Delayed Stroke after Aneurysm Treatment with Flow Diverters in Small Cerebral Vessels: A Potentially Critical Complication Caused by Subacute Vasospasm
Abstract
:1. Introduction
2. Material and Methods
2.1. Ethics Approval
2.2. Patients, Quantification of Vasospastic Deformities, Intimal Hyperplasia, and Cumulative Stenosis
2.3. Interventional Procedures
2.4. Statistical Analysis
- Gender;
- Localization of the aneurysms;
- Severity of disease in case of initial SAH;
- Status of the aneurysm—unruptured vs. ruptured;
- Endovascular strategy (FDS only for incidental aneurysm treatment; FDS only for acutely ruptured aneurysm treatment; plug and pipe: coiling in acute SAH and subsequent FDS implantation; complementary FDS after initial stent-assisted coiling: FDS in-stent implantation).
3. Results
3.1. Patients, Clinically Relevant Features, and Implanted Flow Diverter Stents
3.2. Follow-Up Imaging
3.3. Clinical Outcome
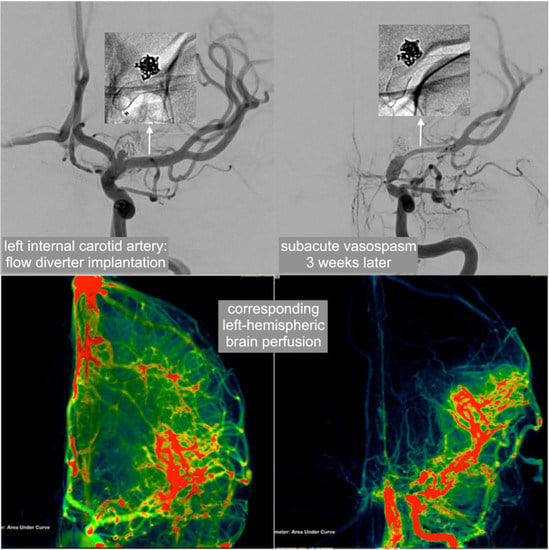
3.4. Presentation and Further Course of the Patient Suffering from Stroke Due to Severe FDS-Induced Vasospasm
3.5. Imaging Findings in the Overall Patient Collective
3.6. Statistical Findings
3.6.1. Normal vs. Non Normal Distribution
3.6.2. Differences Concerning Vasospastic Deformation, Intimal Hyperplasia, and Cumulative Stenosis Comparing Relevant Subgroups
- There were no significant differences in values of subacute vasospasm with stent deformities (p = 0.278), neointimal hyperplasia (p = 0.618), and cumulative stenosis (p = 0.443) when comparing male and female patients.
- The extents of neointimal hyperplasia did not differ significantly among the different aneurysm locations according to Kruskal–Wallis testing (p = 0.338).
- The extents of neointimal hyperplasia did not differ significantly between the distinct endovascular strategies according to Kruskal–Wallis testing (p = 0.116).
- There were no significant differences in values of subacute vasospasm with stent deformities (p = 0.151), neointimal hyperplasia (p = 0.201), and cumulative stenosis (p = 0.223) after using the initial Hunt and Hess grade as a grouping variable.
- The extents of subacute vasospasm, neointimal hyperplasia, and cumulative stenosis did not differ significantly among the groups after using Fisher score as a grouping variable (p = 0.331).
- The extent of subacute vasospasm differed significantly among the different aneurysm locations (p = 0.007). More specifically, according Tukey’s post hoc analysis, vasoconstrictive deformities were significantly stronger at the ICA–MCA junction compared to the ICA–PcomA complex (p = 0.007), the MCA (p = 0.031), and the VBA (p = 0.018), whereas there was only a non-significant tendency of stronger vasoconstrictive deformities when comparing ICA–MCA junction and ICA–AcomA complex (p = 0.095).
- The extents of cumulative stenoses did not differ significantly between the distinct aneurysm locations, although a deformity-like tendency was observable (p = 0.089).
- The extents of vasoconstrictive deformities and cumulative stenoses did not differ significantly among the distinct endovascular strategies (p = 0.732 and p = 0.989).
- The extents of vasoconstrictive deformities, neointimal hyperplasia, and cumulative stenoses did not differ significantly between initially ruptured and incidental aneurysms (p = 0.821, p = 0.778, and p = 0.909).
4. Discussion
Outlook
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Nelson, P.K.; Lylyk, P.; Szikora, I.; Wetzel, S.G.; Wanke, I.; Fiorella, D. The Pipeline Embolization Device for the Intracranial Treatment of Aneurysms. AJNR Am. J. Neuroradiol. 2011, 32, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Möhlenbruch, M.A.; Kizilkilic, O.; Killer-Oberpfalzer, M.; Baltacioglu, F.; Islak, C.; Bendszus, M.; Cekirge, S.; Saatci, I.; Kocer, N. Multicenter Experience with FRED Jr Flow Re-Direction Endoluminal Device for Intracranial Aneurysms in Small Arteries. AJNR Am. J. Neuroradiol. 2017, 38, 1959–1965. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ravindran, K.; DiStasio, M.; Laham, R.; Ogilvy, C.S.; Thomas, A.J.; VanderLaan, P.A.; Alturki, A.Y. Histopathological demonstration of subacute endothelialization following aneurysm re-treatment with the Pipeline embolization device. World Neurosurgery. 2018, 118, 156–160. [Google Scholar] [CrossRef] [PubMed]
- Safain, M.G.; Roguski, M.; Heller, R.S.; Malek, A.M. Flow Diverter Therapy With the Pipeline Embolization Device Is Associated With an Elevated Rate of Delayed Fluid-Attenuated Inversion Recovery Lesions. Stroke. 2016, 47, 789–797. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGuinness, B.J.; Memon, S.; Hope, J.K. Prospective Study of Early MRI Appearances following Flow-Diverting Stent Placement for Intracranial Aneurysms. AJNR Am. J. Neuroradiol. 2015, 36, 943–948. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.B.; Shi, W.W.; Zhang, G.X.; Lu, H.C.; Ma, J. Flow diverter treatment of posterior circulation aneurysms. A meta-analysis. Neuroradiology. 2016, 58, 391–400. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aguilar Pérez, M.; Bhogal, P.; Henkes, E.; Ganslandt, O.; Bäzner, H.; Henkes, H. In-stent Stenosis after p64 Flow Diverter Treatment. Clin. Neuroradiol. 2018, 28, 563–568. [Google Scholar] [CrossRef] [PubMed]
- John, S.; Bain, M.D.; Hui, F.K.; Hussain, M.S.; Masaryk, T.J.; Rasmussen, P.A.; Toth, G. Long-term follow-up of in- stent stenosis after pipeline flow diversion treatment of Intracranial aneurysms. Neurosurgery. 2016, 78, 862–867. [Google Scholar] [CrossRef]
- Kocer, N.; Mondel, P.K.; Yamac, E.; Kavak, A.; Kizilkilic, O.; Islak, C. Is there an association between flow diverter fish mouthing and delayed-type hypersensitivity to metals?—A case-control study. Neuroradiology. 2017, 59, 1171–1178. [Google Scholar] [CrossRef]
- Cohen, J.E.; Gomori, J.M.; Moscovici, S.; Leker, R.R.; Itshayek, E. Delayed complications after flowdiverter stenting: Reactive in-stent stenosis and creeping stents. J. Clin. Neurosci. 2014, 21, 1116–1122. [Google Scholar] [CrossRef]
- Miller, T.R.; Jindal, G.; Gandhi, D. Focal, transient mechanical narrowing of a pipeline embolization device following treatment of an internal carotid artery aneurysm. J. Neurointerv. Surg. 2015, 7, 235. [Google Scholar] [CrossRef] [PubMed]
- Al-Mufti, F.; Amuluru, K.; Gandhi, C.D.; Prestigiacomo, C.J. Flow Diversion for Intracranial Aneurysm Management: A New Standard of Care. Neurotherapeutics. 2016, 13, 582–589. [Google Scholar] [CrossRef] [Green Version]
- Voigt, P.; Schob, S.; Jantschke, R.; Nestler, U.; Krause, M.; Weise, D.; Lobsien, D.; Hoffmann, K.T.; Quäschling, U. Stent-Assisted Coiling of Ruptured and Incidental Aneurysms of the Intracranial Circulation Using Moderately Flow-Redirecting, Braided Leo Stents-Initial Experience in 39 Patients. Front. Neurol. 2017, 8, 602. [Google Scholar] [CrossRef] [PubMed]
- Schob, S.; Hoffmann, K.; Richter, C.; Bhogal, P.; Köhlert, K.; Planitzer, U.; Ziganshyna, S.; Lindner, D.; Scherlach, C.; Nestler, U.; et al. Flow diversion beyond the circle of Willis: Endovascular aneurysm treatment in peripheral cerebral arteries employing a novel low-profile flow diverting stent. J. Neuro. Inter. Surg 2019. [Google Scholar] [CrossRef] [PubMed]
- Rosenfield, K.; Schainfeld, R.; Pieczek, A.; Haley, L.; Isner, J.M. Restenosis of endovascular stents from stent compression. J. Am. Coll. Cardiol. 1997, 29, 328–338. [Google Scholar] [CrossRef]
- Johnson, S.P.; Fujitani, R.M.; Leyendecker, J.R.; Joseph, F.B. Stent deformation and intimal hyperplasia complicating treatment of a post-carotid endarterectomy intimal flap with a Palmaz stent. J. Vasc. Surg. 1997, 25, 764–768. [Google Scholar] [CrossRef]
- Singh, B.; Goyal, A.; Mohan, B.; Chhabra, S.T.; Aslam, N.; Wander, G.S. Coronary Vasospasm Abutting the Stent: A Rare Though Important Cause of Recurrent Angina. J. Invasive. Cardiol. 2018, 30, E46–E47. [Google Scholar]
- Shiraga, S.; Akai, T.; Takata, H.; Iizuka, H. Possible cerebral infarction due to multiple segmental cerebral vasospasms after carotid artery stenting: A Case Report. No. Shinkei. Geka. 2015, 43, 1081–1089. [Google Scholar] [CrossRef]
- Sucato, V.; Sansone, A.; Evola, S.; Novo, G.; Coppola, G.; Corrado, E.; Rotolo, A.; Andolina, G.; Novo, S.; Assennato, P. A rare case of Prinzmetal angina 3 days after coronary artery stenting with a second-generation drug-eluting stent. Coron. Artery. Dis. 2015, 26, 91–93. [Google Scholar] [CrossRef]
- Aghaebrahim, A.; Jadhav, A.P.; Saeed, Y.; Totoraitis, R.; Jankowitz, B.T.; Jovin, T.G.; Molyneaux, B.J. Reversible cerebral vasoconstriction syndrome following carotid stenting. Neurology. 2014, 83, 570–571. [Google Scholar] [CrossRef] [Green Version]
- Küker, W.; Schulz, U. Choroid artery occlusion after treatment of ICA termination aneurysm: Was it caused by stent induced vasospasm? Neuroradiology. 2014, 56, 259–262. [Google Scholar] [CrossRef] [PubMed]
- Rastogi, V.; Asaithambi, G.; Patel, A.; Park, K.; Bidari, S.; Hedna, V.S. Oral verapamil in the prevention of recurrent cerebral ischaemia due to post-stent vasospasm. J. Clin. Pharm. Ther. 2016, 41, 365–367. [Google Scholar] [CrossRef] [PubMed]
- Mühl-Benninghaus, R.; Haußmann, A.; Simgen, A.; Tomori, T.; Reith, W.; Yilmaz, U. Transient in-stent stenosis: A common finding after flow diverter implantation. J. Neurointerv. Surg. 2019, 11, 196–199. [Google Scholar] [CrossRef] [PubMed]
- Lazzaro, M.A.; Teleb, M.S.; Zaidat, O.O. Angiographic lumen changes associated with oversized intracranial stent implantation for aneurysm treatment. J. Neuroimaging. 2013, 23, 508–513. [Google Scholar] [CrossRef] [PubMed]
- Caroff, J.; Iacobucci, M.; Rouchaud, A.; Mihalea, C.; de Carvalho, F.M.; Jocson, V.E.D.; Chalumeau, V.; Da Ros, V.; King, R.M.; Arslanian, R.; et al. The occurrence of neo-intimal hyperplasia after flow-diverter implantation is associated with cardiovascular risks factors and the stent design. J. Neurointerv. Surg. 2019, 11, 610–613. [Google Scholar] [CrossRef] [PubMed]
- Douglas, G.; Van Kampen, E.; Hale, A.B.; McNeill, E.; Patel, J.; Crabtree, M.J.; Ali, Z.; Hoerr, R.A.; Alp, N.J.; Channon, K.M. Endothelial cell repopulation after stenting determines in-stent neointima formation: Effects of bare-metal vs. drug-eluting stents and genetic endothelial cell modification. Eur. Heart J. 2013, 34, 3378–3388. [Google Scholar] [CrossRef]
- Van der Heiden, K.; Gijsen, F.J.; Narracott, A.; Hsiao, S.; Halliday, I.; Gunn, J.; Wentzel, J.J.; Evans, P.C. The effects of stenting on shear stress: Relevance to endothelial injury and repair. Cardiovasc. Res. 2013, 99, 269–275. [Google Scholar] [CrossRef]
- Cornelissen, A.; Vogt, F.J. The effects of stenting on coronary endothelium from a molecular biological view: Time for improvement? J. Cell. Mol. Med. 2019, 23, 39–46. [Google Scholar] [CrossRef]
- Tolosa, E. Collateral circulation in occlusive vascular lesions of the brain. The role of the middle meningeal artery in the collateral circulation in compensating for occlusions of the internal carotid artery or its branches. Prog. Brain Res. 1968, 30, 247–254. [Google Scholar]
- Khan, S.; Amin, F.M.; Christensen, C.E.; Ghanizada, H.; Younis, S.; Olinger, A.C.R.; de Koning, P.J.H.; Larsson, H.B.W.; Ashina, M. Meningeal contribution to migraine pain: A magnetic resonance angiography study. Brain 2019, 142, 93–102. [Google Scholar] [CrossRef]






| Case | Sex | Age (years) | Pathology, Location, Strategy | Proximal Vessel Diameter in mm | Distal Vessel Diameter in mm | Implanted Device | Maximal Device Oversizing | Vasoconstricive Segmental Stenosis %; Location | Time Point of Follow-Up Imaging Post Implantation | Additional In-Stent Stenosis/Neointimal Hyperplasia | Cumulative Local Stenosis |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Male | 51 | Left V4, ruptured dissecting aneurysm, primary Flow Diverting Stent (FDS) | 4.2 | 2.5 | PED 2 400-300 | 1.5 mm, 60% | 15% distal landing zone (distal V4) | 20 weeks | 20% | 35% |
| 2 | Male | 72 | Basilar artery, ruptured blister aneurysm, primary FDS | 2.2 | 1.7 | p48 HPC 300-18 | 1.3 mm, 56% | 45% distal landing zone (basilar tip) | 8 weeks | Radiography only, not assessable | Minimum of 30% |
| 3 | Female | 51 | Left M1, ruptured saccular aneurysm, Plug and Pipe (P&P) | 2 | 1.4 | P48200-15 | 0.6 mm, 30% | 25% proximal landing zone (left M1) | 4 weeks | Radiography only, not assessable | Minimum of 30% |
| 4 * | Male | 64 | Left A1–A2, ruptured saccular aneurysm, P&P after pCONus 2 Stent-Assisted Coiling (SAC) | 2.1 | 1.7 | p48 HPC 300-18 | 1.3 mm, 43% | 12% distal landing zone (A2; uncovered by pCONus) | 5 weeks | Radiography only, not assessable | 12% |
| 5 * | Female | 78 | Right Middle Cerebral Artery (MCA) bifurcation, incidental saccular giant-aneurysm, elective P&P after pCONus 2 SAC | 3.0 | 2.6 | p48 HPC 300-18 | 0.4 mm, 13% | 31% distal landing zone (right M2, not covered by pCONus) | 5 weeks | Radiography only, not assessable | 31% |
| 6 # | Female | 52 | Basilar artery right P1, incidental saccular giant aneurysm, primary FDS | 2.7 | 2.1 | 2 × p48 HPC 300-18 | 0. 9 mm, 30% | 14% distal landing zone (right P1) | 5 weeks | Radiography only, not assessable | 14% |
| 7 | Male | 33 | Right A1, incidental saccular aneurysm, primary FDS | 1.9 | 2.4 | p48 HPC 300-15 | 1.1 mm, 42% | 37% proximal landing zone (right A1) | 5 weeks | Radiography only, not assessable | Minimum of 37% |
| 8 | Female | 49 | Left PcomA-ostium, ruptured saccular aneurysm, P&P | 2.5 | 3.1 | p64 300-15 | 0.5m, 20% | 20% proximal landing zone (ICA) | 14 weeks | 10% | 30% |
| 9 | Male | 37 | Right M1, incidental saccular aneurysm, elective P&P | 2.6 | 2.4 | PED2-275-12 | 0.35 mm, 15% | 33% distal landing zone (M2) and 15% proximal landing zone (M1) | 10 weeks | 10% | 43% |
| 10 | Male | 51 | Left A1–A2, incidental saccular aneurysm, primary FDS | 1.8 | 1.8 | SVB 2.25 × 15 | 0.45 mm, 25% | 33% proximal landing zone (A1) | 13 weeks | 20% | 53% |
| 11 | Female | 18 | Right M2, incidental saccular aneurysm, primary FDS | 1.8 | 1.9 | SVB 2.25 × 15 | 0.45 mm, 25% | 19% proximal landing zone (M2) | 12 weeks | 22% | 41% |
| 12 | Female | 39 | Left A1–A2,ruptured saccular aneurysm, P&P | 1.8 | 1.8 | SVB 2.25 × 20 | 0.45 mm, 25% | 42% proximal landing zone (A1) | 14 weeks | 5% | 47% |
| 13 | Female | 50 | Right A2–A3, incidental saccular aneurysm, primary FDS | 1.8 | 1.7 | SVB 2.25 × 10 | 0.55 mm, 32% | 33% proximal landing zone (A2) | 17 weeks | 10% | 43% |
| 14 * | Female | 38 | Left A1–A2, incidental saccular aneurysm, primary FDS | 1.7 | 2.0 | SVB 2.25 × 10; 2.25 × 15 | 0.55 mm, 32% | 18% proximal landing zone (A1) | 28 weeks | 13% | 31 % |
| 15 | Female | 55 | Right A1/2, ruptured saccular aneurysm, P&P | 1.7 | 1.6 | SVB 2.25 × 15 | 0.65 mm, 40% | 56% proximal landing zone (A1) | 17 weeks | 10% | 66% |
| 16 | Female | 48 | Left PICA, ruptured saccular aneurysm, P&P | 2.4 | 2.3 | SVB 2.25 × 10 | none | None | 14 weeks | 10% | 10% |
| 17 * | Male | 55 | Right A1–A2, incidental aneurysm, primary FDS | 2.0 | 1.9 | SVB 2.25 × 15 | 0.35 mm, 18% | 33% proximal landing zones (each) | 14 weeks | 0% | 33% |
| 18 | Female | 40 | A1–A2, ruptured saccular aneurysm, P&P | 2.2 | 1.7 | SVB 2.25 × 15 | 0.55 mm, 32% | 33% of the proximal and distal landing zones (A1, A2) | 9 weeks | 10% | 43% |
| 19 | Female | 59 | Left paraophthalmic Internal Carotid Artery (ICA), incidental saccular aneurysm, primary FDS | 3.4 | 3.0 | SVB 3.25 × 20 | 0.25 mm, 8% | 17% distal landing zone (ICA) | 12 weeks | 0% | 17% |
| 20 | Female | 70 | Right Posterior Communicating Artery (PcomA), incidental saccular aneurysm, primary FDS | 3.1 | 3.0 | SVB 3.25 × 25 | none | None | 12 weeks | 0% | 0% |
| 21 | Female | 56 | Left Posterior Inferior Cerebellar Artery (PICA), ruptured saccular aneurysm, P&P | 3.4 | 3.2 | SVB 3.25 × 10 | 0.05 mm, 1.5% | None | 12 weeks | 0% | 0% |
| 22 | Female | 39 | Right A1–A2, ruptured saccular aneurysm, P&P | 2.0 | 1.7 | SVB 2.25 × 15 | 0.55 mm, 25% | 25% proximal landing zone (A1) | 16 weeks | 10% | 35% |
| 23 | Female | 58 | Left A1–A2, ruptured saccular aneurysm, P&P | 2.3 | 2.1 | SVB 2.25 × 15 | 0.1 mm, 7% | None | 15 weeks | 0% | 0% |
| 24 * | Female | 58 | Left RCP and left MCA, incidental saccular aneurysm, primary FDS | 3.4 | 1.6 | SVB 3.25 × 20; 3.25 × 25 | 1.6 mm, 51 % | Distal landing zone 25% M1 | 14 weeks | 10% | 35% |
| 25 # | Female | 64 | Right A2–A3, saccular aneurysm, elective P&P after Leo-Baby + coiling | 1.8 | 1.7 (covered by LEO baby stent) | SVB 2.25 × 10 | 0.55 mm, 32% | Proximal landing zone 13% (A2) | 19 weeks | 15% | 28% |
| 26 | Male | 38 | Left ICA bifurcation + RCP, ruptured saccular aneurysm, P&P + primary FDS | 3.6 | 2.5 | SVB 3.25 × 20 | 0.75 mm, 30% | 40% distal landing zone (M1) 30% middle–proximal quarter (ICA) | 13 weeks | 5% | 45% |
| 27 | Female | 27 | Left M1, ruptured saccular aneurysm, P&P | 3.5 | 2.8 | SVB 3.25 × 20 | 0.45 mm, 16% | >85% of the proximal (ICA) and >60% of the distal landing zone (M1) | 3 weeks | 10% | >95% |
| 28 | Male | 63 | Left A1–A2, incidental saccular aneurysm, primary FDS | 2.2 | 1.8 | SVB 2.25 × 15 | 0.45 mm, 25% | 38% of the distal (A2) and 27% of the proximal landing zone (A1) | 16 weeks | 0% | 38% |
| 29 | Male | 52 | Left supraophthalmic ICA, ruptured saccular aneurysm, P&P | 3.2 | 2.9 | SVB 3.25 × 25 | 0.35 mm, 12% | 7% distal landing zone | 8 weeks | 0% | 7% |
| 30 | Male | 40 | Left PICA, ruptured saccular aneurysm, P&P | 2.5 | 2.5 | SVB 2.75 × 25 | 0.25 mm, 10% | 42% proximal landing zone | 6 weeks | 67% | 81% |
| 31 * | Male | 60 | Right M1, ruptured saccular aneurysm, P&P | 3.1 | 2.8 | SVB 2.25 × 15; 2.75 × 15 | none | 0% | 5 weeks | 0% | 0% |
| 32 | Male | 54 | Left A1–A2, ruptured saccular aneurysm, P&P | 2.5 | 1.8 | SVB 2.75 × 20 | 0,95 mm, 52% | 48% proximal landing zone (A1) 44% distal landing zone (A2) | 6 weeks | Radiography only, not assessable | 48% |
| 33 | Female | 55 | Right A1–A2, ruptured saccular aneurysm, P&P | 2.1 | 1.5 | SVB 2.25 × 20 | 0,75 mm, 50% | 33% distal landing zone (A2) 20% proximal landing zone (A1) | 7 weeks | Radiography only, not assessable | 33% |
| 34 | Female | 61 | Right A1–A2, ruptured saccular aneurysm, P&P | 2.0 | 1.9 | SVB 2.25 × 15 | 0,35 mm, 15% | 50% distal landing zone 20% proximal landing zone | 5 weeks | Radiography only, not assessable | 50% |
| 35 | Male | 35 | Left A1–A2, incidental saccular aneurysm, primary FDS | 3.0 | 2.5 | p48 3 × 18 | 0.5 mm, 20% | 53% distal landing zone, 40% proximal landing zone | 4 weeks | 0% | 53% |
| 36 | Male | 36 | Left V4, incidental saccular aneurysm, primary FDS | 3.1 | 2.5 | SVB 2.75 × 25 | 0.25 mm, 10% | 72% proximal landing zone | 5 weeks | 10% | 82% |
| Vasospastic Stenosis in % | Number of Patients | Average Oversizing in % (Mean ± SD) | Average Resulting Device Compression in % (Mean ± SD) | Female/Male Patients | Average Age in Years | Average Size of the Aneurysm (Mean ± SD) |
|---|---|---|---|---|---|---|
| 0–24 | 14 | 19.3 ± 17.8 | 9.6 ± 7.8 | 10/4 | 52.8 | 7.5 ± 4.8 |
| 25–50 | 16 | 31.3 ± 14.3 | 34.8 ± 6.7 | 7/9 | 50.9 | 5.7 ± 6.0 |
| >50 | 6 | 21.8 ± 10.2 | 59.3 ± 14.9 | 3/3 | 42.0 | 5.6 ± 1.4 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schob, S.; Richter, C.; Scherlach, C.; Lindner, D.; Planitzer, U.; Hamerla, G.; Ziganshyna, S.; Werdehausen, R.; Struck, M.F.; Schob, B.; et al. Delayed Stroke after Aneurysm Treatment with Flow Diverters in Small Cerebral Vessels: A Potentially Critical Complication Caused by Subacute Vasospasm. J. Clin. Med. 2019, 8, 1649. https://doi.org/10.3390/jcm8101649
Schob S, Richter C, Scherlach C, Lindner D, Planitzer U, Hamerla G, Ziganshyna S, Werdehausen R, Struck MF, Schob B, et al. Delayed Stroke after Aneurysm Treatment with Flow Diverters in Small Cerebral Vessels: A Potentially Critical Complication Caused by Subacute Vasospasm. Journal of Clinical Medicine. 2019; 8(10):1649. https://doi.org/10.3390/jcm8101649
Chicago/Turabian StyleSchob, Stefan, Cindy Richter, Cordula Scherlach, Dirk Lindner, Uwe Planitzer, Gordian Hamerla, Svitlana Ziganshyna, Robert Werdehausen, Manuel Florian Struck, Bernd Schob, and et al. 2019. "Delayed Stroke after Aneurysm Treatment with Flow Diverters in Small Cerebral Vessels: A Potentially Critical Complication Caused by Subacute Vasospasm" Journal of Clinical Medicine 8, no. 10: 1649. https://doi.org/10.3390/jcm8101649