Recent Progress and Challenges on the Microfluidic Assay of Pathogenic Bacteria Using Biosensor Technology
Abstract
:1. Introduction
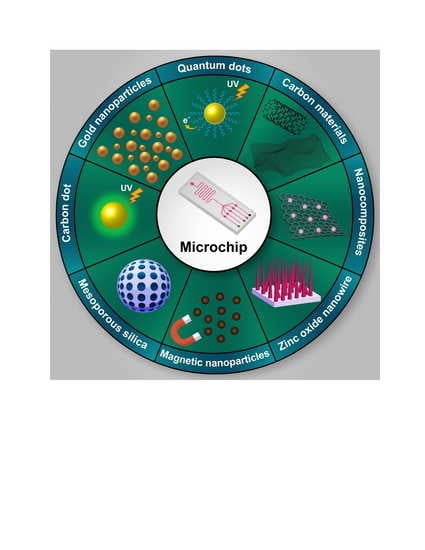
2. Current Methods of Bacterial Detection
3. Application of Microfluidic Biosensors for the Detection of Bacteria
3.1. Optical-Based Microfluidics Biosensor for the Detection of Pathogenic Bacteria
3.2. Paper-Based Microfluidics Biosensors for Pathogen Detection
3.3. Electrochemical-Based Microfluidics Biosensor for the Detection of Pathogenic Bacteria
3.4. Immuno-Based Microfluidics Biosensor for Pathogen Detection
3.5. Aptamer-Based Microfluidics Biosensor for Pathogen Detection
4. Conclusions and Future Perspectives
- Microfluidic with high chemical and thermal stability for special applications.
- Integration of microfluidic and nano fluidic sensors for complete formation and application systems that do not require a specialized workforce operation.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chuang, T.-L.; Chang, C.-C.; Chu-Su, Y.; Wei, S.-C.; Zhao, X.-H.; Hsueh, P.-R.; Lin, C.-W. Disposable surface plasmon resonance aptasensor with membrane-based sample handling design for quantitative interferon-gamma detection. Lab Chip 2014, 14, 2968–2977. [Google Scholar] [CrossRef] [PubMed]
- Mairhofer, J.; Roppert, K.; Ertl, P. Microfluidic systems for pathogen sensing: A review. Sensors 2009, 9, 4804–4823. [Google Scholar] [CrossRef] [PubMed]
- Man, Y.; Ban, M.; Li, A.; Jin, X.; Du, Y.; Pan, L. A microfluidic colorimetric biosensor for in-field detection of Salmonella in fresh-cut vegetables using thiolated polystyrene microspheres, hose-based microvalve and smartphone imaging APP. Food Chem. 2021, 354, 129578. [Google Scholar] [CrossRef] [PubMed]
- Xue, L.; Jin, N.; Guo, R.; Wang, S.; Qi, W.; Liu, Y.; Li, Y.; Lin, J. Microfluidic Colorimetric Biosensors Based on MnO2 Nanozymes and Convergence–Divergence Spiral Micromixers for Rapid and Sensitive Detection of Salmonella. ACS Sens. 2021, 6, 2883–2892. [Google Scholar] [CrossRef]
- Luka, G.; Ahmadi, A.; Najjaran, H.; Alocilja, E.; DeRosa, M.; Wolthers, K.; Malki, A.; Aziz, H.; Althani, A.; Hoorfar, M. Microfluidics integrated biosensors: A leading technology towards lab-on-a-chip and sensing applications. Sensors 2015, 15, 30011–30031. [Google Scholar] [CrossRef] [Green Version]
- Sarikaya, A.; Ladischi, M.; Geng, T.; Bhunia, A.; Apple, H.; Wereley, S. Microfluidic Biocliip for Impedance Spectroscopy of Biological Species. Biomed. Microdevices 2001, 3, 201–209. [Google Scholar]
- Whitesides, G.M. The origins and the future of microfluidics. Nature 2006, 442, 368–373. [Google Scholar] [CrossRef]
- Foudeh, A.M.; Didar, T.F.; Veres, T.; Tabrizian, M. Microfluidic designs and techniques using lab-on-a-chip devices for pathogen detection for point-of-care diagnostics. Lab Chip 2012, 12, 3249–3266. [Google Scholar] [CrossRef]
- Nasseri, B.; Soleimani, N.; Rabiee, N.; Kalbasi, A.; Karimi, M.; Hamblin, M.R. Point-of-care microfluidic devices for pathogen detection. Biosens. Bioelectron. 2018, 117, 112–128. [Google Scholar] [CrossRef]
- Sinha, A.; Tai, T.-Y.; Li, K.-H.; Gopinathan, P.; Chung, Y.-D.; Sarangadharan, I.; Ma, H.-P.; Huang, P.-C.; Shiesh, S.-C.; Wang, Y.-L. An integrated microfluidic system with field-effect-transistor sensor arrays for detecting multiple cardiovascular biomarkers from clinical samples. Biosens. Bioelectron. 2019, 129, 155–163. [Google Scholar] [CrossRef]
- Weng, X.; Neethirajan, S. Paper-based microfluidic aptasensor for food safety. J. Food Saf. 2018, 38, e12412. [Google Scholar] [CrossRef]
- Yu, Z.; Tang, Y.; Cai, G.; Ren, R.; Tang, D. Paper Electrode-Based Flexible Pressure Sensor for Point-of-Care Immunoassay with Digital Multimeter. Anal. Chem. 2019, 91, 1222–1226. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sachdeva, S.; Davis, R.W.; Saha, A.K. Microfluidic point-of-care testing: Commercial landscape and future directions. Front. Bioeng. Biotechnol. 2021, 8, 1602659. [Google Scholar] [CrossRef]
- Ren, K.; Zhou, J.; Wu, H. Materials for microfluidic chip fabrication. Acc. Chem. Res. 2013, 46, 2396–2406. [Google Scholar] [CrossRef] [PubMed]
- Pan, L.-J.; Tu, J.-W.; Ma, H.-T.; Yang, Y.-J.; Tian, Z.-Q.; Pang, D.-W.; Zhang, Z.-L. Controllable synthesis of nanocrystals in droplet reactors. Lab Chip 2018, 18, 41–56. [Google Scholar] [CrossRef] [PubMed]
- Rivet, C.; Lee, H.; Hirsch, A.; Hamilton, S.; Lu, H. Microfluidics for medical diagnostics and biosensors. Chem. Eng. Sci. 2011, 66, 1490–1507. [Google Scholar] [CrossRef]
- Zhao, X.; Li, M.; Liu, Y. Microfluidic-based approaches for foodborne pathogen detection. Microorganisms 2019, 7, 381. [Google Scholar] [CrossRef] [Green Version]
- Weibel, D.B.; Whitesides, G.M. Applications of microfluidics in chemical biology. Curr. Opin. Chem. Biol. 2006, 10, 584–591. [Google Scholar] [CrossRef]
- Hong, J.; Edel, J.B.; Demello, A.J. Micro-and nanofluidic systems for high-throughput biological screening. Drug Discov. Today 2009, 14, 134–146. [Google Scholar] [CrossRef]
- Bringer, M.R.; Gerdts, C.J.; Song, H.; Tice, J.D.; Ismagilov, R.F. Microfluidic systems for chemical kinetics that rely on chaotic mixing in droplets. Philos. Trans. R. Soc. London. Ser. A Math. Phys. Eng. Sci. 2004, 362, 1087–1104. [Google Scholar] [CrossRef] [Green Version]
- Yager, P.; Edwards, T.; Fu, E.; Helton, K.; Nelson, K.; Tam, M.R.; Weigl, B.H. Microfluidic diagnostic technologies for global public health. Nature 2006, 442, 412–418. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.; Chae, J. A regenerative biosensing surface in microfluidics using electrochemical desorption of short-chain self-assembled monolayer. Microfluid. Nanofluidics 2009, 7, 819–827. [Google Scholar] [CrossRef]
- Lazcka, O.; Del Campo, F.J.; Munoz, F.X. Pathogen detection: A perspective of traditional methods and biosensors. Biosens. Bioelectron. 2007, 22, 1205–1217. [Google Scholar] [CrossRef]
- Priyanka, B.; Patil, R.K.; Dwarakanath, S. A review on detection methods used for foodborne pathogens. Indian J. Med. Res. 2016, 144, 327. [Google Scholar] [CrossRef] [PubMed]
- Rohde, A.; Hammerl, J.A.; Appel, B.; Dieckmann, R.; Al Dahouk, S. FISHing for bacteria in food–A promising tool for the reliable detection of pathogenic bacteria? Food Microbiol. 2015, 46, 395–407. [Google Scholar] [CrossRef] [Green Version]
- Houpikian, P.; Raoult, D. Traditional and molecular techniques for the study of emerging bacterial diseases: One laboratory’s perspective. Emerg. Infect. Dis. 2002, 8, 122. [Google Scholar] [CrossRef] [Green Version]
- Chen, T.-L.; Lee, Y.-T.; Kuo, S.-C.; Yang, S.-P.; Fung, C.-P.; Lee, S.-D. Rapid identification of Acinetobacter baumannii, Acinetobacter nosocomialis and Acinetobacter pittii with a multiplex PCR assay. J. Med. Microbiol. 2014, 63, 1154–1159. [Google Scholar] [CrossRef]
- Yao, J.; Yang, M.; Duan, Y. Chemistry, biology, and medicine of fluorescent nanomaterials and related systems: New insights into biosensing, bioimaging, genomics, diagnostics, and therapy. Chem. Rev. 2014, 114, 6130–6178. [Google Scholar] [CrossRef]
- Silk, T.M.; Donnelly, C.W. Increased detection of acid-injured Escherichia coli O157:H7 in autoclaved apple cider by using nonselective repair on trypticase soy agar. J. Food Prot. 1997, 60, 1483–1486. [Google Scholar] [CrossRef]
- Heijnen, L.; Medema, G. Quantitative detection of E. coli, E. coli O157 and other shiga toxin producing E. coli in water samples using a culture method combined with real-time PCR. J. Water Health 2006, 4, 487–498. [Google Scholar] [CrossRef] [Green Version]
- Daly, P.; Collier, T.; Doyle, S. PCR-ELISA detection of Escherichia coli in milk. Lett. Appl. Microbiol. 2002, 34, 222–226. [Google Scholar] [CrossRef] [PubMed]
- Sapsford, K.E.; Rasooly, A.; Taitt, C.R.; Ligler, F.S. Detection of Campylobacter and Shigella species in food samples using an array biosensor. Anal. Chem. 2004, 76, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Perelle, S.; Dilasser, F.; Malorny, B.; Grout, J.; Hoorfar, J.; Fach, P. Comparison of PCR-ELISA and LightCycler real-time PCR assays for detecting Salmonella spp. in milk and meat samples. Mol. Cell. Probes 2004, 18, 409–420. [Google Scholar] [CrossRef] [PubMed]
- Ohk, S.-H.; Bhunia, A.K. Multiplex fiber optic biosensor for detection of Listeria monocytogenes, Escherichia coli O157:H7 and Salmonella enterica from ready-to-eat meat samples. Food Microbiol. 2013, 33, 166–171. [Google Scholar] [CrossRef]
- Wang, S.; Inci, F.; Chaunzwa, T.L.; Ramanujam, A.; Vasudevan, A.; Subramanian, S.; Ip, A.C.F.; Sridharan, B.; Gurkan, U.A.; Demirci, U. Portable microfluidic chip for detection of Escherichia coli in produce and blood. Int. J. Nanomed. 2012, 7, 2591. [Google Scholar]
- Wu, W.; Zhao, S.; Mao, Y.; Fang, Z.; Lu, X.; Zeng, L. A sensitive lateral flow biosensor for Escherichia coli O157:H7 detection based on aptamer mediated strand displacement amplification. Anal. Chim. Acta 2015, 861, 62–68. [Google Scholar] [CrossRef]
- Kant, K.; Shahbazi, M.-A.; Dave, V.P.; Ngo, T.A.; Chidambara, V.A.; Than, L.Q.; Bang, D.D.; Wolff, A. Microfluidic devices for sample preparation and rapid detection of foodborne pathogens. Biotechnol. Adv. 2018, 36, 1003–1024. [Google Scholar] [CrossRef] [Green Version]
- Tunc, I.; Susapto, H.H. Label-free detection of ovarian Cancer antigen CA125 by surface enhanced Raman scattering. J. Nanosci. Nanotechnol. 2020, 20, 1358–1365. [Google Scholar] [CrossRef]
- Liu, H.; Li, C.; Song, R.; Xu, S. A 3D mutilayer curved plasmonic coupling array with abundant and uniform hot spots for surface-enhanced Raman scattering. J. Phys. D Appl. Phys. 2019, 53, 055101. [Google Scholar] [CrossRef]
- Carneiro, M.C.; Sousa-Castillo, A.; Correa-Duarte, M.A.; Sales, M.G.F. Dual biorecognition by combining molecularly-imprinted polymer and antibody in SERS detection. Application to carcinoembryonic antigen. Biosens. Bioelectron. 2019, 146, 111761. [Google Scholar] [CrossRef]
- Lee, T.; Mohammadniaei, M.; Zhang, H.; Yoon, J.; Choi, H.K.; Guo, S.; Guo, P.; Choi, J.W. Single Functionalized pRNA/Gold Nanoparticle for Ultrasensitive MicroRNA Detection Using Electrochemical Surface-Enhanced Raman Spectroscopy. Adv. Sci. 2020, 7, 1902477. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Leustean, L.; Inci, F.; Zheng, M.; Demirci, U.; Wang, S. Plasmonic-based platforms for diagnosis of infectious diseases at the point-of-care. Biotechnol. Adv. 2019, 37, 107440. [Google Scholar] [CrossRef] [PubMed]
- Sakir, M.; Salem, S.; Sanduvac, S.T.; Sahmetlioglu, E.; Sarp, G.; Onses, M.S.; Yilmaz, E. Photocatalytic green fabrication of Au nanoparticles on ZnO nanorods modified membrane as flexible and photocatalytic active reusable SERS substrates. Colloids Surf. A Physicochem. Eng. Asp. 2020, 585, 124088. [Google Scholar] [CrossRef]
- Bhardwaj, H.; Sumana, G.; Marquette, C.A. A label-free ultrasensitive microfluidic surface Plasmon resonance biosensor for Aflatoxin B1 detection using nanoparticles integrated gold chip. Food Chem. 2020, 307, 125530. [Google Scholar] [CrossRef]
- Das, C.M.; Ouyang, Q.; Dinh, X.-Q.; Coquet, P.; Yong, K.-T. A theoretical insight into the use of anti-reflective coatings for the upliftment of sensitivity of surface plasmon resonance sensors. Opt. Commun. 2020, 458, 124748. [Google Scholar] [CrossRef]
- Farmani, H.; Farmani, A.; Biglari, Z. A label-free graphene-based nanosensor using surface plasmon resonance for biomaterials detection. Phys. E Low-Dimens. Syst. Nanostruct. 2020, 116, 113730. [Google Scholar] [CrossRef]
- Zeng, R.; Gong, H.; Li, Y.; Li, Y.; Lin, W.; Tang, D.; Knopp, D. CRISPR-Cas12a-Derived Photoelectrochemical Biosensor for Point-Of-Care Diagnosis of Nucleic Acid. Anal. Chem. 2022, 94, 7442–7448. [Google Scholar] [CrossRef]
- Chen, X.; Nan, Y.; Ma, X.; Liu, H.; Liu, W.; Shi, L.; Guo, T. In-situ detection of small biomolecule interactions using a plasmonic tilted fiber grating sensor. J. Lightwave Technol. 2019, 37, 2792–2799. [Google Scholar] [CrossRef]
- Lao, J.; Han, L.; Wu, Z.; Zhang, X.; Huang, Y.; Tang, Y.; Guo, T. Gold nanoparticle-functionalized surface plasmon resonance optical fiber biosensor: In situ detection of thrombin with 1 n·M detection limit. J. Lightwave Technol. 2019, 37, 2748–2755. [Google Scholar] [CrossRef]
- Lobry, M.; Lahem, D.; Loyez, M.; Debliquy, M.; Chah, K.; David, M.; Caucheteur, C. Non-enzymatic D-glucose plasmonic optical fiber grating biosensor. Biosens. Bioelectron. 2019, 142, 111506. [Google Scholar] [CrossRef] [Green Version]
- Loyez, M.; Ribaut, C.; Caucheteur, C.; Wattiez, R. Functionalized gold electroless-plated optical fiber gratings for reliable surface biosensing. Sens. Actuators B Chem. 2019, 280, 54–61. [Google Scholar] [CrossRef]
- Sypabekova, M.; Korganbayev, S.; González-Vila, Á.; Caucheteur, C.; Shaimerdenova, M.; Ayupova, T.; Bekmurzayeva, A.; Vangelista, L.; Tosi, D. Functionalized etched tilted fiber Bragg grating aptasensor for label-free protein detection. Biosens. Bioelectron. 2019, 146, 111765. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Zhu, L.; Sun, G.; Meng, F.; Song, Y. Fiber brag grating monitoring of a morphing wing based on a polyvinyl chloride reinforced silicone substrate. Opt. Fiber Technol. 2019, 50, 145–153. [Google Scholar] [CrossRef]
- Zhou, Q.; Tang, D. Recent advances in photoelectrochemical biosensors for analysis of mycotoxins in food. Trends Anal. Chem. 2020, 124, 115814. [Google Scholar] [CrossRef]
- Zhou, Q.; Lin, Y.; Zhang, K.; Li, M.; Tang, D. Reduced graphene oxide/BiFeO3 nanohybrids-based signal-on photoelectrochemical sensing system for prostate-specific antigen detection coupling with magnetic microfluidic device. Biosens Bioelectron. 2018, 101, 146–152. [Google Scholar] [CrossRef]
- Qiu, Z.; Shu, J.; Tang, D. Bioresponsive Release System for Visual Fluorescence Detection of Carcinoembryonic Antigen from Mesoporous Silica Nanocontainers Mediated Optical Color on Quantum Dot-Enzyme-Impregnated Paper. Anal. Chem. 2017, 89, 5152–5160. [Google Scholar] [CrossRef]
- Lv, S.; Tang, Y.; Zhang, K.; Tang, D. Wet NH3-Triggered NH2-MIL-125(Ti) Structural Switch for Visible Fluorescence Immunoassay Impregnated on Paper. Anal. Chem. 2018, 90, 14121–14125. [Google Scholar] [CrossRef] [Green Version]
- Yin, Z.; Zhu, L.; Lv, Z.; Li, M.; Tang, D. Persistent luminescence nanorods-based autofluorescence-free biosensor for prostate-specific antigen detection. Talanta 2021, 233, 122563. [Google Scholar] [CrossRef]
- Huang, L.; Wang, J.; Wang, Q.; Tang, D.; Yao, L. Distance-dependent visual fluorescence immunoassay on CdTe quantum dot-impregnated paper through silver ion-exchange reaction. Microchim Acta. 2020, 187, 563. [Google Scholar] [CrossRef]
- Huang, L.; Chen, J.; Yu, Z.; Tang, D. Self-Powered Temperature Sensor with Seebeck Effect Transduction for Photothermal-Thermoelectric Coupled Immunoassay. Anal. Chem. 2020, 92, 2809–2814. [Google Scholar] [CrossRef]
- Yu, Z.; Gong, H.; Xu, J.; Li, Y.; Xue, F.; Zeng, Y.; Liu, X.; Tang, D. Liposome-Embedded Cu2- xAgxS Nanoparticle-Mediated Photothermal Immunoassay for Daily Monitoring of cTnI Protein Using a Portable Thermal Imager. Anal. Chem. 2022, 94, 7408–7416. [Google Scholar] [CrossRef] [PubMed]
- Lv, S.; Zhang, K.; Zhu, L.; Tang, D.; Niessner, R.; Knopp, D. H2-Based Electrochemical Biosensor with Pd Nanowires@ZIF-67 Molecular Sieve Bilayered Sensing Interface for Immunoassay. Anal. Chem. 2019, 91, 12055–12062. [Google Scholar] [CrossRef] [PubMed]
- Azinheiro, S.; Kant, K.; Shahbazi, M.A.; Garrido-Maestu, A.; Prado, M.; Dieguez, L. A smart microfluidic platform for rapid multiplexed detection of foodborne pathogens. Food Control 2020, 114, 107242. [Google Scholar] [CrossRef]
- Zhang, J.; Liu, Q.; Ba, Y.; Cheng, J.; Yang, H.; Cui, Y.; Kong, J.; Zhang, X. F-containing initiatior for ultrasensitive fluorescent detection of lung cancer DNA via atom transfer radical polymerization. Anal. Chim. Acta 2020, 1094, 99–105. [Google Scholar] [CrossRef]
- Kim, K.-I.; Han, C.-H.; Choe, Y.-A.; Ju, K.-S.; Ri, D.-H.; Ri, S.-B.; Kim, S. Influence of temperature and humidity on the detection of benzene vapor by a piezoelectric crystal sensor. Instrum. Sci. Technol. 2019, 47, 436–447. [Google Scholar] [CrossRef]
- Pohanka, M. Piezoelectric immunosensor for the determination of C-Reactive protein. Int. J. Electrochem. Sci 2019, 14, 8470–8478. [Google Scholar] [CrossRef]
- Urdinola, K.B.; Muñoz, P.A.M.; Marín, P.A.; Grajales, M.J. In-Silico Prediction on the MSAMS-Assisted Immobilization of Bovine Serum Albumin on 10 MHz Piezoelectric Immunosensors. J. Mol. Eng. Mater. 2019, 7, 1950001. [Google Scholar] [CrossRef]
- Yuan, M.; Zhang, Q.; Song, Z.; Ye, T.; Yu, J.; Cao, H.; Xu, F. Piezoelectric arsenite aptasensor based on the use of a self-assembled mercaptoethylamine monolayer and gold nanoparticles. Microchim. Acta 2019, 186, 268. [Google Scholar] [CrossRef]
- Zamora-Sequeira, R.; Starbird-Pérez, R.; Rojas-Carillo, O.; Vargas-Villalobos, S. What are the main sensor methods for quantifying pesticides in agricultural activities? A review. Molecules 2019, 24, 2659. [Google Scholar] [CrossRef] [Green Version]
- Arora, P.; Sindhu, A.; Dilbaghi, N.; Chaudhury, A. Biosensors as innovative tools for the detection of food borne pathogens. Biosens. Bioelectron. 2011, 28, 1–12. [Google Scholar] [CrossRef]
- Qiu, J.; Zhou, Y.; Chen, H.; Lin, J.-M. Immunomagnetic separation and rapid detection of bacteria using bioluminescence and microfluidics. Talanta 2009, 79, 787–795. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, K.A.; Chua, B.; Son, A. Development of first generation in-situ pathogen detection system (Gen1-IPDS) based on NanoGene assay for near real time E. coli O157:H7 detection. Biosens. Bioelectron. 2014, 54, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Foudeh, A.M.; Daoud, J.T.; Faucher, S.P.; Veres, T.; Tabrizian, M. Sub-femtomole detection of 16s rRNA from Legionella pneumophila using surface plasmon resonance imaging. Biosens. Bioelectron. 2014, 52, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Tokel, O.; Yildiz, U.H.; Inci, F.; Durmus, N.G.; Ekiz, O.O.; Turker, B.; Cetin, C.; Rao, S.; Sridhar, K.; Natarajan, N. Portable microfluidic integrated plasmonic platform for pathogen detection. Sci. Rep. 2015, 5, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Frasco, M.F.; Chaniotakis, N. Semiconductor quantum dots in chemical sensors and biosensors. Sensors 2009, 9, 7266–7286. [Google Scholar] [CrossRef] [Green Version]
- SalmanOgli, A. Nanobio applications of quantum dots in cancer: Imaging, sensing, and targeting. Cancer Nanotechnol. 2011, 2, 1–19. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Z.; Li, Y.; Li, P.; Zhang, Q.; Zhang, W.; Hu, X.; Ding, X. Monoclonal antibody-quantum dots CdTe conjugate-based fluoroimmunoassay for the determination of aflatoxin B1 in peanuts. Food Chem. 2014, 146, 314–319. [Google Scholar] [CrossRef]
- Sahoo, S.K. Sensing and biosensing with optically active nanomaterials: A note. In Sensing and Biosensing with Optically Active Nanomaterials; Elsevier: Amsterdam, The Netherlands, 2022; pp. 1–7. [Google Scholar]
- Fernández-Argüelles, M.; Costa-Fernández, J.M.; Pereiro, R.; Sanz-Medel, A. Simple bio-conjugation of polymer-coated quantum dots with antibodies for fluorescence-based immunoassays. Analyst 2008, 133, 444–447. [Google Scholar] [CrossRef]
- Speranskaya, E.S.; Beloglazova, N.V.; Abé, S.; Aubert, T.; Smet, P.F.; Poelman, D.; Goryacheva, I.Y.; De Saeger, S.; Hens, Z. Hydrophilic, bright CuInS2 quantum dots as Cd-free fluorescent labels in quantitative immunoassay. Langmuir 2014, 30, 7567–7575. [Google Scholar] [CrossRef]
- Reza, K.K.; Dey, S.; Wuethrich, A.; Wang, J.; Behren, A.; Antaw, F.; Wang, Y.; Sina, A.A.I.; Trau, M. In situ single cell proteomics reveals circulating tumor cell heterogeneity during treatment. ACS Nano 2021, 15, 11231–11243. [Google Scholar] [CrossRef]
- Santhiago, M.; Nery, E.W.; Santos, G.P.; Kubota, L.T. Microfluidic paper-based devices for bioanalytical applications. Bioanalysis 2014, 6, 89–106. [Google Scholar] [CrossRef] [PubMed]
- Noviana, E.; Ozer, T.; Carrell, C.S.; Link, J.S.; McMahon, C.; Jang, I.; Henry, C.S. Microfluidic Paper-Based Analytical Devices: From Design to Applications. Chem. Rev. 2021, 121, 11835–11885. [Google Scholar] [CrossRef] [PubMed]
- Martinez, A.W.; Phillips, S.T.; Butte, M.J.; Whitesides, G.M. Patterned paper as a platform for inexpensive, low-volume, portable bioassays. Angew. Chem. 2007, 119, 1340–1342. [Google Scholar] [CrossRef]
- Beveridge, J.S.; Stephens, J.R.; Williams, M.E. The use of magnetic nanoparticles in analytical chemistry. Annu. Rev. Anal. Chem. 2011, 4, 251–273. [Google Scholar] [CrossRef] [PubMed]
- Fronczek, C.F.; San Park, T.; Harshman, D.K.; Nicolini, A.M.; Yoon, J.-Y. Paper microfluidic extraction and direct smartphone-based identification of pathogenic nucleic acids from field and clinical samples. RSC Adv. 2014, 4, 11103–11110. [Google Scholar] [CrossRef]
- Sayad, A.; Ibrahim, F.; Uddin, S.M.; Cho, J.; Madou, M.; Thong, K.L. A microdevice for rapid, monoplex and colorimetric detection of foodborne pathogens using a centrifugal microfluidic platform. Biosens. Bioelectron. 2018, 100, 96–104. [Google Scholar] [CrossRef]
- Santhiago, M.; Kubota, L.T. A new approach for paper-based analytical devices with electrochemical detection based on graphite pencil electrodes. Sens. Actuators B Chem. 2013, 177, 224–230. [Google Scholar] [CrossRef]
- Carvalhal, R.F.; Simão Kfouri, M.; de Oliveira Piazetta, M.H.; Gobbi, A.L.; Kubota, L.T. Electrochemical detection in a paper-based separation device. Anal. Chem. 2010, 82, 1162–1165. [Google Scholar] [CrossRef]
- Jiang, H.; Sun, Z.; Guo, Q.; Weng, X. Microfluidic thread-based electrochemical aptasensor for rapid detection of Vibrio parahaemolyticus. Biosens. Bioelectron. 2021, 182, 113191. [Google Scholar] [CrossRef]
- Chen, Q.; Wang, D.; Cai, G.; Xiong, Y.; Li, Y.; Wang, M.; Huo, H.; Lin, J. Fast and sensitive detection of foodborne pathogen using electrochemical impedance analysis, urease catalysis and microfluidics. Biosens. Bioelectron. 2016, 86, 770–776. [Google Scholar] [CrossRef]
- Luo, J.; Fang, X.; Ye, D.; Li, H.; Chen, H.; Zhang, S.; Kong, J. A real-time microfluidic multiplex electrochemical loop-mediated isothermal amplification chip for differentiating bacteria. Biosens. Bioelectron. 2014, 60, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Liang, C.; Chu, Y.; Cheng, S.; Wu, H.; Kajiyama, T.; Kambara, H.; Zhou, G. Multiplex loop-mediated isothermal amplification detection by sequence-based barcodes coupled with nicking endonuclease-mediated pyrosequencing. Anal. Chem. 2012, 84, 3758–3763. [Google Scholar] [CrossRef]
- Zhang, Y.; Hu, J.; Zhang, C.-Y. Sensitive detection of transcription factors by isothermal exponential amplification-based colorimetric assay. Anal. Chem. 2012, 84, 9544–9549. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Chen, F.; Wu, Y.; Dong, Y.; Fan, C. Highly sensitive fluorescence assay of DNA methyltransferase activity via methylation-sensitive cleavage coupled with nicking enzyme-assisted signalamplification. Biosens. Bioelectron. 2013, 42, 56–61. [Google Scholar] [CrossRef]
- Cui, L.; Ke, G.; Zhang, W.Y.; Yang, C.J. A universal platform for sensitive and selective colorimetric DNA detection based on Exo III assisted signal amplification. Biosens. Bioelectron. 2011, 26, 2796–2800. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Xue, X.; Li, T.; Zeng, H.; Liu, X. Ultrasensitive and selective colorimetric DNA detection by nicking endonuclease assisted nanoparticle amplification. Angew. Chem. Int. Ed. 2009, 48, 6849–6852. [Google Scholar] [CrossRef]
- Pang, B.; Ding, X.; Wang, G.; Zhao, C.; Xu, Y.; Fu, K.; Sun, J.; Song, X.; Wu, W.; Liu, Y. Rapid and quantitative detection of Vibrio parahemolyticus by the mixed-dye-based loop-mediated isothermal amplification assay on a self-priming compartmentalization microfluidic chip. J. Agric. Food Chem. 2017, 65, 11312–11319. [Google Scholar] [CrossRef]
- Anik, Ü. Electrochemical medical biosensors for POC applications. In Medical Biosensors for Point of Care (POC) Applications; Elsevier: Amsterdam, The Netherlands, 2017; pp. 275–292. [Google Scholar]
- Sardesai, N.P.; Barron, J.C.; Rusling, J.F. Carbon nanotube microwell array for sensitive electrochemiluminescent detection of cancer biomarker proteins. Anal. Chem. 2011, 83, 6698–6703. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Niessner, R.; Tang, D.; Knopp, D. Nanoparticle-based immunosensors and immunoassays for aflatoxins. Anal. Chim. Acta 2016, 912, 10–23. [Google Scholar] [CrossRef]
- Zhu, L.; He, J.; Cao, X.; Huang, K.; Luo, Y.; Xu, W. Development of a double-antibody sandwich ELISA for rapid detection of Bacillus Cereus in food. Sci. Rep. 2016, 6, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Dirks, R.M.; Pierce, N.A. Triggered amplification by hybridization chain reaction. Proc. Natl. Acad. Sci. USA 2004, 101, 15275–15278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, C.; Song, Y.; Jang, K.; Choi, C.-H.; Na, S. Target switching catalytic hairpin assembly and gold nanoparticle colorimetric for EGFR mutant detection. Sens. Actuators B Chem. 2018, 261, 497–504. [Google Scholar] [CrossRef]
- Li, B.; Jiang, Y.; Chen, X.; Ellington, A.D. Probing spatial organization of DNA strands using enzyme-free hairpin assembly circuits. J. Am. Chem. Soc. 2012, 134, 13918–13921. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, L.; Xu, Y.; Ferhan, A.R.; Chen, G.; Kim, D.-H. Oriented gold nanoparticle aggregation for colorimetric sensors with surprisingly high analytical figures of merit. J. Am. Chem. Soc. 2013, 135, 12338–12345. [Google Scholar] [CrossRef] [PubMed]
- Julich, S.; Hotzel, H.; Gärtner, C.; Trouchet, D.; Ahmed, M.F.E.M.; Kemper, N.; Tomaso, H. Evaluation of a microfluidic chip system for preparation of bacterial DNA from swabs, air, and surface water samples. Biologicals 2016, 44, 574–580. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boehm, D.A.; Gottlieb, P.; Hua, S.Z. Surface functionalization of a microfluidic biosensor for bacteria detection and identification. In Proceedings of the Sensors and Smart Structures Technologies for Civil, Mechanical, and Aerospace Systems 2007, San Diego, CA, USA, 19–22 March 2007; pp. 193–200. [Google Scholar]
- Huang, F.; Xue, L.; Qi, W.; Cai, G.; Liu, Y.; Lin, J. An ultrasensitive impedance biosensor for Salmonella detection based on rotating high gradient magnetic separation and cascade reaction signal amplification. Biosens. Bioelectron. 2021, 176, 112921. [Google Scholar] [CrossRef]
- Oh, S.Y.; Heo, N.S.; Shukla, S.; Cho, H.-J.; Vilian, A.; Kim, J.; Lee, S.Y.; Han, Y.-K.; Yoo, S.M.; Huh, Y.S. Development of gold nanoparticle-aptamer-based LSPR sensing chips for the rapid detection of Salmonella typhimurium in pork meat. Sci. Rep. 2017, 7, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Jiang, Y.; Zou, S.; Cao, X. A simple dendrimer-aptamer based microfluidic platform for E. coli O157:H7 detection and signal intensification by rolling circle amplification. Sens. Actuators B Chem. 2017, 251, 976–984. [Google Scholar] [CrossRef]
- Hao, X.; Yeh, P.; Qin, Y.; Jiang, Y.; Qiu, Z.; Li, S.; Le, T.; Cao, X. Aptamer surface functionalization of microfluidic devices using dendrimers as multi-handled templates and its application in sensitive detections of foodborne pathogenic bacteria. Anal. Chim. Acta 2019, 1056, 96–107. [Google Scholar] [CrossRef]
- Macedo, B.; Cordeiro, Y. Unraveling prion protein interactions with aptamers and other PrP-binding nucleic acids. Int. J. Mol. Sci. 2017, 18, 1023. [Google Scholar] [CrossRef] [Green Version]
- Cai, H.; Parks, J.; Wall, T.; Stott, M.; Stambaugh, A.; Alfson, K.; Griffiths, A.; Mathies, R.; Carrion, R.; Patterson, J. Optofluidic analysis system for amplification-free, direct detection of Ebola infection. Sci. Rep. 2015, 5, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.; Kim, H.; Heo, Y.; Yoo, Y.K.; Han, S.I.; Kim, C.; Hur, D.; Kim, H.; Kang, J.Y.; Lee, J.H. Enhanced paper-based ELISA for simultaneous EVs/exosome isolation and detection using streptavidin agarose-based immobilization. Analyst 2020, 145, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Zhuang, J.; Nie, L.; Zhang, J.; Zhang, Y.; Gu, N.; Wang, T.; Feng, J.; Yang, D.; Perrett, S. Intrinsic peroxidase-like activity of ferromagnetic nanoparticles. Nat. Nanotechnol. 2007, 2, 577–583. [Google Scholar] [CrossRef] [PubMed]








| Method | Bacteria | Limit of Detection (LOD) | Pre-Enrichment Time | Detection Time | Ref |
|---|---|---|---|---|---|
| Plate culture | E. coli O157:H7 | 105 CFU/mL | 48–72 h | Not reported | [29] |
| PCR | E. coli O157 | 1 CFU/mL | 16–20 h | ~3 h | [30] |
| PCR-ELISA | E. coli | 102 CFU/mL | 16 h | ~4 h | [31] |
| ELISA | Shigella dysenteriae | ~104 CFU/mL | 48 h | ~4 h | [32] |
| PCR-ELISA | Salmonella spp. | 103 CFU/mL | 18 h | ~5 h | [33] |
| Fiber optic biosensor | Listeria, E. coli O157:H7, Salmonella | ~103 CFU/mL ~103 CFU/mL ~103 CFU/mL | 24 h 24 h 24 h | ~2 h ~2 h ~2 h | [34] |
| Immune-based microchip | E. coli | 50 CFU/mL | 16 h | ~3 h | [35] |
| Aptamer based biosensor | E. coli O157:H7 | 10 CFU/mL | 16 h | ~1.5 h | [36] |
| Target Pathogen | Detection Limit | Method | Assay Time | Ref |
|---|---|---|---|---|
| E. coli O157:H7 | 49 × 10−15 CFU/mL | Surface plasmon resonance integrated microfluidic | Not reported | [72] |
| Legionella pneumophila | 0.45 FM | Surface plasmon resonance integrated microfluidic | Less than 3 h | [73] |
| E. coli and S. aureus | 3.2 × 107, 3.2×105 CFU/mL | Surface plasmon resonance integrated microfluidic | Not reported | [74] |
| Salmonella | 4.4 × 101 to 4.4 × 106 CFU/mL | Microfluidic Colorimetric Biosensor | 45 min | [4] |
| Pseudomonas aeruginosa and Staphylococcus aureus | 500–5000 CFU/mL | Microfluidic Colorimetric Biosensor | Not reported | [85] |
| Salmonella typhimurium | 10 3 CFU/mL, 10 4 CFU/mL | Paper microfluidic | Not reported | [86] |
| Escherichia coli, Salmonella and Vibrio cholerae | 3 × 10−5 ng μL−1 | microfluidic colorimetric biosensor supported by LAMP | 60 min | [87] |
| Salmonella | 6.0 × 101 CFU/mL. | microfluidic colorimetric biosensor | Not reported | [3] |
| Vibrio parahaemolyticus | 5.74 CFU/mL 10–106 CFU/mL | electrochemical aptasensor -based microfluidic | 30 min | [90] |
| Listeria | 1.6×102 CFU/mL | Electrochemical based microfluidic | ~1 h | [91] |
| Mycobacterium tuberculosis (MTB), Haemophilus influenza (HIN), and Klebsiella pneumonia (KPN) | 28 μL−1 17 μL−1 16 μL−1 | electrode-based multiplex microfluidic chip supported by LAMP | 45 min | [92] |
| Vibrio parahemolyticus | 1 ×103 CFU/mL | LAMP | Not reported | [98] |
| Bacillus thuringiensis, Francisella tularensis | 4 × 102 GE/cm2 4 × 103 GE/cm2 | Immunoassay-based microfluidics biosensor | Not reported | [107] |
| E. coli, M. catarrhalis | 9 × 105 CFU/mL | Immunoassay-based microfluidics biosensor | Not reported | [108] |
| Salmonella | 5.3 × 10−2% (w/v) by BAC 2.7 × 10−2% (w/v) without BAC. high sensitivity with up to 98% | immunofluorescence -based microfluidics | Not reported | [71] |
| Salmonella | 101 CFU/mL | immunoassay-based microfluidics | 2 h | [109] |
| S. typhimurium | 10 × 104 CFU/mL | localized surface plasmon resonance (LSPR) sensing chip | within 30 to 35 min | [110] |
| S. aureus, Vibrio parahemolyticus, and S. Typhimurium | 25 CFU/mL 10 CFU/mL 15 CFU/mL | multiplex lateral flow test strip sensor (Luminescence) | Not reported | [59] |
| E. coli O157:H7 | 102 cells/mL | dendrimer-aptamer-RCA microfluidic | Not reported | [111] |
| E. coli O157:H7 | 102 mL−1 cells | Mixes dendrimer-aptamer-RCA microfluidic | Not reported | [112] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bahavarnia, F.; Hasanzadeh, M.; Sadighbayan, D.; Seidi, F. Recent Progress and Challenges on the Microfluidic Assay of Pathogenic Bacteria Using Biosensor Technology. Biomimetics 2022, 7, 175. https://doi.org/10.3390/biomimetics7040175
Bahavarnia F, Hasanzadeh M, Sadighbayan D, Seidi F. Recent Progress and Challenges on the Microfluidic Assay of Pathogenic Bacteria Using Biosensor Technology. Biomimetics. 2022; 7(4):175. https://doi.org/10.3390/biomimetics7040175
Chicago/Turabian StyleBahavarnia, Farnaz, Mohammad Hasanzadeh, Deniz Sadighbayan, and Farzad Seidi. 2022. "Recent Progress and Challenges on the Microfluidic Assay of Pathogenic Bacteria Using Biosensor Technology" Biomimetics 7, no. 4: 175. https://doi.org/10.3390/biomimetics7040175