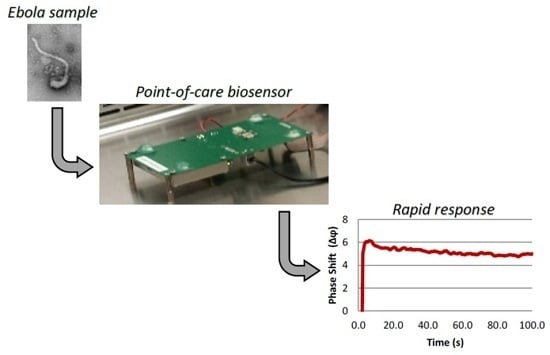
Rapid Detection of Ebola Virus with a Reagent-Free, Point-of-Care Biosensor
Abstract
:1. Introduction
2. Experimental Section
2.1. Fabrication and Functionalization of the SAW Biosensor
2.2. Provenance and Handling of Ebola Virus Strain Zaire (Mayinga) Inactivated
2.3. Virus Detection Using the SAW Biosensor
3. Results and Discussion
3.1. Design Elements of Surface Acoustic Wave Biosensor

3.2. Imaging Analysis of the Ebola Zaire Antigen Sample

3.3. SAW Biosensor Detection of the Ebola Zaire Sample


4. Conclusions/Outlook
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Frieden, T.R.; Damon, I.; Bell, B.P.; Kenyon, T.; Nichol, S. Ebola 2014—New challenges, new global response and responsibility. N. Engl. J. Med. 2014, 371, 1177–1180. [Google Scholar] [CrossRef] [PubMed]
- Hampton, T. Largest-ever outbreak of Ebola Virus disease thrusts experimental therapies, vaccines into spotlight. JAMA 2014, 312, 987–989. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization, What This—The largest Ebola Outbreak in History—Tells the World. Available online: http://www.who.int/csr/disease/ebola/ebola-6-months/lessons/en/ (accessed on 23 March 2015).
- Centers for Disease Control and Prevention, Ebola Outbreaks 2000–2014. Available online: http://www.cdc.gov/vhf/ebola/outbreaks/history/summaries.html (accessed on 23 March 2015).
- World Health Organization, Urgently Needed: Rapid, Sensitive, Safe and Simple Ebola Diagnostic Tests. Available online: http://www.who.int/mediacentre/news/ebola/18-november-2014-diagnostics/en/ (accessed on 23 March 2015).
- Chertow, D.S.; Kleine, C.; Edwards, J.K.; Scaini, R.; Giuliani, R.; Sprecher, A. Ebola Virus Disease in West Africa—Clinical manifestations and management. N. Engl. J. Med. 2014, 371, 2054–2057. [Google Scholar] [CrossRef] [PubMed]
- MacNeil, A.; Rollin, P.E. Ebola and Marburg hemorrhagic fevers: Neglected tropical diseases? PLoS Negl. Trop. Dis. 2012, 6, e1546. [Google Scholar] [CrossRef] [PubMed]
- Tseng, C.P.; Chan, Y.J. Overview of Ebola virus disease in 2014. J. Chin. Med. Assoc. 2015, 78, 51–55. [Google Scholar] [CrossRef] [PubMed]
- WHO Ebola Response Team. Ebola virus disease in West Africa—The first 9 months of the epidemic and forward projections. N. Engl. J. Med. 2014, 16, 1481–1495. [Google Scholar]
- Bartsch, S.M.; Gorham, K.; Lee, B.Y. The cost of an Ebola case. Pathog. Glob. Health 2015, 109, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Schieffelin, J.S.; Shaffer, J.G.; Goba, A.; Gbakie, M.; Gire, S.K.; Colubri, A.; Sealfon, R.S.; Kanneh, L; Moigboi, A.; Momoh, M.; et al. Clinical illness and outcomes in patients with Ebola in Sierra Leone. N. Engl. J. Med. 2014, 371, 2092–2100. [Google Scholar] [CrossRef] [PubMed]
- Bisoffi, M.; Hjelle, B.; Brown, D.C.; Branch, D.W.; Edwards, T.L.; Brozik, S.M.; Bondu-Hawkins, V.S.; Larson, R.S. Detection of viral bioagents using a shear horizontal surface acoustic wave biosensor. Biosens. Bioelectron. 2008, 23, 1397–1403. [Google Scholar] [CrossRef] [PubMed]
- Branch, D.W.; Brozik, S.M. Low-level detection of a bacillus anthracis simulant using Love-wave biosensors on 36 degrees YX LiTaO3. Biosens. Bioelectron. 2004, 19, 849–859. [Google Scholar] [CrossRef] [PubMed]
- Larson, R.S.; Baca, J.T. Versatility of the surface acoustic wave biosensor platform for detecting bacteria and viruses. In Global Point of Care: Strategies for Disasters, Emergencies, and Public Health Resilience; Kost, G.J., Curtis, C.M., Eds.; AACC Press: Washington, DC, USA, 2015; pp. 165–172. [Google Scholar]
- Gronewold, T.M. Surface acoustic wave sensors in the bioanalytical field: recent trends and challenges. Anal. Chim. Acta 2007, 603, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Bisoffi, M.; Severns, V.; Branch, D.W.; Edwards, T.L.; Larson, R.L. Rapid detection of human immunodeficiency virus types 1 and 2 by use of an improved piezoelectric biosensor. J. Clin. Microbiol. 2013, 51, 1685–1691. [Google Scholar] [CrossRef] [PubMed]
- Bente, D.; Gren, J.; Strong, J.E.; Feldmann, H. Disease modeling for Ebola and Marburg viruses. Dis. Model. Mech. 2009, 2, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Geisbert, T.W.; Jahrling, P.B. Use of immunoelectron microscopy to show Ebola virus during the 1989 United States epizootic. J. Clin. Pathol. 1990, 43, 813–816. [Google Scholar] [CrossRef] [PubMed]
- Gentile, M.; Adrian, T.; Scheidler, A.; Ewald, M.; Dianzani, F.; Pauli, G.; Gelderblom, H.R. Determination of the size of HIV using adenovirus type 2 as an internal length marker. J. Virol. Methods 1994, 48, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Towner, J.S.; Rollin, P.E.; Bausch, D.G.; Sanchez, A.; Crary, S.M.; Vincent, M.; Lee, W.F.; Spiropoulou, C.F.; Ksiazek, T.G.; Lukwiya, M.; et al. Rapid diagnosis of Ebola hemorrhagic fever by reverse transcription-PCR in an outbreak setting and assessment of patient viral load as a predictor of outcome. J. Virol. 2004, 78, 4330–4341. [Google Scholar] [CrossRef] [PubMed]
- Rossi, C.A.; Kearney, B.J.; Olschner, S.P.; Williams, P.L.; Robinson, C.G.; Heinrich, M.L.; Zovanyi, A.M.; Ingram, M.F.; Norwood, D.A.; Schoepp, R.J. Evaluation of ViroCyt® Virus Counter for Rapid Filovirus Quantitation. Viruses 2015, 7, 857–872. [Google Scholar] [CrossRef] [PubMed]
- Bisoffi, M.; Severns, V.; Larson, R. CTSA-enhanced innovative device development. Clin. Transl. Sci. 2012, 5, 311–313. [Google Scholar] [CrossRef] [PubMed]
- Beeching, N.J.; Fenech, M.; Houlihan, C.F. Ebola virus disease. BMJ. 2014, 349, p. g7348. Available online: http://www.bmj.com/content/349/bmj.g7348 (accessed on 23 March 2015). [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baca, J.T.; Severns, V.; Lovato, D.; Branch, D.W.; Larson, R.S. Rapid Detection of Ebola Virus with a Reagent-Free, Point-of-Care Biosensor. Sensors 2015, 15, 8605-8614. https://doi.org/10.3390/s150408605
Baca JT, Severns V, Lovato D, Branch DW, Larson RS. Rapid Detection of Ebola Virus with a Reagent-Free, Point-of-Care Biosensor. Sensors. 2015; 15(4):8605-8614. https://doi.org/10.3390/s150408605
Chicago/Turabian StyleBaca, Justin T., Virginia Severns, Debbie Lovato, Darren W. Branch, and Richard S. Larson. 2015. "Rapid Detection of Ebola Virus with a Reagent-Free, Point-of-Care Biosensor" Sensors 15, no. 4: 8605-8614. https://doi.org/10.3390/s150408605