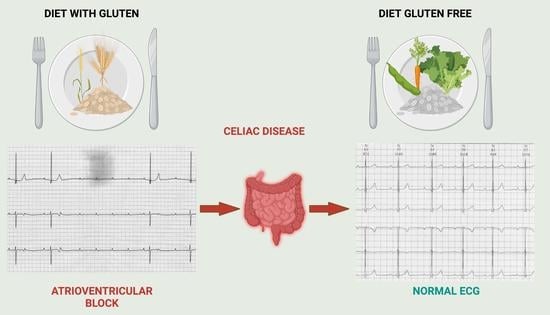
Atrioventricular Block in Celiac Disease: An Unusual Clinical Presentation in a Child. A Case-Based Review
Abstract
:1. Introduction
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baruteau, A.E.; Pass, R.H.; Thambo, J.B.; Behaghel, A.; Le Pennec, S.; Perdreau, E.; Combes, N.; Liberman, L.; McLeod, C.J. Congenital and childhood atrioventricular blocks: Pathophysiology and contemporary management. Eur. J. Pediatr. 2016, 175, 1235–1248. [Google Scholar] [CrossRef]
- Therrien, A.; Kelly, C.P.; Silvester, J.A. Celiac Disease: Extraintestinal Manifestations and Associated Conditions. J. Clin. Gastroenterol. 2020, 54, 8–21. [Google Scholar] [CrossRef]
- Frustaci, A.; Cuoco, L.; Chimenti, C.; Pieroni, M.; Fioravanti, G.; Gentiloni, N.; Maseri, A.; Gasbarrini, G. Celiac disease associated with autoimmune myocarditis. Circulation 2002, 105, 2611–2618. [Google Scholar] [CrossRef] [Green Version]
- Barra, S.N.; Providência, R.; Paiva, L.; Nascimento, J.; Marques, A.L. A review on advanced atrioventricular block in young or middle-aged adults. Pacing Clin. Electrophysiol. 2012, 35, 1395–1405. [Google Scholar] [CrossRef] [PubMed]
- Pinto-Sanchez, M.I.; Silvester, J.A.; Lebwohl, B.; Leffler, D.A.; Anderson, R.P.; Therrien, A.; Kelly, C.P.; Verdu, E.F. Society for the Study of Celiac Disease position statement on gaps and opportunities in coeliac disease. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 875–884. [Google Scholar] [CrossRef]
- Al-Toma, A.; Volta, U.; Auricchio, R.; Castillejo, G.; Sanders, D.S.; Cellier, C.; Mulder, C.J.; Lundin, K. European Society for the Study of Coeliac Disease (ESsCD) guideline for coeliac disease and other gluten-related disorders. United Eur. Gastroenterol. J. 2019, 7, 583–613. [Google Scholar] [CrossRef]
- Leffler, D.A.; Green, P.H.; Fasano, A. Extraintestinal manifestations of coeliac disease. Nat. Rev. Gastroenterol. Hepatol. 2015, 12, 561–571. [Google Scholar] [CrossRef]
- Hidalgo, D.F.; Boonpheng, B.; Nasr, L.; Sikandar, S.; Hidalgo, J.; Intriago, M. Celiac Disease and Risk of Atrial Fibrillation: A Meta-analysis and Systematic Review. Cureus 2020, 12, e6997. [Google Scholar] [CrossRef] [Green Version]
- Ciaccio, E.J.; Lewis, S.K.; Biviano, A.B.; Iyer, V.; Garan, H.; Green, P.H. Cardiovascular involvement in celiac disease. World J. Cardiol. 2017, 9, 652–666. [Google Scholar] [CrossRef]
- Saleh, F.; Greene, E.A.; Mathison, D. Evaluation and management of atrioventricular block in children. Curr. Opin. Pediatr. 2014, 26, 279–285. [Google Scholar] [CrossRef]
- Caio, G.; Volta, U.; Sapone, A.; Leffler, D.A.; De Giorgio, R.; Catassi, C.; Fasano, A. Celiac disease: A comprehensive current review. BMC Med. 2019, 17, 142. [Google Scholar] [CrossRef] [Green Version]
- Child Growth Standards. Available online: https://www.who.int/tools/child-growth-standards/standards/weight-for-length-height (accessed on 30 August 2022).
- Growth Reference Data for 5–19 Years. Available online: https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators/height-for-age (accessed on 30 August 2022).
- Callejas Rubio, J.L.; Ortego, N.; Díez-Ruiz, A.; Guilarte, J.; de la Higuera-Torres, J. Celiac disease presenting as chronic anemia associated with heart block. Am. J. Gastroenterol. 1998, 93, 1391–1392. [Google Scholar] [CrossRef]
- Santoro, L.; De Matteis, G.; Fuorlo, M.; Giupponi, B.; Martone, A.M.; Landi, F.; Landolfi, R.; Santoliquido, A. Atherosclerosis and cardiovascular involvement in celiac disease: The role of autoimmunity and inflammation. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 5437–5444. [Google Scholar] [CrossRef]
- Not, T.; Faleschini, E.; Tommasini, A.; Repetto, A.; Pasotti, M.; Baldas, V.; Spano, A.; Sblattero, D.; Marzari, R.; Campana, C.; et al. Celiac disease in patients with sporadic and inherited cardiomyopathies and in their relatives. Eur. Heart J. 2003, 24, 1455–1461. [Google Scholar] [CrossRef] [Green Version]
- Samy, L.; Barkun, A.; Huynh, T. Cardiac syncope in a woman with undiagnosed celiac disease. Can. Med. Assoc. J. 2017, 189, E365–E367. [Google Scholar] [CrossRef] [Green Version]
- Myrmel, G.M.S.; Lunde, T.; Saeed, S. Clinical spectrum of Celiac disease from a cardiology perspective. Pak. J. Med. Sci. 2022, 38, 782–784. [Google Scholar] [CrossRef]
- Mah, M.W.; Priel, I.E.; Humen, D.P.; Brown, N.E.; Sproule, B.J. Idiopathic pulmonary hemosiderosis, complete heart block and celiac disease. Can. J. Cardiol. 1989, 5, 191–194. [Google Scholar]
- Bernardi, N.; Sciatti, E.; Pancaldi, E.; Alghisi, F.; Drera, A.; Falco, R.; Vizzardi, E. Coeliac and cardiovascular disease: A possible relationship between two apparently separate conditions. Monaldi Arch. Chest Dis. 2022. [Google Scholar] [CrossRef]
- Brito-Zerón, P.; Izmirly, P.M.; Ramos-Casals, M.; Buyon, J.P.; Khamashta, M.A. The clinical spectrum of autoimmune congenital heart block. Nat. Rev. Rheumatol. 2015, 11, 301–312. [Google Scholar] [CrossRef]
- Ouali, S.; Chabrak, S.; Larbi, N.; Kafsi, N. Dilated cardiomyopathy and atrio-ventricular block in coeliac disease. Two case reports. Arch. Mal. Coeur Vaiss. 2006, 99, 1252–1255. [Google Scholar]
- Volta, U.; Caio, G.; Stanghellini, V.; De Giorgio, R. The changing clinical profile of celiac disease: A 15-year experience (1998–2012) in an Italian referral center. BMC Gastroenterol. 2014, 14, 194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vincent Cottin, G.C.-F. Celiac disease revealed by diffuse alveolar hemorrhage and heart block. Respir. Med. Extra 2006, 2, 89–91. [Google Scholar] [CrossRef]
- Myrsky, E.; Syrjänen, M.; Korponay-Szabo, I.R.; Mäki, M.; Kaukinen, K.; Lindfors, K. Altered small-bowel mucosal vascular network in untreated coeliac disease. Scand. J. Gastroenterol. 2009, 44, 162–167. [Google Scholar] [CrossRef]
- Chicco, D.; Taddio, A.; Sinagra, G.; Di Lenarda, A.; Ferrara, F.; Moretti, M.; Martelossi, S.; Di Toro, N.; Ventura, A.; Not, T. Speeding up coeliac disease diagnosis in cardiological settings. Arch. Med. Sci. 2010, 6, 728–732. [Google Scholar] [CrossRef]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mannarino, S.; Santacesaria, S.; Raso, I.; Fini, G.; Pozzi, E.; Cocuccio, C.; Calcaterra, V.; Zuccotti, G. Atrioventricular Block in Celiac Disease: An Unusual Clinical Presentation in a Child. A Case-Based Review. Children 2022, 9, 1627. https://doi.org/10.3390/children9111627
Mannarino S, Santacesaria S, Raso I, Fini G, Pozzi E, Cocuccio C, Calcaterra V, Zuccotti G. Atrioventricular Block in Celiac Disease: An Unusual Clinical Presentation in a Child. A Case-Based Review. Children. 2022; 9(11):1627. https://doi.org/10.3390/children9111627
Chicago/Turabian StyleMannarino, Savina, Sara Santacesaria, Irene Raso, Giulia Fini, Elena Pozzi, Cristina Cocuccio, Valeria Calcaterra, and Gianvincenzo Zuccotti. 2022. "Atrioventricular Block in Celiac Disease: An Unusual Clinical Presentation in a Child. A Case-Based Review" Children 9, no. 11: 1627. https://doi.org/10.3390/children9111627