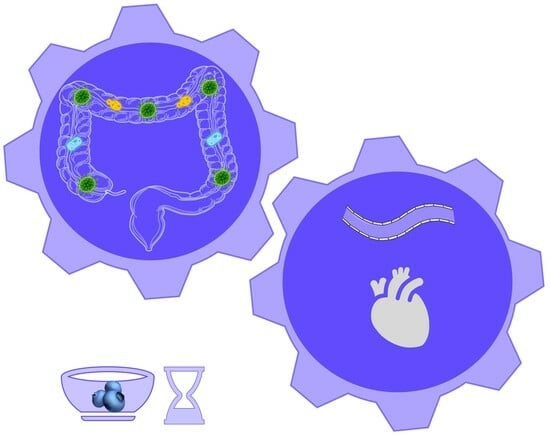
Dose- and Time-Dependent Effect of Dietary Blueberries on Diabetic Vasculature Is Correlated with Gut Microbial Signature
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Experimental Animals
2.3. Standard-Diet- and Blueberry-Supplemented Diets
2.4. Experimental Design
2.5. Measurement of Metabolic Variables and Collection of Tissue Samples
2.6. Measurement of Vascular Inflammation
2.7. Microbial Profiling Using 16S rRNA Amplicon Sequencing
2.8. Bioinformatics Analysis
2.9. Statistical Analysis
3. Results
3.1. Dietary Blueberries Did Not Improve Diabetes-Induced Metabolic Alterations
3.2. Dietary Blueberries Exhibit a Dose-Dependent Ability to Suppress Diabetes-Induced Vascular Inflammation
3.3. Dietary Blueberries Dose- and Time-Dependently Improve Diabetes-Induced Gut Dysbiosis
3.4. Association between Gut Microbial Signature and Vascular Inflammation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Raghavan, S.; Vassy, J.L.; Ho, Y.L.; Song, R.J.; Gagnon, D.R.; Cho, K.; Wilson, P.W.F.; Phillips, L.S. Diabetes Mellitus-Related All-Cause and Cardiovascular Mortality in a National Cohort of Adults. J. Am. Heart Assoc. 2019, 8, e011295. [Google Scholar] [CrossRef] [Green Version]
- Petersen, C.; Bharat, D.; Wankhade, U.D.; Kim, J.S.; Cutler, B.R.; Denetso, C.; Gholami, S.; Nelson, S.; Bigley, J.; Johnson, A.; et al. Dietary Blueberry Ameliorates Vascular Complications in Diabetic Mice Possibly through NOX4 and Modulates Composition and Functional Diversity of Gut Microbes. Mol. Nutr. Food Res. 2022, 66, 2100784. [Google Scholar] [CrossRef] [PubMed]
- Cutler, B.R.; Petersen, C.; Anandh Babu, P.V. Mechanistic insights into the vascular effects of blueberries: Evidence from recent studies. Mol. Nutr. Food Res. 2017, 61, 1600271. [Google Scholar] [CrossRef] [PubMed]
- Bharat, D.; Cavalcanti, R.R.M.; Petersen, C.; Begaye, N.; Cutler, B.R.; Costa, M.M.A.; Ramos, R.; Ferreira, M.R.; Li, Y.; Bharath, L.P.; et al. Blueberry Metabolites Attenuate Lipotoxicity-Induced Endothelial Dysfunction. Mol. Nutr. Food Res. 2018, 62, 1700601. [Google Scholar] [CrossRef]
- Rodriguez-Mateos, A.; Rendeiro, C.; Bergillos-Meca, T.; Tabatabaee, S.; George, T.W.; Heiss, C.; Spencer, J.P. Intake and time dependence of blueberry flavonoid-induced improvements in vascular function: A randomized, controlled, double-blind, crossover intervention study with mechanistic insights into biological activity. Am. J. Clin. Nutr. 2013, 98, 1179–1191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cassidy, A.; Mukamal, K.J.; Liu, L.; Franz, M.; Eliassen, A.H.; Rimm, E.B. High anthocyanin intake is associated with a reduced risk of myocardial infarction in young and middle-aged women. Circulation 2013, 127, 188–196. [Google Scholar] [CrossRef] [Green Version]
- Basu, A.; Du, M.; Leyva, M.J.; Sanchez, K.; Betts, N.M.; Wu, M.; Aston, C.E.; Lyons, T.J. Blueberries decrease cardiovascular risk factors in obese men and women with metabolic syndrome. J. Nutr. 2010, 140, 1582–1587. [Google Scholar] [CrossRef] [Green Version]
- Hou, K.; Wu, Z.X.; Chen, X.Y.; Wang, J.Q.; Zhang, D.; Xiao, C.; Zhu, D.; Koya, J.B.; Wei, L.; Li, J.; et al. Microbiota in health and diseases. Signal Transduct. Target. Ther. 2022, 7, 135. [Google Scholar] [CrossRef]
- Thursby, E.; Juge, N. Introduction to the human gut microbiota. Biochem. J. 2017, 474, 1823–1836. [Google Scholar] [CrossRef]
- Singh, R.K.; Chang, H.W.; Yan, D.; Lee, K.M.; Ucmak, D.; Wong, K.; Abrouk, M.; Farahnik, B.; Nakamura, M.; Zhu, T.H.; et al. Influence of diet on the gut microbiome and implications for human health. J. Transl. Med. 2017, 15, 73. [Google Scholar] [CrossRef] [Green Version]
- Garcia-Rios, A.; Torres-Pena, J.D.; Perez-Jimenez, F.; Perez-Martinez, P. Gut Microbiota: A New Marker of Cardiovascular Disease. Curr. Pharm. Des. 2017, 23, 3233–3238. [Google Scholar] [CrossRef]
- Olofsson, L.E.; Backhed, F. The Metabolic Role and Therapeutic Potential of the Microbiome. Endocr. Rev. 2022, 43, 907–926. [Google Scholar] [CrossRef] [PubMed]
- Petersen, C.; Bharat, D.; Cutler, B.R.; Gholami, S.; Denetso, C.; Mueller, J.E.; Cho, J.M.; Kim, J.S.; Symons, J.D.; Anandh Babu, P.V. Circulating metabolites of strawberry mediate reductions in vascular inflammation and endothelial dysfunction in db/db mice. Int. J. Cardiol. 2018, 263, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.C.; Babu, A.K.S.; Petersen, C.; Wankhade, U.D.; Robeson, M.S.; Putich, M.N.; Mueller, J.E.; O’Farrell, A.S.; Cho, J.M.; Chintapalli, S.V.; et al. Gut Microbes Are Associated with the Vascular Beneficial Effects of Dietary Strawberry on Metabolic Syndrome-Induced Vascular Inflammation. Mol. Nutr. Food Res. 2022, 66, 2200112. [Google Scholar] [CrossRef] [PubMed]
- Kozich, J.J.; Westcott, S.L.; Baxter, N.T.; Highlander, S.K.; Schloss, P.D. Development of a dual-index sequencing strategy and curation pipeline for analyzing amplicon sequence data on the MiSeq Illumina sequencing platform. Appl. Environ. Microbiol. 2013, 79, 5112–5120. [Google Scholar] [CrossRef] [Green Version]
- Bolyen, E.; Rideout, J.R.; Dillon, M.R.; Bokulich, N.A.; Abnet, C.C.; Al-Ghalith, G.A.; Alexander, H.; Alm, E.J.; Arumugam, M.; Asnicar, F.; et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat. Biotechnol. 2019, 37, 852–857. [Google Scholar] [CrossRef]
- Amir, A.; McDonald, D.; Navas-Molina, J.A.; Kopylova, E.; Morton, J.T.; Zech Xu, Z.; Kightley, E.P.; Thompson, L.R.; Hyde, E.R.; Gonzalez, A.; et al. Deblur Rapidly Resolves Single-Nucleotide Community Sequence Patterns. mSystems 2017, 2, e00191-16. [Google Scholar] [CrossRef] [Green Version]
- Bokulich, N.A.; Subramanian, S.; Faith, J.J.; Gevers, D.; Gordon, J.I.; Knight, R.; Mills, D.A.; Caporaso, J.G. Quality-filtering vastly improves diversity estimates from Illumina amplicon sequencing. Nat. Methods 2013, 10, 57–59. [Google Scholar] [CrossRef]
- Price, M.N.; Dehal, P.S.; Arkin, A.P. FastTree 2—Approximately maximum-likelihood trees for large alignments. PLoS ONE 2010, 5, e9490. [Google Scholar] [CrossRef]
- McDonald, D.; Price, M.N.; Goodrich, J.; Nawrocki, E.P.; DeSantis, T.Z.; Probst, A.; Andersen, G.L.; Knight, R.; Hugenholtz, P. An improved Greengenes taxonomy with explicit ranks for ecological and evolutionary analyses of bacteria and archaea. ISME J. 2012, 6, 610–618. [Google Scholar] [CrossRef]
- Lozupone, C.; Lladser, M.E.; Knights, D.; Stombaugh, J.; Knight, R. UniFrac: An effective distance metric for microbial community comparison. ISME J. 2011, 5, 169–172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mokhtari, P.; Jambal, P.; Metos, J.M.; Shankar, K.; Anandh Babu, P.V. Microbial taxonomic and functional shifts in adolescents with type 1 diabetes are associated with clinical and dietary factors. EBioMedicine 2023, 93, 104641. [Google Scholar] [CrossRef] [PubMed]
- Cutler, B.; Gholami, S.; Chua, J.S.; Kuberan, B.; Anandh Babu, P.V. Blueberry metabolites restore cell surface glycosaminoglycans and attenuate endothelial inflammation in diabetic human aortic endothelial cells. Int. J. Cardiol. 2018, 261, 155–158. [Google Scholar] [CrossRef] [PubMed]
- Ivey, K.L.; Chan, A.T.; Izard, J.; Cassidy, A.; Rogers, G.B.; Rimm, E.B. Role of Dietary Flavonoid Compounds in Driving Patterns of Microbial Community Assembly. mBio 2019, 10, e01205-19. [Google Scholar] [CrossRef] [Green Version]
- Arumugam, M.; Raes, J.; Pelletier, E.; Le Paslier, D.; Yamada, T.; Mende, D.R.; Fernandes, G.R.; Tap, J.; Bruls, T.; Batto, J.M.; et al. Enterotypes of the human gut microbiome. Nature 2011, 473, 174–180. [Google Scholar] [CrossRef] [Green Version]
- Binda, C.; Lopetuso, L.R.; Rizzatti, G.; Gibiino, G.; Cennamo, V.; Gasbarrini, A. Actinobacteria: A relevant minority for the maintenance of gut homeostasis. Dig. Liver Dis. 2018, 50, 421–428. [Google Scholar] [CrossRef]
- Ahmadmehrabi, S.; Tang, W.H.W. Gut microbiome and its role in cardiovascular diseases. Curr. Opin. Cardiol. 2017, 32, 761–766. [Google Scholar] [CrossRef] [Green Version]
- Lakshmanan, A.P.; Murugesan, S.; Al Khodor, S.; Terranegra, A. The potential impact of a probiotic: Akkermansia muciniphila in the regulation of blood pressure-the current facts and evidence. J. Transl. Med. 2022, 20, 430. [Google Scholar] [CrossRef]
- Sun, B.; Ma, T.; Li, Y.; Yang, N.; Li, B.; Zhou, X.; Guo, S.; Zhang, S.; Kwok, L.Y.; Sun, Z.; et al. Bifidobacterium lactis Probio-M8 Adjuvant Treatment Confers Added Benefits to Patients with Coronary Artery Disease via Target Modulation of the Gut-Heart/-Brain Axes. mSystems 2022, 7, e0010022. [Google Scholar] [CrossRef]
- Zhao, S.; Liu, W.; Wang, J.; Shi, J.; Sun, Y.; Wang, W.; Ning, G.; Liu, R.; Hong, J. Akkermansia muciniphila improves metabolic profiles by reducing inflammation in chow diet-fed mice. J. Mol. Endocrinol. 2017, 58, 1–14. [Google Scholar] [CrossRef]
- Zhang, T.; Li, Q.; Cheng, L.; Buch, H.; Zhang, F. Akkermansia muciniphila is a promising probiotic. Microb. Biotechnol. 2019, 12, 1109–1125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vendrame, S.; Guglielmetti, S.; Riso, P.; Arioli, S.; Klimis-Zacas, D.; Porrini, M. Six-week consumption of a wild blueberry powder drink increases bifidobacteria in the human gut. J. Agric. Food Chem. 2011, 59, 12815–12820. [Google Scholar] [CrossRef] [PubMed]
- Lu, G.; Zhang, Y.; Ren, Y.; Shi, J.S.; Xu, Z.H.; Geng, Y. Diversity and Comparison of Intestinal Desulfovibrio in Patients with Liver Cirrhosis and Healthy People. Microorganisms 2023, 11, 276. [Google Scholar] [CrossRef]
- Qin, J.; Li, Y.; Cai, Z.; Li, S.; Zhu, J.; Zhang, F.; Liang, S.; Zhang, W.; Guan, Y.; Shen, D.; et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 2012, 490, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Qin, X.; Qiu, J.; Sun, T.; Qu, K.; Din, A.U.; Yan, W.; Li, T.; Chen, Y.; Gu, W.; et al. Desulfovibrio desulfuricans aggravates atherosclerosis by enhancing intestinal permeability and endothelial TLR4/NF-kappaB pathway in Apoe (−/−) mice. Genes Dis. 2023, 10, 239–253. [Google Scholar] [CrossRef]
- Mattana, M.; Tomasello, R.; Cammarata, C.; Di Carlo, P.; Fasciana, T.; Giordano, G.; Lucchesi, A.; Siragusa, S.; Napolitano, M. Clostridium difficile Induced Inflammasome Activation and Coagulation Derangements. Microorganisms 2022, 10, 1624. [Google Scholar] [CrossRef]






| Experimental Mice | Diet | Blueberry Dosage (Human Equivalent) | Duration of Treatment | ||
|---|---|---|---|---|---|
| 4 Weeks | 8 Weeks | 12 Weeks | |||
| db/+ mice (C) | Standard Diet | C4 | C8 | C12 | |
| db/db mice (D) | Standard Diet | D4 | D8 | D12 | |
| db/db mice (D) | 1.27% Freeze-dried blueberry powder supplemented Diet (B1) | ½ cup (80 g) | D4B1 | D8B1 | D12B1 |
| db/db mice (D) | 2.46% Freeze-dried blueberry powder supplemented Diet (B2) | 1 cup (160 g) | D4B2 | D8B2 | D12B2 |
| db/db mice (D) | 3.7% Freeze-dried blueberry powder supplemented Diet (B3) | 1.5 cup (240 g) | D4B3 | D8B3 | D12B3 |
| 4 Weeks | C4 | D4 | D4B1 | D4B2 | D4B3 |
| Body weight (g) | 28.3 ± 0.41 | 44.5 ± 0.56 * | 43.9 ± 0.47 | 43.6 ± 0.47 | 44.1 ± 0.20 |
| Blood glucose (Fasting) | 53.9 ± 4.37 | 188.4 ± 13.37 * | 186.5 ± 23.26 | 152.5 ± 10.95 | 152.3 ± 10.24 |
| Blood glucose (non-fasting) | 179.6 ± 8.82 | 472.1 ± 22.52 * | 537.9 ± 23.88 | 564.4 ± 16.17 | 568.4 ± 15.13 |
| Body fat (%) | 20.5 ± 1.1 | 68.3 ± 087 * | 68.6 ± 0.58 | 67.3 ± 0.67 | 67.3 ± 0.51 |
| Lean body mass (%) | 67.3 ± 0.59 | 40.4 ± 0.39 * | 40.2 ± 0.34 | 40.3 ± 0.42 | 40.4 ± 0.29 |
| Fluid (%) | 12.9 ± 0.2 | 8.3 ± 0.17 * | 8.5 ± 0.15 | 9 ± 0.17 | 8.9 ± 0.16 |
| 8 Weeks | C8 | D8 | D8B1 | D8B2 | D8B3 |
| Body weight (g) | 28.3 ± 0.41 | 44.5 ± 0.56 * | 43.9 ± 0.47 | 43.6 ± 0.47 | 44.1 ± 0.20 |
| Blood glucose (Fasting) | 53.9 ± 4.37 | 188.4 ± 13.37 * | 186.5 ± 23.26 | 152.5 ± 10.95 | 152.3 ± 10.24 |
| Blood glucose (non-fasting) | 179.6 ± 8.82 | 472.1 ± 22.52 * | 537.9 ± 23.88 | 564.4 ± 16.17 | 568.4 ± 15.13 |
| Body fat (%) | 20.5 ± 1.1 | 68.3 ± 087 * | 68.6 ± 0.58 | 67.3 ± 0.67 | 67.3 ± 0.51 |
| Lean body mass (%) | 67.3 ± 0.59 | 40.4 ± 0.39 * | 40.2 ± 0.34 | 40.3 ± 0.42 | 40.4 ± 0.29 |
| Fluid (%) | 12.9 ± 0.2 | 8.3 ± 0.17 * | 8.5 ± 0.15 | 9 ± 0.17 | 8.9 ± 0.16 |
| 12 Weeks | C12 | D12 | D12B1 | D12B2 | D12B3 |
| Body weight (g) | 28.3 ± 0.41 | 44.5 ± 0.56 * | 43.9 ± 0.47 | 43.6 ± 0.47 | 44.1 ± 0.20 |
| Blood glucose (Fasting) | 53.9 ± 4.37 | 188.4 ± 13.37 * | 186.5 ± 23.26 | 152.5 ± 10.95 | 152.3 ± 10.24 |
| Blood glucose (non-fasting) | 179.6 ± 8.82 | 472.1 ± 22.52 * | 537.9 ± 23.88 | 564.4 ± 16.17 | 568.4 ± 15.13 |
| Body fat (%) | 20.5 ± 1.1 | 68.3 ± 087 * | 68.6 ± 0.58 | 67.3 ± 0.67 | 67.3 ± 0.51 |
| Lean body mass (%) | 67.3 ± 0.59 | 40.4 ± 0.39 * | 40.2 ± 0.34 | 40.3 ± 0.42 | 40.4 ± 0.29 |
| Fluid (%) | 12.9 ± 0.2 | 8.3 ± 0.17 * | 8.5 ± 0.15 | 9 ± 0.17 | 8.9 ± 0.16 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Satheesh Babu, A.K.; Petersen, C.; Paz, H.A.; Benedict, K.; Nguyen, M.; Putich, M.; Saldivar-Gonzalez, M.; Zhong, Y.; Larsen, S.; Wankhade, U.D.; et al. Dose- and Time-Dependent Effect of Dietary Blueberries on Diabetic Vasculature Is Correlated with Gut Microbial Signature. Antioxidants 2023, 12, 1527. https://doi.org/10.3390/antiox12081527
Satheesh Babu AK, Petersen C, Paz HA, Benedict K, Nguyen M, Putich M, Saldivar-Gonzalez M, Zhong Y, Larsen S, Wankhade UD, et al. Dose- and Time-Dependent Effect of Dietary Blueberries on Diabetic Vasculature Is Correlated with Gut Microbial Signature. Antioxidants. 2023; 12(8):1527. https://doi.org/10.3390/antiox12081527
Chicago/Turabian StyleSatheesh Babu, Adhini Kuppuswamy, Chrissa Petersen, Henry A. Paz, Kai Benedict, Miley Nguyen, Madison Putich, Miguel Saldivar-Gonzalez, Ying Zhong, Sydney Larsen, Umesh D. Wankhade, and et al. 2023. "Dose- and Time-Dependent Effect of Dietary Blueberries on Diabetic Vasculature Is Correlated with Gut Microbial Signature" Antioxidants 12, no. 8: 1527. https://doi.org/10.3390/antiox12081527