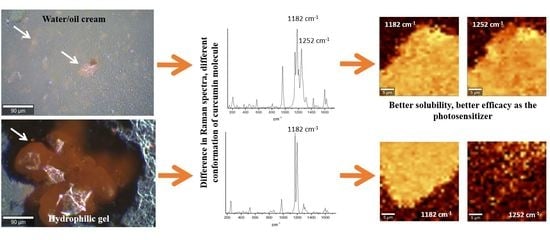
Raman Microspectroscopy as a Tool to Elucidate the Efficacy of Topical Formulations Containing Curcumin
Abstract
:1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Raman Microspectroscopy
4.3. Fluorescence Lifetime Imaging Microscopy
4.4. Photodynamic Therapy
Author Contributions
Funding
Conflicts of Interest
References
- Gupta, A.K.; Jain, H.C.; Lynde, C.W.; MacDonald, P.; Cooper, E.A.; Summerbell, R.C. Prevalence and epidemiology of onychomycosis in patients visiting physicians’ offices: A multicenter Canadian survey of 15,000 patients. J. Am. Acad. Dermatol. 2000, 43, 244–248. [Google Scholar] [CrossRef] [PubMed]
- Albert, S.F.; Weis, Z.H. Management of onychomycosis with topicals. Clin. Podiatr. Med. Surg. 2004, 21, 605–615. [Google Scholar] [CrossRef] [PubMed]
- Martins, E.A.; Guerrer, L.V.; Cunha, K.C.; Soares, M.M.C.N.; de Almeida, M.T.G. Onychomycosis: Clinical, epidemiological and mycological study in the municipality of São José do Rio Preto. Rev. Soc. Bras. Med. Trop. 2007, 40, 596–598. [Google Scholar] [CrossRef] [PubMed]
- Naumann, S.; Meyer, J.P.; Kiesow, A.; Mrestani, Y.; Wohlrab, J.; Neubert, R.H.H. Controlled nail delivery of a novel lipophilic antifungal agent using various modern drug carrier systems as well as in vitro and ex vivo model systems. J. Control. Release 2014, 180, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Van Laborde, S.; Scher, R.K. Developments in the treatment of nail psoriasis, melanonychia striata, and onychomycosis. A review of the literature. Dermatol. Clin. 2000, 18, 37–46. [Google Scholar] [CrossRef]
- Lim, E.H.; Kim, H.R.; Park, Y.O.; Lee, Y.; Seo, Y.J.; Kim, C.D.; Lee, J.H.; Im, M. Toenail onychomycosis treated with a fractional carbon-dioxide laser and topical antifungal cream. J. Am. Acad. Dermatol. 2014, 70, 918–923. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, A.P.; Carbinatto, F.M.; Bagnato, V.S.; Inada, N.M. New strategies for treatment of onychomycosis. Photodiagnosis Photodyn. Ther. 2015, 12, 325. [Google Scholar] [CrossRef]
- Da Silva, A.P.; Chiandrone, D.J.; Tinta, J.W.R.; Kurachi, C.; Inada, N.M.; Bagnato, V.S. Development and comparison of two devices for treatment of onychomycosis by photodynamic therapy. J. Biomed. Opt. 2015, 20, 61109. [Google Scholar] [CrossRef] [PubMed]
- Ledon, J.A.; Savas, J.; Franca, K.; Chacon, A.; Nouri, K. Laser and light therapy for onychomycosis: A systematic review. Lasers Med. Sci. 2014, 29, 823–829. [Google Scholar] [CrossRef] [PubMed]
- Paula Da Silva, A.; Carbinatto, F.M.; Bagnato, V.S.; Inada, N.M. A Promising Strategy for the Treatment of Onychomycosis with Curcumin and Photodynamic Therapy. J. Pharm. Pharmacol. 2015, 3, 434–437. [Google Scholar] [CrossRef]
- Silva, A.P.d.; Kurachi, C.; Bagnato, V.S.; Inada, N.M. Fast elimination of onychomycosis by hematoporphyrin derivative-photodynamic therapy. Photodiagnosis Photodyn. Ther. 2013, 10, 328–330. [Google Scholar] [CrossRef]
- Sotiriou, E.; Koussidou-Ermonti, T.; Chaidemenos, G.; Apalla, Z.; Ioannides, D. Photodynamic therapy for distal and lateral subungual toenail onychomycosis caused by Trichophyton rubrum: Preliminary results of a single-centre open trial. Acta Derm. Venereol. 2010, 90, 216–217. [Google Scholar] [CrossRef] [PubMed]
- Sharman, W.M.; Allen, C.M.; van Lier, J.E. Photodynamic therapeutics: Basic principles and clinical applications. Drug Discov. Today 1999, 4, 507–517. [Google Scholar] [CrossRef]
- Leite, I.S.; Geralde, M.C.; Salina, A.C.G.; Medeiros, A.I.; Dovigo, L.N.; Bagnato, V.S.; Inada, N.M. Near–infrared photodynamic inactivation of S. pneumoniae and its interaction with RAW 264.7 macrophages. J. Biophotonics 2018, 11. [Google Scholar] [CrossRef] [PubMed]
- Pavarina, A.C.; Ribeiro, A.P.D.; Dovigo, L.N.; de Andrade, C.R.; de Souza Costa, C.A.; Vergani, C.E. Photodynamic Therapy to Eradicate Tumor Cells. In Cell Metabolism; Bubulya, P., Ed.; IntechOpen Limited: London, UK, 2011; p. 149. [Google Scholar]
- Kessel, D. Adventures in photodynamic therapy: 1976–2008. J. Porphyr. Phthalocyanines 2008, 12, 877–880. [Google Scholar] [CrossRef] [PubMed]
- Agostinis, P.; Berg, K.; Cengel, K.A.; Foster, T.H.; Girotti, A.W.; Gollnick, S.O.; Hahn, S.M.; Hamblin, M.R.; Juzeniene, A.; Kessel, D.; et al. Photodynamic therapy of cancer: An update. CA Cancer J. Clin. 2011, 61, 250–281. [Google Scholar] [CrossRef]
- Ramirez, D.P.; Kurachi, C.; Inada, N.M.; Moriyama, L.T.; Salvio, A.G.; Vollet Filho, J.D.; Pires, L.; Buzzá, H.H.; de Andrade, C.T.; Greco, C.; et al. Experience and BCC subtypes as determinants of MAL-PDT response: Preliminary results of a national Brazilian project. Photodiagnosis Photodyn. Ther. 2014, 11, 22–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Geralde, M.C.; Leite, I.S.; Inada, N.M.; Salina, A.C.G.; Medeiros, A.I.; Kuebler, W.M.; Kurachi, C.; Bagnato, V.S. Pneumonia treatment by photodynamic therapy with extracorporeal illumination—An experimental model. Physiol. Rep. 2017, 5, e13190. [Google Scholar] [CrossRef] [PubMed]
- Stritt, A.; Merk, H.F.; Braathen, L.R.; Von Felbert, V. Photodynamic therapy in the treatment of actinic keratosis. Photochem. Photobiol. 2008, 84, 388–398. [Google Scholar] [CrossRef] [PubMed]
- Inada, N.M.; da Costa, M.M.; Guimarães, O.C.C.; da Silva Ribeiro, E.; Kurachi, C.; Quintana, S.M.; Lombardi, W.; Bagnato, V.S. Photodiagnosis and treatment of condyloma acuminatum using 5-aminolevulinic acid and homemade devices. Photodiagnosis Photodyn. Ther. 2012, 9, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Inada, N.M.; Lombardi, W.; Leite, M.F.M.; Trujillo, J.R.; Kurachi, C.; Bagnato, V.S. Photodynamic therapy of cervical intraepithelial neoplasia. In Proceedings of the Optical Methods for Tumor Treatment and Detection: Mechanisms and Techniques in Photodynamic Therapy XXIII, San Francisco, CA, USA, 1–2 February 2014; Volume 8931, pp. 89310X-1–89310X-7. [Google Scholar]
- Oliveira, E.R.d.; Inada, N.M.; Ramirez, D.P.; Bagnato, V.S.; Salvio, A.G. Photodynamic therapy for widespread actinic keratosis of the upper limbs: Comparison of pain and response using aminolevulinic acid 15% and methyl aminolevulinate 15% through a new light source device. Photodiagnosis Photodyn. Ther. 2015, 12, 375. [Google Scholar] [CrossRef]
- Goel, A.; Kunnumakkara, A.B.; Aggarwal, B.B. Curcumin as “Curecumin”: From kitchen to clinic. Biochem. Pharmacol. 2008, 75, 787–809. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Esatbeyoglu, T.; Huebbe, P.; Ernst, I.M.A.; Chin, D.; Wagner, A.E.; Rimbach, G. Curcumin-from molecule to biological function. Angew. Chem. Int. Ed. 2012, 51, 5308–5332. [Google Scholar] [CrossRef] [PubMed]
- Bruzell, E.M.; Morisbak, E.; Tønnesen, H.H. Studies on curcumin and curcuminoids. XXIX. Photoinduced cytotoxicity of curcumin in selected aqueous preparations. Photochem. Photobiol. Sci. 2005, 4, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Wikene, K.O.; Hegge, A.B.; Bruzell, E.; Tonnesen, H.H. Formulation and characterization of lyophilized curcumin solid dispersions for antimicrobial photodynamic therapy (aPDT): Studies on curcumin and curcuminoids LII. Drug Dev. Ind. Pharm. 2015, 41, 969–977. [Google Scholar] [CrossRef] [PubMed]
- Butler, H.J.; Ashton, L.; Bird, B.; Cinque, G.; Curtis, K.; Dorney, J.; Esmonde-White, K.; Fullwood, N.J.; Gardner, B.; Martin-Hirsch, P.L.; et al. Using Raman spectroscopy to characterize biological materials. Nat. Protoc. 2016, 11, 664–687. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, R.; Wright, K.L.; Ashton, L. Raman spectroscopy: An evolving technique for live cell studies. Analyst 2016, 141, 3590–3600. [Google Scholar] [CrossRef] [PubMed]
- Palonpon, A.F.; Sodeoka, M.; Fujita, K. Molecular imaging of live cells by Raman microscopy. Curr. Opin. Chem. Biol. 2013, 17, 708–715. [Google Scholar] [CrossRef]
- Surmacki, J.; Musial, J.; Kordek, R.; Abramczyk, H. Raman imaging at biological interfaces: Applications in breast cancer diagnosis. Mol. Cancer 2013, 12, 48. [Google Scholar] [CrossRef] [PubMed]
- Matthäus, C.; Chernenko, T.; Quintero, L.; Miljković, M.; Milane, L.; Kale, A.; Amiji, M.; Torchilin, V.; Diem, M. Raman Micro-spectral Imaging of Cells and Intracellular Drug Delivery Using Nanocarrier Systems. In Confocal Raman Microscopy; Dieing, T., Hollricher, O., Toporski, J., Eds.; Springer: Berlin/Heidelberg, Germany, 2011; pp. 137–163. ISBN 978-3-642-12522-5. [Google Scholar]
- Lee, A.Y.; Erdemir, D.; Myerson, A.S. Crystal Polymorphism in Chemical Process Development. Annu. Rev. Chem. Biomol. Eng. 2011, 2, 259–280. [Google Scholar] [CrossRef] [PubMed]
- Chemburkar, S.R.; Bauer, J.; Deming, K.; Spiwek, H.; Patel, K.; Morris, J.; Henry, R.; Spanton, S.; Dziki, W.; Porter, W.; et al. Dealing with the impact of ritonavir polymorphs on the late stages of bulk drug process development. Org. Process Res. Dev. 2000, 4, 413–417. [Google Scholar] [CrossRef]
- Hédoux, A.; Guinet, Y.; Paccou, L.; Danède, F.; Derollez, P. Polymorphic transformation of anhydrous caffeine upon grinding and hydrostatic pressurizing analyzed by low-frequency raman spectroscopy. J. Pharm. Sci. 2013, 102, 162–170. [Google Scholar] [CrossRef] [PubMed]
- Piqueras, S.; Duponchel, L.; Tauler, R.; De Juan, A. Monitoring polymorphic transformations by using in situ Raman hyperspectral imaging and image multiset analysis. Anal. Chim. Acta 2014, 819, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Taylor, L.S.; Williams, A.C.; York, P. Particle size dependent molecular rearrangements during the dehydration of trehalose dihydrate-in situ FT-Raman spectroscopy. Pharm. Res. 1998, 15, 1207–1214. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Hornedo, N.; Nehm, S.J.; Seefeldt, K.F.; Pagán-Torres, Y.; Falkiewicz, C.J. Reaction crystallization of pharmaceutical molecular complexes. Mol. Pharm. 2006, 3, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Lestari, M.L.A.D.; Indrayanto, G. Curcumin; Academic Press: Burlington, NJ, USA, 2014; Volume 39, ISBN 9780128001738. [Google Scholar]
- Van Nong, H.; Hung, L.X.; Thang, P.N.; Chinh, V.D.; Vu, L.V.; Dung, P.T.; Van Trung, T.; Nga, P.T. Fabrication and vibration characterization of curcumin extracted from turmeric (Curcuma longa) rhizomes of the northern Vietnam. Springerplus 2016, 5, 1147. [Google Scholar] [CrossRef]
- Kolev, T.M.; Velcheva, E.A.; Stamboliyska, B.A.; Spiteller, M. DFT and experimental studies of the structure and vibrational spectra of curcumin. Int. J. Quantum Chem. 2005, 102, 1069–1079. [Google Scholar] [CrossRef]
- Tulloch, A.P. The composition of beeswax and other waxes secreted by insects. Lipids 1970, 5, 247–258. [Google Scholar] [CrossRef]
- Bogdanov, S. Beeswax: Production, Properties, Composition, Control. Bee Prod. Sci. 2016, 2, 1–17. [Google Scholar]
- March, J. Advanced Organic Chemistry; Wiley: New York, NY, USA, 1992; ISBN 9780387683508. [Google Scholar]









© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iermak, I.; da Silva, A.P.; Kurachi, C.; Bagnato, V.S.; Inada, N.M. Raman Microspectroscopy as a Tool to Elucidate the Efficacy of Topical Formulations Containing Curcumin. Pharmaceuticals 2019, 12, 44. https://doi.org/10.3390/ph12010044
Iermak I, da Silva AP, Kurachi C, Bagnato VS, Inada NM. Raman Microspectroscopy as a Tool to Elucidate the Efficacy of Topical Formulations Containing Curcumin. Pharmaceuticals. 2019; 12(1):44. https://doi.org/10.3390/ph12010044
Chicago/Turabian StyleIermak, Ievgeniia, Ana Paula da Silva, Cristina Kurachi, Vanderlei Salvador Bagnato, and Natalia Mayumi Inada. 2019. "Raman Microspectroscopy as a Tool to Elucidate the Efficacy of Topical Formulations Containing Curcumin" Pharmaceuticals 12, no. 1: 44. https://doi.org/10.3390/ph12010044