Published online Apr 21, 2008. doi: 10.3748/wjg.14.2454
Revised: January 21, 2008
Published online: April 21, 2008
Non-invasive predictors of varices in cirrhosis would reduce the need for screening endoscopies. Platelet count and spleen size have been shown to be useful parameters, in mixed groups of cirrhotics with different aetiologies. We evaluated this in two homogeneous groups with cirrhosis due to hepatitis C and alcohol. Non-invasive predictors appear promising in the former group, but less so in the latter group.
- Citation: Sen S, Griffiths WJ. Non-invasive prediction of oesophageal varices in cirrhosis. World J Gastroenterol 2008; 14(15): 2454-2455
- URL: https://www.wjgnet.com/1007-9327/full/v14/i15/2454.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.2454
We read with interest the study by Alempijevic et al on non-invasive prediction of oesophageal varices in cirrhosis[1]. We agree this is an important clinical goal, thus reducing the need to screen all individuals with cirrhosis. Importantly, such predictors must have a high sensitivity, even at the cost of a lower specificity, to ensure that patients with varices are not missed. Platelet count and spleen size appear consistently discriminatory in recent series[2–6]. Giannini et al[23] have suggested the platelet:spleen size ratio as informative. Sharma and Aggarwal[6] have recently proposed a predictor function derived from these two parameters. Of note, all these studies evaluated mixed groups of cirrhosis with different aetiologies. We routinely measure spleen size by ultrasound and performed a retrospective study of all patients with cirrhosis due to either hepatitis C alone (n = 93) or alcohol alone (n = 77) who underwent screening gastroscopy in our unit over a four-year period. Patients with tumour, splenectomy or portal vein thrombosis were excluded.
In the hepatitis C group, both platelet count and spleen size had a good predictive ability for the presence of oesophageal varices, while the platelet: spleen size ratio and the reported predictor function were slightly superior (Table 1). The optimum cut-off for the platelet: spleen size ratio was 6.50, compared with 9.09 by Giannini et al[23], and that for the predictor function was 1.00, compared with the published figure of 1.09 (although the latter was for large varices only). We found, however, that a simple clinical predictor based on the best cut-off values obtained individually for platelet count and spleen size, was the most sensitive predictor of the presence of oesophageal varices. Platelet count ≤ 90 × 109/L and/or spleen size ≥ 14 cm achieved a sensitivity of 92% and a specificity of 69% in this cohort.
| Without varices | With varices | P-value | AUC of ROC curve | Best cut-off predictor value | Sensitivity (%) | Specificity (%) | |
| Hepatitis C cirrhosis | 67 | 26 | |||||
| Platelet count (× 109/L) | 136 ± 53 | 87 ± 44 | < 0.001 | 0.78 | 90 | 78 | 61 |
| Spleen size (cm) | 12.4 ± 2.6 | 15.0 ± 2.3 | < 0.001 | 0.78 | 14 | 82 | 65 |
| Platelet:Spleen ratio | 11.8 ± 6.0 | 6.2 ± 4.3 | < 0.001 | 0.81 | 6.5 | 82 | 65 |
| Platelet and spleen derived predictor[6] | 0.84 | 1 | 79 | 77 | |||
| Alcoholic cirrhosis | 42 | 35 | |||||
| Platelet count (× 109/L) | 200 ± 90 | 142 ± 99 | 0.009 | 0.74 | 130 | 79 | 57 |
| Spleen size (cm) | 11.2 ± 2.4 | 12.9 ± 3.5 | 0.02 | 0.68 | 12 | 71 | 54 |
| Platelet:Spleen ratio | 19.0 ± 10.6 | 13.4 ± 14.2 | 0.06 | 0.75 | 11.1 | 81 | 57 |
| Platelet and spleen derived predictor[6] | 0.72 | 0.09 | 71 | 60 |
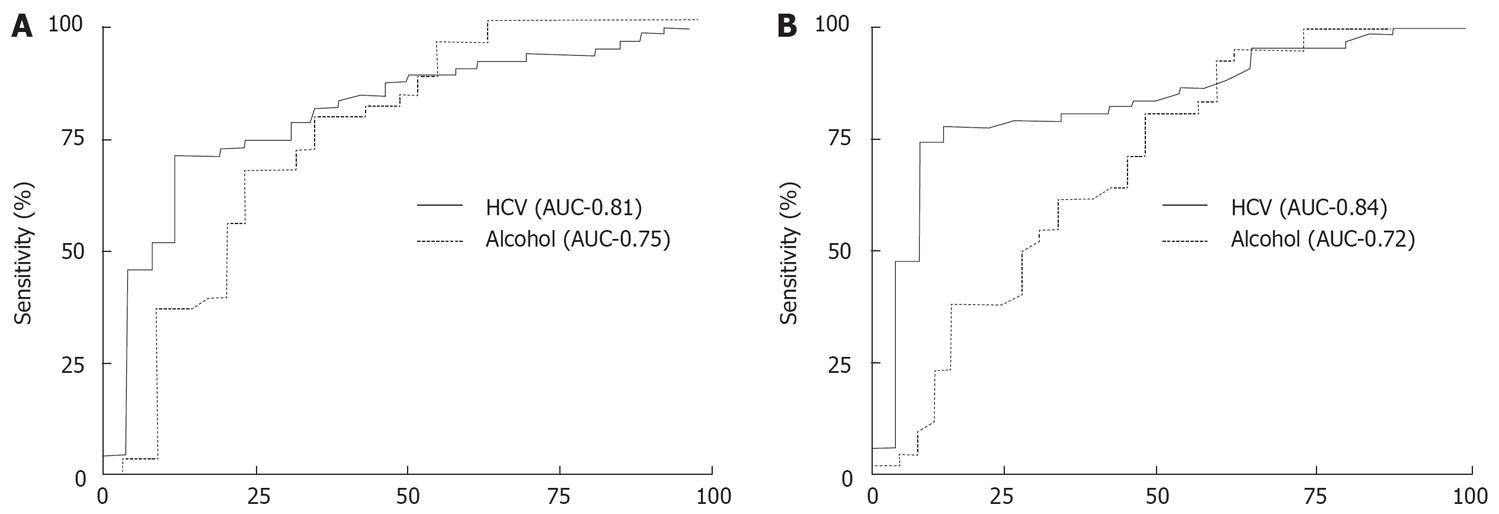
In the alcohol-related cirrhosis group, however, the predictive ability of all these parameters was generally poorer, as evidenced by a lower area under the curve (AUC) as well as a lower sensitivity and specificity compared with hepatitis C (Figure 1 and Table 1). Moreover, for the derived functions, cut-off values, which differed from those noted in the hepatitis C group and from the published values, had to be chosen to get a reasonable balance between sensitivity and specificity. With a platelet count ≤ 120 × 109/L and/or spleen size ≥ 12 cm, only a sensitivity of 74% and a specificity of 55% were obtained.
Our data suggest that easily obtainable non-invasive markers are effective for predicting oesophageal varices in hepatitis C cirrhosis but are not as promising for cirrhosis due to other aetiologies such as alcohol. In hepatitis C cirrhosis, portal pressure is presumably relatively stable whereas in alcohol-related liver disease, portal pressure may vary with consumption and abstinence. Furthermore, alcohol can cause thrombocytopenia through folate deficiency and a direct effect on platelet function and survival which may render platelet count a less accurate marker of portal pressure. This may explain why published predictors of varices which incorporate platelet count and a mix of aetiologies do not demonstrate the high sensitivity we observed in hepatitis C. The right liver lobe/albumin ratio proposed by Alempijevic et al[1] may, however, prove to be more consistently reliable in generalized cirrhosis. Further prospective studies should help to delineate the optimum approach and we look forward to future consensus guidelines which incorporate these strategies, reducing the burden of endoscopy for patients with cirrhosis.
| 1. | Alempijevic T, Bulat V, Djuranovic S, Kovacevic N, Jesic R, Tomic D, Krstic S, Krstic M. Right liver lobe/albumin ratio: contribution to non-invasive assessment of portal hypertension. World J Gastroenterol. 2007;13:5331-5335. [Cited in This Article: ] |
| 2. | Giannini E, Botta F, Borro P, Risso D, Romagnoli P, Fasoli A, Mele MR, Testa E, Mansi C, Savarino V. Platelet count/spleen diameter ratio: proposal and validation of a non-invasive parameter to predict the presence of oesophageal varices in patients with liver cirrhosis. Gut. 2003;52:1200-1205. [Cited in This Article: ] |
| 3. | Giannini EG, Zaman A, Kreil A, Floreani A, Dulbecco P, Testa E, Sohaey R, Verhey P, Peck-Radosavljevic M, Mansi C. Platelet count/spleen diameter ratio for the noninvasive diagnosis of esophageal varices: results of a multicenter, prospective, validation study. Am J Gastroenterol. 2006;101:2511-2519. [Cited in This Article: ] |
| 4. | Thomopoulos KC, Labropoulou-Karatza C, Mimidis KP, Katsakoulis EC, Iconomou G, Nikolopoulou VN. Non-invasive predictors of the presence of large oesophageal varices in patients with cirrhosis. Dig Liver Dis. 2003;35:473-478. [Cited in This Article: ] |
| 5. | Sethar GH, Ahmed R, Rathi SK, Shaikh NA. Platelet count/splenic size ratio: a parameter to predict the presence of esophageal varices in cirrhotics. J Coll Physicians Surg Pak. 2006;16:183-186. [Cited in This Article: ] |
| 6. | Sharma SK, Aggarwal R. Prediction of large esophageal varices in patients with cirrhosis of the liver using clinical, laboratory and imaging parameters. J Gastroenterol Hepatol. 2007;22:1909-1915. [Cited in This Article: ] |