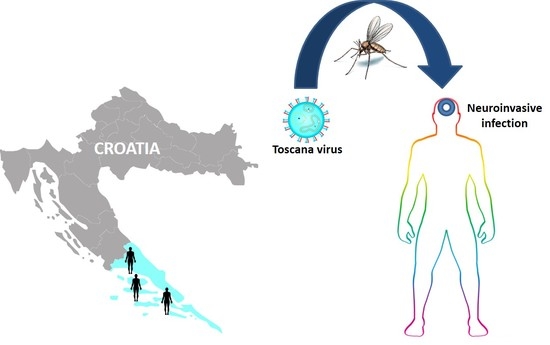
Clinical, Virological, and Immunological Findings in Patients with Toscana Neuroinvasive Disease in Croatia: Report of Three Cases
Abstract
:1. Background
2. Case Reports
2.1. Virology Results
2.2. Anti-Viral Cytokine Response
3. Discussion
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ayhan, N.; Prudhomme, J.; Laroche, L.; Bañuls, A.L.; Charrel, R.N. Broader Geographical Distribution of Toscana Virus in the Mediterranean Region Suggests the Existence of Larger Varieties of Sand Fly Vectors. Microorganisms 2020, 8, 114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cusi, M.G.; Savellini, G.G.; Zanelli, G. Toscana virus epidemiology: From Italy to beyond. Open Virol. J. 2010, 4, 22–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuhn, J.; Bewermeyer, H.; Hartmann-Klosterkoetter, U.; Emmerich, P.; Schilling, S.; Valassina, M. Toscana virus causing severe meningoencephalitis in an elderly traveler. J. Neurol. Neurosurg. Psychiatry 2005, 76, 1605–1606. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papa, A.; Paraforou, T.; Papakonstantinou, I.; Pagdatoglou, K.; Kontana, A.; Koukoubani, T. Severe encephalitis caused by Toscana virus, Greece. Emerg. Infect. Dis. 2014, 20, 1417–1419. [Google Scholar] [CrossRef]
- Marlinge, M.C.; Crespy, L.; Zandotti, C.; Piorkowski, G.; Kaphan, E.; Charrel, R.N.; Ninove, L. Afebrile meningoencephalitis with transient central facial paralysis due to Toscana virus infection, south-eastern France. Euro Surveill. 2014, 19, 20974. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanbonmatsu-Gámez, S.; Pérez-Ruiz, M.; Palop-Borrás, B.; Navarro-Marí, J.M. Unusual manifestation of Toscana virus infection, Spain. Emerg. Infect. Dis. 2009, 15, 347–348. [Google Scholar] [CrossRef]
- Ayhan, N.; Charrel, R.N. An update on Toscana virus distribution, genetics, medical and diagnostic aspects. Clin. Microbiol. Infect. 2020, 26, 1017–1023. [Google Scholar] [CrossRef]
- Cusi, M.G.; Savellini, G.G. Diagnostic tools for Toscana virus infection. Expert Rev. Anti-Infect. 2011, 9, 799–805. [Google Scholar] [CrossRef]
- Punda-Polić, V.; Mohar, B.; Duh, D.; Bradarić, N.; Korva, M.; Fajs, L.; Saksida, A.; Avšič-Županc, T. Evidence of an autochthonous Toscana virus strain in Croatia. J. Clin. Virol. 2012, 55, 4–7. [Google Scholar] [CrossRef]
- Punda-Polić, V.; Jerončić, A.; Mohar, B.; Šiško Kraljević, K. Prevalence of Toscana virus antibodies in residents of Croatia. Clin. Microbiol. Infect. 2012, 18, E200–E203. [Google Scholar] [CrossRef] [Green Version]
- Ayhan, N.; Alten, B.; Ivovic, V.; Martinkovic, F.; Kasap, O.E.; Ozbel, Y.; de Lamballerie, W.; Charrel, R.N. Cocirculation of two Lineages of Toscana Virus in Croatia. Front. Public Health 2017, 5, 336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwaiger, M.; Cassinotti, P. Development of a quantitative real-time RT-PCR assay with internal control for the laboratory detection of tick-borne encephalitis virus (TBEV) RNA. J. Clin. Virol. 2003, 27, 136–145. [Google Scholar] [CrossRef]
- Tang, Y.; Anne Hapip, C.; Liu, B.; Fang, C.T. Highly sensitive TaqMan RT-PCR assay for detection and quantification of both lineages of West Nile virus RNA. J. Clin. Virol. 2003, 36, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Nikolay, B.; Weidmann, M.; Dupressoir, A.; Faye, O.; Boye, C.S.; Diallo, M.; Sall, A.A. Development of a Usutu virus specific real-time reverse transcription PCR assay based on sequenced strains from Africa and Europe. J. Virol. Methods 2014, 197, 51–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weidmann, M.; Sanchez-Seco, M.P.; Sall, A.A.; Ly, P.O.; Thiongane, Y.; Lô, M.M.; Schley, H.; Hufert, F.T. Rapid detection of important human pathogenic Phleboviruses. J. Clin. Virol. 2008, 41, 138–142. [Google Scholar] [CrossRef]
- Li, H.; Cao, Y.X.; He, X.X.; Fu, S.H.; Lyu, Z.; He, Y.; Gao, X.Y.; Liang, G.D.; Wang, H.Y. Real-time RT-PCR Assay for the detection of Tahyna virus. Biomed. Environ. Sci. 2015, 28, 374–377. [Google Scholar]
- Matsuno, K.M.; Weisend, C.; Travassos da Rosa, A.P.; Anzick, S.L.; Dahlstrom, E.; Porcella, S.F.; Dorward, D.W.; Yu, X.J.; Tesh, R.B.; Ebihara, H. Characterization of the Bhanja serogroup viruses (Bunyaviridae): A novel species of the genus Phlebovirus and its relationship with other emerging tick-borne phleboviruses. J. Virol. 2013, 87, 3719–3728. [Google Scholar] [CrossRef] [Green Version]
- Ilic, M.; Barbic, L.; Bogdanic, M.; Tabain, I.; Savic, V.; Kosanovic Licina, M.L.; Kaic, B.; Jungic, A.; Vucelja, M.; Angelov, V.; et al. Tick-borne encephalitis outbreak following raw goat milk consumption in a new micro-location, Croatia, June 2019. Ticks Tick Borne Dis. 2020, 11, 101513. [Google Scholar] [CrossRef]
- Vilibic-Cavlek, T.; Kaic, B.; Barbic, L.; Pem-Novosel, I.; Slavic-Vrzic, V.; Lesnikar, V.; Kurecic-Filipovic, S.; Babic-Erceg, A.; Listes, E.; Stevanovic, V.; et al. First evidence of simultaneous occurrence of West Nile virus and Usutu virus neuroinvasive disease in humans in Croatia during the 2013 outbreak. Infection 2014, 42, 689–695. [Google Scholar] [CrossRef]
- Vilibic-Cavlek, T.; Savic, V.; Sabadi, D.; Peric, L.; Barbic, L.; Klobucar, A.; Miklausic, B.; Tabain, I.; Santini, M.; Vucelja, M.; et al. Prevalence and molecular epidemiology of West Nile and Usutu virus infections in Croatia in the “One Health” context, 2018. Transbound Emerg. Dis. 2019, 66, 1946–1957. [Google Scholar] [CrossRef]
- Pierro, A.; Ficarelli, S.; Ayhann, N.; Morini, S.; Raumer, L.; Bartoletti, M.; Mastroianni, A.; Prati, F.; Schivazappa, S.; Cenni, P.; et al. Characterization of antibody response in neuroinvasive infection caused by Toscana virus. Clin. Microbiol. Infect. 2017, 23, 868–873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rauch, J.; Zammarchi, L.; Corti, G.; Bartoloni, A.; Schlaphof, A.; Schmidt-Chanasit, J.; Tappe, D. Serum cytokine and chemokine changes during Toscana virus meningitis. Med. Microbiol. Immunol. 2019, 208, 727–730. [Google Scholar] [CrossRef] [PubMed]
- Varani, S.; Gelsomino, F.; Bartoletti, M.; Viale, P.; Mastroianni, A.; Briganti, E.; Ortolani, P.; Albertini, F.; Calzetti, C.; Prati, F.; et al. Meningitis caused by Toscana virus is associated with strong antiviral response in the CNS and altered frequency of blood antigen-presenting cells. Viruses 2015, 7, 5831–5843. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, H.; Li, Y.; Wen, B.; Zhang, J.; Wang, C.; Song, Z.; Li, S.; Qu, X.; Huang, R.; Liu, W. Dengue virus and Japanese encephalitis virus infection of the central nervous system share similar profiles of cytokine accumulation in cerebrospinal fluid. Cent. Eur. J. Immunol. 2017, 42, 218–222. [Google Scholar] [CrossRef]
- Bogovič, P.; Lusa, L.; Korva, M.; Lotrič-Furlan, S.; Resman-Rus, K.; Pavletič, M.; Avšič-Županc, T.; Strle, K.; Strle, F. Inflammatory immune responses in patients with tick-borne encephalitis: Dynamics and association with the outcome of the disease. Microorganisms 2019, 7, E514. [Google Scholar] [CrossRef] [Green Version]
- Miller, J.D.; Pruitt, S.; McDonald, T.J. Acute brachial plexus neuritis: An uncommon cause of shoulder pain. Am. Fam. Physician. 2000, 62, 2067–2072. [Google Scholar]
- Torres, M.O.; Gudlavalleti, A.; Mesfin, F.B. Brachial Plexitis (Parsonage Turner Syndrome, Brachial Neuropathy, Brachial Radiculitis). [Updated 2020 July 19]. Available online: https://www.ncbi.nlm.nih.gov/books/NBK448114/ (accessed on 12 August 2020).
- Bartels, S.; de Boni, L.; Kretzschmar, H.A.; Heckmann, J.G. Lethal encephalitis caused by the Toscana virus in an elderly patient. J. Neurol. 2012, 259, 175–177. [Google Scholar] [CrossRef]
- Charrel, R.N.; Bichaud, L.; de Lamballerie, X. Emergence of Toscana virus in the Mediterranean area. World J. Virol. 2012, 1, 135–141. [Google Scholar] [CrossRef]
- Cantu, R.M.; Das, J.M. Viral Meningitis. Available online: https://www.ncbi.nlm.nih.gov/books/NBK545217/ (accessed on 12 August 2020).

| Characteristic | Case 1 | Case 2 | Case 3 |
|---|---|---|---|
| Age | 21 years | 22 years | 54 years |
| Gender | Male | Female | Male |
| Area of residence | Croatian littoral (Middle Dalmatia) | Croatian mainland (worked at the Croatian littoral; Middle Dalmatia from July 2019) | Croatian littoral (stayed on holiday in Middle Dalmatia) |
| Time of disease onset | Late August | Late August | Mid October |
| Clinical presentation | Meningitis | Meningoencephalitis | Meningitis |
| Clinical symptoms | Fever (up to 38 °C), headache, nausea, vomiting, photophobia, weakness | Fever (up to 38 °C), headache, nausea, vomiting, photophobia, dizziness, weakness, arthralgia, maculopapular rash, right-sided brachial plexitis | Severe headache, vomiting, weakness |
| Duration of symptoms | 5 days | 20 days | 5 days |
| Outcome | Recovered | Improved | Recovered |
| Virus | CASE 1 | CASE 2 | CASE 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| ELISA IgM a/IgG b | IFA IgM/IgG c | RT-qPCR | ELISA IgM a/IgG b | IFA IgM/IgG c | RT-qPCR | ELISA IgM a/IgG b | IFA IgM/IgG c | RT-qPCR | |
| TBEV | NegNeg | NT | Neg | Neg/Neg | NT | Neg | Neg/Neg | NT | Neg |
| WNV | Neg/Neg | NT | Neg | Neg/Neg | NT | Neg | Neg/Neg | NT | Neg |
| USUV | NT/Neg | NT | Neg | NT/Neg | NT | Neg | NT/Neg | NT | Neg |
| SFSV | NT | Neg/Neg | NT | NT | Neg/Neg | NT | NT | Neg/Neg | NT |
| SFNV | NT | Neg/Neg | NT | NT | Neg/Neg | NT | NT | Neg/Neg | NT |
| SFCV | NT | Neg/Neg | NT | NT | Neg/Neg | NT | NT | Neg/Neg | NT |
| TOSV | NT | 1000/3200 | Neg | NT | 3200/3200 | Neg | NT | 1000/10,000 | Neg |
| TAHV | NT | NT | Neg | NT | NT | Neg | NT | NT | Neg |
| BHAV | NT | NT | Neg | NT | NT | Neg | NT | NT | Neg |
| Cytokine (pg/mL) | Case 1 | Case 2 | Case 3 | Detection Limits (Minimum Detectable Concentrations + 2xSD, pg/mL) | |||
|---|---|---|---|---|---|---|---|
| Serum | CSF | Serum | CSF | Serum | CSF | ||
| IL-5 | Neg | Neg | 5.35 | Neg | Neg | 3.20 | 1.2 + 1.3 |
| IL-13 | Neg | Neg | 18.68 | Neg | 71.25 | 40.05 | 1.4 + 0.7 |
| IL-2 | 5.92 | Neg | Neg | Neg | Neg | 35.01 | 1.4 + 0.4 |
| IL-6 | Neg | 162.32 | 8.35 | 517.32 | 9.29 | 2683.90 | 1.0 + 0.8 |
| IL-9 | 5.51 | 5.01 | 4.80 | 2.13 | Neg | 7.62 | 1.7 + 1.4 |
| IL-10 | Neg | 199.99 | Neg | 28.08 | Neg | 858.91 | 0.7 + 0.4 |
| IFN-γ | Neg | 110.12 | 28.23 | 206.92 | Neg | 1568.07 | 1.1 + 0.7 |
| TNF-α | 13.75 | Neg | Neg | Neg | Neg | Neg | 0.7 + 0.5 |
| IL-17A | Neg | Neg | 32.94 | Neg | Neg | Neg | 1.9 + 0.6 |
| IL-17F | 15.21 | Neg | Neg | Neg | Neg | Neg | 0.8 + 0.7 |
| IL-4 | 18.43 | Neg | 5.97 | Neg | Neg | Neg | 1.0 + 0.8 |
| IL-21 | 78.13 | Neg | 10.98 | Neg | Neg | Neg | 6.0 + 3.0 |
| IL-22 | Neg | Neg | Neg | 28.49 | Neg | 45.24 | 1.5 + 0.5 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vilibic-Cavlek, T.; Zidovec-Lepej, S.; Ledina, D.; Knezevic, S.; Savic, V.; Tabain, I.; Ivic, I.; Slavuljica, I.; Bogdanic, M.; Grgic, I.; et al. Clinical, Virological, and Immunological Findings in Patients with Toscana Neuroinvasive Disease in Croatia: Report of Three Cases. Trop. Med. Infect. Dis. 2020, 5, 144. https://doi.org/10.3390/tropicalmed5030144
Vilibic-Cavlek T, Zidovec-Lepej S, Ledina D, Knezevic S, Savic V, Tabain I, Ivic I, Slavuljica I, Bogdanic M, Grgic I, et al. Clinical, Virological, and Immunological Findings in Patients with Toscana Neuroinvasive Disease in Croatia: Report of Three Cases. Tropical Medicine and Infectious Disease. 2020; 5(3):144. https://doi.org/10.3390/tropicalmed5030144
Chicago/Turabian StyleVilibic-Cavlek, Tatjana, Snjezana Zidovec-Lepej, Dragan Ledina, Samira Knezevic, Vladimir Savic, Irena Tabain, Ivo Ivic, Irena Slavuljica, Maja Bogdanic, Ivana Grgic, and et al. 2020. "Clinical, Virological, and Immunological Findings in Patients with Toscana Neuroinvasive Disease in Croatia: Report of Three Cases" Tropical Medicine and Infectious Disease 5, no. 3: 144. https://doi.org/10.3390/tropicalmed5030144