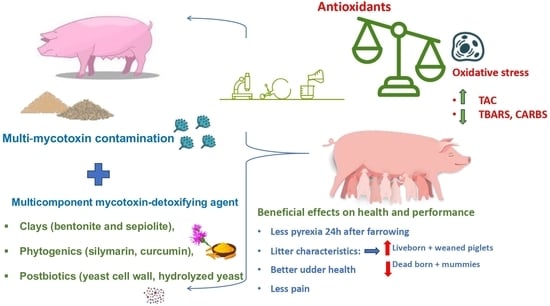
Effects of a Multi-Component Mycotoxin-Detoxifying Agent on Oxidative Stress, Health and Performance of Sows
Abstract
:1. Introduction
2. Results
2.1. Mycotoxins Detection and Quantification in the Feed of Trial Farms
2.2. Oxidative Stress Biomarkers
2.3. Clinical and Performance Parameters
3. Discussion
4. Conclusions
5. Materials and Methods
5.1. Trial Farms: Animals and Diets
5.2. Laboratory Examinations for Mycotoxins in Feed
5.3. Experimental Material
5.4. Study Design
5.4.1. Study 1
5.4.2. Study 2
5.5. Blood Sampling
5.6. Laboratory Examinations for Oxidative Stress Biomarkers
5.7. Clinical Examination and Records
5.8. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AFB1 | Aflatoxin B1 |
| AFB2 | Aflatoxin B2 |
| AFG1 | Aflatoxin G1 |
| AFG2 | Aflatoxin G2 |
| Affs | Aflatoxins |
| AI | Artificial Insemination |
| CARBS | Protein Carbonyls |
| DON | deoxynivalenol |
| FUB1 | Fumonisin B1 |
| FUB2 | Fumonisin B2 |
| FUBsS | Fumonisins |
| GI | Gastrointestinal Tract |
| HPLC | High-Pressure Liquid Chromatography |
| HT2 | Trichothecene Trichothecene Toxin HT2 toxin |
| IUGR | Intrauterine Growth Restriction |
| MDA | Malondialdehyde |
| OTA | Ochratoxin A |
| PDS | Postpartum Dysgalactia Syndrome |
| ROS | Reactive Oxygen Species |
| SD | Standard Deviation |
| SPF | Specific Pathogen-Free |
| T2 | Trichothecene Toxin T2 toxin |
| TAC | Total Antioxidant Capacity |
| TBARS | Thiobarbituric acid reactive substances |
| ZEN | Zearalenone |
References
- Bennett, J.W.; Klich, M. Mycotoxins. Clin. Microbiol. Rev. 2003, 16, 497–516. [Google Scholar] [CrossRef]
- Marroquin-Cardona, A.G.; Johnson, N.M.; Phillips, T.D.; Hayes, A.W. Mycotoxins in a changing global environment—A review. Food Chem. Toxicol. 2014, 69, 220–230. [Google Scholar] [CrossRef]
- Gurikar, C.; Shivaprasad, D.P.; Sabillón, L.; Gowda, N.A.; Siliveru, K. Impact of mycotoxins and their metabolites associated with food grains. Sci. Technol. 2023, 6, 1–9. [Google Scholar] [CrossRef]
- Streit, E.; Naehrer, K.; Rodrigues, I.; Schatzmayr, G. Mycotoxin occurrence in feed and feed raw materials worldwide: Long-term analysis with special focus on Europe and Asia. J. Sci. Food Agric. 2013, 93, 2892–2899. [Google Scholar] [CrossRef] [PubMed]
- FAO/WHO. Expert Committee on Food Additives. Report on Meeting of Experts Committee and Study Groups, Evaluation of Certain Mycotoxins; EB148/47; Excecutive Board: Geneva, Italy, 2020. [Google Scholar]
- Marin, S.; Ramos, A.; Cano-Sancho, G.; Sanchis, V. Mycotoxins: Occurrence, toxicology, and exposure assessment. Food Chem. Toxicol. 2013, 60, 218–237. [Google Scholar] [CrossRef]
- Tkaczyk, A.; Jedziniak, P. Mycotoxin Biomarkers in Pigs-Current State of Knowledge and Analytics. Toxins 2021, 13, 586. [Google Scholar] [CrossRef] [PubMed]
- Bryden, W.L. Mycotoxin contamination of the feed supply chain: Implications for animal productivity and feed security. Anim. Feed Sci. Technol. 2012, 173, 134–158. [Google Scholar] [CrossRef]
- Magnoli, A.P.; Poloni, V.L.; Cavaglieri, L. Impact of mycotoxin contamination in the animal feed industry. Curr. Opin. Food Sci. 2019, 29, 99–108. [Google Scholar] [CrossRef]
- Pierron, A.; Alassane-Kpembi, I.; Oswald, I.P. Impact of mycotoxin on immune response and consequences for pig health. Anim. Nutr. 2016, 2, 63–68. [Google Scholar] [CrossRef]
- Cortinovis, C.; Pizzo, F.; Spicer, L.J.; Caloni, F. Fusarium mycotoxins: Effects on reproductive function in domestic animals—A review. Theriogenology 2013, 80, 557–564. [Google Scholar] [CrossRef]
- Haschek, W.M.; Gumprecht, L.A.; Smith, G.; Tumbleson, M.E.; Constable, P.D. Fumonisin toxicosis in swine: An overview of porcine pulmonary edema and current perspectives. Environ. Health Perspect. 2001, 109, 251–257. [Google Scholar] [PubMed]
- Pinton, P.; Oswald, I.P. Effect of Deoxynivalenol and Other Type B Trichothecenes on the Intestine: A Review. Toxins 2014, 6, 1615–1643. [Google Scholar] [CrossRef] [PubMed]
- Akbari, P.; Braber, S.; Varasteh, S.; Alizadeh, A.; Garssen, J.; Fink-Gremmels, J. The intestinal barrier is an emerging target in the toxicological assessment of mycotoxins. Arch. Toxicol. 2017, 91, 1007–1029. [Google Scholar] [PubMed]
- Lei, M.; Zhang, N.; Qi, D. In vitro investigation of individual and combined cytotoxic effects of aflatoxin B1 and other selected mycotoxins on the cell line porcine kidney 15. Exp. Toxicol. Pathol. 2013, 65, 1149–1157. [Google Scholar] [CrossRef] [PubMed]
- Chaytor, A.C.; Hansen, J.A.; Van Heugten, E.; See, M.T.; Kim, S.W. Occurrence and Decontamination of Mycotoxins in Swine Feed. Asian-Australas. J. Anim. Sci. 2011, 24, 723–738. [Google Scholar] [CrossRef]
- Papatsiros, V.G.; Stylianaki, I.; Tsekouras, N.; Papakonstantinou, G.; Gómez-Nicolau, N.S.; Letsios, M.; Papaioannou, N. Exposure Biomarkers and Histopathological Analysis in Pig Liver After Exposure to Mycotoxins Under Field Conditions: Special Report on Fumonisin B1. Foodborne Pathog. Dis. 2021, 18, 315–321. [Google Scholar] [CrossRef]
- Dänicke, S.; Brüssow, K.P.; Goyarts, T.; Valenta, H.; Ueberschär, K.H.; Tiemann, U. On the transfer of the Fusarium toxins deoxynivalenol (DON) and zearalenone (ZON) from the sow to the full-term piglet during the last third of gestation. Food Chem. Toxicol. 2007, 45, 1565–1574. [Google Scholar] [CrossRef]
- Dolenšek, T.; Švara, T.; Knific, T.; Gombač, M.; Luzar, B.; Jakovac-Strajn, B. The Influence of Fusarium Mycotoxins on the Liver of Gilts and Their Suckling Piglets. Animals 2021, 11, 2534. [Google Scholar] [CrossRef]
- Liu, M.; Zhu, D.; Guo, D.; Zhang, Y.; Shi, B.; Shan, A.; Chen, Z. Toxicity of zearalenone on the intestines of pregnant sows and their offspring and alleviation with modified halloysite nanotubes. J. Sci. Food Agric. 2017, 98, 698–706. [Google Scholar] [CrossRef]
- Malekinejad, H.; Schoevers, E.J.; Daemen, I.J.J.M.; Zijstra, C.; Colenbrander, B.; Fink-Gremmels, J.; Roelen, B.A.J. Exposure of oocytes to the Fusarium toxins zearalenone and deoxynivalenol causes aneuploidy and abnormal embryo development in pigs. Biol. Reprod. 2007, 77, 840–847. [Google Scholar] [CrossRef]
- Zhou, J.; Zhao, L.; Huang, S.; Liu, Q.; Ao, X.; Lei, Y.; Ji, C.; Ma, Q. Zearalenone toxicosis on reproduction as estrogen receptor selective modulator and alleviation of zearalenone biodegradative agent in pregnant sows. J. Anim. Sci. Biotechnol. 2022, 13, 36. [Google Scholar] [CrossRef] [PubMed]
- Hennig-Pauka, I.; Koch, F.J.; Schaumberger, S.; Woechtl, B.; Novak, J.; Sulyok, M.; Nagl, V. Current challenges in the diagnosis of zearalenone toxicosis as illustrated by a field case of hyperestrogenism in suckling piglets. Porc. Health Manag. 2018, 4, 18. [Google Scholar] [CrossRef] [PubMed]
- Grenier, B.; Hackl, M.; Skalicky, X.; Thamhesl, M.; Moll, W.D.; Berrios, R.; Schatzmayr, G.; Nagl, V. MicroRNAs in porcine uterus and serum are affected by zearalenone and represent a new target for mycotoxin biomarker discovery. Sci. Rep. 2019, 9, 9408. [Google Scholar] [CrossRef] [PubMed]
- Benthem de Grave, X.; Saltzmann, J.; Laurain, J.; Rodriguez, M.A.; Molist, F.; Dänicke, S.; Santos, R.R. Transmission of Zearalenone, Deoxynivalenol, and Their Derivatives from Sows to Piglets during Lactation. Toxins 2021, 13, 37. [Google Scholar] [CrossRef]
- Kemper, N. Update on postpartum dysgalactia syndrome in sows. J. Anim. Sci. 2020, 98, S117–S125. [Google Scholar] [CrossRef]
- Huwig, A.; Freimund, S.; Käppeli, O.; Dutler, H. Mycotoxin detoxication of animal feed by different adsorbents. Toxicol. Lett. 2001, 122, 179–188. [Google Scholar] [CrossRef]
- Jouany, J.P. Methods for preventing, decontaminating and minimizing the toxicity of mycotoxins in feeds. Anim. Feed Sci. Technol. 2007, 137, 342–362. [Google Scholar] [CrossRef]
- Kabak, B.; Dobson, A.D.W.; Var, I. Strategies to prevent mycotoxin contamination of food and animal feed: A review. Crit. Rev. Food Sci. Nutr. 2006, 46, 593–619. [Google Scholar] [CrossRef]
- Jard, G.; Liboz, T.; Mathieu, F.; Guyonvarch, A.; Lebrihi, A. Review of mycotoxin reduction in food and feed: From prevention in the field to detoxification by adsorption or transformation. Food Addit. Contam. Part A Chem. Anal. Control Expo. Risk Assess. 2011, 28, 1590–1609. [Google Scholar] [CrossRef]
- Kolosova, A.; Stroka, J. Substances for reduction of the contamination of feed by mycotoxins: A review. World Mycotoxin J. 2011, 4, 225–256. [Google Scholar] [CrossRef]
- Sabater-Vilar, M.; Malekinejad, H.; Selman, M.H.J.; Van Der Doelen, M.A.M.; Fink-Gremmels, J. In vitro assessment of adsorbents aiming to prevent deoxynivalenol and zearalenone mycotoxicoses. Mycopathologia 2007, 163, 81–90. [Google Scholar] [CrossRef]
- Van Le Thanh, B.; Lessard, M.; Chorfi, Y.; dé ric Guay, F. The efficacy of anti-mycotoxin feed additives in preventing the adverse effects of wheat naturally contaminated with Fusarium mycotoxins on performance, intestinal barrier function and nutrient digestibility and retention in weanling pigs. Can. J. Anim. Sci. 2015, 95, 197–209. [Google Scholar] [CrossRef]
- Frobose, H.L.; Stephenson, E.W.; Tokach, M.D.; DeRouchey, J.M.; Woodworth, J.C.; Dritz, S.S.; Goodband, R.D. Effects of potential detoxifying agents on growth performance and deoxynivalenol (DON) urinary balance characteristics of nursery pigs fed DON-contaminated wheat. J. Anim. Sci. 2017, 95, 327–337. [Google Scholar]
- Lauwers, M.; Croubels, S.; Letor, B.; Gougoulias, C.; Devreese, M. Biomarkers for exposure as a tool for efficacy testing of a mycotoxin detoxifier in broiler chickens and pigs. Toxins 2019, 11, 187. [Google Scholar] [CrossRef]
- Jacela, J.Y.; DeRouchey, J.M.; Tokach, M.D. Feed additives for swine: Fact sheets—flavors and mold inhibitors, mycotoxin binders, and antioxidants. J. Swine Health Prod. 2010, 18, 27–32. [Google Scholar] [CrossRef]
- Döll, S.; Dänicke, S. In vivo detoxification of Fusarium toxins. Arch. Anim. Nutr. 2004, 58, 419–441. [Google Scholar] [CrossRef]
- AFSSA; CODA-CERVA; INRA Clermont-Ferrand; INRA Toulouse; IRTA. ISPA Review of mycotoxin-detoxifying agents used as feed additives: Mode of action, efficacy and feed/food safety. EFSA 2009, 6, E22. [Google Scholar]
- Sayyari, A.; Framstad, T.; Krogenæs, A.K. Effects of feeding naturally contaminated deoxynivalenol diets to sows during late gestation and lactation in a high-yield specific pathogen-free herd. Porc. Health Manag. 2018, 4, 26. [Google Scholar] [CrossRef]
- Benthem de Grave, X.; Saltzmann, J.; Laurain, J.; Rodriguez, M.A.; Molist, F.; Dänicke, S.; Santos, R.R. The Ability of an Algoclay-Based Mycotoxin Decontaminant to Decrease the Serum Levels of Zearalenone and Its Metabolites in Lactating Sows. Front. Vet. Sci. 2021, 8, 704796. [Google Scholar] [CrossRef]
- Holanda, D.M.; Kim, S.W. Efficacy of Mycotoxin Detoxifiers on Health and Growth of Newly-Weaned Pigs under Chronic Dietary Challenge of Deoxynivalenol. Toxins 2020, 12, 311. [Google Scholar] [CrossRef]
- Park, S.H.; Kim, J.; Kim, D.; Moon, Y. Mycotoxin detoxifiers attenuate deoxynivalenol-induced pro-inflammatory barrier insult in porcine enterocytes as an in vitro evaluation model of feed mycotoxin reduction. Toxicol. Vitr. 2017, 38, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Hoek, J.B.; Pastorino, J.G. Ethanol, oxidative stress, and cytokine-induced liver cell injury. Alcohol 2002, 27, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.W.; Holanda, D.M.; Gao, X.; Park, I.; Yiannikouris, A. Efficacy of a Yeast Cell Wall Extract to Mitigate the Effect of Naturally Co-Occurring Mycotoxins Contaminating Feed Ingredients Fed to Young Pigs: Impact on Gut Health, Microbiome, and Growth. Toxins 2019, 11, 633. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.B.; Carroll, J.A.; Yoon, I.; Mateo, R.D.; Kim, S.W. Effects of supplementing Saccharomyces cerevisiae fermentation product in sow diets on performance of sows and nursing piglets. J. Anim. Sci. 2011, 89, 2462–2471. [Google Scholar] [CrossRef]
- Hasan, S.; Junnikkala, S.; Peltoniemi, O.; Paulin, L.; Lyyski, A.; Vuoren-maa, J.; Oliviero, C. Dietary supplementation with yeast hydrolysate in pregnancy influences colostrum yield and gut mi- crobiota of sows and piglets after birth. PLoS ONE 2018, 13, e0197586. [Google Scholar] [CrossRef]
- Tan, C.W.; Li, J.Y.; Ji, Y.C.; Yang, Y.Y.; Zhao, X.C.; Chen, M.X.; Xin, Z.Q.; Wen, L.J.; Cui, Z.Y.; Shu, G. Effects of dietary supplementation of different amounts of yeast extract on oxidative stress, milk components, and productive performance of sows. J. Anim. Feed Sci. 2021, 247, 114648. [Google Scholar] [CrossRef]
- Chance, J.A.; DeRouchey, J.M.; Amachawadi, R.G.; Ishengoma, V.; Nagaraja, T.G.; Goodband, R.D.; Woodworth, J.C.; Tokach, M.D.; Kang, Q.; Loughmiller, J.A.; et al. Influence of yeast-based pre- and probiotics in lactation and nursery diets on nursery pig performance and antimicrobial resistance of fecal Escherichia coli. J. Anim. Sci. 2022, 100, skac166. [Google Scholar] [CrossRef]
- Holanda, D.M.; Yiannikouris, A.; Kim, S.W. Investigation of the Efficacy of a Postbiotic Yeast Cell Wall-Based Blend on Newly-Weaned Pigs under a Dietary Challenge of Multiple Mycotoxins with Emphasis on Deoxynivalenol. Toxins 2020, 12, 504. [Google Scholar] [CrossRef]
- Surai, P.F. Silymarin as a natural antioxidant: An overview of the current evidence and perspectives. Antioxidants 2015, 4, 204–247. [Google Scholar] [CrossRef]
- Wellington, K.; Jarvis, B. Silymarin: A review of its clinical properties in the management of hepatic disorders. BioDrugs 2001, 15, 465–489. [Google Scholar] [CrossRef]
- Schumann, J.; Prockl, J.; Kiemer, A.K.; Vollmar, A.M.; Bang, R.; Tiegs, G. Silibinin protects mice from T cell-dependent liver injury. J. Hepatol. 2003, 39, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.L.; Hsu, Y.C.; Chiu, Y.T.; Huang, Y.T. Antifibrotic effects of a herbal combination regimen on hepatic fibrotic rats. Phytother. Res. 2008, 22, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.H.; Huang, S.M.; Yen, G.C. Silymarin: A novel antioxidant with antiglycation and antiinflammatory properties in vitro and in vivo. Antioxid. Redox. Signal. 2011, 14, 353–366. [Google Scholar] [CrossRef] [PubMed]
- Karimi, G.; Vahabzadeh, M.; Lari, P.; Rashedinia, M.; Moshiri, M. “Silymarin”, a promising pharmacological agent for treatment of diseases. Iran. J. Basic Med. Sci. 2011, 14, 308–317. [Google Scholar]
- Farmer, C.; Lapointe, J.; Cormier, I. Providing the plant extract silymarin to lactating sows: Effects on litter performance and oxidative stress in sows. Animal 2017, 11, 405–410. [Google Scholar] [CrossRef]
- Jiang, X.; Lin, S.; Lin, Y.; Fang, Z.; Xu, S.; Feng, B.; Zhuo, Y.; Li, J.; Che, L.; Jiang, X.; et al. Effects of silymarin supplementation during transition and lactation on reproductive performance, milk composition and haematological parameters in sows. J. Anim. Physiol. Anim. Nutr. 2020, 104, 1896–1903. [Google Scholar] [CrossRef]
- Zhang, Q.; Ahn, J.M.; Kim, I.H. Micelle silymarin supplementation to sows’ diet from day 109 of gestation to entire lactation period enhances reproductive performance and affects serum hormones and metabolites. J. Anim. Sci. 2021, 99, skab354. [Google Scholar] [CrossRef]
- Xu, S.; Jiang, X.; Jia, X.; Jiang, X.; Che, L.; Lin, Y.; Zhuo, Y.; Feng, B.; Fang, Z.; Li, J.; et al. Silymarin Modulates Microbiota in the Gut to Improve the Health of Sow from Late Gestation to Lactation. Animals 2022, 12, 2202. [Google Scholar] [CrossRef]
- Wei, L.; Hou, G.; Long, C.; Chen, F.; Bai, X.; Li, R.; Yin, Y. Dietary silymarin ameliorating reproductive and lactation performance of sows via regulating body antioxidant and metabolism. Dig. Chin. Med. 2022, 5, 286–294. [Google Scholar]
- Osweiler, G.D. Occurrence of mycotoxins in grains and feeds. In Diseases of Swine, 9th ed.; Straw, B., Zimmerman, J., D’Allaire, S., Taylor, D., Eds.; Blackwell Publishing: Ames, Iowa, 2006; pp. 915–929. [Google Scholar]
- Tolosa, J.; Rodríguez-Carrasco, Y.; Ruiz, M.J.; Vila-Donat, P. Multi-mycotoxin occurrence in feed, metabolism and carry-over to animal-derived food products: A review. Food Chem. Toxicol. 2021, 158, 112661. [Google Scholar]
- Akande, K.E.; Abubakar, M.M.; Adegbola, T.A.; Bogoro, S.E. Nutritional and health implications of mycotoxins in animal feeds: A review. Pakistan J. Nutr. 2006, 5, 398–403. [Google Scholar]
- Chaytor, A.C.; See, M.T.; Hansen, J.A.; De Souza, A.L.P.; Middleton, T.F.; Kim, S.W. Effects of chronic exposure of diets with reduced concentrations of aflatoxin and deoxynivalenol on growth and immune status of pigs. J. Anim. Sci. 2011, 89, 124–135. [Google Scholar] [CrossRef] [PubMed]
- Bertero, A.; Moretti, A.; Spicer, L.J.; Caloni, F. Fusarium Molds and Mycotoxins: Potential Species-Specific Effects. Toxins 2018, 10, 244. [Google Scholar] [CrossRef] [PubMed]
- Streit, E.; Schatzmayr, G.; Tassis, P.; Tzika, E.; Marin, D.; Taranu, I.; Tabuc, C.; Nicolau, A.; Aprodu, I.; Puel, O.; et al. Current situation of mycotoxin contamination and co-occurrence in animal feed–focus on Europe. Toxins 2012, 4, 788–809. [Google Scholar] [CrossRef] [PubMed]
- Voss, K.A.; Smith, G.W.; Haschek, W.M. Fumonisins, toxicokinetics, mechanism of action and toxicity. Anim. Feed Sci. Technol. 2007, 137, 299–325. [Google Scholar] [CrossRef]
- Zinedine, A.; Soriano, J.M.; Moltó, J.C.; Mañes, J. Review on the toxicity, occurrence, metabolism, detoxification, regulations and intake of zearalenone, an oestrogenic mycotoxin. Food Chem. Toxicol. 2007, 45, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Sayyari, A.; Kruse-Fæste, C.; Hansen, U.; Uhlig, S.; Framstad, T.; Schatzmayr, D.; Sivertsen, T. Effects and biotransformation of the mycotoxin deoxynivalenol in growing pigs fed with naturally contaminated pelleted grains with and without the addition of Coriobacteriaceum DSM 11798. Food Add. Contam. 2018, 35, 1394–1409. [Google Scholar] [CrossRef]
- Holanda, D.M.; Kim, S.W. Mycotoxin Occurrence, Toxicity, and Detoxifying Agents in Pig Production with an Emphasis on Deoxynivalenol. Toxins 2021, 13, 171. [Google Scholar] [CrossRef]
- European Commission (EC). Directive 2002/32/EC of the European Parliament and of the Council of 7 May 2002 on undesirable substances in animal feed. Off. J. Eur. Union 2002, 45, 10–22. [Google Scholar]
- European Commission (EC). Commission Recommendation 2006/576/EC of 17 August 2006 on the presence of deoxynivalenol, zearalenone, ochratoxin A, T-2 and HT-2 and fumonisins in products intended for animal feeding. Off. J. Eur. Union 2006, L229, 7–9. [Google Scholar]
- Eskola, M.; Kos, G.; Elliott, C.T.; Hajšlová, J.; Mayar, S.; Krska, R. Worldwide Contamination of Food-Crops with Mycotoxins: Validity of the Widely Cited ‘FAO Estimate’ of 25%. Crit. Rev. Food Sci. Nutr. 2020, 60, 2773–2789. [Google Scholar] [CrossRef] [PubMed]
- Adhikari, M.; Negi, B.; Kaushik, N.; Adhikari, A.; Al-Khedairy, A.A.; Kaushik, N.K.; Choi, E.H. T-2 mycotoxin: Toxicological effects and decontamination strategies. Oncotarget 2017, 8, 33933–33952. [Google Scholar] [CrossRef]
- Assi, M. The differential role of reactive oxygen species in early and late stages of cancer. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2017, 313, R646–R653. [Google Scholar] [CrossRef] [PubMed]
- Mavrommatis, A.; Giamouri, E.; Tavrizelou, S.; Zacharioudaki, M.; Danezis, G.; Simitzis, P.E.; Zoidis, E.; Tsiplakou, E.; Pappas, A.C.; Georgiou, C.A.; et al. Impact of Mycotoxins on Animals’ Oxidative Status. Antioxidants 2021, 10, 214. [Google Scholar] [CrossRef] [PubMed]
- Nešić, K.; Habschied, K.; Mastanjević, K. Possibilities for the Biological Control of Mycotoxins in Food and Feed. Toxins 2021, 13, 198. [Google Scholar] [CrossRef] [PubMed]
- Kihal, A.; Rodríguez-Prado, M.; Calsamiglia, S. The efficacy of mycotoxin binders to control mycotoxins in feeds and the potential risk of interactions with nutrient: A review. J. Anim. Sci. 2022, 100, 328. [Google Scholar]
- Ledur, P.C.; Santurio, J.M. Cytoprotective effects of curcumin and silymarin on PK-15 cells exposed to ochratoxin A, fumonisin B1 and deoxynivalenol. Toxicon 2020, 185, 97–103. [Google Scholar] [CrossRef]
- Domijan, A.M.; Peraica, M.; Vrdoljak, A.L.; Radic, B.; Zlender, V.; Fuchs, R. The involvement of oxidative stress in ochratoxin A and fumonisin B-1 toxicity in rats. Mol. Nutr. Food Res. 2007, 51, 1147–1151. [Google Scholar] [CrossRef]
- Alassane, K.; Puel, I.O.; Oswald, I.P. Toxicological interactions between the mycotoxins deoxynivalenol, nivalenol and their acetylated derivatives in intestinal epithelial cells. Arch. Toxicol. 2015, 89, 1337–1346. [Google Scholar] [CrossRef]
- Riahi, I.; Ramos, A.J.; Raj, J.; Jakovčević, Z.; Farkaš, H.; Vasiljević, M.; Pérez-Vendrell, A.M. Effect of a Mycotoxin Binder (MMDA) on the Growth Performance, Blood and Carcass Characteristics of Broilers Fed Ochratoxin A and T-2 Mycotoxin Contaminated Diets. Animals 2021, 11, 3205. [Google Scholar] [CrossRef]
- Damiano, S.; Longobardi, C.; Andretta, E.; Prisco, F.; Piegari, G.; Squillacioti, C.; Montagnaro, S.; Pagnini, F.; Badino, P.; Florio, S.; et al. Antioxidative Effects of Curcumin on the Hepatotoxicity Induced by Ochratoxin A in Rats. Antioxidants 2021, 10, 125. [Google Scholar] [CrossRef]
- Yan, E.; Zhang, J.; Han, H.; Wu, J.; Gan, Z.; Wei, C. Curcumin alleviates IUGR jejunum damage by increasing antioxidant capacity through Nrf2/Keap1 pathway in growing pigs. Animals 2019, 10, 41. [Google Scholar] [CrossRef]
- Niu, Y.; He, J.; Ahmad, H.; Shen, M.; Zhao, Y.; Gan, Z. Dietary curcumin supplementation increases antioxidant capacity, upregulates Nrf2 and hmox1 levels in the liver of piglet model with intrauterine growth retardation. Nutrients 2019, 11, 2978. [Google Scholar] [CrossRef]
- Wang, F.; He, J.; Shen, M.; Hang, H.; Niu, Y.; Zhang, L. Effect of curcumin supplementation on intestinal antioxidant function in weaning piglets with intrauterine growth retardation. Food Sci. 2019, 40, 177–183. [Google Scholar]
- Tang, X.; Xiong, K.; Wassie, T.; Wu, X. Curcumin and Intestinal Oxidative Stress of Pigs With Intrauterine Growth Retardation: A Review. Front. Nutr. 2022, 9, 847673. [Google Scholar] [CrossRef]
- Liao, P.; Li, Y.; Li, M.; Chen, X.; Yuan, D.; Tang, M.; Xu, K. Baicalin alleviates deoxynivalenol-induced intestinal inflammation and oxidative stress damage by inhibiting NF-κB and increasing mTOR signaling pathways in piglets. Food Chem. Toxicol. 2020, 140, 111326. [Google Scholar] [CrossRef]
- Li, X.; Zhu, J.; Lin, Q.; Yu, M.; Lu, J.; Feng, J. Effects of curcumin on mitochondrial function, endoplasmic reticulum stress, and mitochondria-associated endoplasmic reticulum membranes in the jejunum of oxidative stress piglets. J. Agric. Food Chem. 2022, 70, 8974–8985. [Google Scholar] [CrossRef]
- Vila-Donat, P.; Marín, S.; Sanchis, V.; Ramos, A.J. A review of the mycotoxin adsorbing agents, with an emphasis on their multi-binding capacity, for animal feed decontamination. Food Chem. Toxicol. 2018, 114, 246–259. [Google Scholar] [CrossRef]
- Kim, S.W.; Brandherm, M.; Freeland, M.; Newton, B.; Cook, D.; Yoon, I. Effects of yeast culture supplementation to gestation and lactation diets on growth of nursing piglets. Asian-Aust. J. Anim. Sci. 2008, 21, 1011–1014. [Google Scholar] [CrossRef]
- Firmin, S.; Gandia, P.; Morgavi, D.P.; Houin, G.; Jouany, J.P.; Bertin, G.; Boudra, H. Modification of aflatoxin B 1 and ochratoxin A toxicokinetics in rats administered a yeast cell wall preparation. Food Addit. Contam. 2010, 27, 1153–1160. [Google Scholar] [CrossRef]
- Yiannikouris, A.; André, G.; Buléon, A.; Jeminet, G.; Canet, I.; François, J.; Bertin, G.; Jouany, J.P. Comprehensive conformational study of key interactions involved in zearalenone complexation with β-D-glucans. Biomacromolecules 2004, 5, 2176–2185. [Google Scholar] [CrossRef]
- Yiannikouris, A.; François, J.; Poughon, L.; Dussap, C.G.; Bertin, G.; Jeminet, G.; Jouany, J.P. Adsorption of zearalenone by b-D-glucans in the Saccharomyces cerevisiae cell wall. J. Food Prot. 2004, 67, 1195–1200. [Google Scholar] [CrossRef]
- Yiannikouris, A.; Francois, J.; Poughon, L.; Dussap, C.G.; Rard Bertin, G.Ä.; Jeminet, G.; Jouany, J.P. Alkali extraction of β-D-glucans from Saccharomyces cerevisiae cell wall and study of their adsorptive properties toward zearalenone. J. Agric. Food Chem. 2004, 52, 3666–3673. [Google Scholar] [CrossRef]
- Yiannikouris, A.; André, G.; Poughon, L.; François, J.; Dussap, C.G.; Jeminet, G.; Bertin, G.; Jouany, J.P. Chemical and conformational study of the interactions involved in mycotoxin complexation with β-d-glucans. Biomacromolecules 2006, 7, 1147–1155. [Google Scholar] [CrossRef]
- Yiannikouris, A.; Kettunen, H.; Apajalahti, J.; Pennala, E.; Moran, C.A. Comparison of the sequestering properties of yeast cell wall extract and hydrated sodium calcium aluminosilicate in three in vitro models accounting for the animal physiological bioavailability of zearalenone. Food Addit. Contam. 2013, 30, 1641–1650. [Google Scholar] [CrossRef]
- Dijkhuizen, A.A.; Krabbenborg, R.M.M.; Huirne, R.B.M. Sow replacement—A comparison of farmers actual decisions and model recommendations. Livest. Prod. Sci. 1989, 23, 207–218. [Google Scholar] [CrossRef]
- Niemi, J.K.; Bergman, P.; Ovaska, S.; Sevón-Aimonen, M.L.; Heinonen, M. Modeling the costs of postpartum dysgalactia syndrome and locomotory disorders on sow productivity and replacement. Front. Vet. Sci. 2017, 4, 181. [Google Scholar] [CrossRef]
- National Research Council. Nutrient Requirements of Swine, 11th ed.; The National Academies Press: Washington, DC, USA, 2012; p. 399. [Google Scholar]
- Stroka, J.; Anklam, E.; Jorissen, U.; Gilbert, J. Immunoaffinity column cleanup with liquid chromatography using post-column brominatation for determination of aflatoxins in peanut butter, pistachio paste, fig paste, and paprika powder: Collaborative study. J. AOAC Intern. 2000, 83, 320–340. [Google Scholar] [CrossRef]
- Gerasopoulos, K.; Stagos, D.; Petrotos, K.; Kokkas, S.; Kantas, D.; Goulas, P.; Kouretas, D. Feed supplemented with polyphenolic byproduct from olive mill wastewater processing improves the redox status in blood and tissues of piglets. Food Chem. Toxicol. 2015, 86, 319–327. [Google Scholar] [CrossRef]
- Keles, M.S.; Taysi, S.; Sen, N.; Aksoy, H.; Akçay, F. Effect of corticosteroid therapy on serum and CSF malondialdehyde and antioxidant proteins in multiple sclerosis. Can. J. Neurol. Sci. 2001, 28, 141–143. [Google Scholar] [CrossRef]
- Patsoukis, N.; Zervoudakis, G.; Panagopoulos, N.T.; Georgiou, C.D.; Angelatou, F.; Matsokis, N.A. Thiol redox state (TRS) and oxidative stress in the mouse hippocampus after pentylenetetrazol-induced epileptic seizure. Neurosci. Lett. 2004, 357, 83–86. [Google Scholar] [CrossRef] [PubMed]
- Janaszewska, A.; Bartosz, G. Assay of total antioxidant capacity: Comparison of four methods as applied to human blood plasma. Scand. J. Clin. Lab. Investig. 2002, 62, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, F. Vergleichende Infrarotthermographische und Bakteriologische Untersuchungen am Gesunden Sowie Durch Mastitis Veränderten Gesäuge Beim Schwein. Ph.D. Thesis, Tierärztliche Hochschule Hannover, Hannover, Germany, 2016. [Google Scholar]
- Rosengart, S.; Chuppava, B.; Schubert, D.C.; Trost, L.-S.; Henne, H.; Tetens, J.; Traulsen, I.; Deermann, A.; Visscher, C.; Wendt, M. Infrared Thermography of the Mammary Gland in Sows with Regard to Health and Performance. Agriculture 2021, 11, 1013. [Google Scholar] [CrossRef]
- Viñuela-Fernández, I.; Jones, E.; Welsh, E.M.; Fleetwood-Walker, S.M. Pain mechanisms and their implication for the management of pain in farm and companion animals. Vet. J. 2007, 174, 227–239. [Google Scholar] [CrossRef] [PubMed]
- Navarro, E.; Mainau, E.; Manteca, X. Development of a Facial Expression Scale Using Farrowing as a Model of Pain in Sows. Animals 2020, 10, 2113. [Google Scholar] [CrossRef] [PubMed]
| Detected Mycotoxin (ppb) | Farm-1 | Farm-2 | Maximum Level (ppb) According to EU Regulation * |
|---|---|---|---|
| Total FUBs | 3468.0 | 6489.5 | (FUB1 + FUB2) 5000 |
| FUB1 | 2767.5 | 5109.4 | |
| FUB2 | 700.5 | 1380.1 | |
| ZEN | 14.6 | - | 100 |
| AFB1 | - | 5.1 | 20 |
| T2 toxin | 4.2 | - | 250 |
| Clinical guide to mycotoxins affecting sows [61] | |||
| Mycotoxin | Dietary level (ppb or ppm) 1 ppm = 1000 ppb | Effects | |
| AFs | >2000 ppb | acute hepatosis, high mortality rate | |
| 400 to 800 ppb | slow-growing suckling pigs due to aflatoxin in milk | ||
| ZEN | 1–3 ppm | vulvovaginitis, prolapses of rectum and vagina | |
| 3–10 ppm | anestrus, pseudopregnancy | ||
| >30 ppm | early embryo loss | ||
| T2 toxin | 3 ppm | low feed intake | |
| 10 ppm | low feed intake; oral/dermal irritation; immune-suppression | ||
| 20 ppm | Anorexia, vomiting | ||
| FU Bs | <20 ppm | No signs | |
| 50 to 100 ppm | decreased feed intake, decreased weight gain, hepatosis | ||
| >100 ppm | Acute pulmonary edema, hepatosis, and death | ||
| Parameters | Farm-1 | Farm-2 | ||||
|---|---|---|---|---|---|---|
| Groups | Groups | |||||
| T1 | T2 | p Value | T1 | T2 | p Value | |
| TBARS | 5.61 ± 0.96 a | 3.83 ± 0.70 b | 0.009 | 7.78 ± 0.67 a | 4.97 ± 1.04 b | <0.001 |
| CARB | 0.73 ± 0.07 a | 0.47 ± 0.11 b | <0.001 | 0.79 ± 0.07 a | 0.51 ± 0.06 b | <0.001 |
| TAC | 0.46 ± 0.01 b | 0.80 ± 0.02 a | <0.001 | 0.31 ± 0.03 b | 0.72 ± 0.02 a | 0.007 |
| Parameters | Farm-1 | Farm-2 | ||||
|---|---|---|---|---|---|---|
| T1 Group (n = 40) | T2 Group (n = 40) | p Value | T1 Group (n = 40) | T2 Group (n = 40) | p Value | |
| Temperature −24 h (0 = normal, up to 40 °C, 1 => 41 °C 2 => 42 °C) | 1.25 ± 0.68 a | 0.23 ± 0.42 b | <0.001 | 1.27 ± 0.71 a | 0.29 ± 0.56 b | <0.001 |
| Mammary glands | ||||||
| Shaping/Regression (0 = in lactation, 1 = poor shape/regression, 2 = not shaped/no milk production) | 1.25 ± 0.68 a | 0.27 ± 0.45 b | <0.001 | 1.31 ± 0.82 a | 0.27 ± 0.45 b | <0.001 |
| Skin color (0 = normal skin color, 1 = moderately red, 2 = severely red) | 1.25 ± 0.71 a | 0.35 ± 0.48 b | <0.001 | 1.33 ± 0.79 a | 0.47 ± 0.56 b | <0.001 |
| Consistency (0 = loose, 1 = elastic, 2 = firm) | 1.10 ± 0.38 a | 0.30 ± 0.48 b | <0.001 | 1.32 ± 0.63 a | 0.37 ± 0.67 b | <0.001 |
| Nodes (0 = absent, 1 = present in skin/subcutis, 2 = present in breast parenchyma) | 0.67 ± 0.47 a | 0.28 ± 0.45 b | <0.001 | 0.72 ± 0.56 a | 0.33 ± 0.52 b | <0.001 |
| Pain (0 = absent,1 = mild, 2 = severe) | 1.33 ± 0.73 a | 0.35 ± 0.48 b | <0.001 | 1.46 ± 0.95 a | 0.55 ± 0.64 b | <0.001 |
| Parameters | Farm-1 | Farm-2 | ||||
|---|---|---|---|---|---|---|
| T1 Group (n = 40) | T2 Group (n = 40) | p Value | T1 Group (n = 40) | T2 Group (n = 40) | p Value | |
| Total Born | 15.78 ± 1.58 a | 15.75 ± 1.49 a | 0.926 | 15.62 ± 1.24 a | 15.65 ± 1.32 a | 0.875 |
| Dead Born | 1.38± 0.74 a | 0.78 ± 0.48 b | <0.001 | 1.76± 0.89 a | 0.87 ± 0.52 b | <0.001 |
| Live Born | 13.08 ± 0.99 a | 14.43 ± 1.19 b | <0.001 | 12.28 ± 0.92 a | 14.38 ± 1.19 b | <0.001 |
| Mummies | 1.35 ± 0.69 a | 0.55 ± 0.50 b | <0.001 | 1.65 ± 0.78 a | 0.42 ± 0.39 b | <0.001 |
| Fostering taking | 0.48 ± 0.82 a | 0.18 ± 0.45 b | 0.045 | 0.32 ± 0.82 a | 0.16 ± 0.34 b | 0.055 |
| Fostering giving | 1.40 ± 0.98 a | 0.78 ± 0.62 b | 0.002 | 1.54 ± 0.97 a | 0.62 ± 0.53 b | 0.003 |
| Weaned | 10.93 ± 1.89 a | 13.28 ± 0.72 b | <0.001 | 10.08 ± 1.65 a | 13.56 ± 0.87 b | <0.001 |
| Composition of Ingredients (kg) | Trial Farm-1 | Trial Farm-2 | ||
|---|---|---|---|---|
| GF | LF | GF | LF | |
| Corn | 300.0 | 345.0 | 300.0 | 328.0 |
| Barley | 280.0 | 200.0 | 470.0 | 400.0 |
| Wheat bran | 235.0 | 190.0 | - | - |
| Soybean meal (46% crude protein) | 120.0 | 170.0 | 72.5 | 148 |
| Sunflower (28% crude protein) | - | - | 75.0 | 25.0 |
| Sugar beet | - | - | 50 | 25.0 |
| Soybean oil | 10.0 | 20.0 | - | 18.0 |
| Protein concentrate (68% crude protein) | 14.0 | 24.0 | ||
| Fish meal | - | - | 25.0 | |
| Vitamins/minerals premix | 30.0 | 40.0 | 30.0 | 30.0 |
| Inactive dried yeast | 5.0 | 5.0 | - | - |
| Mycotoxin binder | 1.5 | 1.5 | 2.5 | 1.0 |
| Dietary cellulose powder | 4.5 | 4.5 | - | - |
| Total | 1000 | 1000 | 1000 | 1000 |
| Analyzed nutrient compositions (%) | GF | LF | GF | LF |
| Crude protein | 16.50 | 18.40 | 13.63 | 16.92 |
| Crude fat | 3.70 | 4.65 | 2.14 | 4.06 |
| Crude fiber | 5.40 | 4.70 | 6.32 | 4.53 |
| Lysine | 0.80 | 0.98 | 0.6 | 1.04 |
| Methionine | 0.29 | 0.33 | 0.20 | 0.35 |
| Methionine + Cystine | 0.60 | 0.63 | 0.80 | 0.60 |
| Calcium | 0.65 | 0.86 | 0.95 | 0.98 |
| Total phosphorus/available phosphorus | 0.76/0.40 | 0.78/0.46 | 0.65/0.35 | 0.67/0.38 |
| Sodium | 0.24 | 0.24 | 0.24 | 0.24 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Papatsiros, V.G.; Eliopoulos, C.; Voulgarakis, N.; Arapoglou, D.; Riahi, I.; Sadurní, M.; Papakonstantinou, G.I. Effects of a Multi-Component Mycotoxin-Detoxifying Agent on Oxidative Stress, Health and Performance of Sows. Toxins 2023, 15, 580. https://doi.org/10.3390/toxins15090580
Papatsiros VG, Eliopoulos C, Voulgarakis N, Arapoglou D, Riahi I, Sadurní M, Papakonstantinou GI. Effects of a Multi-Component Mycotoxin-Detoxifying Agent on Oxidative Stress, Health and Performance of Sows. Toxins. 2023; 15(9):580. https://doi.org/10.3390/toxins15090580
Chicago/Turabian StylePapatsiros, Vasileios G., Christos Eliopoulos, Nikolaos Voulgarakis, Dimitrios Arapoglou, Insaf Riahi, Meritxell Sadurní, and Georgios I. Papakonstantinou. 2023. "Effects of a Multi-Component Mycotoxin-Detoxifying Agent on Oxidative Stress, Health and Performance of Sows" Toxins 15, no. 9: 580. https://doi.org/10.3390/toxins15090580