1. Introduction
Wound healing is a highly complex and dynamic process for restoring impaired or injured tissue to its original physiological form. Full-thickness wounds can be divided into acute or chronic based on the wound-healing progress. These wounds are mainly caused by trauma, infections, immobility, or chronic illness [
1,
2]. Immediate wound management is a realistic approach to improving the rate of healing and minimizing the risk of complications. Dressings and antibiotics are the gold standards for wound-management approaches at the moment. However, ideal wound care has yet to be achieved. In addition, healed wounds develop hypertrophic scars that lead to movement restriction and cosmetic concerns [
3,
4]. It has been reported that treatment costs are in the range of USD 28.1 to 96.8 billion for 8.2 million Medicare beneficiaries [
5]. Hence, a new spectrum in wound-healing technology is essentially necessary. Cutaneous scarring affects 80 million people worldwide, while hypertrophic scarring occurs explicitly in 40–70% of third-degree burn patients [
3]. The current wound-care technologies aim to develop an ideal wound dressing to cater to these problems; it must retain moisture, be biocompatible and biodegradable, promote angiogenesis, and completely re-epithelialize [
3].
Additionally, among the disadvantages of a collagen–gelatin wound dressing is the formation of scarring-contracted tissue [
6,
7]. This scenario could be potentially overcome by adding elastin to the biomaterial fabrication as a distinguished strategy. Elastin is not produced immediately after birth; however, its production can be induced by injuries or diseases but is inadequately expressed during the wound-healing process [
8]. As a result, the intact elastic fiber network appearance is long delayed after injury, hence reducing the mechanical strength and scar elasticity compared to normal physiological skin [
8].
Tissue-engineering technology relies on developing 3D porous biomaterials that provide a microenvironment that resembles the native tissue anatomical structure and proper biodegradation that existed prior to the newly formed tissue. Additionally, it supports the tissue, promotes cell attachment and cell proliferation, and provides signaling molecules to promote tissue regeneration [
9]. Moreover, it functions as a carrier for active or therapeutic compounds to the wound sites [
8]. A feasible strategy for materials’ hybridization could improve the properties and successfully act as a controlled-release device for the incorporation of biomolecules to expedite wound healing. A 2019 review reported that natural-based biomaterials such as collagen, gelatin, and elastin have been widely used in tissue engineering due to their excellent physicochemical and mechanical properties. In addition, they could also reduce prolonged inflammation and immune rejection post-implantation at the wound site [
9].
Existing proteases and enzymes tend to remodel the natural biomaterials in the body. Although natural biomaterials have different stiffness properties, they have relatively low mechanical propensity [
10]. Nevertheless, they can be further modified to develop functionalized biomaterials that require only temporary remodeling at the implanted site [
11]. However, a single type of biomaterial may not meet all the requirements needed for an optimum wound-healing biomaterial due to its advantages and disadvantages. Therefore, researchers will utilize two or more biomaterials to improve the physicochemical and mechanical properties to obtain biomaterial designs that are intended for a final wound-healing application [
12].
The elastin-based biomaterial has gained interest in tissue engineering due to its good biocompatibility, biomechanical, and biodegradation properties in addition to decreasing wound contraction by regulating fibroblast differentiation, elevating dermal regeneration, and enhancing skin elasticity [
13,
14]. Elastin is the second most common structural component in the extracellular matrix (ECM). It plays an essential role in wound healing and contributes to many living tissues’ elasticity and resilience [
15,
16]. Elastin peptides modulate the cellular response to induce monocyte chemotactic and fibroblast migration and proliferation, protease production, keratinocyte migration, smooth muscle proliferation, and promotion of an angiogenic phenotype in endothelial cells [
17,
18,
19,
20,
21,
22,
23]. The remodeling outcome is dependent upon the favorable response of the host immune system. Native ECM is composed of collagen and elastin; therefore, skin wound-dressing biomaterial should include collagen and elastin as the primary biomaterials [
15].
Collagen is the most abundant protein in the ECM, with approximate 30% of total body proteins. Therefore, collagen is a favorable biomaterial for skin wound-healing applications. Collagen contributes to cell attachment, migration, proliferation, and differentiation and gene expression through specific cell receptors and cell-binding sites, and retention, local storage, and delivery of growth factors and cytokines. These attributes play a key role in organogenesis and tissue regeneration [
12,
24]. Gelatin is also known as a molecular derivative of type I collagen due to several of its advantages compared to its precursor. Firstly, it is a promising material in tissue engineering due to its chemical similarities with ECM in the native tissues. It has functional groups that allow facile chemical modifications with other biomaterials of biomolecules [
25]. Gelatin contributes to a balanced hydrophobicity/hydrophilicity of the fabricated biomaterials, resulting in an appropriate release of the bioactive compounds [
1]. Its susceptibility to enzymatic degradation can be used to generate controlled release materials.
Furthermore, it is necessary to confer structural stability to the implanted biomaterials by introducing exogenous cross-linking into the molecular structure [
26]. Exogenous cross-linking agents stabilize the collagen molecule by forming covalent and hydrogen bonds between the fibers [
24]. In addition, the cross-link formation can protect or amend major antigenic receptors and decrease their capacity to bind with antibodies [
22]. However, the synthetic cross-linker is commonly portrayed as a potentially toxic substance, leading to switching to naturally derived cross-linkers [
27]. Therefore, cross-linking agents that are not detrimental to the biomechanics and biocompatibility of the ECM, such as genipin (GNP), may present a good option [
28]. GNP is an aglycone, which is extracted from an iridoid glycoside, called geniposide, from the fruits of
Gardenia jasminoides Ellis. It is a cross-linking agent with high efficacy, good biocompatibility, and insignificant toxicity, and it inhibits fibroblast-induced contraction [
28,
29]. The GNP reacts with primary amines through a nucleophilic attack while, simultaneously, the ring opening of polymerization of GNP creates long-range intermolecular cross-linking [
29,
30]. This long-range intermolecular cross-linking leads to improved mechanical properties and resistance against enzymatic hydrolysis [
31]. Therefore, using functional hybrid biomaterials with natural cross-linkers, incorporated for the rapid treatment of full-thickness wound-care management, is worth explaining.
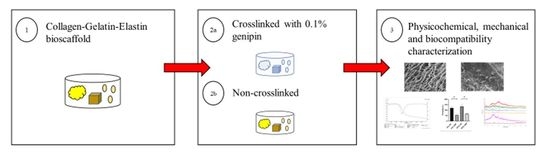
This study aimed to develop a 3D hybrid biomaterial from a combination of collagen (extracted from ovine tendon), Halal gelatin (Nitta Gelatin Inc., Osaka, Japan), and elastin (produced from poultry skin) cross-linked with a natural GNP cross-linker. The biomaterial was fabricated via a freeze-dryer approach followed by physicochemical, mechanical, and cell–biomaterial interaction evaluations.
2. Materials and Methods
This study protocol was approved by the Universiti Kebangsaan Malaysia (UKM) Research Ethics Committee (Code No. JEP-2019-424).
2.1. Collagen Type I Extraction and Purification
The extraction of collagen type I was performed as previously described by Fauzi et al. with some modifications [
32]. Briefly, the freeze-dried ovine tendon was immersed in 0.35 M sterilized acetic acid (Merck, Darmstadt, Germany) for 72 h to dissolve the collagen protein and remove any impurities. The swollen tendons were blended with similar sterilized acetic acid to produce a homogeneous solution at a chilling temperature of 4–8 °C. Then, the blended solution was centrifuged at 5488×
g at 4 °C for 10 min. The supernatant was collected and precipitated, using sodium chloride (Sigma-Aldrich, St. Louis, MO, USA) overnight prior to dialyzing for 72 h. Next, the collagen was pre-frozen at −80 °C for 6 h and lyophilized to obtain the dried collagen flakes for a final working solution preparation (re-dissolved in 0.35 M sterile acetic acid).
2.2. Fabrication of Collagen–Gelatin–Elastin Biomaterials
The mixture of 1.425% (w/v) collagen stock and 0.7% (w/v) gelatin solution was stirred gently at two different ratios, of 4 mL:1 mL and 4.5 mL:0.5 mL, for 5 min. Then, 5 mg and 10 mg of elastin powder were added to the 4:1 and 4.5:0.5 ratios, respectively, and gently mixed for 10 min using a stirrer. The mixed solutions were poured into the desired mold and frozen at −80 °C for 6 h followed by freeze-drying for 24–48 h at −56 °C and 5 mTorr of atmospheric pressure. Then, the freeze-dried biomaterials were cross-linked with 0.1% (w/v) genipin (Fujifilm Wako Pure Chemical Corporation, Shibukawa, Japan) (GNP). Briefly, the GNP solution (0.1% w/v) was made by mixing crystallized GNP powder in 70% ethanol (EtOH; MERCK, Darmstadt, Germany) at room temperature (22–24 °C). The CollaGee biomaterials were then immersed in 0.1% (w/v) GNP at room temperature for 6 h followed by washing, using Dulbecco’s Phosphate Buffered Saline (DPBS) (Sigma-Aldrich, St. Louis, MO, USA) three times to obtain 415_GNP and 4510_GNP formulations of GNP-cross-linked CollaGee biomaterials. Non-cross-linked biomaterials for each corresponding ratio were used as control, namely, 415_NC and 4510_NC. The cross-linked CollaGee biomaterials were then freeze-dried for 24–48 h for further analysis.
2.3. Gross Appearance and Resilience
The gross appearance of the fabricated CollaGee biomaterials was captured using a digital camera (Nikon, Tokyo, Japan). The resilience was determined by placing 300 g of weight on the wet biomaterials for 10 min. Then, the biomaterials were immersed in distilled water for 2 min. The thickness areas of the pre-compression and post-rehydration were documented. The images were analyzed using Image J software (Version 1.53; National Institutes of Health, Bethesda, MD, USA). Resilience experiments were performed in triplicate. The resilience was experimentally determined using the following formula:
where Ab is the thickness area before compression and Ar is the thickness area after rehydration.
2.4. In Vitro Biodegradation
The biodegradability of the CollaGee biomaterials was evaluated by incubating each sample in 0.0006% (
w/
v) collagenase type I (Worthington, Columbus, OH, USA) prepared in phosphate buffered saline (PBS) (Sigma-Aldrich, St. Louis, MO, USA). The initial weight of the biomaterials (Wi) was recorded accordingly, and the biomaterials were placed in the incubator at a temperature of 37 °C. Every 24 h, the biomaterials were washed with PBS and freeze-dried for 12–24 h. Experiments were performed in triplicate. The remaining biomaterials were weighed (Wf) and the weight loss (%) was calculated by using the following formula:
where Wi is the initial weight, Wf is the final weight, and t is the time.
2.5. Swelling Testing
The swelling ratio analysis was performed by rehydrating the biomaterials at 37 °C in DPBS for 1 h. Before rehydration, the biomaterials were weighed in a dry form. Experiments were performed in triplicate. The swelling ratio was calculated as follows:
where Ws is the swollen weight and Wd is the dry weight.
2.6. Cross-Linking Degree Analysis
A ninhydrin assay was used to determine the degree of cross-linking. A 10 mg sample for each group was soaked in 200 µL of a 10× ninhydrin 2% (Sigma-Aldrich, St. Louis, MO, USA) working solution and boiled for 2 min at 100 °C. After cooling down, 200 µL of 95% ethanol was added to the solution. The absorbance was read at 570 nm. Experiments were performed in triplicate. The cross-linking degree was calculated as follows:
where Anc is the absorbance of the non-cross-linked and Ac is the absorbance of the cross-linked.
2.7. 3D Microstructural Analysis
The morphological evaluation was performed on the surface and cross section of the CollaGee biomaterials. A field emission scanning electron microscope (FESEM), operated at 15 kV, was used to observe the cross-section microstructure of the CollaGee biomaterials. The pore size distribution was measured using Image J software (Version 1.53; National Institutes of Health, Bethesda, MD, USA). The porosity was evaluated by measuring the weight difference between pre- and post-submersion in 99.5% ethanol for 18 h. Porosity experiments were performed in triplicate. The porosity was calculated using the following equation:
where Ws is the submerged weight, Wd is the dry weight, ρ is the density of 99.5% ethanol, and V is the volume of the biomaterial.
2.8. Chemical Characterization
The chemical characterization of the CollaGee biomaterials was performed using Fourier-transform infrared spectroscopy (FTIR). The CollaGee biomaterials (1 mm3) were analyzed, and the spectral data were recorded by a PE spectrum 100 FTIR spectrometer (PE, Waltham, MA, USA) at a wavelength range of 700 to 4000 cm−1. The absorbance peaks were analyzed to identify the chemical structure and chemical changes due to cross-linking process. The chemical composition of the CollaGee biomaterials was analyzed using energy-dispersive X-ray (EDX) to identify elements within the fabricated CollaGee and to provide quantitative information. The crystallographic structure analysis of the fabricated CollaGee biomaterials was performed by X-ray diffraction (XRD).
2.9. Thermal Stability
The denaturation temperatures of the CollaGee biomaterials were determined by differential scanning calorimetry (DSC) under a nitrogen atmosphere at a heating rate of 10 °C/minute up to 120 °C. In contrast, thermogravimetric analysis (TGA) of the CollaGee biomaterials was performed at a heating rate of 10 °C/minute under a nitrogen atmosphere of 35 °C to 800 °C.
2.10. Mechanical Testing
The mechanical strength of the CollaGee biomaterials was measured in a dry condition at room temperature. The instrument was fitted with 50 N of load transducer at a crosshead velocity of 0.05 mm/minute. Experiments were performed in triplicate.
2.11. Isolation and Culture of Human Dermal Fibroblasts
HDFs were obtained as redundant tissue from six consenting patients and processed as previously described by Fauzi et al. [
33]. Briefly, 3 cm
2 of skin samples were cleaned, minced, and digested via a dual-enzymatic process using 0.6% collagenase (Worthington, Columbus, OH, USA) type I at 37 °C for 4–6 h followed by treatment with trypsin-EDTA (Sigma-Aldrich, St. Louis, MO, USA) for 10 min. The cell suspension was then centrifuged and resuspended with a co-culture medium containing an equivalent amount of Epilife (Gibco, Waltham, MA, USA) supplemented with 5% fetal bovine serum (FBS) (Sigma-Aldrich, St. Louis, MO, USA) and F12: DMEM (Gibco, Waltham, MA, USA) containing 10% FBS. The skin cell suspensions containing human epidermal keratinocytes (HEK) and HDFs were seeded in a polystyrene culture plate and placed at 37 °C in an incubator supplied with 5% CO
2. The medium was changed three times per week. HDFs were dissociated by differential trypsinization after the cell had achieved 70–80% confluency. HDFs were cultured in a 75 cm
2 T-flask with F12: DMEM containing 10% FBS.
2.12. Cell Toxicity Assessment of CollaGee Biomaterials
The LIVE/DEAD® Cell Viability Assay (Invitrogen, Waltham, MA, USA) was used to analyze the cytotoxic effect of the CollaGee biomaterials according to the manufacturer’s protocol. Briefly, HDFs were cultured on the CollaGee biomaterials for 24 h, incubated with 2 mM calcein AM and 4 mM EthD-1 in DPBS for 30 min, and washed with DPBS. Subsequently, observation of the cultures was performed using a Nikon A1R-A1 confocal laser scanning microscopy. The live cells were stained with green colors while the dead cells were stained with a red color. The morphological features of the cells on the CollaGee biomaterials were observed using a scanning electron microscope (SEM).
2.13. Cell Viability and Attachment Evaluation
The most reliable method in determining the cell viability of HDFs is by using 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) (Invitrogen, Waltham, MA, USA) staining based on the color changes of tetrazolium yellow powder into insoluble, dark-purple crystals of formazan. This occurrence happens only in living cells where succinate dehydrogenase enzymes are present in their mitochondria [
34]. Formazan crystal was then disintegrated in organic solvents such as DMSO and its absorbance was recorded by a spectrophotometer. The resulting absorbance value corresponded to the formazan concentration, which corresponded to the number of living cells.
This test was performed in a direct method. For this purpose, the CollaGee bioscaffolds were firstly sterilized using sterile 70% ethanol. A total of 2 × 10
4 of HDFs was seeded on the top of the CollaGee bioscaffolds in 24-well plates and incubated for 1, 3, and 7 days. The cell-seeded bioscaffolds were cultured and incubated at 37 °C under a 5% CO
2 atmosphere to allow the attachment of the cells to the bioscaffolds. Then, 200 µL of F12: DMEM (Gibco, USA) containing 10% FBS (Sigma-Aldrich, St. Louis, MO, USA) was added to each well and treated for 1, 3, and 7 days. Next, 300 µL of F12: DMEM and 30 µL of MTT reagent (5 mg/mL in PBS) (Sigma-Aldrich, St. Louis, MO, USA) were added to each sample followed by incubation at 37 °C for 4 h for MTT formazan formation. Negative controls were made by adding 300 µL of F12: DMEM to 30 µL of MTT solution without the presence of cells. Then, 225 µL of the medium was discarded from each well by using a micropipette. A total of 100 µL of DMSO (Sigma-Aldrich, St. Louis, MO, USA) was added to each well to dissolve the formazan crystals. The absorbance was measured at 540 nm using a microplate reader (Power Wave XS; Bio-TEK Instruments, Winooski, VT, USA). The percentage of viability was determined using the following equation:
where At is absorbance treated and Au is absorbance untreated.
The cell attachment assay of HDFs was determined by Trypan blue dye exclusion assay. Briefly, HDFs were cultured directly on the CollaGee bioscaffolds and incubated for 24 h. The cultured media were centrifuged for 5 min at 500 rpm (Hettich Zentrifugen, Föhrenstraße, Tuttlingen, Germany). The supernatant was discarded, and the pellet was resuspended in 5 mL of DPBS (Sigma-Aldrich, St. Louis, MO, USA). A viable cell count was carried out on unattached cells by mixing 20 µL of cell suspension with 20 µL of Trypan blue (Sigma-Aldrich, St. Louis, MO, USA) and counting in a hemocytometer (Optik Labor, 0.100 mm, Görlitz, Germany) using a light microscope (Olympus CK40, Tokyo, Japan). Only those cells that were in the four zones of the hemocytometer were counted. Both experiments were performed in triplicate. The percentage of cell attachment was determined using the following equation:
where Ni is the number of initial cells seeding and Nd is the number of cells in DPBS.
2.14. Statistical Analysis
Statistical analysis was performed using GraphPad Prism (Version 5.0; GraphPad Software Inc., San Diego, CA, USA). For multiple groups’ comparison, a two-way variance analysis was used. Statistical significance was set at p < 0.05.
4. Discussion
The limitations of certain currently available collagen products on the market are primarily due to the high risk of infection such as bovine spongiform encephalopathy (mad cow disease) and religious constraints such as with porcine products. Therefore, exploring alternative collagen type I (Col-I) sources such as sheep is currently being established and scrutinized. Col-I from ovine tendon can be extracted via salt precipitation, acid-based digestion, or enzymatic isolation using a neutral saline solution or acidic solution such as acetic acid, hydrochloric acid, and acid–enzyme mixtures such as pepsin with acetic acid [
32]. The selection of extraction methods depends on the material solubility to produce a high yield of purified Col-I. A low concentration of acetic acid as a green chemical footprint approach is favorable in extracting Col-I from mammals and non-mammals. Acetic acid cleaves the cross-link in collagen and solubilizes the unbound collagen. Meanwhile, a salt solution of sodium chloride (NaCl) is used to precipitate collagen from an acidic solution prior to dialysis [
24,
32].
The key determining factors to develop the functional biomaterial are the microporous structure, good mechanical strength, biodegradation rate, and biocompatibility [
35]. In addition, the porosity of the biomaterial is an essential aspect to evaluate the performance of skin tissue engineering development. Skin biomaterial must be highly porous to transport nutrients and remove wound exudates, hence facilitating cell proliferation and vascularization. Pore sizes between 100 and 300 µm are recommended for cell migration, extensive vascularization, and tissue regeneration [
35,
36]. Therefore, developing an acellular skin substitute (ASS) for future skin wound-healing treatment is crucial to cater to the need for ready-to-use products for clinicians and surgeons. The abovementioned factors should comply with any natural-based materials’ development for an ideal ASS or wound dressing. In addition, to prolong the sustainability of a cutaneous biomaterial via a freeze-drying/lyophilization approach and/or cross-linking agents, chemicals and irradiation could reduce the risk of commercial loss in the future. The biomaterials’ hybridization approach may affect the native performance of each material; therefore, physicochemical, mechanical, and cellular compatibility assessments are required to validate its behavior.
Lyophilization technology is a well-established and straightforward method to produce porous microstructures, often in sponge-like 3D structures. This process involves the sublimation step to allow the slow removal of the solvent used inside the polymer mixture via lyophilization under high vacuum conditions. This versatile technology enables controlling the mechanical strength, pore size and distribution, porosity, and pore interconnectivity by modifying the polymer concentration and freeze-drying parameters [
24]. A previous study comparing different drying methods including oven drying, room temperature drying, and freeze-drying revealed the importance of freeze-drying in forming a porous biomaterial. In this study, freeze-dried CollaGee biomaterials achieved optimum pore sizes around 100–200 µm (
Figure 1b) and >50% (
Figure 1c) porosity, which is capable of supporting cell migration to accelerate wound healing. However, oven and room temperature drying could not form porous structures, despite their superior drying rate and tensile strength [
37]. Thus, the freeze-drying approach is still eligible for fabricating a functionalized porous biomaterial for tissue-engineering applications [
38].
The findings revealed that the fabrication of a 3D sponge biomaterial using collagen–gelatin–elastin cross-linked with GNP provides good architecture and physical and mechanical properties and demonstrated no toxicity toward HDFs. As no significant agglomeration of particles was observed on FESEM (
Figure 1b), pre-mixing fabrication using a magnetic stirrer (300–450 rpm) presented a good dispersion of biomaterials, with no sedimentation processes occurring during the preparation stage prior to the freeze-drying step. It was further confirmed by EDX analysis, whereby element distribution was homogeneous on different planes (
Figure 3b). This confirmed a proper fabrication technique. Furthermore, the XRD’s peaks’ analysis, to determine the crystallography of the fabricated biomaterial and CollaGee, confirmed their amorphous phase resembling native collagen, gelatin, and elastin properties (
Figure 3c). Thus, the current pre-mixing fabrication method was proven successful in conserving its original characteristics.
The CollaGee biomaterials generally have poor mechanical strength (
Figure 2e); hence, it is necessary to confer structural stability of the biomaterial by introducing exogenous cross-linking agents. This study used natural GNP to cross-link the CollaGee biomaterials due to a more negligible toxic effect on human skin cells. It showed that cross-linked CollaGee presented a higher mechanical strength compared to NC CollaGee (
Figure 2e). Fauzi et al. demonstrated a high mechanical strength through GNP cross-linking without affecting the degree of porosity [
35]. GNP can form intramolecular and intermolecular cross-linking networks with collagen involving amino acid residues such as lysine, hydroxylysine, and arginine [
33]. The cross-linking mechanism for the GNP–amino group monomer was formed through a nucleophilic attack by the amino group-containing compounds on the third carbon of GNP. Subsequently, the resulting aldehyde group was attacked by the attached secondary amino group. Dimerization occurred at the second stage, probably through radical reaction. Therefore, GNP may form intramolecular and intermolecular cross-linked products with a heterocyclic structure [
24,
32].
Resilience is the ability of a biomaterial to rehydrate into its original form after being loaded with weight. The findings proved that the elasticity and macroporous nature of the biomaterial (
Figure 2a) allowed water to freely flow in and out, thereby facilitating cell migration to the wound sites [
39]. Additionally, the swelling capacity of a biomaterial is an important aspect to evaluate the performance of cutaneous tissue engineering. A higher swelling capacity will facilitate wound healing as better diffusion of signaling molecules and nutrients will accelerate cell proliferation [
40]. The 415_GNP had a significantly higher swelling capacity compared to 4510_GNP (
Figure 2c), which could have been due to a higher percentage of gelatin in 4510_GNP that acted as a water-retaining agent. These data are consistent with a previous study performed by Chloe et al. (2012), in which a collagen–gelatin scaffold had more fluid uptake than biomaterial without gelatin [
41]. These results demonstrated that GNP is a favorable cross-linking agent for the CollaGee biomaterials since it can efficiently cross-link the amino groups even at a low concentration (0.1%
w/
v).
In vitro biodegradation rates were experimented with, using 0.0006% collagenase type I because it resembles the skin microenvironment. Cross-linking with GNP led to the reduction in free amino groups in the hydrolyzed collagen; hence, it may be accountable for a slower degradation rate than the non-cross-linked biomaterials (
Figure 2b) [
35,
42]. This trend may be helpful for skin regeneration in the wound-healing process because faster degradation will lead to a loss of scaffold before a new matrix structure is developed.
Thermal stability, an important feature of biomaterials, means the long-term usability and stability of a biomaterial in extreme environments. The long-term application of regenerative biomaterials at body temperature can lead to damage if the material is thermally unstable [
43]. The endothermic peak is the result of a change of structure to a random coil due to the thermal disruption of hydrogen bonds [
44]. Consistent with Miles et al., cross-linked groups are more thermally stable than the non-cross-linked groups (
Table 1) [
45]. The non-cross-linked groups have larger enthalpy than the cross-linked groups due to the presence of non-cross-linked collagen triple helices. An increase in the elastin did not affect the endothermic peak of the biomaterial [
46]. Cross-linked CollaGee biomaterials showed water loss at a lower heating temperature, which is consistent with a study performed by Shah et al. [
47]. In the first stage, 6 ± 1% of weight loss was observed as structurally bonded water was removed, while a maximum weight loss was seen in the second stage, probably due to chain cleavage of the organic components [
48]. The structural characteristic of the collagen family is the right-handed triple helix of three polypeptide chains [
24]. A weight loss before 400 °C is commonly due to complex processes such as the dehydration of the polysaccharide rings with the vaporization and removal of volatile products [
46]. In the final stage, weight loss was noted to decrease slowly, and a weight loss of only up to 7% was measured (
Figure 4). It could be concluded that the water content and thermal stability of the polymers were greatly influenced by the cross-linking degree and intermolecular chain interaction.
An ideal biomaterial for wound healing should support cell viability and migration inside the biomaterial to proliferate and regenerate new tissue [
41,
46]. In this study, cross-linking with GNP improved the mechanical strength of the biomaterial with negligible cytotoxic effects toward HDFs (
Figure 5a–d), which is consistent with previous studies [
35,
49]. A healthy condition of the HDFs via SEM was characterized by various-shape morphologies with a temporary projection of pseudopodia and excreted matrices (whitish granules) present in the surrounding attached HDFs. Cell attachment of more than 80% and viability of more than 60% proved the non-cytotoxicity of the CollaGee bioscaffolds and a good attachment surface of the HDFs (
Figure 5c,d). In addition, an important similarity between collagen and gelatin is the lack or deficient presence of the aromatic amino acids, tryptophan, tyrosine, and phenylalanine. The lack of these amino acids is one of the major contributing factors to the low antigenicity and toxicity of both gelatin and collagen [
27]. In addition, the blending of elastin with collagen and gelatin was proven to promote fibroblast proliferation in vitro [
3].