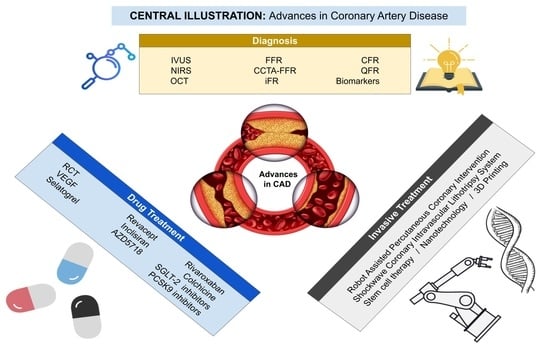
Evolving Diagnostic and Management Advances in Coronary Heart Disease
Abstract
:1. Introduction
2. Diagnoses and Evaluation of Coronary Artery Disease
“But there is a disorder of the breast marked with strong and peculiar symptoms, considerable for the kind of danger belonging to it (...). The seat of it and the sense of strangling and anxiety with which it is attended, may make it not improperly be called angina pectoris.” [2].
2.1. Anatomical Methods
2.1.1. Intravascular Ultrasonography (IVUS)
2.1.2. Near-Infrared Spectroscopy (NIRS)
2.1.3. Optical Coherence Tomography (OCT)
2.2. Functional Methods
2.2.1. Fractional Flow Reserve (FFR)
2.2.2. Computed Tomography Fractional Flow Reserve (CCTA-FFR)
2.2.3. Instant Wave-Free Ratio (iFR)
2.2.4. Coronary Flow Reserve (CFR)
2.2.5. Quantitative Flow Ratio (QFR)
2.2.6. Index of Microcirculatory Resistance (IMR)
2.2.7. Hyperemic Microvascular Resistance (HMR)
2.2.8. Novel Resting Nonhyperemic Pressure Ratios
2.2.9. Cardiac Magnetic Resonance Novelties
2.3. Biomarkers
2.3.1. Pericoronary Fat Attenuation Index (FAI)
2.3.2. MicroRNAs
2.3.3. Polygenic Risk Scores for CAD
3. Novelties in Drug Treatment of Coronary Artery Disease (CAD)
3.1. Reverse Cholesterol Transport
3.2. Vascular Endothelial Growth Factor
3.3. Selatogrel
3.4. Revacept
3.5. Inclisiran
3.6. AZD5718
3.7. Rivaroxaban
3.8. Colchicine
3.9. Sodium-Glucose Cotransporter 2 (SGLT-2) Inhibitors
3.10. PCSK9 Inhibitors
4. Invasive Treatment Novelties
4.1. Robot-Assisted Percutaneous Coronary Intervention
4.2. Shockwave Coronary Intravascular Lithotripsy System
4.3. Stem Cell Therapy for Ischemic Heart Disease
4.4. Nanotechnology
4.5. Three-Dimensional Printing
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Alonso, A.; Beaton, A.Z.; Bittencourt, M.S.; Boehme, A.K.; Buxton, A.E.; Carson, A.P.; Commodore-Mensah, Y.; et al. Heart Disease and Stroke Statistics—2022 Update: A Report From the American Heart Association. Circulation 2022, 145, e153–e639. [Google Scholar] [CrossRef] [PubMed]
- Heberden, W. Some account of a disorder of the breast. Med. Trans. R. Coll. Physicians Lond. 1772, 2, 59–67. [Google Scholar]
- Sones, F.M., Jr.; Shirey, E.K. Cine coronary arteriography. Mod. Concepts Cardiovasc. Dis. 1962, 31, 735. [Google Scholar] [CrossRef] [PubMed]
- Takx, R.A.; Blomberg, B.A.; El Aidi, H.; Habets, J.; de Jong, P.A.; Nagel, E.; Hoffmann, U.; Leiner, T. Diagnostic accuracy of stress myocardial perfusion imaging compared to invasive coronary angiography with fractional flow reserve meta-analysis. Circ. Cardiovasc. Imaging 2015, 8, e002666. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, J.T.; Sheng, X.C.; Feng, Q.; Yin, Y.; Li, Z.; Ding, S.; Pu, J. Pericoronary Fat Attenuation Index Is Associated with Vulnerable Plaque Components and Local Immune-Inflammatory Activation in Patients with Non-ST Elevation Acute Coronary Syndrome. J. Am. Heart Assoc. 2022, 11, e022879. [Google Scholar] [CrossRef]
- Maehara, A.; Mintz, G.S.; Weissman, N.J. Advances in intravascular imaging. Circ. Cardiovasc. Interv. 2009, 2, 482–490. [Google Scholar] [CrossRef] [Green Version]
- Maitre-Ballesteros, L.; Riou, L.; Marliere, S.; Canu, M.; Vautrion, E.; Piliero, N.; Ormezzano, O.; Bouvaist, H.; Broisat, A.; Ghezzi, C.; et al. Coronary Physiology: Delivering Precision Medicine? Rev. Cardiovasc. Med. 2022, 23, 158. [Google Scholar] [CrossRef]
- Yock, P.G.; Linker, D.T.; Angelsen, B.A. Two-dimensional intravascular ultrasound: Technical development and initial clinical experience. J. Am. Soc. Echocardiogr. 1989, 2, 296–304. [Google Scholar] [CrossRef]
- Peng, C.; Wu, H.; Kim, S.; Dai, X.; Jiang, X. Recent Advances in Transducers for Intravascular Ultrasound (IVUS) Imaging. Sensors 2021, 21, 3540. [Google Scholar] [CrossRef]
- Fitzgerald, P.J.; Oshima, A.; Hayase, M.; Metz, J.A.; Bailey, S.R.; Baim, D.S.; Cleman, M.W.; Deutsch, E.; Diver, D.J.; Leon, M.B.; et al. Final results of the can routine ultrasound influence stent expansion (CRUISE) study. Circulation 2000, 102, 523–530. [Google Scholar] [CrossRef]
- Oemrawsingh, P.V.; Mintz, G.S.; Schalij, M.J.; Zwinderman, A.H.; Jukema, J.W.; Wall, E.E. Intravascular ultrasound guidance improves angiographic and clinical outcome of stent implantation for long coronary artery stenoses: Final results of a randomized comparison with angiographic guidance (TULIP Study). Circulation 2003, 107, 62–67. [Google Scholar] [CrossRef] [Green Version]
- Tian, N.-L.; Gami, S.-K.; Ye, F.; Zhang, J.-J.; Liu, Z.-Z.; Lin, S.; Ge, Z.; Shan, S.-J.; You, W.; Chen, L. Angiographic and clinical comparisons of intravascular ultrasound-versus angiography-guided drug-eluting stent implantation for patients with chronic total occlusion lesions: Two-year results from a randomized AIR-CTO study. EuroIntervention 2015, 10, 1409–1417. [Google Scholar] [CrossRef]
- Ahn, J.M.; Kang, S.J.; Mintz, G.S.; Oh, J.H.; Kim, W.J.; Lee, J.Y.; Park, D.W.; Lee, S.W.; Kim, Y.H.; Lee, C.W.; et al. Validation of minimal luminal area measured by intravascular ultrasound for assessment of functionally significant coronary stenosis comparison with myocardial perfusion imaging. JACC Cardiovasc. Interv. 2011, 4, 665–671. [Google Scholar] [CrossRef] [Green Version]
- Park, S.J.; Ahn, J.M.; Kang, S.J.; Yoon, S.H.; Koo, B.K.; Lee, J.Y.; Kim, W.J.; Park, D.W.; Lee, S.W.; Kim, Y.H.; et al. Intravascular ultrasound-derived minimal lumen area criteria for functionally significant left main coronary artery stenosis. JACC Cardiovasc. Interv. 2014, 7, 868–874. [Google Scholar] [CrossRef] [Green Version]
- Stone, G.; Akiko, M.; Lansky, A.; de Bruyne, B.; Cristea, E.; Mintz, G.S.; Mehran, R.; McPherson, J.; Farhat, N.; Marso, S.P.; et al. A Prospective Natural-History Study of Coronary Atherosclerosis. N. Engl. J. Med. 2011, 364, 226–235. [Google Scholar] [CrossRef]
- Hong, S.J.; Mintz, G.S.; Ahn, C.M.; Kim, J.S.; Kim, B.K.; Ko, Y.G.; Kang, T.S.; Kang, W.C.; Kim, Y.H.; Hur, S.H.; et al. Effect of Intravascular Ultrasound-Guided Drug-Eluting Stent Implantation: 5-Year Follow-Up of the IVUS-XPL Randomized Trial. JACC Cardiovasc. Interv. 2020, 13, 62–71. [Google Scholar] [CrossRef]
- Gao, X.; Ge, Z.; Kong, X.-Q.; Kan, J.; Han, L.; Lu, S.; Tian, N.-L.; Lin, S.; Lu, Q.-H.; Wang, Z.-Y.; et al. 3-Year Outcomes of the ULTIMATE Trial Comparing Intravascular Ultrasound Versus Angiography-Guided Drug-Eluting Stent Implantation. J. Am. Coll. Cardiol. Cardiovasc. Interv. 2021, 14, 247–257. [Google Scholar] [CrossRef]
- Ferrari, M.; Mottola, L.; Quaresima, V. Principles, techniques, and limitations of near infrared spectroscopy. Can. J. Appl. Physiol. 2004, 29, 463–487. [Google Scholar] [CrossRef] [Green Version]
- Price, W. Spectroscopy in Science and Technology. Nature 1963, 197, 633. [Google Scholar] [CrossRef]
- Luthria, D.L.; Mukhopadhyay, S.; Lin, L.Z.; Harnly, J.M. A comparison of analytical and data preprocessing methods for spectral fingerprinting. Appl. Spectrosc. 2011, 65, 250–259. [Google Scholar] [CrossRef] [Green Version]
- Johansson, L.E.; Andersson, C.; Ellder, J.; Friberg, P.; Hjalmarson, A.; Hoglund, B.; Irvine, W.M.; Olofsson, H.; Rydbeck, G. Spectral scan of Orion A and IRC+10216 from 72 to 91 GHz. Astron. Astrophys. 1984, 130, 227–256. [Google Scholar] [PubMed]
- National Aeronautics and Space Administration, Science Mission Directorate. Introduction to the Electromagnetic Spectrum. 2010. Available online: http://science.nasa.gov/ems/01_intro (accessed on 26 January 2023).
- Waksman, R.; Di Mario, C.; Torguson, R.; Ali, Z.A.; Singh, V.; Skinner, W.H.; Artis, A.K.; Cate, T.T.; Powers, E.; Kim, C.; et al. Identification of patients and plaques vulnerable to future coronary events with near-infrared spectroscopy intravascular ultrasound imaging: A prospective, cohort study. Lancet 2019, 394, 1629–1637, Erratum in Lancet 2019, 394, 1618. [Google Scholar] [CrossRef] [PubMed]
- Oemrawsingh, R.M.; Cheng, J.M.; García-García, H.M.; van Geuns, R.J.; de Boer, S.P.; Simsek, C.; Kardys, I.; Lenzen, M.J.; van Domburg, R.T.; Regar, E.; et al. Near-infrared spectroscopy predicts cardiovascular outcome in patients with coronary artery disease. J. Am. Coll. Cardiol. 2014, 64, 2510–2518. [Google Scholar] [CrossRef] [PubMed]
- Erlinge, D.; Maehara, A.; Ben-Yehuda, O.; Bøtker, H.E.; Maeng, M.; Kjøller-Hansen, L.; Engstrøm, T.; Matsumura, M.; Crowley, A.; Dressler, O.; et al. mIdentification of vulnerable plaques and patients by intracoronary near-infrared spectroscopy and ultrasound (PROSPECT II): A prospective natural history study. Lancet 2021, 397, 985–995. [Google Scholar] [CrossRef]
- Ono, M.; Kawashima, H.; Hara, H.; Gao, C.; Wang, R.; Kogame, N.; Takahashi, K.; Chichareon, P.; Modolo, R.; Tomaniak, M.; et al. Advances in IVUS/OCT and Future Clinical Perspective of Novel Hybrid Catheter System in Coronary Imaging. Front. Cardiovasc. Med. 2020, 7, 119, Erratum in Front. Cardiovasc. Med. 2020, 7, 594899. [Google Scholar] [CrossRef]
- Ali, Z.A.; Karimi Galougahi, K.; Maehara, A.; Shlofmitz, R.A.; Ben-Yehuda, O.; Mintz, G.S.; Stone, G.W. Intracoronary Optical Coherence Tomography 2018: Current Status and Future Directions. JACC Cardiovasc. Interv. 2017, 10, 2473–2487. [Google Scholar] [CrossRef]
- Bech, G.J.; De Bruyne, B.; Pijls, N.H.; de Muinck, E.D.; Hoorntje, J.C.; Escaned, J.; Stella, P.R.; Boersma, E.; Bartunek, J.; Koolen, J.J.; et al. Fractional flow reserve to determine the appropriateness of angioplasty in moderate coronary stenosis: A randomized trial. Circulation 2001, 103, 2928–2934. [Google Scholar] [CrossRef] [Green Version]
- Pijls, N.H.; Van Gelder, B.; Van der Voort, P.; Peels, K.; Bracke, F.A.; Bonnier, H.J.; el Gamal, M.I. Fractional flow reserve. A useful index to evaluate the influence of an epicardial coronary stenosis on myocardial blood flow. Circulation 1995, 92, 3183–3193. [Google Scholar] [CrossRef]
- Pijls, N.H.; De Bruyne, B.; Peels, K.; Van Der Voort, P.H.; Bonnier, H.J.; Bartunek, J.; Koolen, J.J.; Koolen, J.J. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N. Engl. J. Med. 1996, 334, 1703–1708. [Google Scholar] [CrossRef]
- Tonino, P.A.; De Bruyne, B.; Pijls, N.H.; Siebert, U.; Ikeno, F.; van’t Veer, M.; Klauss, V.; Manoharan, G.; Engstrøm, T.; Oldroyd, K.G.; et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N. Engl. J. Med. 2009, 360, 213–224. [Google Scholar] [CrossRef] [Green Version]
- De Bruyne, B.; Pijls, N.H.; Kalesan, B.; Barbato, E.; Tonino, P.A.; Piroth, Z.; Jagic, N.; Möbius-Winkler, S.; Rioufol, G.; Witt, N.; et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N. Engl. J. Med. 2012, 367, 991–1001, Erratum in N. Engl. J. Med. 2012, 367, 1768. [Google Scholar] [CrossRef] [Green Version]
- Fearon, W.F.; Zimmermann, F.M.; De Bruyne, B.; Piroth, Z.; van Straten, A.H.M.; Szekely, L.; Davidavičius, G.; Kalinauskas, G.; Mansour, S.; Kharbanda, R.; et al. Fractional Flow Reserve-Guided PCI as Compared with Coronary Bypass Surgery. N. Engl. J. Med. 2022, 386, 128–137. [Google Scholar] [CrossRef]
- Lee, J.H.; Hartaigh, B.Ó.; Han, D.; Rizvi, A.; Lin, F.Y.; Min, J.K. Fractional Flow Reserve Measurement by Computed Tomography: An Alternative to the Stress Test. Interv. Cardiol. Rev. 2016, 11, 105–109. [Google Scholar] [CrossRef] [Green Version]
- Min, J.K.; Leipsic, J.; Pencina, M.J.; Berman, D.S.; Koo, B.K.; van Mieghem, C.; Erglis, A.; Lin, F.Y.; Dunning, A.M.; Apruzzese, P.; et al. Diagnostic Accuracy of Fractional Flow Reserve From Anatomic CT Angiography. JAMA 2012, 308, 1237–1245. [Google Scholar] [CrossRef]
- Koo, B.K.; Erglis, A.; Doh, J.H.; Daniels, D.V.; Jegere, S.; Kim, H.S.; Dunning, A.; DeFrance, T.; Lansky, A.; Leipsic, J.; et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenosis Obtained Via Noninvasive Fractional Flow Reserve) study. J. Am. Coll. Cardiol. 2011, 58, 1989–1997. [Google Scholar]
- Nørgaard, B.L.; Leipsic, J.; Gaur, S.; Seneviratne, S.; Ko, B.S.; Ito, H.; Jensen, J.M.; Mauri, L.; De Bruyne, B.; Bezerra, H.; et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: The NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J. Am. Coll. Cardiol. 2014, 63, 1145–1155. [Google Scholar] [CrossRef] [Green Version]
- Douglas, P.S.; De Bruyne, B.; Pontone, G.; Patel, M.R.; Norgaard, B.L.; Byrne, R.A.; Curzen, N.; Purcell, I.; Gutberlet, M.; Rioufol, G.; et al. 1-Year Outcomes of FFRCT-Guided Care in Patients With Suspected Coronary Disease: The PLATFORM Study. J. Am. Coll. Cardiol. 2016, 68, 435–445. [Google Scholar] [CrossRef]
- Curzen, N.; Nicholas, Z.; Stuart, B.; Wilding, S.; Hill, K.; Shambrook, J.; Eminton, Z.; Ball, D.; Barrett, C.; Johnson, L.; et al. Fractional flow reserve derived from computed tomography coronary angiography in the assessment and management of stable chest pain: The FORECAST randomized trial. Eur. Heart J. 2021, 42, 3844–3852. [Google Scholar] [CrossRef]
- Götberg, M.; Christiansen, E.H.; Gudmundsdottir, I.J.; Sandhall, L.; Danielewicz, M.; Jakobsen, L.; Olsson, S.E.; Öhagen, P.; Olsson, H.; Omerovic, E.; et al. Instantaneous Wave-free Ratio versus Fractional Flow Reserve to Guide PCI. N. Engl. J. Med. 2017, 376, 1813–1823. [Google Scholar] [CrossRef] [Green Version]
- Sen, S.; Escaned, J.; Malik, I.S.; Mikhail, G.W.; Foale, R.A.; Mila, R.; Tarkin, J.; Petraco, R.; Broyd, C.; Jabbour, R.; et al. Development and validation of a new adenosine-independent index of stenosis severity from coronary wave-intensity analysis: Results of the ADVISE (ADenosine Vasodilator Independent Stenosis Evaluation) study. J. Am. Coll. Cardiol. 2012, 59, 1392–1402. [Google Scholar] [CrossRef] [Green Version]
- Johnson, N.P.; Jeremias, A.; Zimmermann, F.M.; Adjedj, J.; Witt, N.; Hennigan, B.; Koo, B.-K.; Maehara, A.; Matsunura, M.; Barbato, E.; et al. Continuum of vasodilator stress from rest to contrast medium to adenosine hyperemia for fractional flow reserve assessment. JACC Cardiovasc. Interv. 2016, 9, 757–767. [Google Scholar] [CrossRef] [Green Version]
- Sen, S.; Asress, K.N.; Nijjer, S.; Petraco, R.; Malik, I.S.; Foale, R.A.; Mikhail, G.W.; Foin, N.; Broyd, C.; Hadjiloizou, N.; et al. Diagnostic classification of the instantaneous wave-free ratio is equivalent to fractional flow reserve and is not improved with adenosine administration. Results of CLARIFY (Classification Accuracy of Pressure-Only Ratios Against Indices Using Flow Study). J. Am. Coll. Cardiol. 2013, 61, 1409–1420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelshiker, M.A.; Seligman, H.; Howard, J.P.; Rahman, H.; Foley, M.; Nowbar, A.N.; Rajkumar, C.A.; Shun-Shin, M.J.; Ahmad, Y.; Sen, S.; et al. Coronary flow reserve and cardiovascular outcomes: A systematic review and meta-analysis. Eur. Heart J. 2022, 43, 1582–1593. [Google Scholar] [CrossRef] [PubMed]
- Gould, L.; Lipscomb, K.; Hamilton, G.W. Physiologic basis for assessing critical coronary stenosis. Am. J. Cardiol. 1974, 33, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.D.; Donohue, T.J.; Younis, L.T.; Bach, R.G.; Aguirre, F.V.; Wittry, M.D. Correlation of pharmacologic 99mTc-Sestamibi myocardial perfusion imaging with poststenotic coronary flow reserve in patients with angiographically intermediate coronary artery stenosis. Circulation 1994, 89, 2150–2160. [Google Scholar] [CrossRef] [Green Version]
- Johnson, N.P.; Gould, K.L.; Di Carli, M.F.; Taqueti, V.R. Invasive FFR and Noninvasive CFR in the Evaluation of Ischemia: What Is the Future? J. Am. Coll. Cardiol. 2016, 67, 2772–2788. [Google Scholar] [CrossRef] [Green Version]
- Nakazato, R.; Heo, R.; Leipsic, J.; Min, J.K. CFR and FFR assessment with PET and CTA: Strengths and limitations. Curr. Cardiol. Rep. 2014, 16, 484. [Google Scholar] [CrossRef]
- Indorkar, R.; Kwong, R.Y.; Romano, S.; White, B.E.; Chia, R.C.; Trybula, M.; Evans, K.; Shenoy, C.; Farzaneh-Far, A. Global Coronary Flow Reserve Measured During Stress Cardiac Magnetic Resonance Imaging Is an Independent Predictor of Adverse Cardiovascular Events. JACC Cardiovasc. Imaging 2019, 12, 1686–1695. [Google Scholar] [CrossRef]
- Cortigiani, L.; Rigo, F.; Gherardi, S.; Bovenzi, F.; Molinaro, S.; Picano, E.; Sicari, R. Coronary flow reserve during dipyridamole stress echocardiography predicts mortality. JACC Cardiovasc. Imaging 2012, 5, 1079–1085. [Google Scholar] [CrossRef] [Green Version]
- Albaghdadi, M.; Jaffer, F.A. Wire-Free and Adenosine-Free Fractional Flow Reserve Derived From the Angiogram: A Promising Future Awaiting Outcomes Data. Circ. Cardiovasc. Imaging 2018, 11, e007594. [Google Scholar] [CrossRef] [Green Version]
- Tanigaki, T.; Emori, H.; Kawase, Y.; Kubo, T.; Omori, H.; Shiono, Y.; Sobue, Y.; Shimamura, K.; Hirata, T.; Matsuo, Y.; et al. QFR Versus FFR Derived From Computed Tomography for Functional Assessment of Coronary Artery Stenosis. JACC Cardiovasc. Interv. 2019, 12, 2050–2059. [Google Scholar] [CrossRef]
- Westra, J.; Tu, S.; Winther, S.; Nissen, L.; Vestergaard, M.B.; Andersen, B.K.; Holck, E.N.; Fox Maule, C.; Johansen, J.K.; Andreasen, L.N.; et al. Evaluation of Coronary Artery Stenosis by Quantitative Flow Ratio During Invasive Coronary Angiography: The WIFI II Study (Wire-Free Functional Imaging II). Circ. Cardiovasc. Imaging 2018, 11, e007107. [Google Scholar] [CrossRef]
- Davies, J.E.; Sen, S.; Dehbi, H.M.; Al-Lamee, R.; Petraco, R.; Nijjer, S.S.; Bhindi, R.; Lehman, S.J.; Walters, D.; Sapontis, J.; et al. Use of instantaneous wave-free ratio or fractional flow reserve in PCI. N. Engl. J. Med. 2017, 376, 1824–1834. [Google Scholar] [CrossRef] [Green Version]
- Rodriguez-Leor, O.; de la Torre Hernández, J.M.; García-Camarero, T.; García Del Blanco, B.; López-Palop, R.; Fernández-Nofrerías, E.; Cuellas Ramón, C.; Jiménez-Kockar, M.; Jiménez-Mazuecos, J.; Fernández Salinas, F.; et al. Instantaneous Wave-Free Ratio for the Assessment of Intermediate Left Main Coronary Artery Stenosis: Correlations With Fractional Flow Reserve/Intravascular Ultrasound and Prognostic Implications: The iLITRO-EPIC07 Study. Circ. Cardiovasc. Interv. 2022, 15, 861–871. [Google Scholar] [CrossRef]
- Fearon, W.F.; Balsam, L.B.; Farouque, H.M.; Caffarelli, A.D.; Robbins, R.C.; Fitzgerald, P.J.; Yock, P.G.; Yeung, A.C. Novel index for invasively assessing the coronary microcirculation. Circulation 2003, 107, 3129–3132, Erratum in Circulation 2003, 108, 3165. [Google Scholar] [CrossRef]
- Ng, M.K.; Yeung, A.C.; Fearon, W.F. Invasive assessment of the coronary microcirculation: Superior reproducibility and less hemodynamic dependence of index of microcirculatory resistance compared with coronary flow reserve. Circulation 2006, 113, 2054–2061. [Google Scholar] [CrossRef]
- Aarnoudse, W.; Fearon, W.F.; Manoharan, G.; Geven, M.; van de Vosse, F.; Rutten, M.; De Bruyne, B.; Pijls, N.H.J. Epicardial Stenosis Severity Does Not Affect Minimal Microcirculatory Resistance. Circulation 2004, 110, 2137–2142. [Google Scholar] [CrossRef] [Green Version]
- Kunadian, V.; Chieffo, A.; Camici, P.G.; Berry, C.; Scanned, J.; Maas, A.H.E.M.; Prescott, E.; Karam, N.; Appelman, Y.; Fraccaro, C.; et al. An EAPCI Expert Consensus Document on Ischemia with Non-Obstructive Coronary Arteries in Collaboration with European Society of Cardiology Working Group on Coronary Pathophysiology & Microcirculation Endorsed by Coronary Vasomotor Disorders International. Eur. Heart J. 2020, 41, 3504–3520. [Google Scholar]
- Williams, R.P.; de Waard, G.A.; De Silva, K.; Lumley, M.; Asrress, K.; Arri, S.; Ellis, H.; Mir, A.; Clapp, B.; Chiribiri, A.; et al. Doppler Versus Thermodilution-Derived Coronary Microvascular Resistance to Predict Coronary Microvascular Dysfunction in Patients With Acute Myocardial Infarction or Stable Angina Pectoris. Am. J. Cardiol. 2018, 121, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Amier, R.P.; Teunissen, P.F.A.; Marques, K.M.; Knaapen, P.; van Royen, N. Invasive measurement of coronary microvascular resistance in patients with acute myocardial infarction treated by primary PCI. Heart 2013, 100, 13–20. [Google Scholar] [CrossRef]
- De Waard, G.A.; Nijjer, S.S.; van Lavieren, M.A.; van der Hoeven, N.W.; Petraco, R.; van de Hoef, T.P.; Echavarria-Pinto, M.; Sen, S.; van de Ven, P.M.; Knaapen, P.; et al. Minimal Invasive Microvascular Resistance is a New Index to Assess Microcirculatory Function Independent of Obstructive Coronary Artery Disease. J. Am. Heart Assoc. 2016, 5, e004482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.H.; Lee, J.M.; Park, J.; Choi, K.H.; Hwang, D.; Doh, J.H.; Nam, C.W.; Shin, E.S.; Hoshino, M.; Murai, T.; et al. Prognostic implications of resistive reserve ratio in patients with coronary artery disease. J. Am. Heart Assoc. 2020, 9, e015846. [Google Scholar] [CrossRef] [PubMed]
- Johnson, N.P.; Li, W.; Chen, X.; Hennigan, B.; Watkins, S.; Berry, C.; Fearon, W.F.; Oldroyd, K.G. Diastolic pressure ratio: New approach and validation vs. the instantaneous wave-free ratio. Eur. Heart J. 2019, 40, 2585–2594. [Google Scholar] [CrossRef] [PubMed]
- Van’t Veer, M.; Pijls, N.H.J.; Hennigan, B.; Watkins, S.; Ali, Z.A.; De Bruyne, B.; Zimmermann, F.M.; van Nunen, L.X.; Barbato, E.; Berry, C.; et al. Comparison of different diastolic resting indexes to iFR: Are they all equal? J. Am. Coll. Cardiol. 2017, 70, 3088–3096. [Google Scholar] [CrossRef]
- Antiochos, P.; Ge, Y.; Steel, K.; Chen, Y.Y.; Bingham, S.; Abdullah, S.; Mikolich, J.R.; Arai, A.E.; Bandettini, W.P.; Patel, A.R.; et al. Evaluation of Stress Cardiac Magnetic Resonance Imaging in Risk Reclassification of Patients with Suspected Coronary Artery Disease. JAMA Cardiol. 2020, 5, 1401–1409. [Google Scholar] [CrossRef]
- Ferreira, V.M.; Piechnik, S.K.; Dall’Armellina, E.; Karamitsos, T.D.; Francis, J.M.; Choudhury, R.P.; Friedrich, M.G.; Robson, M.D.; Neubauer, S. Non-contrast T1-mapping detects acute myocardial edema with high diagnostic accuracy: A comparison to T2-weighted cardiovascular magnetic resonance. J. Cardiovasc. Magn. Reson. 2012, 14, 42. [Google Scholar] [CrossRef] [Green Version]
- Antonopoulos, A.S.; Sanna, F.; Sabharwal, N.; Thomas, S.; Oikonomou, E.K.; Herdman, L.; Margaritis, M.; Shirodaria, C.; Kampoli, A.M.; Akoumianakis, I.; et al. Detecting human coronary inflammation by imaging perivascular fat. Sci. Transl. Med. 2017, 9, eaal2658. [Google Scholar] [CrossRef] [Green Version]
- Oikonomou, E.K.; Marwan, M.; Desai, M.Y.; Mancio, J.; Alashi, A.; Hutt Centeno, E.; Thomas, S.; Herdman, L.; Kotanidis, C.P.; Thomas, K.E.; et al. Non-invasive detection of coronary inflammation using computed tomography and prediction of residual cardiovascular risk (the CRISP CT study): A post-hoc analysis of prospective outcome data. Lancet 2018, 392, 929–939. [Google Scholar] [CrossRef] [Green Version]
- Kang, K.; Peng, X.; Luo, J.; Gou, D. Identification of circulating miRNA biomarkers based on global quantitative real-time PCR profiling. J. Anim. Sci. Biotechnol. 2012, 3, 4. [Google Scholar] [CrossRef] [Green Version]
- Ying, S.Y.; Chang, D.C.; Lin, S.L. The microRNA (miRNA): Overview of the RNA genes that modulate gene function. Mol. Biotechnol. 2008, 38, 257–268. [Google Scholar] [CrossRef]
- Ghafouri-Fard, S.; Gholipour, M.; Taheri, M. Role of MicroRNAs in the Pathogenesis of Coronary Artery Disease. Front. Cardiovasc. Med. 2021, 8, 632392. [Google Scholar] [CrossRef]
- Fazmin, I.T.; Achercouk, Z.; Edling, C.E.; Said, A.; Jeevaratnam, K. Circulating microRNA as a Biomarker for Coronary Artery Disease. Biomolecules 2020, 10, 1354. [Google Scholar] [CrossRef]
- Melak, T.; Baynes, H.W. Circulating microRNAs as possible biomarkers for coronary artery disease: A narrative review. Ejifcc 2019, 30, 179–194. [Google Scholar]
- Li, L.; Cai, W.; Ye, Q.; Liu, J.; Li, X.; Liao, X. Comparison of plasma microRNA-1 and cardiac troponin T in early diagnosis of patients with acute myocardial infarction. World J. Emerg. Med. 2014, 5, 182–186. [Google Scholar] [CrossRef] [Green Version]
- Corsten, M.F.; Dennert, R.; Jochems, S.; Kuznetsova, T.; Devaux, Y.; Hofstra, L.; Wagner, D.R.; Staessen, J.A.; Heymans, S.; Schroen, B. Circulating MicroRNA-208b and MicroRNA-499 reflect myocardial damage in cardiovascular disease. Circ. Cardiovasc. Genet. 2010, 3, 499–506. [Google Scholar] [CrossRef]
- Xiao, J.; Shen, B.; Li, J.; Lev, D.; Zhao, Y.; Wang, F.; Xu, J. Serum microRNA-499 and microRNA-208a as biomarkers of acute myocardial infarction. Int. J.Clin. Exp. Med. 2014, 7, 136–141. [Google Scholar]
- Bartel, D.P. MicroRNAs: Genomics, biogenesis, mechanism, and function. Cell 2004, 116, 281–297. [Google Scholar] [CrossRef] [Green Version]
- Sabatine, M.S.; Giugliano, R.P.; Keech, A.C.; Honarpour, N.; Wiviott, S.D.; Murphy, S.A.; Kuder, J.F.; Wang, H.; Liu, T.; Wasserman, S.M.; et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N. Engl. J. Med. 2017, 376, 1713–1722. [Google Scholar] [CrossRef]
- Schwartz, G.G.; Steg, P.G.; Szarek, M.; Bhatt, D.L.; Bittner, V.A.; Diaz, R.; Edelberg, J.M.; Goodman, S.G.; Hanotin, C.; Harrington, R.A.; et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N. Engl. J. Med. 2018, 379, 2097–2107. [Google Scholar] [CrossRef]
- Marston, N.A.; Kamanu, F.K.; Nordio, F.; Gurmu, Y.; Roselli, C.; Sever, P.S.; Pedersen, T.R.; Keech, A.C.; Wang, H.; Lira Pineda, A.; et al. Predicting Benefit From Evolocumab Therapy in Patients With Atherosclerotic Disease Using a Genetic Risk Score: Results From the FOURIER Trial. Circulation 2020, 141, 616–623. [Google Scholar] [CrossRef]
- Damask, A.; Steg, P.G.; Schwartz, G.G.; Szarek, M.; Hagström, E.; Badimon, L.; Chapman, M.J.; Boileau, C.; Tsimikas, S.; Ginsberg, H.N.; et al. Patients With High Genome-Wide Polygenic Risk Scores for Coronary Artery Disease May Receive Greater Clinical Benefit From Alirocumab Treatment in the Odyssey Outcomes Trial. Circulation 2020, 141, 624–636. [Google Scholar] [CrossRef] [PubMed]
- Ford, T.J.; Corcoran, D.; Berry, C. Stable coronary syndromes: Pathophysiology, diagnostic advances and therapeutic need. Heart 2018, 104, 284–292. [Google Scholar] [PubMed]
- Herrmann, J.; Kaski, J.C.; Lerman, A. Coronary microvascular dysfunction in the clinical setting: From the mystery to reality. Eur. Heart J. 2012, 33, 2771–2782. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rader, D.J.; Alexander, E.T.; Weibel, G.L.; Billheimer, J.; Rothblat, G.H. The role of reverse cholesterol transport in animals and humans and relationship to atherosclerosis. J. Lipid Res. 2009, 50, S189–S194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oulmet, M.; Barrett, T.J.; Fisher, E.A. HDL and Reverse Cholesterol Transport: Basic Mechanisms and Their Roles in Vascular Health and Disease. Circ. Res. 2019, 124, 1505–1518. [Google Scholar]
- Brownell, N.; Rohatgi, A. Modulating cholesterol efflux capacity to improve cardiovascular disease. Curr. Opin. Lipidol. 2016, 27, 398. [Google Scholar] [CrossRef]
- Inoue, M.; Itoh, H.; Ueda, M.; Naruko, T.; Kojima, A.; Komatsu, R.; Doi, K.; Ogawa, Y.; Tamura, N.; Takaya, K.; et al. Vascular Endothelial Growth Factor (VEGF) Expression in Human Coronary Atherosclerotic Lesions. Possible Pathophysiological Significance of VEGF in Progression of Atherosclerosis. Circulation 1998, 98, 2108–2116. [Google Scholar] [CrossRef] [Green Version]
- Povsic, T.J.; Henry, T.D.; Ohman, E.M.; Pepine, C.J.; Crystal, R.G.; Rosengart, T.K.; Reinhardt, R.R.; Dittrich, H.C.; Traverse, J.H.; Answini, G.A.; et al. Epicardial delivery of XC001 gene therapy for refractory angina coronary treatment (The EXACT Trial): Rationale, design, and clinical considerations. Am. Heart J. 2021, 241, 38–49. [Google Scholar] [CrossRef]
- Milluzzo, R.P.; Franchina, G.A.; Capodanno, D.; Angiolillo, D.J. Selatogrel, a novel P2Y12 inhibitor: A review of the pharmacology and clinical development. Expert Opin. Investig. Drugs 2020, 29, 537–546. [Google Scholar] [CrossRef]
- Beavers, C.J.; Effoe, S.A.; Dobesh, P.P. Selatogrel: A Novel Subcutaneous P2Y12 Inhibitor. J. Cardiovasc. Pharmacol. 2022, 79, 161–167. [Google Scholar] [CrossRef]
- Sinnaeve, P.; Fahrni, G.; Schelfaut, D.; Spirito, A.; Mueller, C.; Frenoux, J.-M.; Hmissi, A.; Bernaud, C.; Ufer, M.; Moccetti, T.; et al. Subcutaneous Selatogrel Inhibits Platelet Aggregation in Patients With Acute Myocardial Infarction. J. Am. Coll. Cardiol. 2020, 75, 2588–2597. [Google Scholar] [CrossRef]
- Storey, R.F.; Gurbel, P.A.; Ten Berg, J.; Beranud, C.; Dangas, G.D.; Frenoux, J.-M.; Gorog, D.A.; Hmissi, A.; Kunadian, V.; James, S.K.; et al. Pharmacodynamics, pharmacokinetics, and safety of single-dose subcutaneous administration of selatogrel, a novel P2Y12 receptor antagonist, in patients with chronic coronary syndromes. Eur. Heart J. 2020, 41, 3132–3140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schönberger, T.; Ziegler, M.; Borst, O.; Konrad, I.; Nieswandt, B.; Massberg, S.; Ochmann, C.; Jürgens, T.; Seizer, P.; Langer, H.; et al. The dimeric platelet collagen receptor GPVI-Fc reduces platelet adhesion to activated endothelium and preserves myocardial function after transient ischemia in mice. Am. J. Physiol. Cell Physiol. 2012, 303, C757–C766. [Google Scholar] [CrossRef] [PubMed]
- Gensicke, H.; van der Worp, H.B.; Nederkoorn, P.J.; Macdonald, S.; Gaines, P.A.; van der Lugt, A.; Mali, W.P.T.M.; Lyrer, P.A.; Peters, N.; Featherstone, R.L.; et al. Ischemic brain lesions after carotid artery stenting increase future cerebrovascular risk. J. Am. Coll. Cardiol. 2015, 65, 521–529. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ungerer, M.; Li, Z.; Baumgartner, C.; Goebel, S.; Vogelmann, J.; Holthhoff, H.-P.; Gawaz, M.; Münch, G. The GPVI-Fc fusion protein Revacept reduces thrombus formation and improves vascular dysfunction in atherosclerosis without any impact on bleeding times. PLoS ONE 2013, 8, e71193. [Google Scholar] [CrossRef] [Green Version]
- Alberti, S.; Zhang, O.; D’Agostino, I.; Bruno, A.; Tacconelli, S.; Contursi, A.; Guarnieri, S.; Dovizio, M.; Falcone, L.; Ballerini, P.; et al. The antiplatelet agent revacept prevents the increase of systemic thromboxane A2 biosynthesis and neointima hyperplasia. Sci. Rep. 2020, 10, 21420. [Google Scholar] [CrossRef]
- Jamasbi, J.; Megens, R.T.; Bianchini, M.; Münch, G.; Ungerer, M.; Faussner, A.; Sherman, S.; Walker, A.; Goyal, P.; Jung, S.; et al. Differential inhibition of human atherosclerotic platelet-induced platelet activation by dimeric GPVI-Fc and Anti-GPVI antibodies: Functional and imaging studies. J. Am. Coll. Cardiol. 2015, 65, 2404–2415. [Google Scholar] [CrossRef] [Green Version]
- Uphaus, T.; Richards, T.; Welmar, C.; Neugebauer, H.; Poli, S.; Weissenborn, K.; Imray, C.; Michalski, D.; Rashid, H.; Loftus, I.; et al. Revacept, an Inhibitor of Platelet Adhesion in Symptomatic Carotid Stenosis: A Multicenter Randomized Phase II Trial. Stroke 2022, 53, 2718–2729. [Google Scholar] [CrossRef]
- Mayer, K.; Hein-Rothweiler, R.; Shüpke, S.; Janisch, M.; Bernlochner, I.; Ndrepepa, G.; Sibbing, D.; Gori, T.; Borst, O.; Holdenrieder, S.; et al. Efficacy and Safety of Revacept, a Novel Lesion-Directed Competitive Antagonist to Platelet Glycoprotein VI, in Patients Undergoing Elective Percutaneous Coronary Intervention for Stable Ischemic Heart Disease: The Randomized, Double-blind, Placebo-Controlled ISAR-PLASTER Phase 2 Trial. JAMA Cardiol. 2021, 6, 753–761. [Google Scholar]
- Macchi, C.; Sirtori, C.R.; Corsini, A.; Santos, R.D.; Watts, G.F.; Ruscica, M. A new Dawn for managing dyslipidemias: The era of RNA-based therapies. Pharmacol. Res. 2019, 150, 104413. [Google Scholar] [CrossRef]
- Ray, K.K.; Landmesser, U.; Leiter, L.A.; Kallend, D.; Dufour, R.; Karakas, M.; Hall, T.; Troquay, R.P.; Turner, T.; Visseren, F.L.; et al. Two Phase 3 Trials of Inclisiran in Patients with Elevated LDL Cholesterol. N. Engl. J. Med. 2020, 382, 1507–1519. [Google Scholar] [CrossRef]
- Ray, K.K.; Troquay, R.P.T.; Visseren, F.L.J.; Leiter, L.A.; Scott Wright, R.; Vikarunnessa, S.; Talloczy, Z.; Zang, X.; Maheux, P.; Lesogor, A.; et al. Long-term efficacy and safety of inclisiran in patients with high cardiovascular risk and elevated LDL cholesterol (ORION-3): Results from the 4-year open-label extension of the ORION-1 trial. Lancet Diabetes Endocrinol. 2023, 11, 109–119. [Google Scholar] [CrossRef]
- Pettersen, D.; Davidsson, O.; Whatling, C. Recent advances for FLAP inhibitors. Bioorg. Med. Chem. Lett. 2015, 25, 2607–2612. [Google Scholar] [CrossRef]
- Ericsson, H.; Nelander, K.; Lagerstrom-Fermer, M.; Balendran, C.; Bhat, M.; Chialda, L.; Gan, L.M.; Heijer, M.; Kjaer, M.; Lambert, J.; et al. Initial Clinical Experience with AZD5718, a Novel Once Daily Oral 5-Lipoxygenase Activating Protein Inhibitor. Clin. Transl. Sci. 2018, 11, 330–338. [Google Scholar] [CrossRef] [Green Version]
- Prescott, E.; Pernow, J.; Saraste, A.; Åkerblom, A.; Angerås, O.; Erlinge, D.; Grove, E.L.; Hedman, M.; Jensen, L.O.; Svedlund, S.; et al. Design and rationale of FLAVOUR: A phase IIa efficacy study of the 5-lipoxygenase activating protein antagonist AZD5718 in patients with recent myocardial infarction. Contemp. Clin. Trials Commun. 2020, 19, 100629. [Google Scholar] [CrossRef]
- Mega, J.L.; Braunwald, E.; Wiviott, S.D.; Bassand, J.P.; Bhatt, D.L.; Bode, C.; Burton, P.; Cohen, M.; Cook-Bruns, N.; Fox, K.A.; et al. Rivaroxaban in patients with a recent acute coronary syndrome. N. Engl. J. Med. 2012, 366, 9–19. [Google Scholar] [CrossRef] [Green Version]
- Eikelboom, J.W.; Connolly, S.J.; Bosch, J.; Dagenais, G.R.; Hart, R.G.; Shestakovska, O.; Diaz, R.; Alings, M.; Lonn, E.M.; Anand, S.S.; et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N. Engl. J. Med. 2017, 377, 1319–1330. [Google Scholar] [CrossRef]
- Naito, R.; Miyauchi, K.; Yasuda, S.; Kaikita, K.; Akao, M.; Ako, J.; Matoba, T.; Nakamura, M.; Hagiwara, N.; Kimura, K.; et al. Rivaroxaban Monotherapy vs Combination Therapy With Antiplatelets on Total Thrombotic and Bleeding Events in Atrial Fibrillation With Stable Coronary Artery Disease: A Post Hoc Secondary Analysis of the AFIRE Trial. JAMA Cardiol. 2022, 7, 787–794. [Google Scholar] [CrossRef]
- Dasgeb, B.; Kornreich, D.; McGuinn, K.; Okon, L.; Brownell, I.; Sackett, D.L. Colchicine: An ancient drug with novel applications. Br. J. Dermatol. 2018, 178, 350–356. [Google Scholar] [CrossRef]
- Chen, K.; Schenone, A.L.; Borges, N.; Militello, M.; Menon, V. Teaching an old dog new tricks: Colchicine in cardiovascular medicine. Am. J. Cardiovasc. Drugs 2017, 17, 347–360. [Google Scholar] [CrossRef]
- Imazio, M.; Gaita, F. Colchicine for cardiovascular medicine. Future Cardiol. 2016, 12, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Olsen, A.M.; Fosbøl, E.L.; Lindhardsen, J.; Folke, F.; Charlot, M.; Selmer, C.; Bjerring Olesen, J.; Lamberts, M.; Ruwald, M.H.; Køber, L.; et al. Long-Term cardiovascular risk of nonsteroidal anti-inflammatory drug use according to time passed after first-time myocardial infarction: A nationwide cohort study. Circulation 2012, 126, 1955–1963. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vogel, R.A.; Forrester, J.S. Cooling off hot hearts: A specific therapy for vulnerable plaque? J. Am. Coll. Cardiol. 2013, 61, 411–412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giugliano, G.R.; Giugliano, R.P.; Gibson, C.M.; Kuntz, R.E. Meta-Analysis of corticosteroid treatment in acute myocardial infarction. Am. J. Cardiol. 2003, 91, 1055–1059. [Google Scholar] [CrossRef]
- Nidorf, S.M.; Eikelboom, J.W.; Budgeon, C.A.; Thompson, P.L. Low-dose colchicine for secondary prevention of cardiovascular disease. J. Am. Coll. Cardiol. 2013, 61, 404–410. [Google Scholar] [CrossRef] [Green Version]
- Nidorf, S.M.; Fiolet, A.T.L.; Mosterd, A.; Eikelboom, J.W.; Schut, A.; Opstal, T.S.J.; The, S.H.K.; Xu, X.F.; Ireland, M.A.; Lenderink, T.; et al. Colchicine in Patients with Chronic Coronary Disease. N. Engl. J. Med. 2020, 383, 1838–1847. [Google Scholar] [CrossRef]
- Opstal, T.S.J.; van Broekhoven, A.; Fiolet, A.T.L.; Mosterd, A.; Eikelboom, J.W.; Nidorf, S.M.; Thompson, P.L.; Budgeon, C.A.; Bartels, L.; de Nooijer, R.; et al. Long-Term Efficacy of Colchicine in Patients With Chronic Coronary Disease: Insights From LoDoCo2. Circulation 2022, 145, 626–628. [Google Scholar] [CrossRef]
- Tardif, J.C.; Kouz, S.; Waters, D.D.; Bertrand, O.F.; Diaz, R.; Maggioni, A.P.; Pinto, F.J.; Ibrahim, R.; Gamra, H.; Kiwan, G.S.; et al. Efficacy and Safety of Low-Dose Colchicine after Myocardial Infarction. N. Engl. J. Med. 2019, 381, 2497–2505. [Google Scholar] [CrossRef]
- Tong, D.C.; Quinn, S.; Nasis, A.; Hiew, C.; Roberts-Thomson, P.; Adams, H.; Sriamareswaran, R.; Htun, N.M.; Wilson, W.; Stub, D.; et al. Colchicine in Patients With Acute Coronary Syndrome: The Australian COPS Randomized Clinical Trial. Circulation 2020, 142, 1890–1900. [Google Scholar] [CrossRef]
- Imazio, M.; Andreis, A.; Brucato, A.; Adler, Y.; De Ferrari, G.M. Colchicine for acute and chronic coronary syndromes. Heart 2020, 106, 1555–1560. [Google Scholar] [CrossRef]
- Zinman, B.; Wanner, C.; Lachin, J.M.; Fitchett, D.; Bluhmki, E.; Hantel, S.; Mattheus, M.; Devins, T.; Johansen, O.E.; Woerle, H.J.; et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N. Engl. J. Med. 2015, 373, 2117–2128. [Google Scholar] [CrossRef] [Green Version]
- Wiviott, S.D.; Raz, I.; Bonaca, M.P.; Mosenzon, O.; Kato, E.T.; Cahn, A.; Silverman, M.G.; Zelniker, T.A.; Kuder, J.F.; Murphy, S.A.; et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N. Engl. J. Med. 2019, 380, 347–357. [Google Scholar] [CrossRef]
- Perkovic, V.; Jardine, M.J.; Neal, B.; Bompoint, S.; Heerspink, H.J.L.; Charytan, D.M.; Edwards, R.; Agarwal, R.; Bakris, G.; Bull, S.; et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N. Engl. J. Med. 2019, 380, 2295–2306. [Google Scholar] [CrossRef] [Green Version]
- Cannon, C.P.; Pratley, R.; Dagogo-Jack, S.; Mancuso, J.; Huyck, S.; Masiukiewicz, U.; Charbonnel, B.; Frederich, R.; Gallo, S.; Cosentino, F.; et al. Cardiovascular outcomes with ertugliflozin in type 2 diabetes. N. Engl. J. Med. 2020, 383, 1425–1435. [Google Scholar] [CrossRef]
- Heerspink, H.J.L.; Stefánsson, B.V.; Correa-Rotter, R.; Chertow, G.M.; Greene, T.; Hou, F.F.; Mann, J.F.E.; McMurray, J.J.V.; Lindberg, M.; Rossing, P.; et al. Dapagliflozin in patients with chronic kidney disease. N. Engl. J. Med. 2020, 383, 1436–1446. [Google Scholar] [CrossRef]
- McMurray, J.J.V.; Solomon, S.D.; Inzucchi, S.E.; Køber, L.; Kosiborod, M.N.; Martinez, F.A.; Ponikowski, P.; Sabatine, M.S.; Anand, I.S.; Bělohlávek, J.; et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N. Engl. J. Med. 2019, 381, 1995–2008. [Google Scholar] [CrossRef] [Green Version]
- Packer, M.; Anker, S.D.; Butler, J.; Filippatos, G.; Pocock, S.J.; Carson, P.; Januzzi, J.; Verma, S.; Tsutsui, H.; Brueckmann, M.; et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N. Engl. J. Med. 2020, 383, 1413–1424. [Google Scholar] [CrossRef]
- Bhatt, D.L.; Szarek, M.; Steg, P.G.; Cannon, C.P.; Leiter, L.A.; McGuire, D.K.; Lewis, J.B.; Riddle, M.C.; Voors, A.A.; Metra, M.; et al. Sotagliflozin in patients with diabetes and recent worsening heart failure. N. Engl. J. Med. 2021, 384, 117–128. [Google Scholar] [CrossRef]
- Bhatt, D.L.; Szarek, M.; Pitt, B.; Cannon, B.P.; Leiter, L.A.; McGuire, D.K.; Lewis, J.B.; Riddle, M.C.; Inzucchi, S.E.; Kosiborod, M.N.; et al. Sotagliflozin in patients with diabetes and chronic kidney disease. N. Engl. J. Med. 2021, 384, 129–139. [Google Scholar] [CrossRef]
- Anker, S.D.; Butler, J.; Filippatos, G.; Ferreira, J.P.; Bocchi, E.; Böhm, M.; Brunner-La Rocca, H.P.; Choi, D.J.; Chopra, V.; Chuquiure-Valenzuela, E.; et al. Empagliflozin in heart failure with a preserved ejection fraction. N. Engl. J. Med. 2021, 385, 1451–1461. [Google Scholar] [CrossRef]
- Udell, J.A.; Jones, W.S.; Petrie, M.C.; Harrington, J.; Anker, S.D.; Bhatt, D.L.; Hernandez, A.F.; Butler, J. Sodium Glucose Cotransporter-2 Inhibition for Acute Myocardial Infarction: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2022, 79, 2058–2068. [Google Scholar] [CrossRef] [PubMed]
- Von Lewinski, D.; Kolesnik, E.; Tripolt, N.J.; Pferschy, P.N.; Benedikt, M.; Wallner, M.; Alber, H.; Berger, R.; Lichtenauer, M.; Saely, C.H.; et al. Empagliflozin in acute myocardial infarction: The EMMY trial. Eur. Heart J. 2022, 43, 4421–4432. [Google Scholar] [CrossRef] [PubMed]
- Harrington, J.; Udell, J.A.; Jones, W.S.; Anker, S.D.; Bhatt, D.L.; Petrie, C.; Vedin, O.; Sumin, M.; Zwiener, I.; Hernandez, A.F.; et al. Empagliflozin in patients post myocardial infarction rationale and design of the EMPACT-MI trial. Am. Heart J. 2022, 253, 86–98. [Google Scholar] [CrossRef] [PubMed]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337, Erratum in Eur. Heart J. 2022, 43, 4468. [Google Scholar] [CrossRef]
- Cho, L.; Rocco, M.; Colquhoun, D.; Sullivan, D.; Rosenson, R.S.; Dent, R.; Xue, A.; Scott, R.; Wasserman, S.M.; Stroes, E. Clinical Profile of Statin Intolerance in the Phase 3 GAUSS-2 Study. Cardiovasc. Drugs Ther. 2016, 30, 297–304. [Google Scholar] [CrossRef]
- Erviti, J.; Wright, J.; Bassett, K.; Ben-Eltriki, M.; Jauca, C.; Saiz, L.C.; Leache, L.; Gutiérrez-Valencia, M.; Perry, T.L. Restoring mortality data in the FOURIER cardiovascular outcomes trial of evolocumab in patients with cardiovascular disease: A reanalysis based on regulatory data. BMJ Open 2022, 12, e060172. [Google Scholar] [CrossRef]
- Goldstein, J.A.; Balter, S.; Cowley, M.; Hodgson, J.; Klein, L.W.; Interventional Committee of the Society of Cardiovascular Intervention. Occupational hazards of interventional cardiologists: Prevalence of orthopedic health problems in contemporary practice. Catheter Cardiovasc. Interv. 2004, 63, 407–411. [Google Scholar] [CrossRef]
- Chakravartti, J.; Rao, S.V. Robotic Assisted Percutaneous Coronary Intervention: Hype or Hope? J. Am. Heart Assoc. 2019, 8, e012743. [Google Scholar] [CrossRef]
- Maor, E.; Eleid, M.F.; Gulati, R.; Lerman, A.; Sandhu, G.S. Current and future use of robotic devices to perform percutaneous coronary interventions: A review. J. Am. Heart Assoc. 2017, 6, e006239. [Google Scholar] [CrossRef]
- Weisz, G.; Metzger, D.C.; Caputo, R.P.; Delgado, J.A.; Marshall, J.J.; Vetrovec, G.W.; Reisman, M.; Waksman, R.; Granada, J.F.; Novack, V.; et al. Safety and feasibility of robotic percutaneous coronary intervention PRECISE (percutaneous robotically-enhanced coronary intervention) study. J. Am. Coll. Cardiol. 2013, 61, 1596–1600. [Google Scholar] [CrossRef] [Green Version]
- Mahmud, E.; Naghi, J.; Ang, L.; Harrison, J.; Behnamfar, O.; Pourdjabbar, A.; Reeves, R.; Patel, M. Demonstration of the safety and feasibility of robotically assisted percutaneous coronary intervention in complex coronary lesions: Results of the CORA-PCI study (Complex Robotically Assisted Percutaneous Coronary Intervention). JACC Cardiovasc. Interv. 2017, 10, 1320–1327. [Google Scholar] [CrossRef]
- Madder, R.D.; VanOosterhout, S.M.; Jacoby, M.E.; Collins, J.S.; Borgman, A.S.; Mulder, A.N.; Elmore, M.A.; Campbell, J.L.; McNamara, R.F.; Wohns, D.H. Percutaneous coronary intervention using a combination of robotics and telecommunications by an operator in a separate physical location from the patient: An early exploration into the feasibility of telestenting (the REMOTE-PCI study). EuroIntervention 2017, 12, 1569–1576. [Google Scholar] [CrossRef] [Green Version]
- Madder, R.D.; VanOosterhout, S.; Mulder, A.; Bush, J.; Martin, S.; Rash, A.; Tan, J.M.; Parker, J.; Li, Y.; Kottenstette, N.; et al. Feasibility of robotic telestenting over long geographic distances a pre-clinical ex vivo and in vivo study. EuroIntervention 2019, 15, e510–e512. [Google Scholar] [CrossRef] [Green Version]
- Mori, S.; Yasuda, S.; Kataoka, Y.; Morii, I.; Kawamura, A.; Miyazaki, S. Significant association of coronary artery calcification in stent delivery route with restenosis after sirolimus-eluting stent implantation. Circ. J. 2009, 73, 1856–1863. [Google Scholar] [CrossRef] [Green Version]
- Wiemer, M.; Butz, T.; Schmidt, W.; Schmitz, K.P.; Horstkotte, D.; Langer, C. Scanning electron microscopic analysis of different drug eluting stents after failed implantation: From nearly undamaged to major damaged polymers. Catheter Cardiovasc. Interv. 2010, 75, 905–911. [Google Scholar] [CrossRef]
- Tzafriri, A.R.; Garcia-Polite, F.; Zani, B.; Stanley, J.; Muraj, B.; Knutson, J.; Kohler, R.; Markham, P.; Nikanorov, A.; Edelman, E.R. Calcified plaque modification alters local drug delivery in the treatment of peripheral atherosclerosis. J. Control. Release 2017, 264, 203–210. [Google Scholar] [CrossRef] [Green Version]
- Kobayashi, Y.; Okura, H.; Kume, T.; Yamada, R.; Kobayashi, Y.; Fukuhara, K.; Koyama, T.; Nezuo, S.; Neishi, Y.; Hayashida, A.; et al. Impact of target lesion coronary calcification on stent expansion. Circ. J. 2014, 78, 2209–2214. [Google Scholar] [CrossRef] [Green Version]
- Chambers, J.W.; Feldman, R.L.; Himmelstein, S.I.; Bhatheja, R.; Villa, A.E.; Strickman, N.E.; Shlofmitz, R.A.; Dulas, D.D.; Arab, D.; Khanna, P.K.; et al. Pivotal trial to evaluate the safety and efficacy of the orbital atherectomy system in treating de novo, severely calcified coronary lesions (ORBIT II). J. Am. Coll. Cardiol. Cardiovasc. Interv. 2014, 7, 510–518. [Google Scholar] [CrossRef] [Green Version]
- Lee, M.; Généreux, P.; Shlofmitz, R.; Phillipson, D.; Anose, B.M.; Martinsen, B.J.; Himmelstein, S.I.; Chambers, J.W. Orbital atherectomy for treating de novo severely calcified coronary narrowing (1-year results from the pivotal ORBIT II trial). Am. J. Cardiol. 2015, 115, 1685–1690. [Google Scholar]
- Yamamoto, M.H.; Maehara, A.; Karimi Galougahi, K.; Mintz, G.S.; Parviz, Y.; Kim, S.S.; Koyama, K.; Amemiya, K.; Kim, S.Y.; Ishida, M.; et al. Mechanisms of orbital versus rotational atherectomy plaque modification in severely calcified lesions assessed by optical coherence tomography. J. Am. Coll. Cardiol. Cardiovasc. Interv. 2017, 10, 2584–2586. [Google Scholar] [CrossRef]
- De Waha, S.; Allali, A.; Büttner, H.J.; Toelg, R.; Geist, V.; Neumann, F.J.; Khattab, A.A.; Richardt, G.; Abdel-Wahab, M. Rotational atherectomy before paclitaxel-eluting stent implantation in complex calcified coronary lesions: Two-year clinical outcome of the randomized ROTAXUS trial. Catheter Cardiovasc. Interv. 2016, 87, 691–700. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Wahab, M.; Richardt, G.; Joachim Büttner, H.; Toelg, R.; Geist, V.; Meinertz, T.; Schofer, J.; King, L.; Neumann, F.J.; Khattab, A.A. High-speed rotational atherectomy before paclitaxel-eluting stent implantation in complex calcified coronary lesions: The randomized ROTAXUS (Rotational Atherectomy Prior to Taxus Stent Treatment for Complex Native Coronary Artery Disease) trial. J. Am. Coll. Cardiol. Cardiovasc. Interv. 2013, 6, 10–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dippel, E.J.; Kereiakes, D.J.; Tramuta, D.A.; Broderick, T.M.; Shimshak, T.M.; Roth, E.M.; Hattemer, C.R.; Runyon, J.P.; Whang, D.D.; Schneider, J.F.; et al. Coronary perforation during percutaneous coronary intervention in the era of abciximab platelet glycoprotein Iib/IIIa blockade: An algorithm for percutaneous management. Catheter Cardiovasc. Interv. 2001, 52, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Dini, C.S.; Tomberli, B.; Mattesini, A.; Ristalli, F.; Valente, S.; Stolcova, M.; Meucci, F.; Baldereschi, G.; Fanelli, F.; Shlofmitz, R.A.; et al. Intravascular lithotripsy for calcific coronary and peripheral artery stenoses. EuroIntervention 2019, 15, 714–721. [Google Scholar] [CrossRef] [Green Version]
- Yeoh, J.; Hill, J. Intracoronary lithotripsy for the treatment of calcified plaque. Interv. Cardiol. Clin. 2019, 8, 411–424. [Google Scholar] [CrossRef]
- Brinton, T.J.; Ali, Z.A.; Hill, J.M.; Meredith, I.T.; Maehara, A.; Illindala, U.; Lansky, A.; Götberg, M.; Van Mieghem, N.M.; Whitbourn, R.; et al. Feasibility of Shockwave coronary intravascular lithotripsy for the treatment of calcified coronary stenoses: First description. Circulation 2019, 139, 834–836. [Google Scholar] [CrossRef]
- Ali, Z.A.; Nef, H.; Escaned, J.; Werner, N.; Banning, A.P.; Hill, J.M.; De Bruyne, B.; Montorfano, M.; Lefevre, T.; Stone, G.W.; et al. Safety and effectiveness of coronary intravascular lithotripsy for treatment of severely calcified coronary stenoses: The disrupt CAD II study. Circ. Cardiovasc. Interv. 2019, 12, e008434. [Google Scholar] [CrossRef]
- Hill, J.M.; Kereiakes, D.J.; Shlofmitz, R.A.; Klein, A.J.; Riley, R.F.; Price, M.J.; Herrmann, H.C.; Bachinsky, W.; Waksman, R.; Stone, G.W.; et al. Intravascular lithotripsy for treatment of severely calcified coronary artery disease: The Disrupt CAD III study. J. Am. Coll. Cardiol. 2020, 76, 2635–2646. [Google Scholar] [CrossRef]
- Saito, S.; Yamazaki, S.; Takahashi, A.; Namiki, A.; Kawasaki, T.; Otsuji, S.; Nakamura, S.; Shibata, Y.; Disrupt CAD IV Investigators. Intravascular lithotripsy for vessel preparation in severely calcified coronary arteries prior to stent placement: Primary outcomes from the Japanese Disrupt CAD IV study. Circ. J. 2021, 85, 826–833. [Google Scholar] [CrossRef]
- Kereiakes, D.J.; Di Mario, C.; Riley, R.F.; Fajadet, J.; Shlofmitz, R.A.; Saito, S.; Ali, Z.A.; Klein, A.J.; Price, M.J.; Hill, J.M.; et al. Intravascular Lithotripsy for Treatment of Calcified Coronary Lesions: Patient-Level Pooled Analysis of the Disrupt CAD Studies. JACC Cardiovasc. Interv. 2021, 14, 1337–1348. [Google Scholar] [CrossRef]
- Terashivili, M.; Bosnjak, Z.J. Stem Cell Therapies in Cardiovascular Disease. J. Cardiothorac. Vasc. Anesth 2019, 33, 209–222. [Google Scholar] [CrossRef]
- Yu, H.; Lu, K.; Zhu, J.; Wang, J. Stem cell therapy for ischemic heart diseases. Br. Med. Bull. 2017, 121, 135–154. [Google Scholar] [CrossRef] [Green Version]
- Fernandes, S.; Chong, J.J.H.; Paige, S.L.; Iwata, M.; Torok-Storb, B.; Keller, G.; Reinecke, H.; Murry, C.E. Comparison of Human Embryonic Stem Cell-Derived Cardiomyocytes, Cardiovascular Progenitors, and Bone Marrow Mononuclear Cells for Cardiac Repair. Stem Cell Rep. 2015, 5, 753–762. [Google Scholar] [CrossRef] [Green Version]
- Fisher, S.A.; Zhang, H.; Doree, C.; Mathur, A.; Martin-Rendon, E. Stem cell treatment for acute myocardial infarction. Cochrane Database Syst. Rev. 2015, 9, CD006536. [Google Scholar] [CrossRef]
- Malliaras, K.; Makkar, R.R.; Smith, R.R.; Cheng, K.; Wu, E.; Bonow, R.O.; Marban, L.; Mendizabal, A.; Cingolani, E.; Johnston, P.V.; et al. Intracoronary cardiosphere-derived cells after myocardial infarction: Evidence of therapeutic regeneration in the final 1-year results of the CADUCEUS trial (CArdiosphere-Derived aUtologous stem CElls to reverse ventricUlar dySfunction). J. Am. Coll. Cardiol. 2014, 63, 110–122. [Google Scholar] [CrossRef] [Green Version]
- Maguire, G. Stem cell therapy without the cells. Commun. Integr. Biol. 2013, 6, e26631. [Google Scholar] [CrossRef]
- Haynesworth, S.E.; Baber, M.A.; Caplan, A.I. Cytokine expression by human marrow-derived mesenchymal progenitor cells in vitro: Effects of dexamethasone and IL-1 alpha. J. Cell. Physiol. 1996, 166, 585–592. [Google Scholar] [CrossRef]
- Patschan, D.; Plotkin, M.; Goligorsky, M.S. Therapeutic use of stem and endothelial progenitor cells in acute renal injury: Ça ira. Curr. Opin. Pharmacol. 2006, 6, 176–183. [Google Scholar] [CrossRef]
- Tögel, F.; Hu, Z.; Weiss, K. Administered mesenchymal stem cells protect against ischemic acute renal failure through differentiation-independent mechanisms. Am. J. Physiol. Ren. Physiol. 2005, 289, 31–42. [Google Scholar] [CrossRef] [Green Version]
- Gnecchi, M.; He, H.; Noiseux, N.; Liang, O.D.; Zhang, L.; Morello, F.; Mu, H.; Melo, L.G.; Pratt, R.E.; Ingwall, J.S.; et al. Evidence supporting paracrine hypothesis for Akt-modified mesenchymal stem cell-mediated cardiac protection and functional improvement. FASEB J. 2006, 20, 661–669. [Google Scholar] [CrossRef]
- Timmers, L.; Lim, S.K.; Arslan, F.; Armstrong, J.S.; Hoefer, I.E.; Doevendans, P.A.; Piek, J.J.; El Oakley, R.M.; Choo, A.; Lee, C.N.; et al. Reduction of myocardial infarct size by human mesenchymal stem cell conditioned medium. Stem Cell Res. 2008, 1, 129–137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gnecchi, M.; Zhang, Z.; Ni, A.; Dzau, V.J. Paracrine mechanisms in adult stem cell signaling and therapy. Circ. Res. 2008, 103, 1204–1219. [Google Scholar] [CrossRef] [PubMed]
- Davidson, S.M.; Takov, K.; Yellon, D.M. Exosomes and Cardiovascular Protection. Cardiovasc. Drugs Ther. 2017, 31, 77–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barile, L.; Lionetti, V.; Cervio, E.; Matteucci, M.; Gherghiceanu, M.; Popescu, L.M.; Torre, T.; Siclari, F.; Moccetti, T.; Vassalli, G. Extracellular vesicles from human cardiac progenitor cells inhibit cardiomyocyte apoptosis and improve cardiac function after myocardial infarction. Cardiovasc. Res. 2014, 103, 530–541. [Google Scholar] [CrossRef]
- Gray, W.D.; French, K.M.; Ghosh-Choudhary, S.; Maxwell, J.T.; Brown, M.E.; Platt, M.O.; Searles, C.D.; Davis, M.E. Identification of Therapeutic Covariant MicroRNA Clusters in Hypoxia-Treated Cardiac Progenitor Cell Exosomes Using Systems Biology. Circ. Res. 2015, 116, 255–263. [Google Scholar] [CrossRef] [Green Version]
- Karimi, M.; Zare, H.; Bakhshian Nik, A.; Yazdani, N.; Hamrang, M.; Mohamed, E.; Sahandi Zangabad, P.; Moosavi Basri, S.M.; Bakhtiari, L.; Hamblin, M.R. Nanotechnology in diagnosis and treatment of coronary artery disease. Nanomedicine 2016, 11, 513–530. [Google Scholar] [CrossRef]
- Lewis, D.R.; Kamisoglu, K.; York, A.W.; Moghe, P.V. Polymer-based therapeutics: Nanoassemblies and nanoparticles future for management of atherosclerosis. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2011, 3, 400–420. [Google Scholar] [CrossRef]
- Flores, A.M.; Ye, J.; Jarr, K.U.; Hosseini-Nassab, N.; Smith, B.R.; Leeper, N.J. Nanoparticle Therapy for Vascular Diseases. Arterioscler. Thromb. Vasc. Biol. 2019, 39, 635–646. [Google Scholar] [CrossRef]
- Doshi, N.; Prabhakarpandian, B.; Rea-Ramsey, A.; Pant, K.; Sundaram, S.; Mitragotri, S. Flow and adhesion of drug carriers in blood vessels depend on their shape: A study using model synthetic microvascular networks. J. Control. Release 2010, 146, 196–200. [Google Scholar] [CrossRef] [Green Version]
- Gupta, A.S. Nanomedicine approaches in vascular disease: A review. Nanomedicine 2011, 7, 763–779. [Google Scholar] [CrossRef]
- Srinivasan, R.; Marchant, R.E.; Gupta, A.S. In vitro and in vivo platelet targeting by cyclic RGD-modified liposomes. J. Biomed. Mater. Res. Part A 2010, 93, 1004–1015. [Google Scholar]
- Reddy, M.K.; Vasir, J.K.; Sahoo, S.K.; Jain, T.K.; Yallapu, M.M.; Labhasetwar, V. Inhibition of apoptosis through localized delivery of rapamycin-loaded nanoparticles prevented neointimal hyperplasia and reendothelialized injured artery. Circulation 2008, 1, 209–216. [Google Scholar] [CrossRef] [Green Version]
- Masuda, S.; Nakano, K.; Funakoshi, K.; Zhao, G.; Meng, W.; Kimura, S.; Matoba, T.; Miyagawa, M.; Iwata, E.; Sunagawa, K.; et al. Imatinib mesylate-incorporated nanoparticle-eluting stent attenuates in-stent neointimal formation in porcine coronary arteries. J. Atheroscl. Thromb. 2011, 18, 1043–1053. [Google Scholar] [CrossRef] [Green Version]
- Bozsak, F.; Gonzalez-Rodriguez, D.; Sternberger, Z.; Belitz, P.; Bewley, T.; Chomaz, J.M.; Barakat, A.I. Optimization of drug delivery by drug-eluting stents. PLoS ONE 2015, 10, e0130182. [Google Scholar] [CrossRef] [Green Version]
- Yu, M.; Xu, B.; Kandzari, D.E.; Wu, Y.; Yan, H.; Chen, J.; Qian, J.; Qiao, S.; Yang, Y.; Gao, R.L. First report of a novel polymer-free dual-drug eluting stent in de novo coronary artery disease: Results of the first in human BICARE trial. Catheter Cardiovasc. Interv. 2014, 83, 405–411. [Google Scholar] [CrossRef]
- Kim, T.G.; Lee, Y.; Park, T.G. Controlled gene-eluting metal stent fabricated by bio-inspired surface modification with hyaluronic acid and deposition of DNA/PEI polyplexes. Int. J. Pharm. 2010, 384, 181–188. [Google Scholar] [CrossRef]
- Paul, A.; Shao, W.; Shum-Tim, D.; Prakash, S. The attenuation of restenosis following arterial gene transfer using carbon nanotube coated stent incorporating TAT/DNA (Ang1+Vegf) nanoparticles. Biomaterials 2012, 33, 7655–7664. [Google Scholar] [CrossRef]
- Joo, J.N.H.; Nam, S.H.; Nam, S.H.; Baek, I.; Park, J.-S. Thermal process for enhancing mechanical strength of PLGA nanoparticle layers on coronary stents. Bull. Korean Chem. Soc. 2009, 30, 1985–1988. [Google Scholar]
- Kamaly, N.; Fredman, G.; Fojas, J.J.; Subramanian, M.; Choi, W.I.; Zepeda, K.; Vilos, C.; Yu, M.; Gadde, S.; Wu, J.; et al. Targeted interleukin-10 nanotherapeutics developed with a microfluidic chip enhance resolution of inflammation in advanced atherosclerosis. ACS Nano 2016, 10, 5280–5292. [Google Scholar] [CrossRef] [Green Version]
- Sager, H.B.; Dutta, P.; Dahlman, J.E.; Hulsmans, M.; Courties, G.; Sun, Y.; Heidt, T.; Vinegoni, C.; Borodovsky, A.; Fitzgerald, K.; et al. RNAi targeting multiple cell adhesion molecules reduces immune cell recruitment and vascular inflammation after myocardial infarction. Sci. Transl. Med. 2016, 8, 342ra80. [Google Scholar] [CrossRef] [Green Version]
- Winter, P.M.; Caruthers, S.D.; Zhang, H.; Williams, T.A.; Wickline, S.A.; Lanza, G.M. Antiangiogenic synergism of integrin-targeted fumagillin nanoparticles and atorvastatin in atherosclerosis. JACC Cardiovasc. Imaging 2008, 1, 624–634. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lewis, D.R.; Petersen, L.K.; York, A.W.; Zablocki, K.R.; Joseph, L.B.; Kholodovych, V.; Prud’homme, R.K.; Uhrich, K.E.; Moghe, P.V. Sugar-based amphiphilic nanoparticles arrest atherosclerosis in vivo. Proc. Natl. Acad. Sci. USA 2015, 112, 2693–2698. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duivenvoorden, R.; Tang, J.; Cormode, D.P.; Mieszawska, A.J.; Izquierdo-Garcia, D.; Ozcan, C.; Otten, M.J.; Zaidi, N.; Lobatto, M.E.; van Rijs, S.M.; et al. A statin-loaded reconstituted high-density lipoprotein nanoparticle inhibits atherosclerotic plaque inflammation. Nat. Commun. 2014, 5, 3065. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawata, H.; Uesugi, Y.; Soeda, T.; Takemoto, Y.; Sung, J.H.; Umaki, K.; Kato, K.; Ogiwara, K.; Nogami, K.; Ishigami, K.; et al. A new drug delivery system for intravenous coronary thrombolysis with thrombus targeting and stealth activity recoverable by ultrasound. J. Am. Coll. Cardiol. 2012, 60, 2550–2557. [Google Scholar] [CrossRef] [Green Version]
- Pawlowski, C.L.; Li, W.; Sun, M.; Ravichandran, K.; Hickman, D.; Kos, C.; Kaur, G.; Sen Gupta, A. Platelet microparticle-inspired clot-responsive nanomedicine for targeted fibrinolysis. Biomaterials 2017, 128, 94–108. [Google Scholar] [CrossRef]
- Bi, F.; Zhang, J.; Su, Y.; Tang, Y.C.; Liu, J.N. Chemical conjugation of urokinase to magnetic nanoparticles for targeted thrombolysis. Biomaterials 2009, 30, 5125–5130. [Google Scholar] [CrossRef]
- Palekar, R.U.; Jallouk, A.P.; Myerson, J.W.; Pan, H.; Wickline, S.A. Inhibition of thrombin with PPACK-nanoparticles restores disrupted endothelial barriers and attenuates thrombotic risk in experimental atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2016, 36, 446–455. [Google Scholar] [CrossRef] [Green Version]
- Ma, Y.H.; Wu, S.Y.; Wu, T.; Chang, Y.J.; Hua, M.Y.; Chen, J.P. Magnetically targeted thrombolysis with recombinant tissue plasminogen activator bound to polyacrylic acid-coated nanoparticles. Biomaterials 2009, 30, 3343–3351. [Google Scholar] [CrossRef]
- Zhou, J.; Guo, D.; Zhang, Y.; Wu, W.; Ran, H.; Wang, Z. Construction and evaluation of Fe3O4-based PLGA nanoparticles carrying rtPA used in the detection of thrombosis and in targeted thrombolysis. ACS Appl. Mater. Interfaces 2014, 6, 5566–5576. [Google Scholar] [CrossRef]
- Marsh, J.N.; Senpan, A.; Hu, G.; Scott, M.J.; Gaffney, P.J.; Wickline, S.A.; Lanza, G.M. Fibrin-targeted perfluorocarbon nanoparticles for targeted thrombolysis. Nanomedicine 2007, 2, 533–543. [Google Scholar] [CrossRef]
- Marsh, J.N.; Hu, G.; Scott, M.J.; Zhang, H.; Goette, M.J.; Gaffney, P.J.; Caruthers, S.D.; Wickline, S.A.; Abendschein, D.; Lanza, G.M. A fibrin-specific thrombolytic nanomedicine approach to acute ischemic stroke. Nanomedicine 2011, 6, 605–615. [Google Scholar] [CrossRef] [Green Version]
- Farooqi, K.M.; Sengupta, P.P. Echocardiography and three-dimensional printing: Sound ideas to touch a heart. J. Am. Soc. Echocardiogr. 2015, 28, 398–403. [Google Scholar] [CrossRef]
- Vukicevic, M.; Mosadegh, B.; Min, J.K.; Little, S.H. Cardiac 3D Printing and its Future Directions. JACC Cardiovasc. Imaging 2017, 10, 171–184. [Google Scholar] [CrossRef]
- Lindquist, E.M.; Gosnell, J.M.; Khan, S.K.; Byl, J.L.; Zhou, W.; Jiang, J.; Vettukattil, J.J. 3D printing in cardiology: A review of applications and roles for advanced cardiac imaging. Ann. 3D Print. Med. 2021, 4, 100034. [Google Scholar] [CrossRef]
- Byrne, N.; Velasco, F.M.; Tandon, A.; Valverde, I.; Hussain, T. A systematic review of image segmen- tation methodology, used in the additive manufacture of patient-specific 3D printed models of the cardiovascular system. JRSM Cardiovasc. Dis. 2016, 5, 2048004016645467. [Google Scholar]
- Garekar, S.; Bharati, A.; Chokhandre, M.; Mali, S.; Trivedi, B.; Changela, V.P.; Solanki, N.; Gaikwad, S.; Agarwal, V. Clinical application and multidisciplinary assessment of three dimensional printing in double outlet right ventricle with remote ventricular septal defect. World J. Pediatr. Congenit. Heart Surg. 2016, 7, 344–350. [Google Scholar] [CrossRef]
- Javan, R.; Herrin, D.; Tangestanipoor, A. Understanding spatially complex segmental and branch anatomy using 3D printing: Liver, lung, prostate, coronary arteries, and circle of Willis. Acad. Radiol. 2016, 23, 1183–1189. [Google Scholar] [CrossRef]
- Xiong, G.; Kolli, K.; Soohoo, H.A.; Min, J.K. In-vitro assessment of coronary hemodynamics in 3D printed patient-specific geometry. Circulation 2015, 132, 19898. [Google Scholar] [CrossRef]
- Schmauss, D.; Haeberle, S.; Hagl, C.; Sodian, R. Three-dimensional printing in cardiac surgery and interventional cardiology: A single-centre experience. Eur. J. Cardiothorac. Surg. 2015, 47, 1044–1052. [Google Scholar] [CrossRef] [Green Version]
- Russ, M.; O’Hara, R.; Setlur Nagesh, S.V.; Mokin, M.; Jimenez, C.; Siddiqui, A.; Bednarek, D.; Rudin, S.; Ionita, C. Treatment planning for image-guided neurovascular interventions using patient-specific 3D printed phantoms. In Proceedings of the Medical Imaging 2015: Biomedical Applications in Molecular, Structural, and Functional Imaging, Orlando, FL, USA, 21–26 February 2015; Volume 9417, p. 941726. [Google Scholar]
- Kolli, K.K.; Min, J.K.; Ha, S.; Soohoo, H.; Xiong, G. Effect of varying hemodynamic and vascular conditions on fractional flow reserve: An in vitro study. J. Am. Heart Assoc. 2016, 5, e003634. [Google Scholar] [CrossRef] [Green Version]
| IVUS | OCT | NIRS | |
|---|---|---|---|
| Resolution | + | ++ | NA |
| PCI (stent sizing, expansion) | ++ | ++ | NA |
| Necrotic core | + | + | ++ |
| Detection of thin cap | ± | ++ | - |
| Thrombus | ± | + | - |
| Stent tissue coverage | + | ++ | - |
| Calcification | ++ | - | - |
| Remodeling | ++ | - | - |
| Neointimal hyperplasia | + | ++ | - |
| Requires blood-free field of view | No | Yes | No |
| Method | Advantages | Limitations |
|---|---|---|
| FFR | Prognostic studies available | Guidewire: cost; complication Hyperemia: cost; side effect of adenosine Increase time of procedure |
| iFR | Validated by noninferiority studies vs. FFR Hyperemia-independent Quicker than FFR | Guidewire: cost; complication Hyperemia: cost; side effects of adenosine Specific software required |
| QFR | Hyperemia-independent No pressure wire | Specific software required Precise acquisition of angiography Manual correction by expert |
| CCTA-FFR | Noninvasive Increase performance of CCTA | Cost Offline analysis |
| CFR | Study all coronary tree Prognostic performance Overall assessment (macro- and microcirculation) | Variability: intrinsic plus variable resting condition Guidewire: cost; complication Hyperemia: cost; side effects of adenosine Increase time of the procedure |
| IMR | Microcirculatory analysis | Guidewire: cost; complication Hyperemia: cost; side effect of adenosine Increase time of the procedure |
| HMR | Microcirculation analysis | Guidewire: cost; complication Hyperemia: cost; side effect of adenosine Increase time of the procedure Doppler: additional cost; Doppler signal not analyzable in 30% of patients No cutoff value |
| IMR | HMR | |
|---|---|---|
| Method | Thermodilution | Doppler |
| Definition | Thyperemia × Pd | Pd/Vhyperemia |
| Abnormal value | ≥25 units | >1.9 mmHg/cm/s |
| Limitations | T: surrogate of flow Requires hyperemia | V: surrogate of flow Requires hyperemia |
| Pressure Index | Hyperemia | Cutoff | Calculation of Index |
|---|---|---|---|
| FFR | Required | ≤0.80 | Average Pd/Pa during entire cycle at hyperemia (typically averaged over 3 beats) |
| Resting Pd/Pa | NHPR | ≤0.91 | Average Pd/Pa during entire cycle at hyperemia (typically averaged over 3 beats) |
| RFR | NHPR | ≤0.89 | Instant lowest filtered Pd/Pa ratio during the entire cardiac cycle (over 5 beats) |
| iFR | NHPR | ≤0.89 | Average Pd/Pa during wave-free period (over 5 beats) |
| DFR | NHPR | ≤0.89 | Average Pd/Pa during period between Pa < mean Pa and down-sloping Pa (over 5 beats) |
| dPR | NHPR | ≤0.89 | Average Pd/Pa during entire diastole (over 5 beats) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Oliveira Laterza Ribeiro, M.; Correia, V.M.; Herling de Oliveira, L.L.; Soares, P.R.; Scudeler, T.L. Evolving Diagnostic and Management Advances in Coronary Heart Disease. Life 2023, 13, 951. https://doi.org/10.3390/life13040951
de Oliveira Laterza Ribeiro M, Correia VM, Herling de Oliveira LL, Soares PR, Scudeler TL. Evolving Diagnostic and Management Advances in Coronary Heart Disease. Life. 2023; 13(4):951. https://doi.org/10.3390/life13040951
Chicago/Turabian Stylede Oliveira Laterza Ribeiro, Matheus, Vinícius Machado Correia, Lucas Lentini Herling de Oliveira, Paulo Rogério Soares, and Thiago Luis Scudeler. 2023. "Evolving Diagnostic and Management Advances in Coronary Heart Disease" Life 13, no. 4: 951. https://doi.org/10.3390/life13040951