JOURNAL OF DENTISTRY AND ORAL SCIENCES
Pleomorphic Adenoma of Palate - A Case Report and Review of Literature
| ReceivedOct 2, 2020 | RevisedOct 21, 2020 | AcceptedOct 30, 2020 | PublishedOct 30, 2020 |
Sameer Kaura1, Sumit K Bansal2, Rashi Bahl2, Prineet Sangha3, Simarpreet Singh3 and Himanta Bansal4
1Professor and Head, Department of Oral and Maxillofacial Surgery, Baba Jaswant Singh Dental College, Ludhiana, Punjab, India
2Professor, Department of Oral and Maxillofacial Surgery, Baba Jaswant Singh Dental College, Ludhiana, Punjab, India
3Senior Lecturer, Department of Oral and Maxillofacial Surgery, Baba Jaswant Singh Dental College, Ludhiana, Punjab, India
4Professor and Head, Department of Oral Pathology, Baba Jaswant Singh Dental College, Ludhiana, Punjab, India
*Corresponding Author: Sameer Kaura, Professor, and Head, Department of Oral and Maxillofacial Surgery, Baba Jaswant Singh Dental College, Ludhiana, Punjab, India.
Received Date: 10-02-2020; Published Date: 10-30-2020
Copyright© 2020 by Kaura S, et al. All rights reserved. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
10% of pleomorphic adenomas occur in the minor salivary glands with the palate being the most common site. Pleomorphic adenomas account for the majority of palatal tumors; however, minor salivary gland tumours have a higher risk of malignancy compared to tumors of the major salivary glands, so definite diagnostic evaluation should be executed. A case of 26-year-old man with a longstanding history of a soft palate pleomorphic adenoma which required excision under general anaesthetia We discuss the appropriate preoperative investigations, operative technique for surgical excision, histopathologic interpretation for this patient and a brief review of literature for pleomorphic adenoma.
Keywords
Pleomorphic adenoma; Minor salivary glands; Palatal tumors
Introduction
Pleomorphic adenoma (1866) was originally called a benign mixed tumor and its classic microscopic manifestation as described in 1874 [1,2] and the change in name to “pleomorphic adenoma” was first considered in 1948 with further considerable controversy has followed. The cellular component of a pleomorphic adenoma consists of epidermoid cells and myoepithelial cells. The exact name is “mixed tumor”, If the two cells have independent origins [1,3] and the term is used as “pleomorphic adenoma” when the two cells have a common origin [2,4,5]. The most common tumor (50%) of the major and minor salivary glands is Pleomorphic adenoma. The parotid gland accounts for maximum approximately 85% of these tumors, whereas the submandibular gland and the intraoral minor salivary glands account for 8% and 7%, respectively [3,4,6]. The most common site involving minor salivary glands where pleomorphic adenoma originates is the palate, followed by the lip. According to Vicente et al, the most common location affected by pleomorphic adenoma in the minor salivary glands region is the hard palate (42.5%), followed by upper lip mucosa and soft palate (16.7%), cheek mucosa and retromolar trigone (11.1%) and lower lip mucosa and tuberosity (5.6%) [5,7]. Heterotopic localization of pleomorphic adenomas which is infrequent has been described in paranasal sinuses, middle ear, tongue, and alimentary and respiratory tracts [4,5,8]. Carretta et al. described a 22-year-old woman with a pulmonary pleomorphic adenoma [8]. Yim et al. reported a 40-year old woman who had a pleomorphic adenoma in the auricle [8,9].The development of intraosseous pleomorphic adenoma is rare. A mixed tumor can occur at any age (women are affected slightly more often are than men) and is most prevalent in the fourth to sixth decades of life. Pleomorphic adenoma is a benign mixed tumor that appears as a firm painless mass that does not cause ulceration of the normal-appearing and adjacent mucosa. The mass is generally mobile in soft tissue regions but not in the hard palate region. The lack of a well-defined capsule is noted especially in the benign mixed tumors located in the palate. The invasion of the lesion in periosteum or bone is noted in this condition and out of which 25% of benign mixed tumors can undergo malignant transformation [5,7,9].
On histopathological considerations, this lesion is a combination of stromal and myoepithelial contents which may include hyaline, chondroid or myxoid contents. Microscopically this lesion involves the proliferation of cellular components having myoepithelial and/or ductal patterns. The most important role is determined by myoepithelial cells in the appearance and composition of the benign mixed tumor. In many studies, this lesion has a complete range of cells that includes a complete form of epithelial components and myoepithelial spectrum on the other end. In some cases, a mixture of both ductal and myoepithelial patterns with well-developed cells is evident. Some studies revealed that a single cell has the potential to differentiate into epithelial or myoepithelial components which are responsible for the origin of the lesion [9,11].
Case Report
A 26 years old man reported to the Department of Oral and Maxillofacial Surgery in Baba Jaswant Singh Dental College and Hospital, Ludhiana, India, with a chief complaint of mass present on the right side of the hard palate for 1 month which slowly increased in size until it becomes clinically evident.
Figure 1: Palatal swelling on hard and soft palate junction extended towards the midline.

Upon clinical examination, the lesion has a smooth surface,non-ulcerated, multinodular, non-tender, non-fluctuant extending towards the midline. The lesions measured about 3 × 2 cm upon palpation and involving the right maxillary third molar.
The NCCT was performed with axial (Figure 2), sagital and coronal sections to determine the mediolateral and anteroposterior extension of the lesion. NCCT revealed the lesion on the right side of the palate oval in shape approximately 3 cm in diameter with well-defined margins. The lesion has the same density as that of adjacent soft tissues with some scattered calcifications.
Figure 2: Axial section (CT SCAN) of palate revealing extension of the lesion.

An incisional biopsy was then performed. Surgical specimens were fixed in 10% formalin, routinely processed, and embedded in paraffin wax. Sections were stained with hematoxylin and eosin; special stain included periodic acid-Schiff with and without diastase digestion. The histologic picture showed the cellular and myxoid components in the stroma. The epithelial cells are forming ducts containing coagulum in few areas. The cells are growing in the form of cords and sheets and many spindle cells are seen which gives the myxoid appearance to many areas. The tumor, consistent with pleomorphic adenoma (cellular form), was separated from the salivary gland by a fibrous capsule.
Surgical Procedure
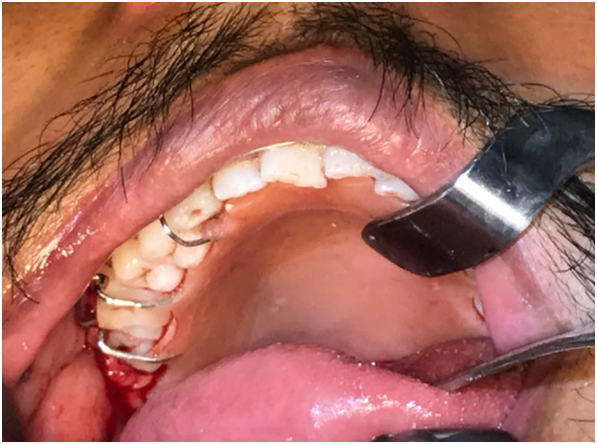
Surgical resection of tissue was planned for the patient under general anesthesia. Under endotracheal intubation, general anesthesia was administered and the patient was prepared with povidone-iodine. Local anesthesia (2% lignocaine) with adrenaline (1:2,00,000) was administered around the lesion for hemostatic purposes. The surgical site was marked with indelible ink involving the safe margins of 1cm from the lesion (Figure 3). The incision was made and blunt dissection was performed and excision of the whole encapsulated mass was done along with safe margins of 1cm from the extent of the lesion which includes the periosteum and bone involving the lesion (Figure 4).
Figure 3: Marking of the incision.

Figure 4: Surgical excision of the lesion.

Along with the excision of the lesion, the extraction of the right maxillary third molar was done.The surgical wound was covered with a buccal fat pad from the right side and closed with the advancement of adjacent mucosa in layers in a watertight fashion (Figure 5). There was no slight shift of uvula to the right after the final closure of the wound which did not affect the speech and swallowing of the patient postoperatively.
The surgical wound was covered with a buccal fat pad from the right side and the site was closed with resorbable sutures in a watertight fashion with the advancement of mucosa from the buccal side towards the palatal side. Because of the advancement of the mucosa, there is no change in the position of the uvula and due to which there is no change in the activity of speech and swallowing postoperatively.
Figure 5: Closure of defect using the buccal fat pad.

Hawley’s appliance was used as a surgical splint that helps in reducing palatal swelling, edema and hematoma postoperatively (Figure 6). The patient’s postoperative course was uneventful. No recurrence was observed after a follow-up of 1 year.
Figure 6: Surgical splint.
The excised tissue was sent for histopathological examination which has the same features as that of tissue taken during incisional biopsy (Figure 7).
Figure 7: Histological features include duct-like structures and consist of polygonal, spindle-shaped cells.

Discussion
According to various studies, among different variations of all salivary gland tumors, pleomorphic adenoma is most common and constitutes 70% of all salivary gland tumors.84% of tumor involves parotid gland, 8% in the submandibular gland and 4-6% occurred in minor salivary glands. The most common site involving minor salivary glands in the palate (54%), next followed by the upper lip and then buccal mucosa. The rare sites involved by tumor are sinuses, larynx, epiglottis, trachea, tongue, soft palate, vulva and external auditory canal.
Clinically, pleomorphic adenoma presents as a slow-growing asymptomatic, unilateral firm mass that may become large if untreated. When originating in the minor salivary glands, in most cases, it occurs on the soft and hard palate due to the highest concentration of salivary glands here and is typically a firm or rubbery submucosal mass without ulceration or surrounding ulceration [7,11,15]. The key feature of pleomorphic adenoma of minor salivary glands is that there is no capsule and is very thin if it is present which gives the wrong interpretation of infiltration. Since pleomorphic adenoma cannot invade the bone, this is not caused by bony invasion but rather by inelasticity of palatal mucosa, which becomes distended by tumor mass and eventuate in cupped-out resorption of bone which is seen in radiographs [11,13,16].
For the planning surgery of hard and soft palate tumors, key factors are to be considered for anesthetic purposes during intubation and postoperative airway management. Standardized intravenous protocols are appropriate for adults without airway obstruction e.g. propofol 4–6 mg/kg. Placement of head ring and roll under the patient’s shoulders help in extension of the neck and moves the head down, and throat packs are to be placed to absorb blood and salivary secretions. Local anaesthesia (2 % lignocaine with 1:200,000 adrenaline) can be used for infiltration for intraoperative analgesia, haemostatic purposes which improves the surgical field [6,8,17]. Reduction of anesthetic requirements by providing proper ventilation with smooth muscle relaxation promotes rapid patient consciousness, retaining the patient’s reflexes, lowering of PaCO2, which may reduce the blood loss. Extubation should be done when the patient is fully awake and nasopharyngeal airways (NPA) can be used for patients at high risk of airway obstructions postoperatively, which may be inserted before emergence. Once the swelling has been subsided and the patient has restored the breathing through the mouth, (NPA) can be removed on the following day. For the first initial 12–24 hrs, careful monitoring should be carried out for any changes in vital signs, early detection of any airway obstruction or postoperative bleeding [13,14,18].
Palatal abscess, odontogenic and non-odontogenic tumors & cysts, soft tissue tumors and salivary gland tumors are included in the differential diagnosis. Palatal abscess which is associated with the non-vital tooth is excluded from differential diagnosis upon clinical examination. The lesion is not cystic, so odontogenic and non-the odontogenic cyst is not included in the present case. Soft tissue tumors involving palate and minor salivary glands like adenoid cystic, mucoepidermoid, polymorphous low-grade adenocarcinomas and other soft tissue tumors considered in this case can be fibroma, neurofibroma, lipoma, neurilemmoma [17,19,20].
The key point for the treatment of salivary gland tumor is surgical resection of the lesion along with adjacent normal soft tissue. If the lesion involves the bone then the periosteum and bone are to be included in the surgical procedure. Soft tissue defects after resection can be reconstructed with some soft tissues or it can be left as it is to granulate. Bony defects in a dentate patient can be treated conservatively with an obturator. Careful preoperative diagnosis and patient evaluation of pleomorphic adenoma by radiographic and histopathologic interpretation are necessary as the majority of soft tissue tumors involving minor salivary glands arising in the palate are malignant. Complete surgical excision with a wide margin provides definitive diagnosis and treatment for this rare tumor [4,6,18].
Conclusion
Pleomorphic adenoma of the palate is rare for which diagnostic investigations with FNAC and radiological investigations are necessary due to the higher risk of malignancy in minor salivary glands as compared to tumors of the major salivary glands. For accurate histopathological diagnosis, excisional biopsy is a mandatory and preoperative assessment of lesion that should be done for the best surgical approach to ensure complete excision. Long-term follow-up of the patient is necessary as the recurrence rate is high.
References
1. Byakodi S, Charanthimath S, Hiremath S, Kashalikar JJ. Pleomorphic adenoma of palate: a case report. Int J Dent Case Rep. 2011;1:36–40.
2. Kumar SS, Reddy PS, Prabhakar G. Pleomorphic adenoma of the nasal septum—case report. Indian J Pathol Microbiol. 2004;47:397–398.
3. Daryani D, Gopakumar R, Ajila V. Pleomorphic adenoma of soft palate: myoepithelial cell predominant. Indian J Dent Res. 2011;22:853–856.
4. Su A, Apple SK, Moatamed NA. Pleomorphic adenoma of the vulva, clinical reminder of a rare occurrence. Rare Tumours2012;4:e16
5. Shetty KC, Bhat V, Bhat SP, Hegde KS. Pleomorphic adenoma of the soft palate. World Artic Ear Nose Throat 2012;5(1)
6. Lingam RK, Daghir AA, Nigar E, Abbas SA, Kumar M. Pleomorphic adenoma (benign mixed tumour) of the salivary glands: its diverse clinical, radiological, and histopathological presentation. Br J Oral Maxillofac Surg. 2011;49:14–20
7. Dalati T, Hussein MR. Juvenile pleomorphic adenoma of the cheek: a case report and review of the literature. Diagn Pathol. 2009;4:32.
8. Yim YM, Yoon JW, Seo JW (2009). Pleomorphic adenoma in the auricle. J CraniofacSurg;20:951-952.
9. Dhanuthai K, Sappayatosok K, Kongin K. Pleomorphic adenoma of the palate in a child: a case report. Med Oral Patol Oral Cir Bucal, 2009;14:E73-E75
10. Lingam RK, Daghir AA, Nigar E. Pleomorphic adenoma (benign mixed tumour) of the salivary glands: its diverse clinical, radiological, and histopathological presentation. Br J Oral Maxillofac Surg. 2011;49:14-20.
11. Nouraei SAR, Ferguson MS, Clarke PM. Metastasizing pleomorphic salivary adenoma. Arch Otolaryngol Head Neck Surg. 2006;132:788-793.
12. Shabaan H, Bruce J, Davenport PJ. Recurrent pleomorphic adenoma of the palate in a child. Br J Plast Surg. 2001;54:245.
13. Hakeem AH, Hazarika B, Pradhan SA, Kannan R. Primary pleomorphic adenoma of minor salivary gland in the parapharyngeal space. World J Surg Oncol 2009;7:85
14. Pogrel MA. The management of salivary gland tumors of the palate. J Oral Maxillofac Surg. 1994;52(5):454–459.
15. Motomura H, Harada T, Muraoka M, Taniguchi T. Elongated uvula with a pleomorphic adenoma: a rare cause of obstructive sleep apnoea. Ann Plast Surg.2000;45(1):61–63.
16. Jaber MA. Intraoral minor salivary gland tumors: a review of 75 cases in a Libyan population. Int J Oral Maxillofac Surg.2006;35(2):150–154.
17. Lingam RK, Daghir AA, Nigar E, Abbas SA, Kumar M. Pleomorphic adenoma (benign mixed tumour) of the salivary glands: its diverse clinical, radiological, and histopathological presentation. Br J Oral Maxillofac Surg.2011;49:14–20.
18. Pramod Krishna B. PLEOMORPHIC adenoma of minor salivary gland in a 14-year-old child. J Maxillofac Oral Surg. 2013;12(2):228-31.
19. Shaaban H, Bruce J, Davenport PJ. Recurrent pleomorphic adenoma of the palate in a child.Br J Plast Surg. 2011;54(3):245-7.
20. Hmidi M, Aatifi H, Boukhari A, Zalagh M, Messary A. Pleomorphic adenoma of the soft palate: major tumor in a minor gland. Pan Afr Med J. 2015;22:281.
21. Shrestha A, Reddy NS, Ganguly SN. Pleomorphic adenoma of the upper lip: a case report. J Coll Med Sci (Nepal).2010;6:51–53.
22. Forde CT, Millard R, Ali S. Soft Palate Pleomorphic Adenoma of a Minor Salivary Gland: An Unusual Presentation. Case Rep Otolaryngol 2018 Mar 31;2018:3986098.
