Comparison of one-stage treatment versus two-stage treatment for the management of patients with common bile duct stones: A meta-analysis
- 1Department of Hepatobiliary Surgery, Luzhou people's Hospital, Luzhou, China
- 2Department of Anesthesiology, Luzhou people's Hospital, Luzhou, China
Background: Cholelithiasis is a frequently occurring disease in clinic. Due to changes in people's living environments, dietary habits and the aging population, cholelithiasis incidence is increasing. Currently, laparoscopic cholecystectomy (LC) is the preferred treatment for gallbladder stones, but the surgical method for patients with choledocholithiasis is controversial. An endoscopic retrograde cholangiopancreatography (pERCP) is performed preoperatively, followed by LC as the general treatment method. However, pERCP still has some disadvantages, such as prolonged hospital stay, increased incidence of postoperative pancreatitis, and increased duration of anesthesia. Therefore, intraoperative endoscopic retrograde cholangiopancreatography (iERCP) is proposed.
Objective: To compare the efficacy and safety of one-stage treatment and two-stage treatment for the management of patients with cholecystolithiasis and choledocholithiasis.
Search strategy: PubMed, Embase, Web of Science, and Cochrane databases were searched through October 2022. The search terms include cholangiolithiasis/bile duct stones/calculi, endoscopic retrograde cholangiopancreatography/ERCP, endoscopic sphincterotomy/EST, laparoendoscopic rendezvous (LERV), and laparoscopic cholecystectomy/LC.
Selection criteria: For the treatment of patients with cholecystolithiasis and choledocholithiasis in adults, randomized controlled trials (RCTs) comparing LC with iERCP vs. pERCP followed by LC were conducted.
Data collection and analysis: Data extraction and quality assessment were performed by two reviewers. We used Revman version 5.3 to analyze the collected data. The trials were grouped according to the evaluation results such as the overall mortality rate, overall morbidity rate, clearance rate of choledocholithiasis, incidence of pancreatitis, the length of hospitalization, and the length of operation.
Results: 9 RCTs (950 participants) were included in this meta-analyses. The overall morbidity rate in LC + iERCP group is lower than that in LC + pERCP group (RR: 0.57, 95% CI = 0.41–0.79, p = 0.0008). The clearance rate of choledocholithiasis in LC + iERCP group was almost the same as that in LC + pERCP group (RR: 1.03, 95% CI = 0.98–1.08, p = 0.28). The incidence of pancreatitis in LC + iERCP group is lower than that in LC + pERCP group (RR: 0.29, 95% CI = 0.13–0.67, p = 0.004). The length of operation of the LC + iERCP group seems to be similar to that of the LC + pERCP group (MD: 16.63 95% CI = −5.98–39.24, p = 0.15). LC + iERCP group has a shorter length of hospitalization than that in LC + pERCP group (MD: −2.68 95% CI = −3.39–−1.96, p < 0.00001). LC + iERCP group has lower postoperative second ERCP rate than that in LC + pERCP group (RR: 0.13, 95% CI = 0.03–0.57, p = 0.006).
Conclusion: Our study suggest that LC + iERCP may be a better option than LC + pERCP in the management of patients with both cholecystolithiasis and choledocholithiasis. This procedure can reduce the overall incidence of postoperative complications, especially the occurrence of postoperative pancreatitis. It could shorten the length of hospital stay, reduce postoperative second ERCP rate.
Introduction
In the field of hepatobiliary surgery, cholelithiasis is one of the most frequent and frequently occurring diseases. With the change of living environment, people's eating habits and aging, the incidence rate and incidence of diseases increased year by year, which has become a major disease affecting the quality of daily life. Epidemiological reports show that the worldwide incidence rate of cholelithiasis is about 10% to 35%, while gallstone patients account for 75% to 80% of cholelithiasis, of which more than 15% are combined with common bile duct stones (1).
Laparoscopic cholecystectomy is the first choice for the treatment of cholecystolithiasis. For a long time in the past, patients with cholecystolithiasis and choledocholithiasis need open choledochectomy or laparoscopic common bile duct exploration. With the gradual development of endoscopic technology in recent years, some new concepts and surgical methods have been widely recognized.
In 1968, McCunne et al. (2) from Washington University School of Medicine reported ERCP for the first time. Cholangiopancreatography was performed by inserting contrast agent into the duodenal Vater nipple under lateral endoscopic intubation to diagnose biliary and pancreatic diseases. In 1972, British gastroenterologist Cotton (3) first named ERCP based on his own experience and the experience of doctors all over the world, which is still in use today. In 1974, Kawai et al. (4) and Classen et al. (5) successively reported that ERCP was used for duodenal sphincterotomy to remove choledocholithiasis, which opened the era of ERCP treatment.
Laparoscopic cholecystectomy (LC) combined with laparoscopic common bile duct exploration (LCBDE) and endoscopic retrograde cholangiopancreatography (ERCP)/endoscopic sphincterotomy (EST) combined with laparoscopic cholecystectomy (EST + LC) are effective methods for the treatment of cholecystolithiasis combined with choledocholithiasis. The rendezvous technique was described for the first time by Deslandres et al. in 1993., and first completed by Feretis et al. In 1994. During laparoscopic cholecystectomy, a guide wire was inserted from the cystic duct to the duodenal papilla through the common bile duct, so as to guide the tube insertion under duodenoscopy. Finally, the stone basket can be applied through papillary. As a result of rendezvous technology, iERCP has a shorter learning curve and lower technical requirements for laparoscopic surgery, making it less complex to use (6). The aim of this meta-analysis was to evaluate the safety and effectiveness of pERCP vs. iERCP.
Objective
To compare the efficacy and safety of one-stage treatment and two-stage treatment for the management of patients with cholecystolithiasis and choledocholithiasis.
Methodology
Research types
Trials performed and published in English were considered when random assignments were made to one-stage LC combined with iERCP and two-stage pERCP followed by LC.
Participant types
In our review, only randomized controlled trials in patients with cholecystolithiasis and choledocholithiasis were considered, regardless of clinical symptoms.
Intervention types
Trials comparing one-stage LC combined with iERCP and two-stage pERCP followed by LC were considered.
Outcome measure types
Trials were considered if they demonstrated any of the following clinical outcomes:
1. Overall mortality rate (30 days postoperative).
2. Overall morbidity rate (30 days postoperative).
3. Incidence of pancreatitis.
4. Operative time.
5. Postoperative second ERCP rate.
6. Clearance rate of choledocholithiasis.
7. The length of hospital stay (time from admission to postoperative discharge).
Search strategy
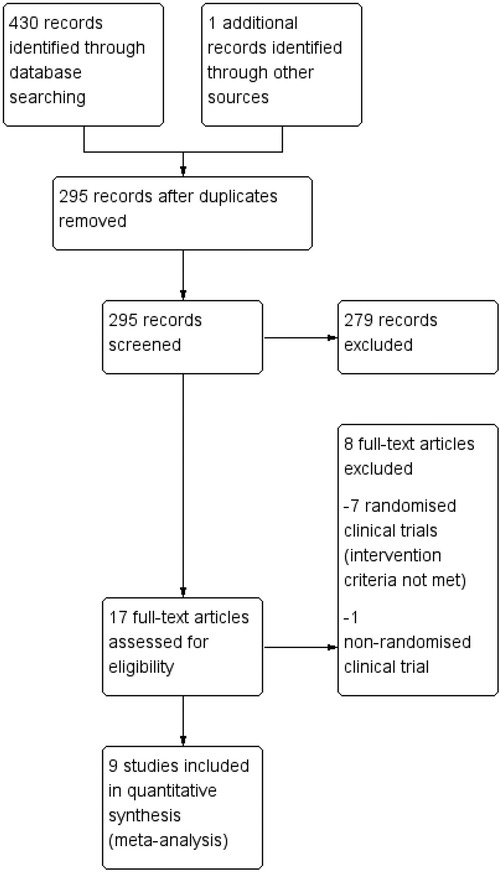
The following keywords were used to search PubMed, Embase, Web of Science, and Cochrane databases for all randomized controlled trials citing pre-operative vs. intra-operative ERCP in patients with cholecystolithiasis and choledocholithiasis: cholangiolithiasis/bile duct stones/calculi, endoscopic retrograde cholangiopancreatography/ERCP, endoscopic sphincterotomy/EST, laparoendoscopic rendezvous (LERV), and laparoscopic cholecystectomy/LC. The reference lists of published and review articles were thoroughly screened manually for duplicate studies and included only those that were relevant. The literature search deadline was October 2022. In PubMed, the detailed literature search strategy is (“cholangiolithiasis”[Title/Abstract] OR “bile duct stones” [Title/Abstract] OR “bile duct calculi” [Title/Abstract]) AND (“endoscopic retrograde cholangiopancreatography” [Title/Abstract] OR “ERCP” [Title/Abstract] OR “endoscopic sphincterotomy” [Title/Abstract] OR “EST” [Title/Abstract]) OR [“laparoendoscopic rendezvous” (Title/Abstract)] AND (“laparoscopic cholecystectomy” [Title/Abstract] OR “LC” [Title/Abstract]). After reviewing the titles and abstracts of relevant literatures retrieved, 430 literatures were obtained initially. Our study included 9 final articles after obtaining the full text and further reading.
Data collection and analysis
Based on the protocol's criteria, all potential trials were deemed as qualified (7). Literature quality evaluation and data extraction were independently completed by 2 evaluators and cross-checked. First, 2 evaluators independently reviewed all cited titles and abstracts to identify eligible references and eliminate duplications. Secondly, the full text of the qualified literature is read to determine whether it is finally selected. In case of disagreement during cross checking, both parties shall discuss and solve it. Two reviewers independently assessed the quality of the included studies based on the Cochrane Handbook for Systematic Reviews of Interventions, including random sequence generation, concealment of allocation, blinding of personnel and participants, blinding of outcome assessments, incomplete outcome data, and selective reporting. For missing information, we contacted the author by email to supplement it.
Statistical analysis and publication bias
For dichotomous variables, the risk ratio (RR) and 95% confidence intervals (CI) were calculated. For continuous variables, the therapeutic effect was expressed as mean difference (MD) with 95% CI. If different measurement methods or units were used for the same index and the mean values were significantly different, standardized mean difference (SMD) with 95% CI was used. If there were zero events in both groups, risk difference (RD) was used to avoid excluding zero events. Heterogeneity was assessed using I-square statistics (I2) (8). An I2 value greater than 50% indicates significant heterogeneity (8). In case of obvious heterogeneity, sensitivity analysis was performed by excluding each study separately, and then the pooled RR value and its 95% CI were recalculated for the remaining studies to evaluate the stability of the results. The fixed-effects model was used when heterogeneity was low, and the random-effects model was used when heterogeneity was high. p < 0.05 was considered statistically significant. We used a funnel plot to detect publication bias. Meta-analysis was performed using Review Manager Version 5.3.
Results
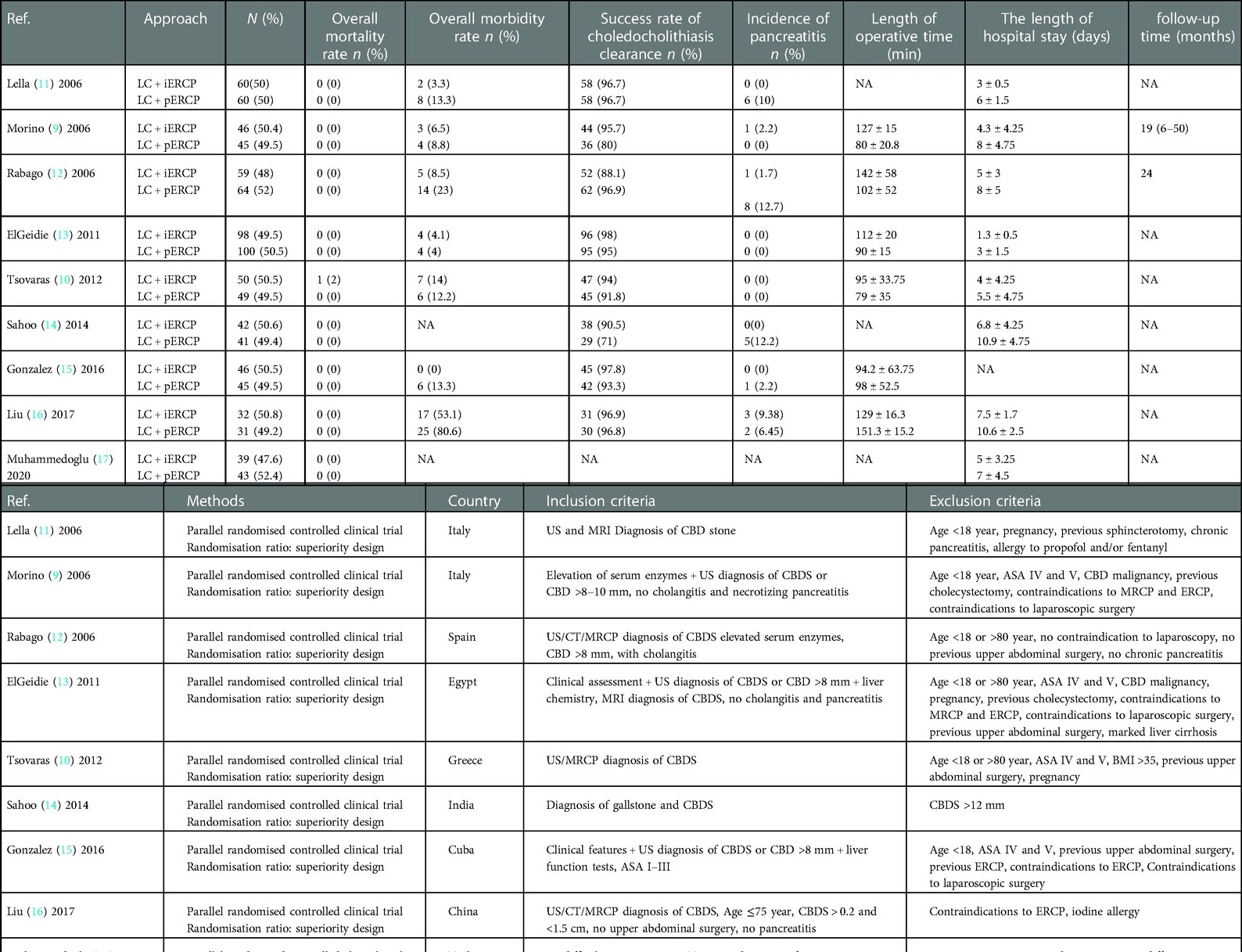
9 RCTs were included in this meta-analyses. The characteristics of included studies are summarized in Table 1 (9–17). Figure 1 illustrates the process of selecting relevant studies.
We evaluated the quality of the included RCTs according to the Cochrane Collaboration's Tool (see Figures 2A,B).
Overall mortality rate (30 days postoperative)
All nine trials (950 participants) measured overall mortality. According to the study of Tzovaras et al. (10), the only death in the LERV group was that of a 78-year-old, ASA III patient who was discharged on the 2nd postoperative day after having a successful rendezvous procedure. As a result of an intra-abdominal abscess that required drainage, the patient was re-hospitalized on day seven. On day 18, the patient died of multiple organ failure.
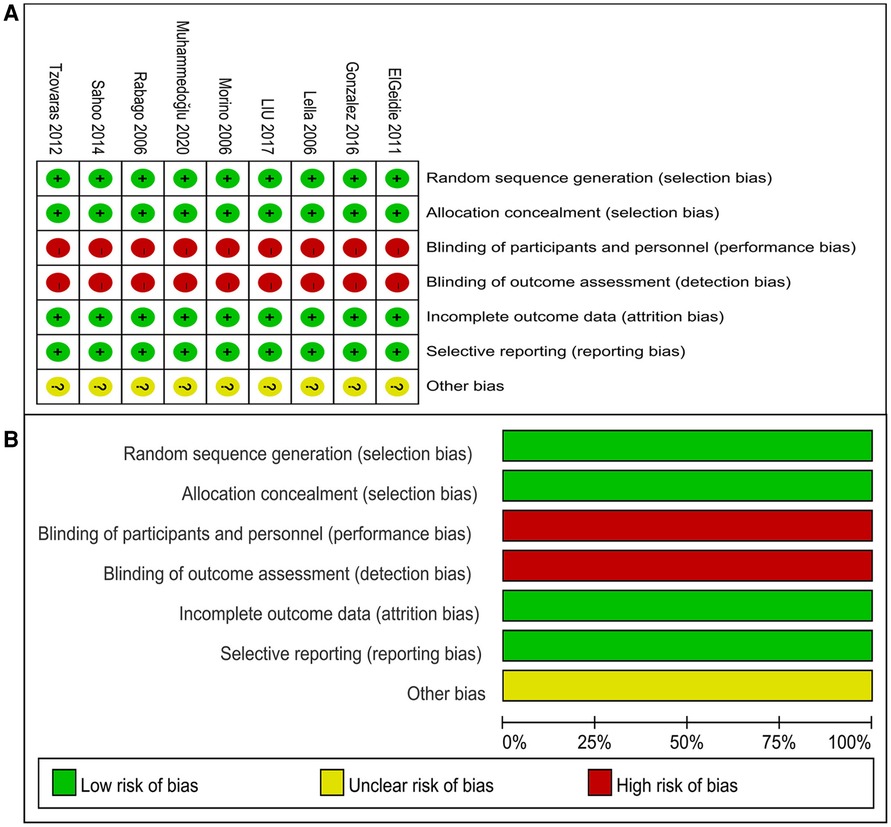
Overall morbidity rate (30 days postoperative)
Seven trials (785 participants) reported lower overall morbidity in the LC + iERCP group than that in the LC + pERCP group (RR: 0.57, 95% CI = 0.41–0.79, p = 0.0008) (Figure 3A). Statistical analysis showed that overall mortality were statistically significant between two groups, favoring LC + iERCP group. There was no heterogeneity among trials (I2 = 14%). The funnel plot has basically symmetrical sides, indicating no apparent publication bias.
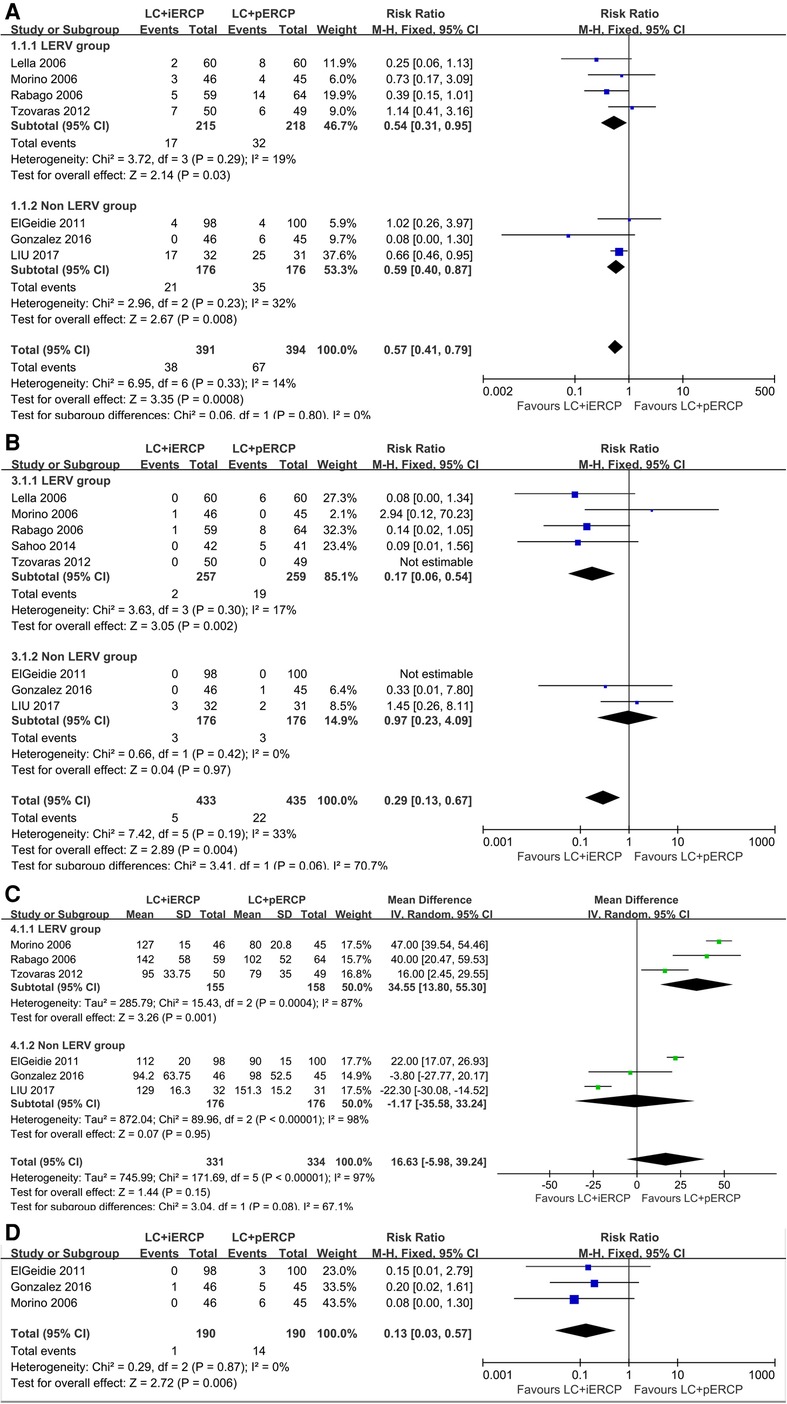
Figure 3. Forest plot of clinical outcomes. (A) Overall morbidity rate. (B) Incidence of pancreatitis. (C) Operative time. (D) Postoperative second ERCP rate.
Conclusion The overall morbidity rate in LC + iERCP group is lower than that in LC + pERCP group.
Incidence of pancreatitis
Eight trials (868 participants) reported lower incidence of pancreatitis in the LC + iERCP group than that in the LC + pERCP group (RR: 0.29, 95% CI = 0.13–0.67, p = 0.004) (Figure 3B). Statistical analysis showed that incidence of pancreatitis were statistically significant between two groups, favoring LC + iERCP group. In subgroup analysis, we found that in the LERV group, the incidence of pancreatitis in one-stage group was lower than that in two-stage group (RR: 0.17, 95% CI = 0.06–0.54, p = 0.002), while in the non LERV group, the incidence of pancreatitis in LC + iERCP group was similar to that in LC + pERCP group (RR: 0.97, 95% CI = 0.23–4.09, p = 0.97). The heterogeneity among trials was low (I2 = 33%). The funnel plot has basically symmetrical sides, indicating no apparent publication bias.
Conclusion The incidence of pancreatitis in LC + iERCP group is lower than that in LC + pERCP group.
Operative time
Six trials (665 participants) reported similar operative time between the two groups (MD: 16.63 95% CI = −5.98–39.24, p = 0.15) (Figure 3C). Between the two groups, there was no significant difference. In subgroup analysis, we found that in the LERV group, the operative time in one-stage group was shorter than that in two-stage group (MD: 34.55 95% CI = 13.80–55.30, p = 0.001), while in the non LERV group, the operative time in LC + iERCP group was similar to that in LC + pERCP group (MD: −1.17 95% CI = −35.58–33.24, p = 0.95). The heterogeneity among the trials is high (I2 = 97%). We found that heterogeneity was still high after excluding studies one by one. We did not find the source of heterogeneity after intensive reading of the six studys. The funnel plot has basically symmetrical sides, indicating no apparent publication bias.
Conclusion The length of operation of the LC + iERCP group seems to be similar to that of the LC + pERCP group.
Postoperative second ERCP rate
Only three trials (380 participants) reported lower postoperative second ERCP rate in the single-stage group compared to the two-stage group (RR: 0.13, 95% CI = 0.03–0.57, p = 0.006) (Figure 3D). There was a statistically significant difference between the two groups, favoring LC + iERCP. The heterogeneity among trials was low (I2 = 0%).
Conclusion LC + iERCP group has lower postoperative second ERCP rate than that in LC + pERCP group.
Clearance rate of choledocholithiasis
Eight trials (868 participants) reported similar clearance rate of choledocholithiasis between the two groups (RR: 1.03, 95% CI = 0.98–1.08, p = 0.28) (Figure 4A). There was no significant difference between the two groups. There is significant heterogeneity among the trials (I2 = 54%). We found that heterogeneity was significantly reduced by excluding two studys (Morino 2006 and Sahoo 2014) (RR: 1.01, 95% CI = 0.98–1.04, p = 0.61, I2 = 10%) (Figure 4B). We considered that inclusion and exclusion criteria may be the main cause of heterogeneity after intensive reading of the two studys. The funnel plot has basically symmetrical sides, indicating no apparent publication bias.
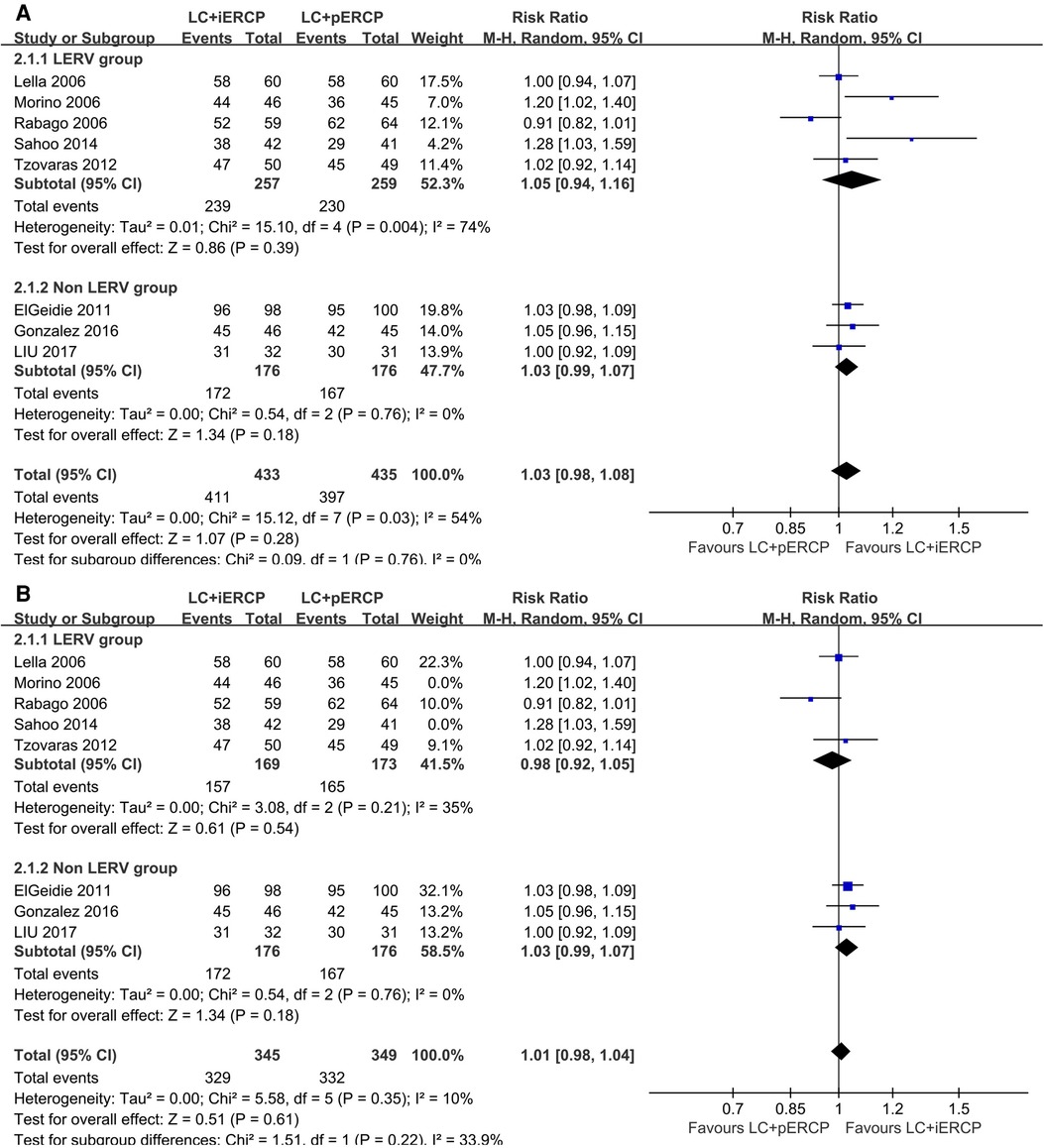
Figure 4. Forest plot of clearance rate of choledocholithiasis. (A) the pooled RR value of eight trials. (B) the pooled RR value of six trials after excluding two studys (Morino 2006 and Sahoo 2014).
Conclusion The clearance rate of choledocholithiasis in LC + iERCP group was almost the same as that in LC + pERCP group.
The length of hospital stay
Eight trials (859 participants) reported a shorter length of hospital stay in the LC + iERCP group compared to the LC + pERCP group (MD: −2.68 95% CI = −3.39–−1.96, p < 0.00001) (Figure 5A). There was a statistically significant difference between the two groups, favoring LC + iERCP. There is significant heterogeneity among the trials (I2 = 80%). Heterogeneity was significantly reduced after the exclusion of one study (ElGeidie 2011) (MD: −2.97 95% CI = −3.31–−2.64, p < 0.00001, I2 = 0%) (Figure 5B). We considered that inclusion and exclusion criteria may be the main cause of heterogeneity after intensive reading of the study. The funnel plot has basically symmetrical sides, indicating no apparent publication bias.
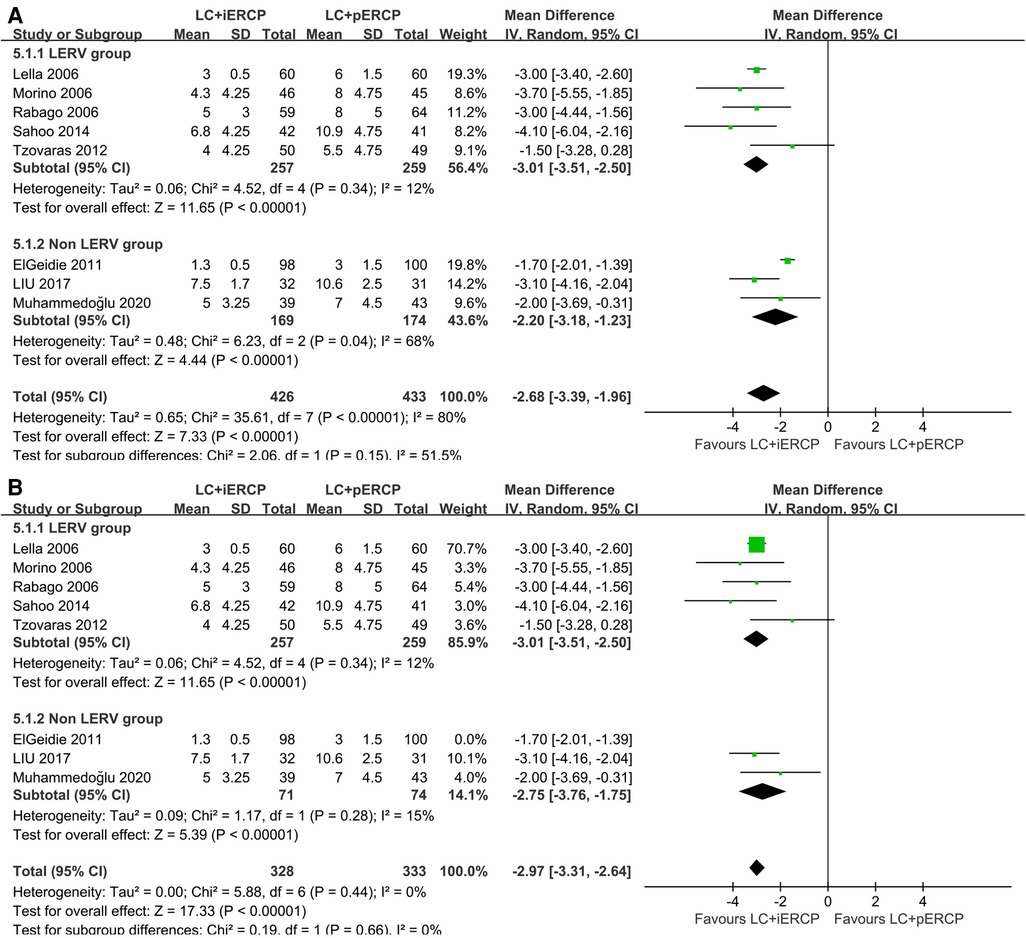
Figure 5. Forest plot of the length of hospital stay. (A) the pooled MD of eight trials. (B) the pooled MD of seven trials after excluding one study (ElGeidie 2011).
Conclusion LC + iERCP group has a shorter length of hospital stay than that in LC + pERCP group.
Discussion
Cholelithiasis is one of the frequent biliary diseases both at home and abroad, including gallbladder stones and choledocholithiasis. A gallstone passage from the cystic duct into the common bile duct is the most common cause of choledocholithiasis. Nearly 18% of patients hospitalized for cholecystolithiasis have choledocholithiasis (18), and within the first year following cholecystectomy, approximately 3.8% will experience choledocholithiasis symptomsy (19). The traditional surgical methods are open cholecystectomy and choledocholithotomy. These treatment methods are effective. Postoperative indwelling tube can reduce the incidence of bile leakage. Reserving stone removal channel is an effective method for the treatment of postoperative residual bile duct stones. However, its disadvantages are large trauma, slow recovery, intolerance to high-risk patients, long hospital stay, and catheter-related complications (20). With the progress of medical technology, people are more and more inclined to ensure the treatment effect. At the same time, the surgical method of small trauma and fast healing is adopted. Therefore, minimally invasive diagnosis and treatment came into being and has been widely used (21).
At present, LC + LCBDE and ERCP + LC are the two main minimally invasive surgical methods for the treatment of cholecystolithiasis and choledocholithiasis (22). Laparoscopic common bile duct exploration requires special expertise, which is not usually widely available, leaving ERCP as the most popular treatment for common bile duct stones. At present, there are three surgical methods for LC + ERCP in the treatment of cholecystolithiasis combined with choledocholithiasis: preoperative, intraoperative and postoperative ERCP. However, which method is better is still controversial. At present, preoperative ERCP is the most common clinical approach. However, this traditional two-stage procedure have some disadvantages. For example, before performing a cholecystectomy, patients have to wait for one to two days, during which time gallstones may enter the CBD and patients may suffer more pain and stay in the hospital longer. However, one-stage approach may have some advantages in these aspects.
In recent years, more and more studies have focused on the feasibility of one-stage procedure. The rapid development of medical technology and the accumulation of surgical and endoscopic experience make this method applied in clinic. Mattila et al. (23) compared the advantages of one stage LC + LCBDE to the 2 stage pre-ERCP + LC. The study found that the one stage LC + LCBDE had a higher CBD clearance rate, fewer procedures, shorter hospital stays, and lower hospital costs. The retrospective study concluded that one-stage LC + LCBDE might be an attractive treatment strategy for cholecystocholedocholithiasis if local expertise and resources are available. In patients with cholecystolithiasis and choledocholithiasis, Saito et al. (24) demonstrated the safety and feasibility of one-stage cholecystectomy after ERCP. These studys highlight the advantage of one-stage procedure.
Vakayil et al. (25), in a retrospective study, compared the benefits of the LC + LCBDE procedure with the LC + iERCP procedure for the management of choledocholithiasis. The study showed a statistically significant difference between the two procedures as for the mean operative time (p < 0.001). The study showed low morbidity and mortality in both groups. The study concluded that centers with extensive endoscopic experience might be more inclined to LC + iERCP because of its ease of access and shorter operative time.
There is still disagreement about the order of ERCP and LC for execution, as well as the follow time between the procedures. Several articles agree that LC should be carried out shortly after ERCP. It was reported that early LC was safe within 72 h after ERCP (26). However, some scholars believed that the time interval might lead to the emergence of new secondary common bile duct stone (27). Other disadvantages include longer hospital stay, increased treatment costs and readmission rate (28–31).
Our paper aimed at comparing the efficacy and safety of the single-stage and two-stage procedure. The main indicator of the therapeutic effect of common bile duct stones is whether the stones are removed. Chester Tan et al. (32) reported the CBD stones clearance rate in the one-stage group and two-stage group was 93.3% and 89.4%, respectively, which had a similar result to previous research results. In our study, we also found the clearance rate of choledocholithiasis in LC + iERCP group was almost the same as that in LC + pERCP group. We analyzed that the main reason was due to the continuous improvement of endoscopic technology and equipment. Only 1 patient death was reported in the 9 studies we included, who died on postoperative day 18 due to multiple organ failure. The patient's death is not directly related to the operation itself. The main reasons for the death of this patient were related to the patient's age, ASA status and delayed readmission (the patient was readmitted after 48 h of fever at home).
The main complications associated with ERCP include bleeding, perforation, cholangitis, cholecystitis, gastric ulcer, hyperamylasemia and pancreatitis. The main complications associated with LC include biliary tract injury, bile leak, bleeding, abdominal fluid, pneumonia, etc. Our study found lower overall morbidity rate in LC + iERCP group than that in LC + pERCP group (9.72% vs. 17.01%). We analyzed that the main reasons may be due to different anesthesia methods and the length of operation. Pancreatitis is one of the most common and serious postoperative complications of ERCP, with an incidence of 1%–5% (33). An incidence of pancreatitis of 3.11 percent was observed in our study. The risk factors inducing PEP are not yet clear. At present, most current studies have suggested two main aspects: one is patient-related factors, including female patients, age less than 50 years, pancreatic division, Oddi sphincter dysfunction, recurrent pancreatitis (at least 2 times) and history of PEP; the other is surgery-related factors, consisting of a precut sphincterotomy or sphincterotomy, excessive papillary injury, difficulty in catheterization or multiple catheterization attempts, failure of common bile duct lithotomy, history of pancreatic duct injection or endoscopic operation, deep placement of guide wire into pancreatic duct and no pancreatic duct stent placement (34–36). The 2014 European Society for Digestive Endoscopy (ESGE) Guidelines for PEP prevention pointed out that Oddi sphincter dysfunction, female patients, history of pancreatitis, catheterization attempt >10 min, pancreatic duct injection history, and guide wire length >1 cm into pancreatic duct were clear PEP risk factors, and the rest were possible risk factors (37). PEP can prolong the hospital stay and increase the medical cost of ERCP patients. At the same time, the risk of other complications and even death is significantly increased. In our study, we found the incidence of pancreatitis in LC + iERCP group is lower than that in LC + pERCP group. In subgroup analysis, we found that in the LERV group, the incidence of pancreatitis in LC + iERCP group was lower than that in LC + pERCP group, while in the non LERV group, the incidence of pancreatitis in LC + iERCP group was similar to that in LC + pERCP group. The main reason for our analysis was that the LERV group reduced the number of catheterizations.
A retrospectively cohort study (38) found that the one-stage group experienced a longer total operative time compared to the two-stage group (139.8 ± 46.8 min vs. 107.7 ± 40.6 min, p < 0.05). The retrospective study analysed this difference may because of the difficulty of LERV technology. In our study, the operative time, as assessed in six of the nine RCTs, was about the same between the two groups. However, in the subgroup analysis, we found that the LERV group had shorter operative time. The main reason for our analysis was that the application of LERV technology significantly shortened the intubation time of ERCP. Eight of the nine trials reported a shorter length of hospital stay in the LC + iERCP group compared to the LC + pERCP group. In the two-stage group, the interval time between the two procedures was generally 1 to 3 days, which led to a longer stay for the patient and a lack of compliance on their part. And the higher overall morbidity rate in two-stage group may also lead to longer hospital stays. Our results suggested that one-stage group had lower postoperative second ERCP rate than that in two-stage group. The most important reason was that gallbladder stones fell into the common bile duct during the interval time between operations.
Although single-stage surgery has a wide application prospect, we also need to pay attention to some problems in the operation process. First, endoscopic gas injection should be minimized during ERCP operation, and the residual gas in the intestine and stomach should be sucked as far as possible at the end of the operation. Second, we should try our best to complete the ERCP operation in the position of the LC, and minimize the movement of the patient's position to avoid some potential risks. Third, for some special cases such as Mirizzi syndrome, LERV technology may not be suitable, in which case we need traditional catheterization combined with Spyglass to complete the operation. Fourth, for the removal of large common bile duct stones, lithotripsy followed by balloon dilation may be a better choice.
According to our study, LERV technology can significantly reduce operation time and the occurrence of postoperative pancreatitis; therefore, we should incorporate this technology into one-stage surgeries as much as possible. Moreover, we recommend that standardized, effective procedures be developed to ensure the operation's success.
Of course, our research has some shortcomings: First, the inclusion criteria and exclusion criteria of the included literatures were not consistent; Second, most of the literature did not provide follow-up time and long-term stone recurrence rate; Third, the heterogeneity of the included literatures was large and no causes were found; Fourth, most of the included literature was too old, and there was little literature on the comparison between the two groups in the last 5 years; Sixth, The number of documents included was small; Seventh, none of the included literatures used a complication scale.
Conclusion
Our study suggest that LC + iERCP may be a better option than LC + pERCP in the management of patients with both cholecystolithiasis and choledocholithiasis. This procedure can reduce the overall incidence of postoperative complications, especially the occurrence of postoperative pancreatitis. It could shorten the length of hospital stay, reduce postoperative second ERCP rate.
Author contributions
SN: is the principal investigator with overall responsibility for the original draft. SN and SF: performed searching for relevant studies, data collection, and data analysis. KF: provided help in designing, data analysis and editing of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2023.1124955/full#supplementary-material.
References
1. Song ME, Chung MJ, Lee DJ, Oh TG, Park JY, Bang S, et al. Cholecystectomy for prevention of recurrence after endoscopic clearance of bile duct stones in Korea. Yonsei Med J. (2016) 57(1):132–1377. doi: 10.3349/ymj.2016.57.1.132
2. McCune WS, Shorb PE, Moscovitz H. Endoscopic cannulation of the ampulla of vater: a preliminary report. Ann Surg. (1968) 167(5):752–6. doi: 10.1097/00000658-196805000-00013
3. Cotton PB. Cannulation of the papilla of vater by endoscopy and retrograde cholangiopancreatography(ERCP). Gut. (1972) 13(12):1014–25. doi: 10.1136/gut.13.12.1014
4. Kawai K, Akasaka Y, Murakami K. Endoscopic sphincterotomy of the ampulla of vater. Gastrointest Endosc. (1974) 20(4):148–51. doi: 10.1016/S0016-5107(74)73914-1
5. Classen M, Demling L. Endoscopic sphincterotomy of the papilla of vater and extraction of stones from the choledochal duct (author's transl). Dtsch Med Wochenschr. (1974) 99(11):496–7. doi: 10.1055/s-0028-1107790
6. La Greca G, Barbagallo F, Sofia M, Latteri S, Russello D. Simultaneous laparoendoscopic rendezvous for the treatment of cholecystocholedocholithiasis. Surg Endosc. (2009) 24(4):769–80. doi: 10.1007/s00464-009-0680-3
7. Liberati A, Altman D, Tetzlaff J, Mulrow C, Gøtzsche P, Ioannidis J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: expla- nation and elaboration. PLoS Med. (2009) 6:e1000100. doi: 10.1371/journal.pmed.1000100
8. Higgins JPT, Green S. editors. Cochrane handbook for systematic reviews of interventions version 5.1.0 (updated March 2011). Copenhagen, Denmark: The Cochrane Collaboration, 2011 (2011).
9. Morino M, Baracchi F, Miglietta C, Furlan N, Ragona R, Garbarini A. Preoperative endoscopic sphincterotomy versus laparoendoscopic rendezvous in patients with gallbladder and bile duct stones. Ann Surg. (2006) 244:889–93; discussion 893–896. doi: 10.1097/01.sla.0000246913.74870.fc
10. Tsovaras G, Baloyiannis I, Zachari E, Symeonidis D, Zacharoulis D, Kapsoritakis A, et al. Laparoendoscopic rendezvous versus preoperative ERCP and laparoscopic cholecystectomy for the management of cholecystocholedocholithiasis: interim analysis of a controlled randomized trial. Ann Surg. (2012) 255:435–9. doi: 10.1097/SLA.0b013e3182456ec0
11. Lella F, Bagnolo F, Rebuffat C, Scalambra M, Bonassi U, Colombo E. Use of the laparoscopic-endoscopic approach, the so-called ‘‘rendezvous’’ technique, in cholecystocholedocholithiasis: a valid method in cases with patient-related risk factors for post-ERCP pancreatitis. Surg Endosc. (2006) 20:419–23. doi: 10.1007/s00464-005-0356-6
12. Rábago LR, C Vicente, F Soler, M Delgado, I Moral, Guerra I, et al. Two-stage treatment with preoperative endoscopic retrograde cholangiopancreatography (ERCP) compared with single-stage treatment with intraoperative ERCP for patients with symptomatic cholelithiasis with possible choledocholithiasis. Endoscopy. (2006) 38:779–86. doi: 10.1055/s-2006-944617
13. Elgeiddie AA, ElEbidy GL, Naeem YM. Preoperative versus intra-operative endoscopic sphincterotomy for management of common bile duct stones. Sure Endosc. (2011) 25(4):1230–7. doi: 10.1007/s00464-010-1348-8
14. Sahoo M, Pattnaik A, Kumar A. Randomized study on single stage laparo-endoscopic rendezvous (intraoperative ERCP) procedure versus two stage approach (preoperative ERCP followed by laparoscopic cholecystectomy) for the management of cholelithiasis with choledocholithiasis. J Minim Access Surg. (2014) 10:139–43. doi: 10.4103/0972-9941.134877
15. Barreras González JE, Torres Peña R, Ruiz Torres J, Martínez Alfonso MÁ, Brizuela Quintanilla R, Morera Pérez M. Endoscopic versus laparoscopic treatment for choledocholithiasis: a prospective randomized controlled trial. Endosc Int Open. (2016) 4:E1188–93. doi: 10.1055/s-0042-116144
16. Zhiyi Liu, Luyao Zhang, Yanling Liu, Yang Gu, Tieliang Sun. Efficiency and safety of one-step procedure combined laparoscopic cholecystectomy and eretrograde cholangiopancreatography for treatment of cholecysto-choledocholithiasis: a randomized controlled trial. Am Surg. (2017) 83(11):1263–7. doi: 10.1177/000313481708301129
17. Muhammedoğlu B, Kale IT. Comparison of the safety and efficacy of single-stage endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy versus two-stage ERCP followed by laparoscopic cholecystectomy six-to-eight weeks later: a randomized controlled trial. Int J Surg. (2020) 76:37–44. doi: 10.1016/j.ijsu.2020.02.021
18. Martin DJ, Vernon DR, Toouli J. Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev. (2006) 2:CD003327. doi: 10.1002/14651858.CD003327.pub2
19. Jarhult J. Is preoperative evaluation of the biliary tree necessary in uncomplicated gallstone disease? Results of a randomized trial. Scand J Surg. (2005) 94:31–3. doi: 10.1177/145749690509400108
20. Enochsson L, Lindberg B, Swahn F, Arnelo U. Intraoperative endoscopic retrograde cholangiopancreatography (ERCP) to remove common bile duct stones during routine laparoscpic cholecystectomy does not prolong hospitalization. Surg Endosc. (2004) 18:367–71. doi: 10.1007/s00464-003-9021-0
21. David W. Exploration of the common bile duct in the era of laparoscopic cholecystectomy. ANZ J Surg. (2002) 72(4):252. doi: 10.1046/j.1445-2197.2002.02386.x
22. Lu J, Cheng Y, Xiong XZ, Lin YX, Wu SJ, Cheng NS. Two-stage vs single-stage management for concomitant gallstones and common bile duct stones. World J Gastroenterol. (2012) 18(24):3156–66. doi: 10.3748/wjg.v18.i24.3156
23. Mattila A, Mrena J, Kellokumpi I. Cost-analysis and effectiveness of one-stage laparoscopic versus two-stage endolaparoscopic management of cholecystocholedocholithiasis: a retrospective cohort study. BMC Surg. (2017) 17(1):79. doi: 10.1186/s12893-017-0274-2
24. Saito H, Kadono Y, Kamikawa K, Urata A, Imamura H, Matsushita I, et al. The incidence of complications in single-stage endoscopic stone removal for patients with common bile duct stones: a propensity score analysis. Intern. Med. (2018) 57(4):469–77. doi: 10.2169/internalmedicine.9123-17
25. Victor Vakayil, Klinker ST, Sulciner ML, Reema Mallick, Guru Trikudanathan, Amateau SK, et al. Single-stage management of choledocholithiasis: intraoperative ERCP versus laparoscopic common bile duct exploration. Surg Endosc. (2020) 34(10):4616–25. doi: 10.1007/s00464-019-07215-w
26. Ming Li VK, Kai Yum JL, Yeung YP. Optimal timing of elective laparoscopic cholecystectomy after acute cholangitis and subsequent clearance of choledocholithiasis. An J Surg. (2010) 200(4):483–8. doi: 10.1016/j.amjsurg.2009.11.010
27. Siegel JH, Safrany L, Ben-Zvi JS, Pullano WE, Cooperman A, Stenzel M, et al. Duodenoscopic sphincterotomy in patients with gallbladders in situ: report of a series of 1272 patients. Am J Gastroenterol. (1988) 83:1255–8.3189263
28. Lau JY, Leow CK, Fung TM, Suen BY, Yu LM, Lai PB, et al. Cholecystectomy or gallbladder in situ after endoscopic sphincterotomy and bile duct stone removal in Chinese patients. Gastroenterology. (2006) 130(1):96–103. doi: 10.1053/j.gastro.2005.10.015
29. Hong DF, Gao M, Mou YP, Cai XJ, Bryner U. Study on laparoscopic cholecystectomy combined with intraoperative endoscopic sphincterectomy and stone removal. Chin J Surg. (2000) 38:677–9.11832137
30. Hong DF, Gao M, Bryner U, Cai XJ, Mou YP. Intraoperative endoscopic sphincterotomy during laparoscopic cholecystectomy. World J Gastroenterol. (2000) 6:448–50. doi: 10.3748/wjg.v6.i3.448
31. Hong DF, Li JD, Gao M, Yuan XM, Wang JG, Cai XJ, et al. One hundred and six cases analyses of laparoscopic technique combined with intraoperative cholangiogram and endoscopic sphincterotomy in sequential treatment of cholelithiasis. Chin J Gen Surg. (2003) 15:648–50.
32. Chester Tan, Omar Ocampo, Raymund Ong, Kim Shi Tan. Comparison of one stage laparoscopic cholecystectomy combined with intra-operative endoscopic sphincterotomy versus two-stage pre-operative endoscopic sphincterotomy followed by laparoscopic cholecystectomy for the management of pre-operatively diagnosed patients with common bile duct stones: a meta-analysis. Surg Endosc. (2018) 32:770–8. doi: 10.1007/s00464-017-5739-y
33. Jeurnink SM, Siersema PD, Steyerberg EW, Dees J, Poley JW, Haringsma J, et al. Predictors of complications after endoscopic retrograde cholangiopancreatography: a prognostic model for early discharge. Surg Endosc. (2011) 25(9):2892–900. doi: 10.1007/s00464-011-1638-9
34. Iorgulescu A, Sandu I, Turcu F, Iordache N. Post-ERCP acute pancreatitis and its risk factors. J Med Life. (2013) 6(1):109–13.23599832
35. Wan J, Ren Y, Zhu Z, Xia L, Lu N. How to select patients and timing for rectal indomethacin to prevent post-ERCP pancreatitis: a systematic review and meta-analysis. BMC Gastroenterol. (2017) 17(1):43. doi: 10.1186/s12876-017-0599-4
36. Freeman ML. Preventign post-ERCP pancreatitis: update 2016. Curr Treat Options Gastro. (2016) 14(3):1–8. doi: 10.1007/s11938-016-0097-8
37. Dumonceau JM, Andriulli A, Elmunzer BJ, Mariani A, Meister T, Deviere J, et al. Prophylaxis of post-ERCP pancreatitis: european society of gastrointestinal endoscopy (ESGE) guideline—updated June 2014. Endoscopy. (2014) 46(9):799–815. doi: 10.1055/s-0034-1377875
Keywords: cholangiolithiasis, endoscopic retrograde cholangiopancreatography, endoscopic sphincterotomy, laparoendoscopic rendezvous, laparoscopic cholecystectomy
Citation: Nie S, Fu S and Fang K (2023) Comparison of one-stage treatment versus two-stage treatment for the management of patients with common bile duct stones: A meta-analysis. Front. Surg. 10:1124955. doi: 10.3389/fsurg.2023.1124955
Received: 15 December 2022; Accepted: 11 January 2023;
Published: 3 February 2023.
Edited by:
Argyrios Ioannidis, Athens Medical Group, GreeceReviewed by:
Roberto de la Plaza Llamas, University Hospital of Guadalajara, SpainFrancesco Mongelli, Lugano Regional Hospital, Switzerland
© 2023 Nie, Fu and Fang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kaiyan Fang fang1989kaiyan@163.com
Specialty Section This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
 Shanmao Nie
Shanmao Nie Shangyu Fu2
Shangyu Fu2  Kaiyan Fang
Kaiyan Fang