Towards a Whole Sample Imaging Approach Using Diffusion Tensor Imaging to Examine the Foreign Body Response to Explanted Medical Devices
Abstract
:1. Introduction
2. Materials and Methods
2.1. Device Fabrication & Animal Study
2.2. MR Imaging and Analysis
2.3. Tissue Processing and Histology
2.4. Scanning Electron Microscopy (SEM)
2.5. MicroCT
2.6. Statistical Methods
3. Results
3.1. In Vivo Implantation of Macroencapsulation Devices
3.2. Multi-Contrast MRI
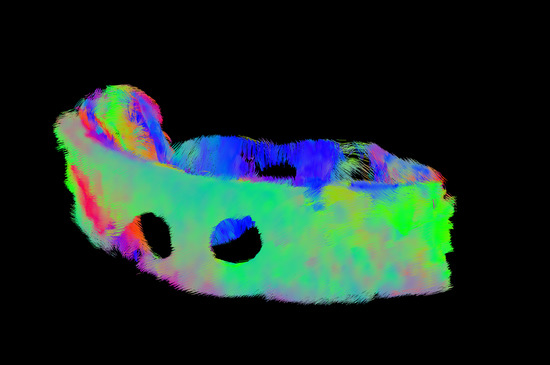
3.3. DTI Metrics
3.4. MicroCT & SEM Imaging
3.5. Histological Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| DTI | Diffusion tensor imaging |
| ERC | European research council |
| FA | Fractional anisotropy |
| FBR | Foreign body response |
| FEFA | First eigenvector-fractional anisotropy |
| MD | Mean diffusivity |
| MicroCT | Micro computed tomography |
| MRI | Magnetic resonance imaging |
| PLM | Polarized light Microscopy |
| SEM | Scanning electron microscopy |
| TPU | Thermoplastic polyurethane |
References
- Anderson, J.M. Inflammatory Response to Implants. ASAIO Trans. 1988, 34, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.M.; Rodriguez, A.; Chang, D.T. Foreign Body Reponse to Biomaterials. Semin. Immunol. 2008, 20, 86–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wynn, T.A.; Ramalingam, T.R. Mechanisms of Fibrosis: Therapeutic Translation for Fibrotic Disease. Nat. Med. 2012, 18, 1028–1040. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duffy, G.P.; Robinson, S.T.; O’Connor, R.; Wylie, R.; Mauerhofer, C.; Bellavia, G.; Straino, S.; Cianfarani, F.; Mendez, K.; Beatty, R.; et al. Implantable Therapeutic Reservoir Systems for Diverse Clinical Applications in Large Animal Models. Adv. Healthc. Mater. 2020, 9, 2000305. [Google Scholar] [CrossRef]
- Coulter, F.B.; Levey, R.E.; Robinson, S.T.; Dolan, E.B.; Deotti, S.; Monaghan, M.; Dockery, P.; Coulter, B.S.; Burke, L.P.; Lowery, A.J.; et al. Additive Manufacturing of Multi-Scale Porous Soft Tissue Implants That Encourage Vascularization and Tissue Ingrowth. Adv. Healthc. Mater. 2021, 10, 2100229. [Google Scholar] [CrossRef]
- Kaufmann, B.A.; Sanders, J.M.; Davis, C.; Xie, A.; Aldred, P.; Sarembock, I.J.; Lindner, J.R. Molecular Imaging of Inflammation in Atherosclerosis with Targeted Ultrasound Detection of Vascular Cell Adhesion Molecule-1. Circulation 2007, 116, 276–284. [Google Scholar] [CrossRef] [Green Version]
- Breckwoldt, M.O.; Chen, J.W.; Stangenberg, L.; Aikawa, E.; Rodriguez, E.; Qiu, S.; Moskowitz, M.A.; Weissleder, R. Tracking the Inflammatory Response in Stroke in Vivo by Sensing the Enzyme Myeloperoxidase. Proc. Natl. Acad. Sci. USA 2008, 105, 18584–18589. [Google Scholar] [CrossRef] [Green Version]
- Selvam, S.; Kundu, K.; Templeman, K.L.; Murthy, N.; García, A.J. Minimally Invasive, Longitudinal Monitoring of Biomaterial-Associated Inflammation by Fluorescence Imaging. Biomaterials 2011, 32, 7785–7792. [Google Scholar] [CrossRef] [Green Version]
- Jones, D.K. (Ed.) Diffusion MRI: Theory, Methods, and Applications; Illustrated edition; Oxford University Press: Oxford UK, 2011. [Google Scholar]
- Raya, J.G.; Melkus, G.; Adam-Neumair, S.; Dietrich, O.; Mützel, E.; Reiser, M.F.; Putz, R.; Kirsch, T.; Jakob, P.M.; Glaser, C. Diffusion-Tensor Imaging of Human Articular Cartilage Specimens with Early Signs of Cartilage Damage. Radiology 2013, 266, 831–841. [Google Scholar] [CrossRef] [Green Version]
- Akyildiz, A.C.; Chai, C.-K.; Oomens, C.W.J.; van der Lugt, A.; Baaijens, F.P.T.; Strijkers, G.J.; Gijsen, F.J.H. 3D Fiber Orientation in Atherosclerotic Carotid Plaques. J. Struct. Biol. 2017, 200, 28–35. [Google Scholar] [CrossRef]
- Carruth, E.D.; Teh, I.; Schneider, J.E.; McCulloch, A.D.; Omens, J.H.; Frank, L.R. Regional Variations in Ex-Vivo Diffusion Tensor Anisotropy Are Associated with Cardiomyocyte Remodeling in Rats after Left Ventricular Pressure Overload. J. Cardiovasc. Magn. Reson. 2020, 22, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tornifoglio, B.; Stone, A.J.; Johnston, R.D.; Shahid, S.S.; Kerskens, C.; Lally, C. Diffusion Tensor Imaging and Arterial Tissue: Establishing the Influence of Arterial Tissue Microstructure on Fractional Anisotropy, Mean Diffusivity and Tractography. Sci. Rep. 2020, 10, 20718. [Google Scholar] [CrossRef] [PubMed]
- Raya, J.G.; Horng, A.; Dietrich, O.; Krasnokutsky, S.; Beltran, L.S.; Storey, P.; Reiser, M.F.; Recht, M.P.; Sodickson, D.K.; Glaser, C. Articular Cartilage: In Vivo Diffusion-Tensor Imaging. Radiology 2012, 262, 550–559. [Google Scholar] [CrossRef] [PubMed]
- Andersson, G.; Orädd, G.; Sultan, F.; Novikov, L.N. In Vivo Diffusion Tensor Imaging, Diffusion Kurtosis Imaging, and Tractography of a Sciatic Nerve Injury Model in Rat at 9.4T. Sci. Rep. 2018, 8, 12911. [Google Scholar] [CrossRef]
- Stoeck, C.T.; von Deuster, C.; Fuetterer, M.; Polacin, M.; Waschkies, C.F.; van Gorkum, R.J.H.; Kron, M.; Fleischmann, T.; Cesarovic, N.; Weisskopf, M.; et al. Cardiovascular Magnetic Resonance Imaging of Functional and Microstructural Changes of the Heart in a Longitudinal Pig Model of Acute to Chronic Myocardial Infarction. J. Cardiovasc. Magn. Reson. Off. J. Soc. Cardiovasc. Magn. Reson. 2021, 23, 103. [Google Scholar] [CrossRef]
- Mekkaoui, C.; Jackowski, M.P.; Kostis, W.J.; Stoeck, C.T.; Thiagalingam, A.; Reese, T.G.; Reddy, V.Y.; Ruskin, J.N.; Kozerke, S.; Sosnovik, D.E. Myocardial Scar Delineation Using Diffusion Tensor Magnetic Resonance Tractography. J. Am. Heart Assoc. 2018, 7, e007834. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, W.; Chen, J. Diffusion Tensor Imaging (DTI) of the Cesarean-Scarred Uterus in Vivo at 3T: Comparison Study of DTI Parameters Between Nonpregnant and Pregnant Cases. J. Magn. Reson. Imaging JMRI 2020, 51, 124–130. [Google Scholar] [CrossRef] [PubMed]
- De Faria Castro Fleury, E.; Gianini, A.C.; Ayres, V.; Ramalho, L.C.; Seleti, R.O.; Roveda, D. Breast Magnetic Resonance Imaging: Tips for the Diagnosis of Silicone-Induced Granuloma of a Breast Implant Capsule (SIGBIC). Insights Imaging 2017, 8, 439–446. [Google Scholar] [CrossRef]
- Dolan, E.B.; Varela, C.E.; Mendez, K.; Whyte, W.; Levey, R.E.; Robinson, S.T.; Maye, E.; O’Dwyer, J.; Beatty, R.; Rothman, A.; et al. An Actuatable Soft Reservoir Modulates Host Foreign Body Response. Sci. Robot. 2019, 4, eaax7043. [Google Scholar] [CrossRef] [Green Version]
- Dolan, E.B.; Hofmann, B.; de Vaal, M.H.; Bellavia, G.; Straino, S.; Kovarova, L.; Pravda, M.; Velebny, V.; Daro, D.; Braun, N.; et al. A Bioresorbable Biomaterial Carrier and Passive Stabilization Device to Improve Heart Function Post-Myocardial Infarction. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 103, 109751. [Google Scholar] [CrossRef]
- Monaghan, M.G.; Holeiter, M.; Brauchle, E.; Layland, S.L.; Lu, Y.; Deb, A.; Pandit, A.; Nsair, A.; Schenke-Layland, K. Exogenous MiR-29B Delivery Through a Hyaluronan-Based Injectable System Yields Functional Maintenance of the Infarcted Myocardium. Tissue Eng. Part A 2018, 24, 57–67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rolfe, B.; Mooney, J.; Zhang, B.; Jahnke, S.; Le, S.-J.; Chau, Y.-Q.; Huang, Q.; Wang, H.; Campbell, G.; Campbell, J.; et al. The Fibrotic Response to Implanted Biomaterials: Implications for Tissue Engineering; IntechOpen: London, UK, 2011; ISBN 978-953-307-663-8. [Google Scholar]
- Gopinathan, P.A.; Kokila, G.; Siddeeqh, S.; Prakash, R.; L, P. Reexploring Picrosirius Red: A Review. Indian J. Pathol. Oncol. 2020, 7, 196–203. [Google Scholar] [CrossRef]
- Koren, R.; Yaniv, E.; Kristt, D.; Shvero, J.; Veltman, V.; Grushko, I.; Feinmesser, R.; Sulkes, J.; Gal, R. Capsular Collagen Staining of Follicular Thyroid Neoplasms by Picrosirius Red: Role in Differential Diagnosis. Acta Histochem. 2001, 103, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.; Tanna, N.; Margolies, L. Magnetic Resonance Imaging of Breast Implants. Top. Magn. Reson. Imaging TMRI 2014, 23, 345–353. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.T.; Jankharia, B.B. Imaging of Common Breast Implants and Implant-Related Complications: A Pictorial Essay. Indian J. Radiol. Imaging 2016, 26, 216–225. [Google Scholar] [CrossRef]






Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Levey, R.E.; Tornifoglio, B.; Stone, A.J.; Kerskens, C.; Robinson, S.T.; Coulter, F.B.; Bagnall, R.; O’Connor, R.; Dolan, E.B.; Dockery, P.; et al. Towards a Whole Sample Imaging Approach Using Diffusion Tensor Imaging to Examine the Foreign Body Response to Explanted Medical Devices. Polymers 2022, 14, 4819. https://doi.org/10.3390/polym14224819
Levey RE, Tornifoglio B, Stone AJ, Kerskens C, Robinson ST, Coulter FB, Bagnall R, O’Connor R, Dolan EB, Dockery P, et al. Towards a Whole Sample Imaging Approach Using Diffusion Tensor Imaging to Examine the Foreign Body Response to Explanted Medical Devices. Polymers. 2022; 14(22):4819. https://doi.org/10.3390/polym14224819
Chicago/Turabian StyleLevey, Ruth E., Brooke Tornifoglio, Alan J. Stone, Christian Kerskens, Scott T. Robinson, Fergal B. Coulter, Robert Bagnall, Raymond O’Connor, Eimear B. Dolan, Peter Dockery, and et al. 2022. "Towards a Whole Sample Imaging Approach Using Diffusion Tensor Imaging to Examine the Foreign Body Response to Explanted Medical Devices" Polymers 14, no. 22: 4819. https://doi.org/10.3390/polym14224819