 0.93, P < 0.001). To further clarify the efficacy of the 2D method, two investigators independently assessed the reproducibility of the CT attenuation values measured by the 2D method. As demonstrated in Figure 3B, there was a significant correlation in the CT attenuation values measured between the two investigators (ICC = 0.91, P < 0.001), suggesting that the CT attenuation values measured by the 2D method were reproducible regardless of the investigator. From the data obtained by the 2D method, an ROC curve was drawn. The area under the curve was calculated as 0.82, which indicated strong abilities to predict perforation sites. A cut-off value of a perforation site was estimated at 18 HU. Using this cut-off value, the sensitivity of colorectal perforation prediction was 87.5% (21/24), whereas the specificity was 70.4% (19/27).
The site prediction rate of conventional perforation site prediction using CT findings was 82.4% (42/51), whereas the rate of the new method using the CT attenuation values of ascites was 78.4% (40/51). Applying our new method to the nine patients for whom perforation sites could not be predicted by CT findings, five could be precisely predicted. Thus, the site prediction rate improved by 9.8% compared to that of the CT findings alone (Table 4).
| Site prediction rate | |
| CT findings | 42 (82.4) |
| CT attenuation values of ascites | 40 (78.4) |
| Combining both methods | 47 (92.2) |
In this study, we showed that the CT attenuation values of ascites in patients with GI perforations were correlated with the perforation sites (colorectal or others), suggesting that the CT attenuation values of ascites are useful for diagnosing perforation sites. The CT attenuation values of ascites were particularly correlated with SSIs. The CT attenuation values measured in any three points on a single CT image, which is more convenient, was comparable with volume rendering and could immediately improve the diagnostic procedure for patients with acute abdomen. These results propose a new application of CT and suggest that this imaging method is useful for the evaluation of morphological as well as qualitative and quantitative findings.
CT is a strong modality for the diagnosis of GI perforation and should be performed routinely for most patients with acute abdomen[10,19-24]. A previous study proposed that a triad of characteristics (the concentration of extraluminal air bubbles, segmental bowel wall thickening, and focal defect of the bowel wall) was associated with the site of bowel perforation indicated by CT[14]. However, it was noted that 14% of all patients did not have any of these characteristics, and the perforation sites could not be predicted[14]. In this study, nine patients (17.6%) did not exhibit any of the three characteristics and, consequently, the perforation sites could not be predicted. Using the CT attenuation values with a cut-off point of 18 HU as an auxiliary diagnosis, the accuracy of perforation site prediction was improved by 9.8%. These results suggested that combining the two methods could enhance the efficiency and power of GI perforation diagnosis.
The CT attenuation value is defined as the radiodensity of each material and is expressed in HUs, in which the radiodensity of distilled water at standard pressure and temperature was defined as 0 HU, whereas that of air was defined as -1000 HU. Each tissue has unique CT attenuation values, although the values vary by tissue components. These quantitative values have been applied to clinical diagnosis in several studies. Nandalur et al[25] analyzed the CT attenuation values of 145 pleural effusions and found that the mean attenuation of exudates (17.1 HU) was significantly higher than that of transudates (12.5 HU). Allen et al[26] reported that abdominal fluid collections exhibiting high fluid attenuation (> 20 HU) was a significant predictor of infection, suggesting that an infectious component has a higher CT attenuation value than does water. The findings of this study provide further evidence that a CT attenuation value is approximately proportional to the extent of the bacterial and contaminated contents derived from GI perforation. Thus, the application of the CT attenuation value is considered to be useful for evaluating fluid collections with the objective of quantitative and qualitative analyses. However, further investigations are required to define the role of CT attenuation values in clinical practice.
Volume rendering is extremely useful for obtaining anatomical and morphological information and has become a respected technique in the surgery. Frequently, 3D reconstruction of intra-abdominal organs has been utilized for preoperative assessment. The 3D reconstruction of vessels from preoperative CT clarifies the cross relationship of the ileocolic artery or the right colic artery with the superior mesenteric vein, which is important for appropriate lymphadenectomy in a right hemicolectomy[27]. A narrow pelvis, which is considered an operative risk in rectal surgery, can be evaluated preoperatively by 3D reconstruction of the pelvis[28]. Recent attempts to perform surgery by projecting a 3D reconstructed image on the patient’s body, with a beam fixed to the operating table to enhance spatial perception during surgical intervention (augmented reality) have been successful[29,30]. In this study, we used a novel method to measure CT attenuation values that was predominantly intended to minimize the influence of partial volume effects and biases incurred by each patient or image when measuring the values. Our finding suggested that the volume rendering method was useful in terms of qualitative and quantitative evaluations. However, it appears to be difficult to apply this method in practice during emergency situations. In the pursuit of more suitable clinical applications, we measured the CT attenuation values of ascites on a single CT image (2D method) and found that the 2D method was reproducible and strongly correlated with the volume rendering method. The 2D method was considered to be more suitable in practical applications.
There were some limitations to this study. First, the sample size was relatively small for conclusive results. Considering the rarity of GI perforation, a multi-centric prospective study should be conducted to assess the efficacy of CT attenuation values. In addition, this study was a retrospective analysis that potentially included selection bias.
Prediction of perforation sites is important because they greatly influence patient morbidity and mortality. To improve risk management, perforation site prediction is useful in evaluating the risk of postoperative complications at an early stage[11,18]. The results of the logistic regression analysis in this study suggested that the CT attenuation values of ascites might be helpful in evaluating the risk of postoperative complications. The CT attenuation values of ascites were better correlated with SSI than with systemic complications. This result was consistent with the fact that high CT attenuation values of ascites were significantly correlated with colorectal perforation, which increased the values because of infection and subsequent inflammation, and that the SSI risk in colorectal perforation was higher than that at other perforation sites. Our results indicated that CT attenuation values reflected local inflammation or properties of ascites.
The CT attenuation values of ascites in patients with GI perforations could simply and objectively predict perforation sites and is useful for predicting postoperative complications, particularly for SSIs. Our findings suggested that the evaluation of the CT attenuation values of ascites could assist in prompt and accurate diagnoses and decrease patient mortality and morbidity by shortening the time from diagnosis to appropriate intensive care. This study demonstrated that CT could reveal morphological characteristics as well as qualitative and quantitative information.
Despite recent advances in imaging techniques, surgical treatment, and intensive medical care, peritonitis caused by gastrointestinal (GI) perforation is associated with various complications. To prevent postoperative complications, prediction of perforation sites is important for surgeons to plan strategies for intensive perioperative care of patients with fatal illnesses.
Although the use of multi-detector row computed tomography (CT) has led to improvements in the diagnosis of GI perforation and the prediction of perforation sites, more precise identification of perforation sites is important for surgeons for appropriate and immediate patient management, particularly in an emergent situation.
The authors report that the CT attenuation values of ascites in patients with GI perforations could simply and objectively predict perforation sites and are useful for predicting postoperative complications. Applying the new method to the patients for whom perforation sites could not be predicted by the conventional perforation prediction using CT findings, the site prediction rate improved by 9.8% compared to that of the CT findings alone.
The study results suggest that the CT attenuation values of ascites could be helpful for predicting perforation sites, particularly in cases in which the perforation sites are difficult to predict by CT findings alone.
The CT attenuation value is defined as the radiodensity of each material and is expressed in HUs, in which the radiodensity of distilled water at the standard pressure and temperature was defined as 0 HU, whereas that of air was defined as -1000 HU. Each tissue has unique CT attenuation values, although the values vary by tissue components.
Using the cut-off value of the CT value of ascites, suggested by the authors, added five correct perforation site predictions. This simple method of differentiating colorectal perforation from other sites should be applied in emergency CT of acute abdomen.
P- Reviewer: Gong JS S- Editor: Ma YJ L- Editor: A E- Editor: Liu XM
| 1. | Rosen MP, Sands DZ, Longmaid HE, Reynolds KF, Wagner M, Raptopoulos V. Impact of abdominal CT on the management of patients presenting to the emergency department with acute abdominal pain. AJR Am J Roentgenol. 2000;174:1391-1396. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 162] [Cited by in F6Publishing: 170] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 2. | Ng CS, Watson CJ, Palmer CR, See TC, Beharry NA, Housden BA, Bradley JA, Dixon AK. Evaluation of early abdominopelvic computed tomography in patients with acute abdominal pain of unknown cause: prospective randomised study. BMJ. 2002;325:1387. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 114] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 3. | Tsujimoto H, Yaguchi Y, Hiraki S, Sakamoto N, Kumano I, Matsumoto Y, Yoshida K, Sugasawa H, Ono S, Yamamoto J. Peritoneal computed tomography attenuation values reflect the severity of peritonitis caused by gastrointestinal perforations. Am J Surg. 2011;202:455-460. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Noguiera C, Silva AS, Santos JN, Silva AG, Ferreira J, Matos E, Vilaça H. Perforated peptic ulcer: main factors of morbidity and mortality. World J Surg. 2003;27:782-787. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 68] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 5. | Svanes C, Lie RT, Svanes K, Lie SA, Søreide O. Adverse effects of delayed treatment for perforated peptic ulcer. Ann Surg. 1994;220:168-175. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 81] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 6. | Lehnert T, Buhl K, Dueck M, Hinz U, Herfarth C. Two-stage radical gastrectomy for perforated gastric cancer. Eur J Surg Oncol. 2000;26:780-784. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 48] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Shinkawa H, Yasuhara H, Naka S, Yanagie H, Nojiri T, Furuya Y, Ariki K, Niwa H. Factors affecting the early mortality of patients with nontraumatic colorectal perforation. Surg Today. 2003;33:13-17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 39] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Mäkelä JT, Kiviniemi H, Laitinen S. Prognostic factors of perforated sigmoid diverticulitis in the elderly. Dig Surg. 2005;22:100-106. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 40] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Bielecki K, Kamiński P. [Surgical treatment of colonic diverticulitis--personal observations]. Wiad Lek. 2001;54:233-240. [PubMed] [Cited in This Article: ] |
| 10. | Maniatis V, Chryssikopoulos H, Roussakis A, Kalamara C, Kavadias S, Papadopoulos A, Andreou J, Stringaris K. Perforation of the alimentary tract: evaluation with computed tomography. Abdom Imaging. 2000;25:373-379. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 104] [Cited by in F6Publishing: 111] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 11. | Kim SH, Shin SS, Jeong YY, Heo SH, Kim JW, Kang HK. Gastrointestinal tract perforation: MDCT findings according to the perforation sites. Korean J Radiol. 2009;10:63-70. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 91] [Cited by in F6Publishing: 96] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 12. | Catalano C, Fraioli F, Laghi A, Napoli A, Pediconi F, Danti M, Nardis P, Passariello R. High-resolution multidetector CT in the preoperative evaluation of patients with renal cell carcinoma. AJR Am J Roentgenol. 2003;180:1271-1277. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 147] [Cited by in F6Publishing: 160] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 13. | Chen CH, Huang HS, Yang CC, Yeh YH. The features of perforated peptic ulcers in conventional computed tomography. Hepatogastroenterology. 2001;48:1393-1396. [PubMed] [Cited in This Article: ] |
| 14. | Hainaux B, Agneessens E, Bertinotti R, De Maertelaer V, Rubesova E, Capelluto E, Moschopoulos C. Accuracy of MDCT in predicting site of gastrointestinal tract perforation. AJR Am J Roentgenol. 2006;187:1179-1183. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 160] [Cited by in F6Publishing: 166] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 15. | Oguro S, Funabiki T, Hosoda K, Inoue Y, Yamane T, Sato M, Kitano M, Jinzaki M. 64-Slice multidetector computed tomography evaluation of gastrointestinal tract perforation site: detectability of direct findings in upper and lower GI tract. Eur Radiol. 2010;20:1396-1403. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 33] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Schwesinger WH, Page CP, Gaskill HV, Steward RM, Chopra S, Strodel WE, Sirinek KR. Operative management of diverticular emergencies: strategies and outcomes. Arch Surg. 2000;135:558-562; discussion 562-563. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 69] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 17. | Gaertner WB, Kwaan MR, Madoff RD, Willis D, Belzer GE, Rothenberger DA, Melton GB. The evolving role of laparoscopy in colonic diverticular disease: a systematic review. World J Surg. 2013;37:629-638. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 18. | Ghekiere O, Lesnik A, Hoa D, Laffargue G, Uriot C, Taourel P. Value of computed tomography in the diagnosis of the cause of nontraumatic gastrointestinal tract perforation. J Comput Assist Tomogr. 2007;31:169-176. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 42] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 19. | Ghahremani GG. Radiologic evaluation of suspected gastrointestinal perforations. Radiol Clin North Am. 1993;31:1219-1234. [PubMed] [Cited in This Article: ] |
| 20. | Ongolo-Zogo P, Borson O, Garcia P, Gruner L, Valette PJ. Acute gastroduodenal peptic ulcer perforation: contrast-enhanced and thin-section spiral CT findings in 10 patients. Abdom Imaging. 1999;24:329-332. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 43] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Sherck J, Shatney C, Sensaki K, Selivanov V. The accuracy of computed tomography in the diagnosis of blunt small-bowel perforation. Am J Surg. 1994;168:670-675. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 119] [Cited by in F6Publishing: 119] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 22. | Gonzalez JG, Gonzalez RR, Patiño JV, Garcia AT, Alvarez CP, Pedrosa CS. CT findings in gastrointestinal perforation by ingested fish bones. J Comput Assist Tomogr. 1988;12:88-90. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 49] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Lohrmann C, Ghanem N, Pache G, Makowiec F, Kotter E, Langer M. CT in acute perforated sigmoid diverticulitis. Eur J Radiol. 2005;56:78-83. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 54] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 24. | Furukawa A, Sakoda M, Yamasaki M, Kono N, Tanaka T, Nitta N, Kanasaki S, Imoto K, Takahashi M, Murata K. Gastrointestinal tract perforation: CT diagnosis of presence, site, and cause. Abdom Imaging. 2005;30:524-534. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 99] [Cited by in F6Publishing: 72] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 25. | Nandalur KR, Hardie AH, Bollampally SR, Parmar JP, Hagspiel KD. Accuracy of computed tomography attenuation values in the characterization of pleural fluid: an ROC study. Acad Radiol. 2005;12:987-991. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | Allen BC, Barnhart H, Bashir M, Nieman C, Breault S, Jaffe TA. Diagnostic accuracy of intra-abdominal fluid collection characterization in the era of multidetector computed tomography. Am Surg. 2012;78:185-189. [PubMed] [Cited in This Article: ] |
| 27. | Spasojevic M, Stimec BV, Fasel JF, Terraz S, Ignjatovic D. 3D relations between right colon arteries and the superior mesenteric vein: a preliminary study with multidetector computed tomography. Surg Endosc. 2011;25:1883-1886. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 28. | Ogiso S, Yamaguchi T, Hata H, Fukuda M, Ikai I, Yamato T, Sakai Y. Evaluation of factors affecting the difficulty of laparoscopic anterior resection for rectal cancer: “narrow pelvis” is not a contraindication. Surg Endosc. 2011;25:1907-1912. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 29. | Sugimoto M, Yasuda H, Koda K, Suzuki M, Yamazaki M, Tezuka T, Kosugi C, Higuchi R, Watayo Y, Yagawa Y. Image overlay navigation by markerless surface registration in gastrointestinal, hepatobiliary and pancreatic surgery. J Hepatobiliary Pancreat Sci. 2010;17:629-636. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 30. | Volonté F, Pugin F, Bucher P, Sugimoto M, Ratib O, Morel P. Augmented reality and image overlay navigation with OsiriX in laparoscopic and robotic surgery: not only a matter of fashion. J Hepatobiliary Pancreat Sci. 2011;18:506-509. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 104] [Cited by in F6Publishing: 88] [Article Influence: 6.8] [Reference Citation Analysis (0)] |