Type 2 Diabetes Mellitus: A Review of Multi-Target Drugs
Abstract
:1. Introduction
- Type 1 diabetes mellitus (T1DM): due to autoimmune β-cell destruction, usually leading to absolute insulin deficiency;
- Type 2 diabetes mellitus (T2DM): due to a progressive loss of β-cell insulin secretion frequently on the background of insulin resistance;
- Gestational diabetes mellitus (GDM): diabetes diagnosed in the second or third trimester of pregnancy that was not clearly overt prior to gestation;
- Specific types of diabetes due to other causes, e.g., monogenic diabetes syndromes (such as neonatal diabetes and maturity-onset diabetes of the young (MODY)), diseases of the exocrine pancreas (such as cystic fibrosis and pancreatitis), and drug- or chemical-induced diabetes (such as with glucocorticoid use, in the treatment of HIV/AIDS, or after organ transplantation).
1.1. Type 2 Diabetes Mellitus (T2DM)
- Genetic influencesGenetics play a very strong role in the development of T2DM [23]. The most common forms of T2DM are polygenetic, so there are changes in multiple genes, but there are also some rare forms of diabetes that are caused by single gene mutation, known as monogenic diabetes. It is important not be confused with T1DM, so it is crucial to have a correct diagnose in order to receive a proper treatment.
- Environmental influencesNew understandings of the progression of T2DM are related both to the lifestyle and to the gut microbiota and the dynamics that leads to microbiome dysbiosis [24]. This change in the microbiota composition is able to reshape intestinal barrier functions and to induce metabolomic and signaling pathways related to the insulin resistance.
- AgeUntil two decades ago, T2DM was usually found in adults and seniors. This was consequential to the increase of insulin resistance due to body composition modification (less muscle in favor of more adipose tissues), to the reduced “sugar burning” capacity and to the progressive decrease of physical activity.Leading to the impressive growth of obesity rate, the average age of onset is lowering, and diabetes can now be found even in children.
- ObesityA person with a body mass index (BMI) equal to or greater than 30 kg/m2 is generally considered obese [25,26].The increase of adipose tissue is a primary risk factor in diabetes. In fact, there is a direct correlation between fat percentage and insulin resistant cells, especially if the fat is concentrated in the abdominal area.Around 80% of T2DM patients are obese, which is not, however, a necessary condition to develop diabetes.
- Poor physical fitness
- Hypertension and high triglycerides levelsThese are conditions usually associated with insulin resistance, so they increase diabetes risk.
- SmokingSmoking is associated with diabetes and other health conditions such as cancer and heart diseases.
- Gestational DiabetesWomen, that develop diabetes during the pregnancy, have higher risk of suffering for T2DM later in life.
- Polycystic Ovary SyndromePolycystic Ovary Syndrome (PCOS) is a common hormonal disorder that causes irregular menstrual cycles, hirsutism, acne, and, frequently, obesity.
- a)
- biguanides, like metformin, which reduce gluconeogenesis in the liver;
- b)
- insulin secretagogues which stimulate the pancreas to secrete insulin and include drugs such as sulfonylureas;
- c)
- insulin sensitizers which improve sensitivity of peripheral tissues to insulin and include thialzolidinediones and;
- d)
- insulin or its analogues which provide insulin exogenously in the form of recombinant insulin.
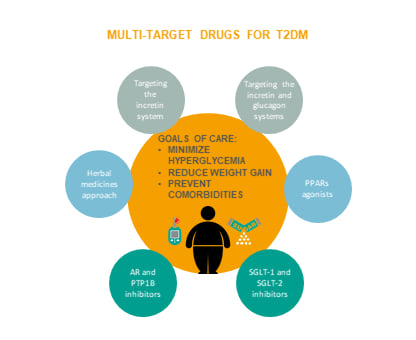
1.2. Multi-Target Compounds
2. Incretin-Based Therapies
2.1. Overview
2.2. Targeting the Incretin System
2.2.1. Dual Agonists
2.3. Targeting the Incretin/Glucagon Systems
2.3.1. Dual Agonists
2.3.2. Triagonists
2.4. Targeting Not Only the Incretin System
3. Targeting Other Systems
3.1. SGLT-1/SGLT-2 Inhibitors
3.2. AR/PTP1B Dual Inhibitors
4. PPARs-Based Therapies
4.1. Overview
4.2. Dual Agonists
4.3. Pan Agonists
5. Herbal Medicines Approach
5.1. Momordica Charantia
5.2. Panax Ginseng
5.3. Trigonella Foenum-Graecum
5.4. Scutellariae Radix
5.5. Coptidis Rhizoma
6. Conclusions and Future Directions
Author Contributions
Funding
Conflicts of Interest
References
- Sun, X.; Yu, W.; Hu, C. Genetics of type 2 diabetes: Insights into the pathogenesis and its clinical application. BioMed Res. Int. 2014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaul, N.; Ali, S. Genes, Genetics, and Environment in Type 2 Diabetes: Implication in Personalized Medicine. DNA Cell Biol. 2016, 35, 1–12. [Google Scholar] [CrossRef] [PubMed]
- WHO|Diabetes Programme. WHO. 2019. Available online: https://www.who.int/diabetes/en/ (accessed on 27 January 2019).
- Cho, N.H.; Shaw, J.E.; Karuranga, S.; Huang, Y.; Fernandes, J.D.R.; Ohlrogge, A.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 2018, 138, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Association, A.D. Classification and diagnosis of diabetes: Standards of medical care in Diabetesd2018. Diabetes Care 2018, 41, 13–27. [Google Scholar]
- Saisho, Y. Importance of Beta Cell Function for the Treatment of Type 2 Diabetes. J. Clin. Med. 2014, 3, 923–943. [Google Scholar] [CrossRef] [Green Version]
- Rosenbloom, A.L.; Joe, J.R.; Young, R.S.; Winter, W.E. Emerging epidemic of type 2 diabetes in youth. Diabetes Care 1999, 22, 345–354. [Google Scholar] [CrossRef]
- Dabelea, D.; Pettitt, D.J.; Jones, K.L.; Arslanian, S.A. Type 2 diabetes mellitus in minority children and adolescents. An emerging problem. Endocrinol. Metab. Clin. North Am. 1999, 28, 709–729. [Google Scholar] [CrossRef]
- Sinha, R.; Fisch, G.; Teague, B.; Tamborlane, W.V.; Banyas, B.; Allen, K.; Savoye, M.; Rieger, V.; Taksali, S.; Barbetta, G.; et al. Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. N. Engl. J. Med. 2002, 346, 802–810. [Google Scholar] [CrossRef]
- Guerre-Millo, M. Adipose tissue hormones. J. Endocrinol. Investig. 2002, 25, 855–861. [Google Scholar] [CrossRef]
- Jalovaara, K.; Santaniemi, M.; Timonen, M.; Jokelainen, J.; Kesäniemi, Y.A.; Ukkola, O.; Keinänen-Kiukaanniemi, S.; Rajala, U. Low serum adiponectin level as a predictor of impaired glucose regulation and type 2 diabetes mellitus in a middle-aged Finnish population. Metabolism 2008, 57, 1130–1134. [Google Scholar] [CrossRef]
- Zhang, Y.; Scarpace, P.J. The role of leptin in leptin resistance and obesity. Physiol. Behav. 2006, 88, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Kelesidis, T.; Kelesidis, I.; Chou, S.; Mantzoros, C.S. Narrative Review: The Role of Leptin in Human Physiology: Emerging Clinical Applications. Ann. Intern. Med. 2010, 152, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Esmaili, S.; Hemmati, M.; Karamian, M. Physiological role of adiponectin in different tissues: A review. Arch. Physiol. Biochem. 2020, 126, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Yadav, A.; Jyoti, P.; Jain, S.K.; Bhattacharjee, J. Correlation of adiponectin and leptin with insulin resistance: A pilot study in healthy North Indian population. Indian J. Clin. Biochem. 2011, 26, 193–196. [Google Scholar] [CrossRef] [Green Version]
- Sears, B.; Perry, M. The role of fatty acids in insulin resistance. Lipids Health Dis. 2015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boden, G. Effects of free fatty acids (FFA) on glucose metabolism: Significance for insulin resistance and type 2 diabetes. Exp. Clin. Endocrinol. Diabetes 2003, 111, 121–124. [Google Scholar] [CrossRef]
- Vergès, B. Pathophysiology of diabetic dyslipidaemia: Where are we? Diabetologia 2015, 58, 886–899. [Google Scholar] [CrossRef] [Green Version]
- Ference, B.A.; Ginsberg, H.N.; Graham, I.; Ray, K.K.; Packard, C.J.; Bruckert, É.; Hegele, R.A.; Krauss, R.M.; Raal, F.J.; Schunkert, H.; et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 2017, 38, 2459–2472. [Google Scholar] [CrossRef] [Green Version]
- Bonnefond, A.; Froguel, P.; Vaxillaire, M. The emerging genetics of type 2 diabetes. Trends Mol. Med. 2010, 16, 407–416. [Google Scholar] [CrossRef]
- McCarthy, M.I. Genomics, Type 2 Diabetes, and Obesity. N. Engl. J. Med. 2010, 363, 2339–2350. [Google Scholar] [CrossRef] [Green Version]
- Kahn, S.E. The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of Type 2 diabetes. Diabetologia 2003, 46, 3–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ali, O. Genetics of type 2 diabetes. World J. Diabetes 2013, 4, 114–123. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Tripathi, P. Gut microbiome and type 2 diabetes: Where we are and where to go? J. Nutr. Biochem. 2019, 63, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Seidell, J.C. Assessing obesity: Classification and epidemiology. Br. Med Bull. 1997, 53, 238–252. [Google Scholar] [CrossRef] [Green Version]
- Apovian, C.M. Obesity: Definition, comorbidities, causes, and burden. Am. J. Manag. Care 2016, 22, 176–185. [Google Scholar]
- Hu, F.B. Sedentary lifestyle and risk of obesity and type 2 diabetes. Lipids 2003, 38, 103–108. [Google Scholar] [CrossRef]
- Wu, Y.; Ding, Y.; Tanaka, Y.; Zhang, W. Risk factors contributing to type 2 diabetes and recent advances in the treatment and prevention. Int. J. Med Sci. 2014, 11, 1185–1200. [Google Scholar] [CrossRef] [Green Version]
- McGovern, A.; Tippu, Z.; Hinton, W.; Munro, N.; Whyte, M.; De Lusignan, S. Comparison of medication adherence and persistence in type 2 diabetes: A systematic review and meta-analysis. Diabetes Obes. Metab. 2018, 20, 1040–1043. [Google Scholar] [CrossRef] [Green Version]
- Buse, J.B.; Wexler, D.J.; Tsapas, A.; Rossing, P.; Mingrone, G.; Mathieu, C.; D’Alessio, D.A.; Davies, M.J. 2019 update to: Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2020, 43, 487–493. [Google Scholar] [CrossRef] [Green Version]
- Morphy, R.; Rankovic, Z. Designed multiple ligands. An emerging drug discovery paradigm. J. Med. Chem. 2005, 48, 6523–6543. [Google Scholar] [CrossRef]
- Zimmermann, G.R.; Lehár, J.; Keith, C.T. Multi-target therapeutics: When the whole is greater than the sum of the parts. Drug Discov. Today 2007, 12, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Irwin, N. New perspectives on exploitation of incretin peptides for the treatment of diabetes and related disorders. World J. Diabetes 2015, 6, 1285–1295. [Google Scholar] [CrossRef] [PubMed]
- Drucker, D.J. The biology of incretin hormones. Cell Metab. 2006, 3, 153–165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drucker, D.J. Deciphering metabolic messages from the gut drives therapeutic innovation: The 2014 banting lecture. Diabetes 2015, 64, 317–326. [Google Scholar] [CrossRef] [Green Version]
- Toft-Nielsen, M.B.; Damholt, M.B.; Madsbad, S.; Hilsted, L.M.; Hughes, T.E.; Michelsen, B.K.; Holst, J.J. Determinants of the impaired secretion of glucagon-like peptide-1 in type 2 diabetic patients. J. Clin. Endocrinol. Metab. 2001, 86, 3717–3723. [Google Scholar] [CrossRef]
- Xu, G.; Kaneto, H.; Laybutt, D.R.; Duvivier-Kali, V.F.; Trivedi, N.; Suzuma, K.; King, G.L.; Weir, G.C.; Bonner-Weir, S. Downregulation of GLP-1 and GIP receptor expression by hyperglycemia: Possible contribution to impaired incretin effects in diabetes. Diabetes 2007, 56, 1551–1558. [Google Scholar] [CrossRef] [Green Version]
- Pathak, V.; Vasu, S.; Flatt, P.R.; Irwin, N. Effects of chronic exposure of clonal β-cells to elevated glucose and free fatty acids on incretin receptor gene expression and secretory responses to GIP and GLP-1. Diabetes Obes. Metab. 2014, 16, 357–365. [Google Scholar] [CrossRef]
- Højberg, P.V.; Vilsbøll, T.; Rabøl, R.; Knop, F.K.; Bache, M.; Krarup, T.; Holst, J.J.; Madsbad, S. Four weeks of near-normalisation of blood glucose improves the insulin response to glucagon-like peptide-1 and glucose-dependent insulinotropic polypeptide in patients with type 2 diabetes. Diabetologia 2009, 52, 199–207. [Google Scholar] [CrossRef] [Green Version]
- Piteau, S.; Olver, A.; Kim, S.J.; Winter, K.; Pospisilik, J.A.; Lynn, F.C.; Manhart, S.; DeMuth, H.-U.; Speck, M.; Pederson, R.A.; et al. Reversal of islet GIP receptor down-regulation and resistance to GIP by reducing hyperglycemia in the Zucker rat. Biochem. Biophys. Res. Commun. 2007, 362, 1007–1012. [Google Scholar] [CrossRef]
- Asmar, M.; Tangaa, W.; Madsbad, S.; Hare, K.; Astrup, A.; Flint, A.; Bülow, J.; Holst, J.J. On the role of glucose-dependent insulintropic polypeptide in postprandial metabolism in humans. Am. J. Physiol. Endocrinol. Metab. 2010, 298, 614–621. [Google Scholar] [CrossRef] [Green Version]
- Esposito, K.; Mosca, C.; Brancario, C.; Chiodini, P.; Ceriello, A.; Giugliano, D. GLP-1 receptor agonists and HBA1c target of of >7% in type 2 diabetes: Meta-analysis of randomized controlled trials. Curr. Med. Res. Opin. 2011, 27, 1519–1528. [Google Scholar] [CrossRef] [PubMed]
- Pocai, A. Unraveling oxyntomodulin, GLP1’s enigmatic brother. J. Endocrinol. 2012, 215, 335–346. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amori, R.E.; Lau, J.; Pittas, A.G. Efficacy and safety of incretin therapy in type 2 diabetes: Systematic review and meta-analysis. J. Am. Med Assoc. 2007, 298, 194–206. [Google Scholar] [CrossRef] [PubMed]
- Finan, B.; Tao, M.; Ottaway, N.; Muller, D.T.; Habegger, K.M.; Kirchner, H.; Holland, J.; Hembree, J.; Raver, C.; Lockie, S.H.; et al. Unimolecular dual incretins maximize metabolic benefits in rodents, monkeys, and humans. Sci. Transl. Med. 2013. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coskun, T.; Sloop, K.W.; Loghin, C.; Alsina-Fernandez, J.; Urva, S.; Bokvist, K.B.; Cui, X.; Briere, D.A.; Cabrera, O.; Roell, W.C.; et al. LY3298176, a novel dual GIP and GLP-1 receptor agonist for the treatment of type 2 diabetes mellitus: From discovery to clinical proof of concept. Mol. Metab. 2018, 18, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Lund, A.; Bagger, J.I.; Christensen, M.; Knop, F.K.; Vilsbøll, T. Glucagon and Type 2 Diabetes: The Return of the Alpha Cell. Curr. Diabetes Rep. 2014, 14, 1–7. [Google Scholar] [CrossRef]
- Parker, J.A.; McCullough, K.A.; Field, B.C.T.; Minnion, J.S.; Martin, N.M.; Ghatei, M.A.; Bloom, S.R. Glucagon and GLP-1 inhibit food intake and increase c-fos expression in similar appetite regulating centres in the brainstem and amygdala. Int. J. Obes. 2013, 37, 1391–1398. [Google Scholar] [CrossRef] [Green Version]
- Sadry, S.A.; Drucker, D.J. Emerging combinatorial hormone therapies for the treatment of obesity and T2DM. Nat. Rev. Endocrinol. 2013, 9, 425–433. [Google Scholar] [CrossRef]
- Cegla, J.; Troke, R.C.; Jones, B.; Tharakan, G.; Kenkre, J.; McCullough, K.A.; Lim, C.T.; Parvizi, N.; Hussein, M.; Chambers, E.S.; et al. Coinfusion of low-dose GLP-1 and glucagon in man results in a reduction in food intake. Diabetes 2014, 63, 3711–3720. [Google Scholar] [CrossRef] [Green Version]
- Day, J.W.; Ottaway, N.; Patterson, J.; Gelfanov, V.; Smiley, D.; Gidda, J.; Findeisen, H.; Bruemmer, D.; Drucker, D.J.; Chaudhary, N.; et al. A new glucagon and GLP-1 co-agonist eliminates obesity in rodents. Nat. Chem. Biol. 2009, 5, 749–757. [Google Scholar] [CrossRef]
- Pocai, A.; Carrington, P.E.; Adams, J.R.; Wright, M.; Eiermann, G.; Zhu, L.; Du, X.; Petrov, A.; Lassman, M.E.; Jiang, G.; et al. Glucagon-like peptide 1/glucagon receptor dual agonism reverses obesity in mice. Diabetes 2009, 58, 2258–2266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Day, J.W.; Gelfanov, V.; Smiley, D.; Carrington, P.E.; Eiermann, G.; Chicchi, G.; Erion, M.D.; Gidda, J.; Thornberry, N.A.; Tschöp, M.H.; et al. Optimization of co-agonism at GLP-1 and glucagon receptors to safely maximize weight reduction in DIO-rodents. Biopolymers 2012, 98, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Lynch, A.M.; Pathak, N.; Flatt, Y.E.; Gault, V.A.; O’Harte, F.P.; Irwin, N.; Flatt, P. Comparison of stability, cellular, glucose-lowering and appetite supressing effects of oxyntomodulin analogues modified at the N-terminus. Eur. J. Pharmacol. 2014, 743, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Meek, C.L.; Lewis, H.B.; Reimann, F.; Gribble, F.M.; Park, A.J. The effect of bariatric surgery on gastrointestinal and pancreatic peptide hormones. Peptides 2016, 77, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Laferrère, B. Bariatric surgery and obesity: Influence on the incretins. Int. J. Obes. 2016, 6, 32–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhat, V.K.; Kerr, B.D.; Vasu, S.; Flatt, P.R.; Gault, V.A. A DPP-IV-resistant triple-acting agonist of GIP, GLP-1 and glucagon receptors with potent glucose-lowering and insulinotropic actions in high-fat-fed mice. Diabetologia 2013, 56, 1417–1424. [Google Scholar] [CrossRef] [PubMed]
- Chepurny, O.G.; Bonaccorso, R.L.; Leech, C.A.; Wöllert, T.; Langford, G.M.; Schwede, F.; Roth, C.L.; Doyle, R.P.; Holz, G.G. Chimeric peptide EP45 as a dual agonist at GLP-1 and NPY2R receptors. Sci. Rep. 2018, 8, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Hasib, A.; Ng, M.T.; Khan, D.; Gault, V.A.; Flatt, P.R.; Irwin, N. A novel GLP-1/xenin hybrid peptide improves glucose homeostasis, circulating lipids and restores GIP sensitivity in high fat fed mice. Peptides 2018, 100, 202–211. [Google Scholar] [CrossRef]
- Lu, Y.; Griffen, S.C.; Boulton, D.W.; Leil, T.A. Use of systems pharmacology modeling to elucidate the operating characteristics of SGLT1 and SGLT2 in renal glucose reabsorption in humans. Front. Pharmacol. 2014. [Google Scholar] [CrossRef] [Green Version]
- JLiu, J.; Lee, T.W.; DeFronzo, R.A. Why do SGLT2 inhibitors inhibit only 30–50% of renal glucose reabsorption in humans? Diabetes 2012, 61, 2199–2204. [Google Scholar]
- Busch, R.S.; Kane, M.P. Combination SGLT2 inhibitor and GLP-1 receptor agonist therapy: A complementary approach to the treatment of type 2 diabetes. Postgrad. Med. 2017, 129, 686–697. [Google Scholar] [CrossRef] [PubMed]
- Inzucchi, S.E.; Zinman, B.; Wanner, C.; Ferrari, R.; Fitchett, D.; Hantel, S.; Espadero, R.-M.; Espadero, R.-M.; Woerle, H.-J.; Broedl, U.C.; et al. SGLT-2 inhibitors and cardiovascular risk: Proposed pathways and review of ongoing outcome trials. Diabetes Vasc. Dis. Res. 2015, 12, 90–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zambrowicz, B.; Freiman, J.; Brown, P.M.; Frazier, K.S.; Turnage, A.; Bronner, J.; Ruff, D.; Shadoan, M.; Banks, P.; Mseeh, F.; et al. LX4211, a dual SGLT1/SGLT2 inhibitor, improved glycemic control in patients with type 2 diabetes in a Randomized, placebo-controlled trial. Clin. Pharmacol. Ther. 2012, 92, 158–169. [Google Scholar] [CrossRef] [PubMed]
- Maccari, R.; Del Corso, A.; Paoli, P.; Adornato, I.; Lori, G.; Balestri, F.; Cappiello, M.; Naß, A.; Wolber, G.; Ottanà, R. An investigation on 4-thiazolidinone derivatives as dual inhibitors of aldose reductase and protein tyrosine phosphatase 1B, in the search for potential agents for the treatment of type 2 diabetes mellitus and its complications. Bioorg. Med. Chem. Lett. 2018, 28, 3712–3720. [Google Scholar] [CrossRef]
- Cabrero, A.; Laguna, J.C.; Vázquez, M. Peroxisome proliferator-activated receptors and the control of inflammation. In Curr. Drug Targets. Inflamm. Allergy; 2002; 1, pp. 243–248. Available online: http://www.ncbi.nlm.nih.gov/pubmed/14561188 (accessed on 2 February 2019). [CrossRef]
- Ogata, T.; Miyauchi, T.; Sakai, S.; Irukayama-Tomobe, Y.; Goto, K.; Yamaguchi, I. Stimulation of peroxisome-proliferator-activated receptor alpha (PPAR alpha) attenuates cardiac fibrosis and endothelin-1 production in pressure-overloaded rat hearts. Clin. Sci. 2002, 103, 284–288. [Google Scholar] [CrossRef]
- Tai, E.S.; Collins, D.; Robins, S.J.; O’Connor, J.; Bloomfield, H.; Ordovás, J.M.; Schaefer, E.J.; Brousseau, M.E. The L162V polymorphism at the peroxisome proliferator activated receptor alpha locus modulates the risk of cardiovascular events associated with insulin resistance and diabetes mellitus: The Veterans Affairs HDL Intervention Trial (VA-HIT). Atherosclerosis 2006, 187, 153–160. [Google Scholar] [CrossRef]
- Dent, A.L.; Shaffer, A.L.; Yu, X.; Allman, D.; Staudt, L.M. Control of inflammation, cytokine expression, and germinal center formation by BCL-6. Science 1997, 276, 589–592. [Google Scholar] [CrossRef]
- Takano, H.; Hasegawa, H.; Zou, Y.; Komuro, I. Pleiotropic Actions of PPARg Activators Thiazolidinediones in Cardiovascular Diseases. Curr. Pharm. Des. 2004, 10, 2779–2786. [Google Scholar] [CrossRef]
- Pourcet, B.; Fruchart, J.C.; Staels, B.; Glineur, C. Selective PPAR modulators, dual and pan PPAR agonists: Multimodal drugs for the treatment of Type 2 diabetes and atherosclerosis. Expert Opin. Emerg. Drugs 2006, 11, 379–401. [Google Scholar] [CrossRef]
- Balakumar, P.; Rose, M.; Ganti, S.S.; Krishan, P.; Singh, M. PPAR dual agonists: Are they opening Pandora’s Box? Pharmacol. Res. 2007, 56, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Mamnoor, P.K.; Hegde, P.; Datla, S.R.; Damarla, R.K.B.; Rajagopalan, R.; Chakrabarti, R. Antihypertensive effect of ragaglitazar: A novel PPARα and γ dual activator. Pharmacol. Res. 2006, 54, 129–135. [Google Scholar] [CrossRef]
- Gonzalez, I.C.; Lamar, J.; Iradier, F.; Xu, Y.; Winneroski, L.L.; York, J.; Yumibe, N.; Zink, R.; Montrose-Rafizadeh, C.; Etgen, G.J.; et al. Design and synthesis of a novel class of dual PPARγ/δ agonists. Bioorganic Med. Chem. Lett. 2007, 17, 1052–1055. [Google Scholar] [CrossRef] [PubMed]
- Tenenbaum, A.; Motro, M.; Fisman, E.Z. Dual and pan-peroxisome proliferator-activated receptors (PPAR) co-agonism: The bezafibrate lessons. Cardiovasc. Diabetol. 2005. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stefanski, A.; Majkowska, L. Existing and potential therapeutic approaches targeting peroxisome proliferator-activated receptors in the management of Type 2 diabetes. Expert Opin. Ther. Pat. 2006, 16, 1713–1733. [Google Scholar] [CrossRef]
- Ernst, E. Major Herbs of Ayurveda. Focus Altern. Complement. Ther. 2010, 8, 98. [Google Scholar] [CrossRef]
- Ota, A.; Ulrih, N.P. An overview of herbal products and secondary metabolites used for management of type two diabetes. Front. Pharmacol. 2017. [Google Scholar] [CrossRef]
- Ahmed, I.; Adeghate, E.; Cummings, E.; Sharma, A.K.; Singh, J. Beneficial effects and mechanism of action of Momordica charantia juice in the treatment of streptozotocin-induced diabetes mellitus in rat. Mol. Cell. Biochem. 2004, 261, 63–70. [Google Scholar] [CrossRef]
- Sridhar, M.G.; Vinayagamoorthi, R.; Suyambunathan, V.A.; Bobby, Z.; Selvaraj, N. Bitter gourd (Momordica charantia) improves insulin sensitivity by increasing skeletal muscle insulin-stimulated IRS-1 tyrosine phosphorylation in high-fat-fed rats. Br. J. Nutr. 2008, 99, 806–812. [Google Scholar] [CrossRef] [Green Version]
- Uebanso, T.; Arai, H.; Taketani, Y.; Fukaya, M.; Yamamoto, H.; Mizuno, A.; Uryu, K.; Hada, T.; Takeda, E. Extracts of Momordica charantia suppress postprandial hyperglycemia in rats. J. Nutr. Sci. Vitaminol. 2007, 53, 482–488. [Google Scholar] [CrossRef] [Green Version]
- Nhiem, N.X.; Van Kiem, P.; Van Minh, C.; Ban, N.K.; Cuong, N.X.; Tung, N.H.; Hà, L.M.; Ha, D.T.; Tai, B.H.; Quang, T.H.; et al. α-Glucosidase inhibition properties of cucurbitane-type triterpene glycosides from the fruits of Momordica charantia. Chem. Pharm. Bull. 2010, 58, 720–724. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, H.J.; Lee, Y.-H.; Park, S.K.; Kang, E.S.; Kim, H.-J.; Lee, Y.C.; Choi, C.S.; Park, S.E.; Ahn, C.W.; Cha, B.-S.; et al. Korean red ginseng (Panax ginseng) improves insulin sensitivity and attenuates the development of diabetes in Otsuka Long-Evans Tokushima fatty rats. Metabolism 2009, 58, 1170–1177. [Google Scholar] [CrossRef]
- Mollah, M.L.; Kim, G.-S.; Kim, G.-S.; Moon, H.-K.; Chung, S.-K.; Cheon, Y.-P.; Kim, J.-K.; Kim, K.S. Antiobesity effects of wild ginseng (Panax ginseng C.A. meyer) mediated by PPAR-γ, GLUT4 and LPL in ob/ob mice. Phyther. Res. 2009, 23, 220–225. [Google Scholar] [CrossRef] [PubMed]
- Gloyn, A.L.; Drucker, D.J. Precision medicine in the management of type 2 diabetes. Lancet Diabetes Endocrinol. 2018, 6, 891–900. [Google Scholar] [CrossRef]
- Xie, F.; Chan, J.C.N.; Ma, R.C.W. Precision medicine in diabetes prevention, classification and management. J. Diabetes Investig. 2018, 9, 998–1015. [Google Scholar] [CrossRef] [Green Version]













© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Artasensi, A.; Pedretti, A.; Vistoli, G.; Fumagalli, L. Type 2 Diabetes Mellitus: A Review of Multi-Target Drugs. Molecules 2020, 25, 1987. https://doi.org/10.3390/molecules25081987
Artasensi A, Pedretti A, Vistoli G, Fumagalli L. Type 2 Diabetes Mellitus: A Review of Multi-Target Drugs. Molecules. 2020; 25(8):1987. https://doi.org/10.3390/molecules25081987
Chicago/Turabian StyleArtasensi, Angelica, Alessandro Pedretti, Giulio Vistoli, and Laura Fumagalli. 2020. "Type 2 Diabetes Mellitus: A Review of Multi-Target Drugs" Molecules 25, no. 8: 1987. https://doi.org/10.3390/molecules25081987