Childhood Food Experiences and Selected Eating Styles as Determinants of Diet Quality in Adulthood—A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Sample Collection
2.2. Instruments: Intuitive Eating Scale-2 (IES-2), Dutch Eating Behavior Questionnaire (DEBQ), Adult’s Memories of Feeding in Childhood (AMoFiC)
2.3. Assessment of the Diet Quality
2.4. Sociodemographic Characteristics
2.5. Statistical Analysis
3. Results
3.1. Psychosocial Characteristics of the Study Sample
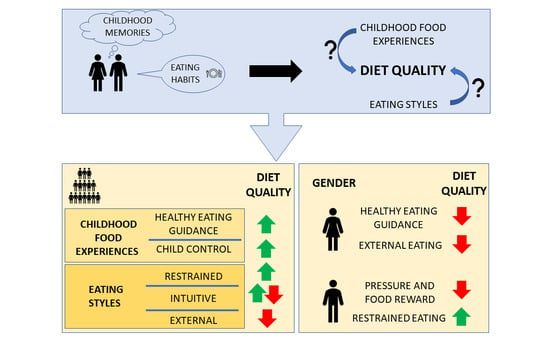
3.2. Determinants of the Diet Quality
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- The Official Website of the World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 20 January 2023).
- Bhurosy, T.; Jeewon, R. Overweight and Obesity Epidemic in Developing Countries: A Problem with Diet, Physical Activity, or Socioeconomic Status? Sci. World J. 2014, 2014, 964236. [Google Scholar] [CrossRef] [PubMed]
- Jeffers, A.J.; Mason, T.B.; Benotsch, E.G. Psychological eating factors, affect, and ecological momentary assessed diet quality. Eat. Weight Disord.—Stud. Anorex. Bulim. Obes. 2019, 25, 1151–1159. [Google Scholar] [CrossRef] [PubMed]
- Scherwitz, L.; Kesten, D. Seven Eating Styles Linked to Overeating, Overweight, and Obesity. Explor. J. Sci. Health 2005, 1, 342–359. [Google Scholar] [CrossRef] [PubMed]
- Zarychta, K.; Kulis, E.; Gan, Y.; Chan, C.K.Y.; Horodyska, K.; Luszczynska, A. Why are you eating, mom? Maternal emotional, restrained, and external eating explaining children’s eating styles. Appetite 2019, 141, 104335. [Google Scholar] [CrossRef]
- Kerin, J.L.; Webb, H.J.; Zimmer-Gembeck, M.J. Intuitive, mindful, emotional, external and regulatory eating behaviours and beliefs: An investigation of the core components. Appetite 2019, 132, 139–146. [Google Scholar] [CrossRef]
- van Strien, T.; Frijters, J.E.R.; Bergers, G.P.A.; Defares, P.B. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int. J. Eat. Disord. 1986, 5, 295–315. [Google Scholar] [CrossRef]
- van Strien, T.; Konttinen, H.M.; Ouwens, M.A.; van de Laar, F.A.; Winkens, L.H.H. Mediation of emotional and external eating between dieting and food intake or BMI gain in women. Appetite 2020, 145, 104493. [Google Scholar] [CrossRef]
- Lluch, A.; Herbeth, B.; Méjean, L.; Siest, G. Dietary intakes, eating style and overweight in the Stanislas Family Study. Int. J. Obes. 2000, 24, 1493–1499. [Google Scholar] [CrossRef]
- Cleobury, L.; Tapper, K. Reasons for eating “unhealthy” snacks in overweight and obese males and females. J. Hum. Nutr. Diet. 2014, 27, 333–341. [Google Scholar] [CrossRef]
- Magklis, E.; Howe, L.D.; Johnson, L. Eating Style and the Frequency, Size and Timing of Eating Occasions: A cross-sectional analysis using 7-day weighed dietary records. Sci. Rep. 2019, 9, 15133. [Google Scholar] [CrossRef]
- Camilleri, G.M.; Méjean, C.; Bellisle, F.; Andreeva, V.A.; Kesse-Guyot, E.; Hercberg, S.; Péneau, S. Intuitive eating dimensions were differently associated with food intake in the general population-based nutrinet-santé study. J. Nutr. 2017, 147, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Barad, A.; Cartledge, A.; Gemmill, K.; Misner, N.M.; Santiago, C.E.; Yavelow, M.; Langkamp-Henken, B. Associations Between Intuitive Eating Behaviors and Fruit and Vegetable Intake Among College Students. J. Nutr. Educ. Behav. 2019, 51, 758–762. [Google Scholar] [CrossRef] [PubMed]
- Horwath, C.; Hagmann, D.; Hartmann, C. Intuitive eating and food intake in men and women: Results from the Swiss food panel study. Appetite 2019, 135, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Madden, C.E.L.; Leong, S.L.; Gray, A.; Horwath, C.C. Eating in response to hunger and satiety signals is related to BMI in a nationwide sample of 1601 mid-age New Zealand women. Public Health Nutr. 2012, 15, 2272–2279. [Google Scholar] [CrossRef] [PubMed]
- Małachowska, A.; Jeżewska-Zychowicz, M. Polish Adaptation and Validation of the Intuitive (IES-2) and Mindful (MES) Eating Scales—The Relationship of the Concepts with Healthy and Unhealthy Food Intake (a Cross-Sectional Study). Nutrients 2022, 14, 1109. [Google Scholar] [CrossRef]
- Małachowska, A.; Jeżewska-Zychowicz, M.; Gębski, J. Polish Adaptation of the Dutch Eating Behaviour Questionnaire (DEBQ): The Role of Eating Style in Explaining Food Intake—A Cross-Sectional Study. Nutrients 2021, 13, 4486. [Google Scholar] [CrossRef]
- van Strien, T.; Herman, C.P.; Verheijden, M.W. Eating style, overeating, and overweight in a representative Dutch sample. Does external eating play a role? Appetite 2009, 52, 380–387. [Google Scholar] [CrossRef]
- Van Strien, T.; Herman, C.P.; Verheijden, M.W. Dietary restraint and body mass change. A 3-year follow up study in a representative Dutch sample. Appetite 2014, 76, 44–49. [Google Scholar] [CrossRef]
- Ruzanska, U.A.; Warschburger, P. Intuitive eating mediates the relationship between self-regulation and BMI—Results from a cross-sectional study in a community sample. Eat. Behav. 2019, 33, 23–29. [Google Scholar] [CrossRef]
- Barrada, J.R.; Cativiela, B.; Van Strien, T.; Cebolla, A. Intuitive Eating: A Novel Eating Style? Evidence from a Spanish Sample. Eur. J. Psychol. Assess. 2020, 36, 19–31. [Google Scholar] [CrossRef]
- Liu, Y.; Cui, T.; Barnhart, W.R.; Wang, Q.; Yu, Y.; He, J. Associations among retrospective parenting styles, retrospective food parenting, and current eating behaviors in Chinese adults. Appetite 2023, 184, 106512. [Google Scholar] [CrossRef] [PubMed]
- Lopez, T.D.; Hernandez, D.; Bode, S.; Ledoux, T. A complex relationship between intuitive eating and diet quality among university students. J Am. Coll. Health, 2021; online ahead of print. [Google Scholar] [CrossRef]
- Jackson, A.M.; Parker, L.; Sano, Y.; Cox, A.E.; Lanigan, J. Associations between body image, eating behavior, and diet quality. Nutr. Health, 2022; online ahead of print. [Google Scholar] [CrossRef]
- Tacad, D.K.; Cervantes, E.; Bouzid, Y.; Stephensen, C.; Keim, N. Dietary Restraint Constructs Are Associated With Diet Quality and Nutrient Intake. Curr. Dev. Nutr. 2022, 6, 401. [Google Scholar] [CrossRef]
- Borelli, J.; Pignotti, G.P.; Widaman, A. Examining the Relationship Between Intuitive Eating and Diet Quality Among College Students. Curr. Dev. Nutr. 2020, 4, 1290. [Google Scholar] [CrossRef]
- Denny, K.N.; Loth, K.; Eisenberg, M.E.; Neumark-Sztainer, D. Intuitive eating in young adults. Who is doing it, and how is it related to disordered eating behaviors? Appetite 2013, 60, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Scaglioni, S.; De Cosmi, V.; Ciappolino, V.; Parazzini, F.; Brambilla, P.; Agostoni, C. Factors Influencing Children’s Eating Behaviours. Nutrients 2018, 10, 706. [Google Scholar] [CrossRef]
- Russell, C.G.; Haszard, J.J.; Taylor, R.W.; Heath, A.L.M.; Taylor, B.; Campbell, K.J. Parental feeding practices associated with children’s eating and weight: What are parents of toddlers and preschool children doing? Appetite 2018, 128, 120–128. [Google Scholar] [CrossRef]
- Lopez, N.V.; Schembre, S.; Belcher, B.R.; O’Connor, S.; Maher, J.P.; Arbel, R.; Margolin, G.; Dunton, G.F. Parenting styles, food-related parenting practices, and children’s healthy eating: A mediation analysis to examine relationships between parenting and child diet. Appetite 2018, 128, 205–213. [Google Scholar] [CrossRef]
- Peters, J.; Dollman, J.; Petkov, J.; Parletta, N. Associations between parenting styles and nutrition knowledge and 2–5-year-old children’s fruit, vegetable and non-core food consumption. Public Health Nutr. 2013, 16, 1979–1987. [Google Scholar] [CrossRef]
- Kremers, S.P.J.; Brug, J.; De Vries, H.; Engels, R.C.M.E. Parenting style and adolescent fruit consumption. Appetite 2003, 41, 43–50. [Google Scholar] [CrossRef]
- De Bourdeaudhuij, I.; te Velde, S.; Brug, J.; Due, P.; Wind, M.; Sandvik, C.; Maes, L.; Wolf, A.; Perez Rodrigo, C.; Yngve, A.; et al. Personal, social and environmental predictors of daily fruit and vegetable intake in 11-year-old children in nine European countries. Eur. J. Clin. Nutr. 2007, 62, 834–841. [Google Scholar] [CrossRef]
- Puhl, R.M.; Schwartz, M.B. If you are good you can have a cookie: How memories of childhood food rules link to adult eating behaviors. Eat. Behav. 2003, 4, 283–293. [Google Scholar] [CrossRef] [PubMed]
- Ellis, J.M.; Galloway, A.T.; Webb, R.M.; Martz, D.M.; Farrow, C.V. Recollections of pressure to eat during childhood, but not picky eating, predict young adult eating behavior. Appetite 2016, 97, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Tan, C.C.; Ruhl, H.; Chow, C.M.; Ellis, L. Retrospective reports of parental feeding practices and emotional eating in adulthood: The role of food preoccupation. Appetite 2016, 105, 410–415. [Google Scholar] [CrossRef] [PubMed]
- Galloway, A.T.; Farrow, C.V.; Martz, D.M. Retrospective reports of child feeding practices, current eating behaviors, and BMI in college students. Obesity 2010, 18, 1330–1335. [Google Scholar] [CrossRef] [PubMed]
- Williams, N.A.; Dev, D.A.; Hankey, M.; Blitch, K. Role of food preoccupation and current dieting in the associations of parental feeding practices to emotional eating in young adults: A moderated mediation study. Appetite 2017, 111, 195–202. [Google Scholar] [CrossRef]
- Robert Batsell, W.; Brown, A.S.; Ansfield, M.E.; Paschall, G.Y. “You will eat all of that!”: A retrospective analysis of forced consumption episodes. Appetite 2002, 38, 211–219. [Google Scholar] [CrossRef]
- Brink, P.J.; Ferguson, K.; Sharma, A. Dieters Project. J. Child Adolesc. Psychiatr. Nurs. 1999, 13, 17–25. [Google Scholar] [CrossRef]
- Branen, L.; Fletcher, J. Comparison of college students’ current eating habits and recollections of their childhood food practices. J. Nutr. Educ. Behav. 1999, 31, 304–310. [Google Scholar] [CrossRef]
- Van Tine, M.L.; McNicholas, F.; Safer, D.L.; Agras, W.S. Follow-up of selective eaters from childhood to adulthood. Eat. Behav. 2017, 26, 61–65. [Google Scholar] [CrossRef]
- Małachowska, A.; Jeżewska-Zychowicz, M. Does Examining the Childhood Food Experiences Help to Better Understand Food Choices in Adulthood? Nutrients 2021, 13, 983. [Google Scholar] [CrossRef]
- Jezewska-Zychowicz, M.; Gawecki, J.; Wadolowska, L.; Czarnocinska, J.; Galinski, G.; Kollajtis-Dolowy, A.; Roszkowski, W.; Wawrzyniak, A.; Przybylowicz, K.; Stasiewicz, B.; et al. Dietary Habits and Nutrition Beliefs Questionnaire for people 15–65 yearsold, version 1.1.—Interviewer administered questionnaire. In Dietary Habits and Nutrition Beliefs Questionnaire and the Manual for Developing of Nutritional Data; Gawecki, J., Ed.; The Committee of Human Nutrition, Polish Academy of Sciences: Olsztyn, Poland, 2018; pp. 3–20. [Google Scholar]
- Wądołowska, L.; Krusińska, B. The manual for developing nutritional data from the KomPAN®questionnaire. In Dietary Habits and Nutrition Beliefs Questionnaire and the Manual for Developing Nutritional Data; Gawecki, J., Ed.; The Committee of Human Nutrition, Polish Academy of Sciences: Olsztyn, Poland, 2018; pp. 34–52. [Google Scholar]
- Binder, A.; Naderer, B.; Matthes, J. A “Forbidden Fruit Effect”: An Eye-Tracking Study on Children’s Visual Attention to Food Marketing. Int. J. Environ. Res. Public Health 2020, 17, 1859. [Google Scholar] [CrossRef] [PubMed]
- Berge, J.M.; MacLehose, R.F.; Larson, N.; Laska, M.; Neumark-Sztainer, D. Family Food Preparation and Its Effects on Adolescent Dietary Quality and Eating Patterns. J. Adolesc. Health 2016, 59, 530. [Google Scholar] [CrossRef] [PubMed]
- Laska, M.N.; Larson, N.I.; Neumark-Sztainer, D.; Story, M. Does involvement in food preparation track from adolescence to young adulthood and is it associated with better dietary quality? Findings from a ten-year longitudinal study. Public Health Nutr. 2012, 15, 1150. [Google Scholar] [CrossRef] [PubMed]
- Neumark-Sztainer, D.; Wall, M.; Larson, N.I.; Eisenberg, M.E.; Loth, K. Dieting and disordered eating behaviors from adolescence to young adulthood: Findings from a 10-year longitudinal study. J. Am. Diet. Assoc. 2011, 111, 1004. [Google Scholar] [CrossRef]
- Coffino, J.A.; Orloff, N.C.; Hormes, J.M. Dietary restraint partially mediates the relationship between impulsivity and binge eating only in lean individuals: The importance of accounting for body mass in studies of restraint. Front. Psychol. 2016, 7, 1499. [Google Scholar] [CrossRef]
- Shloim, N.; Edelson, L.R.; Martin, N.; Hetherington, M.M. Parenting styles, feeding styles, feeding practices, and weight status in 4-12 year-old children: A systematic review of the literature. Front. Psychol. 2015, 6, 1849. [Google Scholar] [CrossRef]
- Steele, R.G.; Jensen, C.D.; Gayes, L.A.; Leibold, H.C. Medium is the message: Moderate parental control of feeding correlates with improved weight outcome in a pediatric obesity intervention. J. Pediatr. Psychol. 2014, 39, 708–717. [Google Scholar] [CrossRef]
- Dickens, E.; Ogden, J. The role of parental control and modelling in predicting a child’s diet and relationship with food after they leave home. A prospective study. Appetite 2014, 76, 23–29. [Google Scholar] [CrossRef]
- Hazzard, V.M.; Loth, K.A.; Berge, J.M.; Larson, N.I.; Fulkerson, J.A.; Neumark-Sztainer, D. Does exposure to controlling parental feeding practices during adolescence predict disordered eating behaviors 8 years later in emerging adulthood? Pediatr. Obes. 2020, 15, e12709. [Google Scholar] [CrossRef]
- Del Parigi, A.; Chen, K.; Gautier, J.F.; Salbe, A.D.; Pratley, R.E.; Ravussin, E.; Reiman, E.M.; Antonio Tataranni, P. Sex differences in the human brain’s response to hunger and satiation. Am. J. Clin. Nutr. 2002, 75, 1017–1022. [Google Scholar] [CrossRef]
- Harris, H.; Mallan, K.M.; Nambiar, S.; Daniels, L.A. The relationship between controlling feeding practices and boys’ and girls’ eating in the absence of hunger. Eat. Behav. 2014, 15, 519–522. [Google Scholar] [CrossRef] [PubMed]
- Loth, K.A.; Maclehose, R.F.; Fulkerson, J.A.; Crow, S.; Neumark-Sztainer, D. Are food restriction and pressure-to-eat parenting practices associated with adolescent disordered eating behaviors? Int. J. Eat. Disord. 2014, 47, 310. [Google Scholar] [CrossRef] [PubMed]
- van Strien, T.; Bazelier, F.G. Perceived parental control of food intake is related to external, restrained and emotional eating in 7–12-year-old boys and girls. Appetite 2007, 49, 618–625. [Google Scholar] [CrossRef] [PubMed]
- Philippe, K.; Chabanet, C.; Issanchou, S.; Monnery-Patris, S. Are food parenting practices gendered? Impact of mothers’ and fathers’ practices on their child’s eating behaviors. Appetite 2021, 166, 105433. [Google Scholar] [CrossRef] [PubMed]
- Martin, S.L.; McCann, J.K.; Gascoigne, E.; Allotey, D.; Fundira, D.; Dickin, K.L. Engaging family members in maternal, infant and young child nutrition activities in low- and middle-income countries: A systematic scoping review. Matern. Child Nutr. 2021, 17, e13158. [Google Scholar] [CrossRef]
- Movassagh, E.Z.; Baxter-Jones, A.D.G.; Kontulainen, S.; Whiting, S.J.; Vatanparast, H. Tracking Dietary Patterns over 20 Years from Childhood through Adolescence into Young Adulthood: The Saskatchewan Pediatric Bone Mineral Accrual Study. Nutrients 2017, 9, 990. [Google Scholar] [CrossRef]
- Leal, D.B.; de Assis, M.A.A.; Hinnig, P.d.F.; Schmitt, J.; Lobo, A.S.; Bellisle, F.; di pietro, P.F.; Vieira, F.K.; Araujo, P.H.d.M.; de Andrade, D.F. Changes in Dietary Patterns from Childhood to Adolescence and Associated Body Adiposity Status. Nutrients 2017, 9, 1098. [Google Scholar] [CrossRef]
- Luque, V.; Escribano, J.; Closa-Monasterolo, R.; Zaragoza-Jordana, M.; Ferré, N.; Grote, V.; Koletzko, B.; Totzauer, M.; Verduci, E.; ReDionigi, A.; et al. Unhealthy Dietary Patterns Established in Infancy Track to Mid-Childhood: The EU Childhood Obesity Project. J. Nutr. 2018, 148, 752–759. [Google Scholar] [CrossRef]
- Tylka, T.L. Development and psychometric evaluation of a measure of intuitive eating. J. Couns. Psychol. 2006, 53, 226–240. [Google Scholar] [CrossRef]
- Hensley-Hackett, K.; Bosker, J.; Keefe, A.; Reidlinger, D.; Warner, M.; D’Arcy, A.; Utter, J. Intuitive Eating Intervention and Diet Quality in Adults: A Systematic Literature Review. J. Nutr. Educ. Behav. 2022, 54, 1099–1115. [Google Scholar] [CrossRef]
- Reents, J.; Seidel, A.K.; Wiesner, C.D.; Pedersen, A. The Effect of Hunger and Satiety on Mood-Related Food Craving. Front. Psychol. 2020, 11, 568908. [Google Scholar] [CrossRef] [PubMed]
- Burton, P.; Smit, H.J.; Lightowler, H.J. The influence of restrained and external eating patterns on overeating. Appetite 2007, 49, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Ferrer-Garcia, M.; Pla-Sanjuanelo, J.; Dakanalis, A.; Vilalta-Abella, F.; Riva, G.; Fernandez-Aranda, F.; Sánchez, I.; Ribas-Sabaté, J.; Andreu-Gracia, A.; Escandón-Nagel, N.; et al. Eating behavior style predicts craving and anxiety experienced in food-related virtual environments by patients with eating disorders and healthy controls. Appetite 2017, 117, 284–293. [Google Scholar] [CrossRef]
- Cepeda-Benito, A.; Fernandez, M.C.; Moreno, S. Relationship of gender and eating disorder symptoms to reported cravings for food: Construct validation of state and trait craving questionnaires in Spanish. Appetite 2003, 40, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Polivy, J.; Herman, C.P.; Mills, J.S. What is restrained eating and how do we identify it? Appetite 2020, 155, 104820. [Google Scholar] [CrossRef] [PubMed]
- Imamura, F.; Micha, R.; Khatibzadeh, S.; Fahimi, S.; Shi, P.; Powles, J.; Mozaffarian, D. Dietary quality among men and women in 187 countries in 1990 and 2010: A systematic assessment. Lancet Glob. Health 2015, 3, e132–e142. [Google Scholar] [CrossRef]
- Eskandari, F.; Lake, A.A.; Rose, K.; Butler, M.; O’Malley, C. A mixed-method systematic review and meta-analysis of the influences of food environments and food insecurity on obesity in high-income countries. Food Sci. Nutr. 2022, 10, 3689–3723. [Google Scholar] [CrossRef]
| Variables | Total (N = 708) N (%) | Women (N = 477) N (%) | Men (N = 231) N (%) | |
|---|---|---|---|---|
| Age (years) | 18–24 | 94 (13.3) | 65 (13.6) | 29 (12.6) |
| 25–39 | 349 (49.3) | 253 (53.0) | 96 (41.6) | |
| 40–54 | 193 (27.3) | 120 (25.2) | 73 (31.6) | |
| 55–65 | 72 (10.2) | 39 (8.2) | 33 (14.3) | |
| Education | Primary | 3 (0.4) | 3 (0.6) | 0 (0.0) |
| Lower secondary | 3 (0.4) | 2 (0.4) | 1 (0.4) | |
| Upper secondary | 113 (16.0) | 68 (14.3) | 45 (19.5) | |
| Higher (e.g., BSc and MSc) | 589 (83.2) | 404 (84.7) | 185 (80.1) | |
| Place of Residence | Village | 113 (16.0) | 78 (16.4) | 35 (15.2) |
| Town below 20,000 inhabitants | 43 (6.1) | 31 (6.5) | 12 (5.2) | |
| Town between 20,000 and 100,000 inhabitants | 109 (15.4) | 69 (14.5) | 40 (17.3) | |
| City with over 100,000 inhabitants | 443 (62.6) | 299 (62.7) | 144 (62.3) | |
| Subscales | Total (N = 708) M ± SD | Women (N = 477) M ± SD | Men (N = 231) M ± SD |
|---|---|---|---|
| Restrictions 1 | 1.93 ± 0.60 | 1.94 ± 0.61 | 1.93 ± 0.56 |
| Healthy Eating Guidance 1 | 3.21 ± 0.90 | 3.22 ± 0.93 | 3.19 ± 0.84 |
| Pressure and Food Reward 1 | 2.62 ± 0.94 | 2.64 ± 0.97 | 2.58 ± 0.87 |
| Monitoring 1 | 2.57 ± 1.06 | 2.60 ± 1.09 | 2.50 ± 0.98 |
| Child Control 1 | 2.55 ± 0.78 | 2.60 ± 0.81 | 2.46 ± 0.70 |
| RHSC 2 | 3.40 ± 0.81 | 3.36 ± 0.85 | 3.46 ± 0.71 |
| EPR *** 2 | 3.33 ± 1.15 | 3.13 ± 1.16 | 3.75 ± 0.99 |
| B-FCC 2 | 3.43 ± 0.78 | 3.44 ± 0.81 | 3.41 ± 0.71 |
| UPE 2 | 3.63 ± 0.82 | 3.60 ± 0.83 | 3.67 ± 0.79 |
| ExtEat ** 3 | 2.97 ± 0.72 | 3.04 ± 0.73 | 2.85 ± 0.67 |
| ResEat *** 3 | 2.62 ± 0.88 | 2.70 ± 0.88 | 2.45 ± 0.86 |
| Diet Quality Indices | Total (N = 708) | Women (N = 477) | Men (N = 231) | |||
|---|---|---|---|---|---|---|
| M ± SD | Min–Max | M ± SD | Min–Max | M ± SD | Min–Max | |
| nHDI-14 *** | 14.90 ± 8.44 | 0.21–54.79 | 13.82 ± 7.90 | 0.64–54.79 | 17.15 ± 9.07 | 0.21–54.29 |
| pHDI-10 *** | 24.26 ± 11.11 | 1.20–66.40 | 25.84 ± 10.97 | 2.00–66.40 | 20.99 ± 10.69 | 1.20–56.40 |
| DQI *** | 9.35 ± 14.25 | −41.49–62.69 | 12.02 ± 13.74 | −20.99–62.69 | 3.85 ± 13.73 | −41.49–44.13 |
| Total (N = 708) | Women (N = 477) | Men (N = 231) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| B (SE) | t | p | B (SE) | t | p | B (SE) | t | p | |
| Intercept | 10.207 (3.63) | 2.81 | 0.005 | 12.459 (4.17) | 2.99 | 0.003 | 2.018 (6.96) | 0.29 | 0.772 |
| Restrictions 1 | 0.916 (0.62) | 1.48 | 0.140 | 0.626 (0.69) | 0.91 | 0.365 | 0.38 (1.28) | 0.30 | 0.767 |
| Healthy Eating Guidance 1 | 0.596 (0.40) | 1.48 | 0.139 | 0.879 (0.44) | 2.00 | 0.046 | −0.007 (0.85) | −0.01 | 0.994 |
| Pressure and Food Reward 1 | 0.368 (0.32) | 1.14 | 0.253 | −0.079 (0.35) | −0.22 | 0.824 | 1.587 (0.68) | 2.34 | 0.020 |
| Monitoring 1 | −0.315 (0.36) | −0.89 | 0.376 | −0.318 (0.39) | −0.82 | 0.414 | 0.003 (0.75) | 0.00 | 0.997 |
| Child Control 1 | 0.426 (0.38) | 1.12 | 0.265 | 0.624 (0.41) | 1.50 | 0.134 | 0.309 (0.83) | 0.37 | 0.709 |
| RHSC 2 | 0.353 (0.44) | 0.8 | 0.422 | 0.644 (0.5) | 1.30 | 0.196 | 0.285 (0.87) | 0.33 | 0.743 |
| EPR 2 | 0.323 (0.31) | 1.04 | 0.297 | −0.349 (0.35) | −0.99 | 0.323 | 0.871 (0.65) | 1.34 | 0.181 |
| B-FCC 2 | −2.742 (0.44) | −6.24 | <0.001 | −2.886 (0.49) | −5.86 | <0.001 | −1.91 (0.88) | −2.17 | 0.031 |
| UPE 2 | 1.678 (0.46) | 3.66 | <0.001 | 1.238 (0.53) | 2.32 | 0.021 | 2.75 (0.85) | 3.22 | 0.002 |
| ExtEat 3 | 1.02 (0.48) | 2.13 | 0.033 | 0.99 (0.54) | 1.86 | 0.044 | 1.022 (0.96) | 1.07 | 0.286 |
| ResEat 3 | −0.845 (0.43) | −1.96 | 0.050 | −0.702 (0.51) | −1.38 | 0.167 | −0.486 (0.79) | −0.62 | 0.537 |
| Variables | Total (N = 708) | Women (N = 477) | Men (N = 231) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B (SE) | t | p | B (SE) | t | p | B (SE) | t | p | |
| Intercept | 10.803 (4.94) | 2.19 | 0.029 | 13.615 (6.10) | 2.23 | 0.026 | 4.417 (8.49) | 0.52 | 0.603 |
| Restrictions 1 | 0.360 (0.84) | 0.43 | 0.670 | 1.02 (1.01) | 1.01 | 0.313 | −0.173 (1.56) | −0.11 | 0.912 |
| Healthy Eating Guidance 1 | 1.126 (0.55) | 2.06 | 0.040 | 1.005 (0.64) | 1.57 | 0.118 | 0.865 (1.04) | 0.83 | 0.407 |
| Pressure and Food Reward 1 | −0.092 (0.44) | −0.21 | 0.834 | −0.316 (0.52) | −0.61 | 0.541 | 0.896 (0.83) | 1.08 | 0.280 |
| Monitoring 1 | −0.6 (0.48) | −1.24 | 0.215 | −0.527 (0.57) | −0.93 | 0.355 | −1.227 (0.91) | −1.35 | 0.180 |
| Child Control 1 | 0.859 (0.52) | 1.65 | 0.049 | 0.757 (0.61) | 1.25 | 0.213 | 0.651 (1.01) | 0.65 | 0.520 |
| RHSC 2 | 0.305 (0.60) | 0.51 | 0.609 | 0.666 (0.73) | 0.92 | 0.360 | −0.263 (1.06) | −0.25 | 0.804 |
| EPR 2 | −0.963 (0.42) | −2.29 | 0.023 | −0.972 (0.52) | −1.89 | 0.050 | 0.496 (0.79) | 0.63 | 0.532 |
| B-FCC 2 | 2.727 (0.60) | 4.56 | <0.001 | 2.91 (0.72) | 4.04 | <0.001 | 2.005 (1.07) | 1.87 | 0.043 |
| UPE 2 | −1.446 (0.62) | −2.32 | 0.021 | −1.905 (0.78) | −2.44 | 0.015 | −0.762 (1.04) | −0.73 | 0.466 |
| ExtEat 3 | 1.174 (0.65) | 1.80 | 0.072 | 1.301 (0.79) | 1.65 | 0.099 | 0.846 (1.17) | 0.73 | 0.469 |
| ResEat 3 | 1.259 (0.58) | 2.15 | 0.032 | 0.35 (0.74) | 0.47 | 0.637 | 2.418 (0.96) | 2.52 | 0.012 |
| Variables | Total (N = 708) | Women (N = 477) | Men (N = 231) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B (SE) | t | p | B (SE) | t | p | B (SE) | t | p | |
| Intercept | 0.596 (5.97) | 0.1 | 0.921 | 1.156 (7.20) | 0.16 | 0.873 | 2.399 (10.23) | 0.23 | 0.815 |
| Restrictions 1 | −0.556 (1.02) | −0.55 | 0.586 | 0.394 (1.19) | 0.33 | 0.741 | −0.553 (1.88) | −0.29 | 0.770 |
| Healthy Eating Guidance 1 | 0.53 (0.66) | 0.80 | 0.423 | 0.126 (0.76) | 0.17 | 0.868 | 0.872 (1.26) | 0.69 | 0.488 |
| Pressure and Food Reward 1 | −0.46 (0.53) | −0.87 | 0.385 | −0.237 (0.61) | −0.39 | 0.697 | −0.691 (1.00) | −0.69 | 0.490 |
| Monitoring 1 | −0.285 (0.58) | −0.49 | 0.626 | −0.208 (0.67) | −0.31 | 0.756 | −1.23 (1.10) | −1.12 | 0.265 |
| Child Control 1 | 0.433 (0.63) | 0.69 | 0.490 | 0.134 (0.72) | 0.19 | 0.852 | 0.342 (1.22) | 0.28 | 0.779 |
| RHSC 2 | −0.047 (0.72) | −0.07 | 0.948 | 0.022 (0.86) | 0.03 | 0.980 | −0.548 (1.28) | −0.43 | 0.669 |
| EPR 2 | −1.286 (0.51) | −2.53 | 0.012 | −0.623 (0.61) | −1.02 | 0.306 | −0.375 (0.96) | −0.39 | 0.695 |
| B-FCC 2 | 5.469 (0.72) | 7.57 | <0.001 | 5.796 (0.85) | 6.81 | <0.001 | 3.915 (1.29) | 3.03 | 0.003 |
| UPE 2 | −3.124 (0.75) | −4.15 | <0.001 | −3.143 (0.92) | −3.41 | 0.002 | −3.512 (1.26) | −2.79 | 0.006 |
| ExtEat 3 | 0.154 (0.79) | 0.20 | 0.845 | 0.301 (0.93) | 0.32 | 0.746 | −0.176 (1.41) | −0.13 | 0.901 |
| ResEat 3 | 2.104 (0.71) | 2.98 | 0.003 | 1.052 (0.88) | 1.20 | 0.230 | 2.905 (1.16) | 2.51 | 0.013 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Małachowska, A.; Gębski, J.; Jeżewska-Zychowicz, M. Childhood Food Experiences and Selected Eating Styles as Determinants of Diet Quality in Adulthood—A Cross-Sectional Study. Nutrients 2023, 15, 2256. https://doi.org/10.3390/nu15102256
Małachowska A, Gębski J, Jeżewska-Zychowicz M. Childhood Food Experiences and Selected Eating Styles as Determinants of Diet Quality in Adulthood—A Cross-Sectional Study. Nutrients. 2023; 15(10):2256. https://doi.org/10.3390/nu15102256
Chicago/Turabian StyleMałachowska, Aleksandra, Jerzy Gębski, and Marzena Jeżewska-Zychowicz. 2023. "Childhood Food Experiences and Selected Eating Styles as Determinants of Diet Quality in Adulthood—A Cross-Sectional Study" Nutrients 15, no. 10: 2256. https://doi.org/10.3390/nu15102256