Short-Term Effect of SARS-CoV-2 Spike Protein Receptor-Binding Domain-Specific Antibody Induction on Neutrophil-Mediated Immune Response in Mice
Abstract
:1. Introduction
2. Results
2.1. Induction and Characterization of RBD-Specific Antibody Response
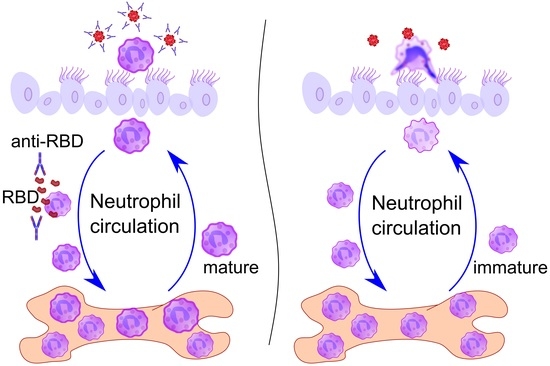
2.2. Elevated Neutrophil Recruitment to the Bloodstream in Response to the Model Virus Particle Application in Mice with Induced RBD-Specific Antibodies
2.3. Neutrophil-Mediated Immune Response to Inhaled Model Virus Particles in the Airways of Mice with Induced RBD-Specific Antibodies
2.4. Bone Marrow Neutrophil Activation and Maturation in Mice with Induced RBD-Specific Antibodies
2.5. The Reactivity of Bone Marrow Neutrophils from Mice with RBD-Specific Antibodies
3. Discussion
4. Materials and Methods
4.1. Animals and Ethics Statement
4.2. RBD-Specific Antibody Induction
4.3. 100 nm Fluorescent Particles and RBD Application
4.4. Blood Collection
4.5. Blood Cell Analysis by Flow Cytometry
4.6. Bone Marrow Cells Analysis
4.7. Neutrophil Isolation
4.8. Extracellular Nucleotide Detection and Imaging
4.9. Bronchoalveolar Lavage (BAL) Collection
4.10. Antibody Detection
4.11. Whole-Mount Lung Immunohistochemistry and Optical Clearing
4.12. Whole-Mount Conducting Airway Specimen Preparation and Staining
4.13. Confocal Laser Scanning Microscopy (CLSM)
4.14. Quantitative Image Analysis
4.15. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sahin, U.; Muik, A.; Derhovanessian, E.; Vogler, I.; Kranz, L.M.; Vormehr, M.; Baum, A.; Pascal, K.; Quandt, J.; Maurus, D.; et al. COVID-19 Vaccine BNT162b1 Elicits Human Antibody and TH1 T Cell Responses. Nature 2020, 586, 594–599. [Google Scholar] [CrossRef]
- Föhse, F.K.; Geckin, B.; Overheul, G.J.; van de Maat, J.; Kilic, G.; Bulut, O.; Dijkstra, H.; Lemmers, H.; Sarlea, S.A.; Reijnders, M.; et al. The BNT162b2 MRNA Vaccine Against SARS-CoV-2 Reprograms Both Adaptive and Innate Immune Responses. medRxiv 2021, 03, 21256520. [Google Scholar] [CrossRef]
- Logunov, D.Y.; Dolzhikova, I.V.; Shcheblyakov, D.V.; Tukhvatulin, A.I.; Zubkova, O.V.; Dzharullaeva, A.S.; Kovyrshina, A.V.; Lubenets, N.L.; Grousova, D.M.; Erokhova, A.S.; et al. Safety and Efficacy of an RAd26 and RAd5 Vector-Based Heterologous Prime-Boost COVID-19 Vaccine: An Interim Analysis of a Randomised Controlled Phase 3 Trial in Russia. Lancet 2021, 397, 671–681. [Google Scholar] [CrossRef]
- Byazrova, M.G.; Kulemzin, S.V.; Astakhova, E.A.; Belovezhets, T.N.; Efimov, G.A.; Chikaev, A.N.; Kolotygin, I.O.; Gorchakov, A.A.; Taranin, A.V.; Filatov, A.V. Memory B Cells Induced by Sputnik V Vaccination Produce SARS-CoV-2 Neutralizing Antibodies Upon Ex Vivo Restimulation. Front. Immunol. 2022, 13, 840707. [Google Scholar] [CrossRef] [PubMed]
- Kozlovskaya, L.I.; Piniaeva, A.N.; Ignatyev, G.M.; Gordeychuk, I.V.; Volok, V.P.; Rogova, Y.V.; Shishova, A.A.; Kovpak, A.A.; Ivin, Y.Y.; Antonova, L.P.; et al. Long-Term Humoral Immunogenicity, Safety and Protective Efficacy of Inactivated Vaccine against COVID-19 (CoviVac) in Preclinical Studies. Emerg. Microbes Infect. 2021, 10, 1790–1806. [Google Scholar] [CrossRef]
- Falach, R.; Bar-On, L.; Lazar, S.; Kadar, T.; Mazor, O.; Aftalion, M.; Gur, D.; Evgy, Y.; Shifman, O.; Aminov, T.; et al. Mice with Induced Pulmonary Morbidities Display Severe Lung Inflammation and Mortality Following Exposure to SARS-CoV-2. JCI Insight 2021, 6, e145916. [Google Scholar] [CrossRef]
- Agrawal, A.; Jha, T.; Gogoi, P.; Diwaker, P.; Goel, A.; Khan, A.M.; Saxena, A.K. Effect of Convalescent Plasma Therapy on Mortality in Moderate-to-Severely Ill COVID-19 Patients. Transfus. Apher. Sci. 2022, 11, 103455. [Google Scholar] [CrossRef] [PubMed]
- Geckin, B.; Konstantin Föhse, F.; Domínguez-Andrés, J.; Netea, M.G. Trained Immunity: Implications for Vaccination. Curr. Opin. Immunol. 2022, 77, 102190. [Google Scholar] [CrossRef]
- Chumakov, K.; Avidan, M.S.; Benn, C.S.; Bertozzi, S.M.; Blatt, L.; Chang, A.Y.; Jamison, D.T.; Khader, S.A.; Kottilil, S.; Netea, M.G.; et al. Old Vaccines for New Infections: Exploiting Innate Immunity to Control COVID-19 and Prevent Future Pandemics. Proc. Natl. Acad. Sci. USA 2021, 118, e2101718118. [Google Scholar] [CrossRef]
- ten Doesschate, T.; van der Vaart, T.W.; Debisarun, P.A.; Taks, E.; Moorlag, S.J.; Paternotte, N.; Boersma, W.G.; Kuiper, V.P.; Roukens, A.H.; Rijnders, B.J.; et al. Bacillus Calmette-Guérin Vaccine to Reduce Healthcare Worker Absenteeism in COVID-19 Pandemic, a Randomized Controlled Trial. Clin. Microbiol. Infect. 2022. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Moorlag, S.J.; Rodriguez-Rosales, Y.A.; Gillard, J.; Fanucchi, S.; Theunissen, K.; Novakovic, B.; de Bont, C.M.; Negishi, Y.; Fok, E.T.; Kalafati, L.; et al. BCG Vaccination Induces Long-Term Functional Reprogramming of Human Neutrophils. Cell Rep. 2020, 33, 108387. [Google Scholar] [CrossRef]
- Veras, F.P.; Pontelli, M.C.; Silva, C.M.; Toller-Kawahisa, J.E.; de Lima, M.; Nascimento, D.C.; Schneider, A.H.; Caetité, D.; Tavares, L.A.; Paiva, I.M.; et al. SARS-CoV-2-Triggered Neutrophil Extracellular Traps Mediate COVID-19 Pathology. J. Exp. Med. 2020, 217, e20201129. [Google Scholar] [CrossRef]
- Middleton, E.A.; He, X.Y.; Denorme, F.; Campbell, R.A.; Ng, D.; Salvatore, S.P.; Mostyka, M.; Baxter-Stoltzfus, A.; Borczuk, A.C.; Loda, M.; et al. Neutrophil Extracellular Traps Contribute to Immunothrombosis in COVID-19 Acute Respiratory Distress Syndrome. Blood 2020, 136, 1169–1179. [Google Scholar] [CrossRef] [PubMed]
- Barnes, B.J.; Adrover, J.M.; Baxter-Stoltzfus, A.; Borczuk, A.; Cools-Lartigue, J.; Crawford, J.M.; Daßler-Plenker, J.; Guerci, P.; Huynh, C.; Knight, J.S.; et al. Targeting Potential Drivers of COVID-19: Neutrophil Extracellular Traps. J. Exp. Med. 2020, 217, e20200652. [Google Scholar] [CrossRef]
- Sing, C.W.; Tang, C.T.L.; Chui, C.S.L.; Fan, M.; Lai, F.T.T.; Li, X.; Wan, E.Y.F.; Wong, C.K.H.; Chan, E.W.Y.; Hung, I.F.N.; et al. COVID-19 Vaccines and Risks of Hematological Abnormalities: Nested Case–Control and Self-Controlled Case Series Study. Am. J. Hematol. 2022, 97, 470–480. [Google Scholar] [CrossRef] [PubMed]
- Yavuz, S.Ş.; Tunçer, G.; Altuntaş-Aydın, Ö.; Aydın, M.; Pehlivanoğlu, F.; Tok, Y.; Mese, S.; Gündüz, A.; Güçlü, C.G.; Özdoğan, İ.; et al. Comparison of the Clinical and Laboratory Findings and Outcomes of Hospitalized COVID-19 Patients Who Were Either Fully Vaccinated with Coronavac or Not: An Analytical, Cross Sectional Study. Vaccines 2022, 10, 733. [Google Scholar] [CrossRef] [PubMed]
- Stavnezer, J. Immunoglobulin Class Switching. Curr. Opin. Immunol. 1996, 8, 199–205. [Google Scholar] [CrossRef]
- Liu, Z.; Gu, Y.; Shin, A.; Zhang, S.; Ginhoux, F. Analysis of Myeloid Cells in Mouse Tissues with Flow Cytometry. STAR Protoc. 2020, 1, 100029. [Google Scholar] [CrossRef]
- Khoyratty, T.E.; Ai, Z.; Ballesteros, I.; Eames, H.L.; Mathie, S.; Martín-Salamanca, S.; Wang, L.; Hemmings, A.; Willemsen, N.; von Werz, V.; et al. Distinct Transcription Factor Networks Control Neutrophil-Driven Inflammation. Nat. Immunol. 2021, 22, 1093–1106. [Google Scholar] [CrossRef] [PubMed]
- Barrientos, L.; Marin-Esteban, V.; de Chaisemartin, L.; Le-Moal, V.L.; Sandré, C.; Bianchini, E.; Nicolas, V.; Pallardy, M.; Chollet-Martin, S. An Improved Strategy to Recover Large Fragments of Functional Human Neutrophil Extracellular Traps. Front. Immunol. 2013, 4, 166. [Google Scholar] [CrossRef] [Green Version]
- Ermert, D.; Zychlinsky, A.; Urban, C. Fungal and Bacterial Killing by Neutrophils. In Host-Pathogen Interactions; Methods Mol Biology; Humana Press: Totowa, NJ, USA, 2009; pp. 293–312. [Google Scholar]
- Mircescu, M.M.; Lipuma, L.; van Rooijen, N.; Pamer, E.G.; Hohl, T.M. Essential Role for Neutrophils but Not Alveolar Macrophages at Early Time Points Following Aspergillus Fumigatus Infection. J. Infect. Dis. 2009, 200, 647–656. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johansson, C.; Kirsebom, F.C.M. Neutrophils in Respiratory Viral Infections. Mucosal Immunol. 2021, 14, 815–827. [Google Scholar] [CrossRef]
- Mishra, H.K.; Long, C.; Bahaie, N.S.; Walcheck, B. Regulation of CXCR2 Expression and Function by a Disintegrin and Metalloprotease-17 (ADAM17). J. Leukoc. Biol. 2015, 97, 447–454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eash, K.J.; Greenbaum, A.M.; Gopalan, P.K.; Link, D.C. CXCR2 and CXCR4 Antagonistically Regulate Neutrophil Trafficking from Murine Bone Marrow. J. Clin. Investig. 2010, 120, 2423–2431. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Jönsson, F. Expression, Role, and Regulation of Neutrophil Fcγ Receptors. Front. Immunol. 2019, 10, 1958. [Google Scholar] [CrossRef] [PubMed]
- Beutier, H.; Gillis, C.M.; Iannascoli, B.; Godon, O.; England, P.; Sibilano, R.; Reber, L.L.; Galli, S.J.; Cragg, M.S.; van Rooijen, N.; et al. IgG Subclasses Determine Pathways of Anaphylaxis in Mice. J. Allergy Clin. Immunol. 2017, 139, 269–280.e7. [Google Scholar] [CrossRef] [Green Version]
- Borgoyakova, M.B.; Karpenko, L.I.; Rudometov, A.P.; Volosnikova, E.A.; Merkuleva, I.A.; Starostina, E.V.; Zadorozhny, A.M.; Isaeva, A.A.; Nesmeyanova, V.S.; Shanshin, D.V.; et al. Self-Assembled Particles Combining SARS-CoV-2 RBD Protein and RBD DNA Vaccine Induce Synergistic Enhancement of the Humoral Response in Mice. Int. J. Mol. Sci. 2022, 23, 2188. [Google Scholar] [CrossRef]
- Lamerton, R.E.; Marcial-Juarez, E.; Faustini, S.E.; Perez-Toledo, M.; Goodall, M.; Jossi, S.E.; Newby, M.L.; Chapple, I.; Dietrich, T.; Veenith, T.; et al. SARS-CoV-2 Spike- and Nucleoprotein-Specific Antibodies Induced After Vaccination or Infection Promote Classical Complement Activation. Front. Immunol. 2022, 13, 838780. [Google Scholar] [CrossRef]
- Afzali, B.; Noris, M.; Lambrecht, B.N.; Kemper, C. The State of Complement in COVID-19. Nat. Rev. Immunol. 2022, 22, 77–84. [Google Scholar] [CrossRef]
- Eriksson, O.; Hultström, M.; Persson, B.; Lipcsey, M.; Ekdahl, K.N.; Nilsson, B.; Frithiof, R. Mannose-Binding Lectin Is Associated with Thrombosis and Coagulopathy in Critically Ill COVID-19 Patients. Thromb. Haemost. 2020, 120, 1720–1724. [Google Scholar] [CrossRef]
- Noris, M.; Benigni, A.; Remuzzi, G. The Case of Complement Activation in COVID-19 Multiorgan Impact. Kidney International 2020, 98, 314–322. [Google Scholar] [CrossRef]
- Lukácsi, S.; Nagy-Baló, Z.; Erdei, A.; Sándor, N.; Bajtay, Z. The Role of CR3 (CD11b/CD18) and CR4 (CD11c/CD18) in Complement-Mediated Phagocytosis and Podosome Formation by Human Phagocytes. Immunol. Lett. 2017, 189, 64–72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurtovic, L.; Beeson, J.G. Complement Factors in COVID-19 Therapeutics and Vaccines. Trends Immunol. 2021, 42, 94–103. [Google Scholar] [CrossRef] [PubMed]
- Chrysanthopoulou, A.; Gkaliagkousi, E.; Lazaridis, A.; Arelaki, S.; Pateinakis, P.; Ntinopoulou, M.; Mitsios, A.; Antoniadou, C.; Argyriou, C.; Georgiadis, G.S.; et al. Angiotensin II Triggers Release of Neutrophil Extracellular Traps, Linking Thromboinflammation with Essential Hypertension. JCI Insight 2021, 6, e148668. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, K.E.; Khan, Z.; Giani, J.F.; Cao, D.Y.; Bernstein, E.A.; Shen, X.Z. Angiotensin-Converting Enzyme in Innate and Adaptive Immunity. Nat. Rev. Nephrol. 2018, 14, 325–336. [Google Scholar] [CrossRef] [PubMed]
- Muratori, P.; Lenzi, M.; Muratori, L.; Granito, A. Antinuclear Antibodies in COVID 19. Clin. Transl. Sci. 2021, 14, 1627–1628. [Google Scholar] [CrossRef] [PubMed]
- Darmarajan, T.; Paudel, K.R.; Candasamy, M.; Chellian, J.; Madheswaran, T.; Sakthivel, L.P.; Goh, B.H.; Gupta, P.K.; Jha, N.K.; Devkota, H.P.; et al. Autoantibodies and Autoimmune Disorders in SARS-CoV-2 Infection: Pathogenicity and Immune Regulation. Environ. Sci. Pollut. Res. 2022, 3, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Pascolini, S.; Vannini, A.; Deleonardi, G.; Ciordinik, M.; Sensoli, A.; Carletti, I.; Veronesi, L.; Ricci, C.; Pronesti, A.; Mazzanti, L.; et al. COVID-19 and Immunological Dysregulation: Can Autoantibodies Be Useful? Clin. Transl. Sci. 2021, 14, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Pascolini, S.; Granito, A.; Muratori, L.; Lenzi, M.; Muratori, P. Coronavirus Disease Associated Immune Thrombocytopenia: Causation or Correlation? J. Microbiol. Immunol. Infect. 2021, 54, 531–533. [Google Scholar] [CrossRef] [PubMed]
- Suwanchote, S.; Rachayon, M.; Rodsaward, P.; Wongpiyabovorn, J.; Deekajorndech, T.; Wright, H.L.; Edwards, S.W.; Beresford, M.W.; Rerknimitr, P.; Chiewchengchol, D. Anti-Neutrophil Cytoplasmic Antibodies and Their Clinical Significance. Clin. Rheumatol. 2018, 37, 875–884. [Google Scholar] [CrossRef]
- d’Alessandro, M.; Conticini, E.; Bergantini, L.; Cameli, P.; Cantarini, L.; Frediani, B.; Bargagli, E. Neutrophil Extracellular Traps in ANCA-Associated Vasculitis and Interstitial Lung Disease: A Scoping Review. Life 2022, 12, 317. [Google Scholar] [CrossRef] [PubMed]
- Torres-Ruiz, J.; Absalón-Aguilar, A.; Nuñez-Aguirre, M.; Pérez-Fragoso, A.; Carrillo-Vázquez, D.A.; Maravillas-Montero, J.L.; Mejía-Domínguez, N.R.; Llorente, L.; Alcalá-Carmona, B.; Lira-Luna, J.; et al. Neutrophil Extracellular Traps Contribute to COVID-19 Hyperinflammation and Humoral Autoimmunity. Cells 2021, 10, 2545. [Google Scholar] [CrossRef] [PubMed]
- Izci Duran, T.; Turkmen, E.; Dilek, M.; Sayarlioglu, H.; Arik, N. ANCA-Associated Vasculitis after COVID-19. Rheumatol. Int. 2021, 41, 1523–1529. [Google Scholar] [CrossRef] [PubMed]
- Baier, E.; Olgemöller, U.; Biggemann, L.; Buck, C.; Tampe, B. Dual-Positive MPO- and PR3-ANCA-Associated Vasculitis Following SARS-CoV-2 MRNA Booster Vaccination: A Case Report and Systematic Review. Vaccines 2022, 10, 653. [Google Scholar] [CrossRef]
- Kim, B.C.; Kim, H.S.; Han, K.H.; Han, S.Y.; Jo, H.A. A Case Report of MPO-ANCA-Associated Vasculitis Following Heterologous MRNA1273 COVID-19 Booster Vaccination. J. Korean Med. Sci. 2022, 37, e204. [Google Scholar] [CrossRef]
- Lindquist, R.L.; Shakhar, G.; Dudziak, D.; Wardemann, H.; Eisenreich, T.; Dustin, M.L.; Nussenzweig, M.C. Visualizing Dendritic Cell Networks in Vivo. Nat. Immunol. 2004, 5, 1243–1250. [Google Scholar] [CrossRef]
- Shevchenko, M.A.; Bolkhovitina, E.L.; Servuli, E.A.; Sapozhnikov, A.M. Elimination of Aspergillus Fumigatus Conidia from the Airways of Mice with Allergic Airway Inflammation. Respir. Res. 2013, 14, 78. [Google Scholar] [CrossRef] [PubMed] [Green Version]





Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bolkhovitina, E.L.; Vavilova, J.D.; Bogorodskiy, A.O.; Zagryadskaya, Y.A.; Okhrimenko, I.S.; Sapozhnikov, A.M.; Borshchevskiy, V.I.; Shevchenko, M.A. Short-Term Effect of SARS-CoV-2 Spike Protein Receptor-Binding Domain-Specific Antibody Induction on Neutrophil-Mediated Immune Response in Mice. Int. J. Mol. Sci. 2022, 23, 8234. https://doi.org/10.3390/ijms23158234
Bolkhovitina EL, Vavilova JD, Bogorodskiy AO, Zagryadskaya YA, Okhrimenko IS, Sapozhnikov AM, Borshchevskiy VI, Shevchenko MA. Short-Term Effect of SARS-CoV-2 Spike Protein Receptor-Binding Domain-Specific Antibody Induction on Neutrophil-Mediated Immune Response in Mice. International Journal of Molecular Sciences. 2022; 23(15):8234. https://doi.org/10.3390/ijms23158234
Chicago/Turabian StyleBolkhovitina, Elena L., Julia D. Vavilova, Andrey O. Bogorodskiy, Yuliya A. Zagryadskaya, Ivan S. Okhrimenko, Alexander M. Sapozhnikov, Valentin I. Borshchevskiy, and Marina A. Shevchenko. 2022. "Short-Term Effect of SARS-CoV-2 Spike Protein Receptor-Binding Domain-Specific Antibody Induction on Neutrophil-Mediated Immune Response in Mice" International Journal of Molecular Sciences 23, no. 15: 8234. https://doi.org/10.3390/ijms23158234