Malignant Tumors Misdiagnosed as Liver Hemangiomas
- 1Departments of General Surgery, Istanbul Faculty of Medicine, Istanbul University, Istanbul, Turkey
- 2Departments of Radiology, Istanbul Faculty of Medicine, Istanbul University, Istanbul, Turkey
- 3Departments of Pathology, Istanbul Faculty of Medicine, Istanbul University, Istanbul, Turkey
Background and Aim: To derive lessons from the data of patients who were followed for various periods with the misdiagnosis of liver hemangioma and eventually found to have a malignancy.
Material and Methods: The records of 23 patients treated between 2003 and 2018 were analyzed retrospectively.
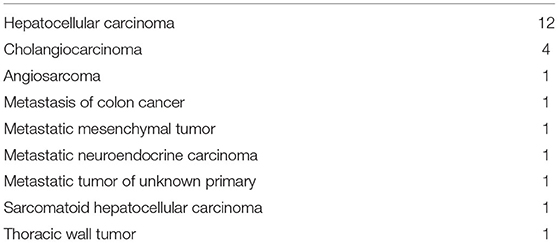
Results: Twelve patients were men and 11 were women; median (range) age was 55 (35–80). The principal diagnostic modality for the initial diagnosis was ultrasonography (n:8), magnetic resonance imaging (MRI) (n:13), and computed tomography (CT) (n:2). At our institution, MRI was performed in 16 patients; the diagnosis was made with the available MRI and CT studies in five and two patients, respectively. In other words, the ultrasonography interpretations were not confirmed on MRI; in others, the MRI or CT examinations were of low quality or they had not been interpreted properly. Fifteen patients underwent surgery; the other patients received chemotherapy (n:6) or chemoembolization (n:2). The misdiagnosis caused a median (range) 10 (0–96) months delay in treatment. The final diagnoses were hepatocellular carcinoma in 12 patients, cholangiocarcinoma in four patients, metastatic mesenchymal tumor, metastasis of colon cancer, metastatic neuroendocrine carcinoma, sarcomatoid hepatocellular carcinoma, angiosarcoma, thoracic wall tumor, and metastatic tumor of unknown primary in one patient each.
Conclusions: High-quality MRI with proper interpretation and judicious follow up are vital for the accurate differential diagnosis of liver lesions.
Introduction
Hemangioma is the most common liver tumor with an incidence between 1 and 20% (1). The diagnosis is being made with increasing frequency due to the widespread availability of and broadening indications for imaging techniques. Actually, treatment is indicated in a very small subset of patients for pain, enlargement, diagnostic uncertainty, and extremely rare indications such as rupture and Kasabach-Merritt syndrome. The real burden to the health care system is the problem of making accurate diagnoses in a very high number of patients-an issue that entails the risk of missed malignancies. Although the issue has been commonly discussed on an anecdotal basis in hepatopancreatobiliary surgery circles, case reports and only a single series including 28 patients (Portolani) have been published (2–11). Most case reports are actually “clinician's success” stories in which the radiological ambiguity was resolved, usually by biopsy or resection (3–5, 9, 10, 12, 13). Others and the paper by Portolani et al. are on the most probably underreported problem of the patients whose courses took an unfavorable direction due to misdiagnosis (2, 6–8, 11).
In this paper, the institutional experience was analyzed to derive lessons from the data of 23 patients who were followed for various periods with the misdiagnosis of liver hemangioma and eventually found to have a malignancy.
Aim of the Study
To derive lessons from the data of patients who were followed for various periods with the misdiagnosis of liver hemangioma and eventually found to have a malignancy.
Materials and Methods
The records of 23 patients who attended the outpatient clinic between 2003 and 2018 were analyzed retrospectively. This is a retrospective study on the data of the patients who were treated at our hospital according to the best practices of the study period. Our IRB waives the need for ethical approval for these observational studies. The research was conducted according to the principles of the World Medical Association Declaration of Helsinki “Ethical Principles for Medical Research Involving Human Subjects” (amended in October 2013).
Results
Twelve patients were men and 11 were women; median (range) age was 55 (35–80).
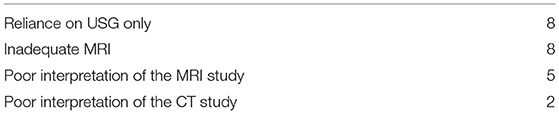
Ten of the 23 patients were HBsAg positive and one patient was anti-HCV antibody positive; one other patient had been a moderate-to-heavy drinker for 15 years. The causes of the initial diagnostic errors were summarized in Table 1; the issue was resolved by proper MRI at our institution (n:13) or correct interpretation of the available MRI (n:5) or CT (n:2) studies.
Fifteen patients underwent surgery. The other eight patients received chemotherapy (n:6) or chemoembolization (n:2). The misdiagnosis caused a median (range) 10 (0–96) months delay in treatment. The final diagnoses were summarized in Table 2.
Of the eight patients who were not the candidates for surgery, four had been referred with the wrong diagnoses but there were no significant delays before treatment: hepatocellular carcinoma in an 80-year-old patient with comorbid conditions, hepatocellular carcinoma with peritoneal metastases, metastatic sigmoid colon carcinoma, and metastatic tumor of unknown origin. The histories of the other four patients reveal important lessons for the clinician:
First, the patient who had a neuroendocrine tumor had undergone laparoscopic cholecystectomy 2 years before. The preoperative MRI examination had detected a “hemangioma” in the left lobe; the operation report was not available. Multiple liver masses (largest: 115 mm) and the pancreatic primary tumor were diagnosed at our institution. Second, the patient with giant inoperable cholangiocarcinoma surrounding the superior mesenteric and hepatic arteries and invading the portal vein had been under follow-up for 4 years, with USG only at various centers with the diagnosis of liver hemangioma.
Third, the 44-year-old woman with extensive intrahepatic dissemination of hepatocellular carcinoma had been a known HBV carrier for 2 years but had not been referred to liver imaging until she became symptomatic. She was treated with chemoembolization.
The fourth patient had undergone resection of a 11-cm retroperitoneal tumor; the pathological diagnosis was “mesenchymal tumor with lipomatous areas” and the pathologist stated that there was no evidence of malignancy. In fact, she had multiple but operable metastases that were interpreted as “hemangiomas” on the preoperative USG and “hemangiomas or cystic metastases” on the preoperative CT (the films were not available); the MRI examination recommended by the radiologist had not been performed. The liver lesions were followed by USG for 2 years without apparent growth in size. At 7 years after the operation, she presented with abdominal pain; the metastases had increased in number and the largest liver lesion had grown from 4 to 13 cm. Core biopsy of the liver lesion and examination of the original paraffin sections at the university pathology department revealed mesenchymal tumor with hemangiopericytomatous pattern; the Ki-67 index was 3% in the primary tumor and 20% in the liver metastasis. She was referred to the oncology department.
The two patients with the longest delays in diagnoses (86 and 96 months) were HBV carriers in whom a single mass lesion had been misdiagnosed as a hemangioma (most probably regenerative of dysplastic nodules) and was not followed up properly. Single hepatocellular carcinomas (6 and 3.3 cm, respectively) and were eventually diagnosed by MRI; there were no concomitant hemangiomas.
Discussion
Misdiagnosis of a malignancy as a hemangioma is a widely acknowledged but most probably underreported issue. There are three aspects:
First, the sheer magnitude of the problem. The total population of the OECD countries exceeds 1 billion people. The reported incidence of liver hemangiomas varies between 1 and 20% (1). In 2015, the average number of CT examinations in the OECD countries was 143 per 1,000 population; the corresponding number for MRI was 64.8 (14). Although these figures include examinations for all locations, it is obvious that the differential diagnosis of at least several hundred thousands of hemangiomas is a major undertaking. The very high (98–99%) but-not-100% sensitivity and specificity of MRI for hemangiomas leave a speciously small error margin that actually poses risks to thousands of patients (15). For the sake of comparison, during the study period of the present report on 23 misdiagnosed cases, liver hemangioma (multiple in some cases) was correctly identified in 1,243 patients (data collected for a another study with the following exclusion criteria: previous treatment for any malignancy (except for well-differentiated thyroid carcinoma), use of vasoconstrictor or anticoagulant drugs, history of liver surgery for any indication and cirrhosis).
Second, the misconception that a proper USG examination is adequate for the diagnosis of a hemangioma and further examination is unnecessary (16, 17). Only 80 % of the liver hemangiomas have a typical appearance on USG (18, 19). Also, hemangiomas undergo various changes (e.g., sclerosis) and their appearances change over time (20).
Third is the distinction between efficacy and effectiveness in imaging. The performance of experienced radiologists using state-of-the-art technology at a university hospital cannot represent the overall performance of an imaging technique under less-than-ideal diverse conditions. The so-called atypical hemangioma may actually be a misdiagnosed hepatocellular carcinoma or cholangiocarcinoma. Therefore, the responsibility of these patients should be assumed by specialized teams including dedicated radiologists (21). Sixteen of the 24 patients in this series had undergone a CT or MRI examination. The quality of the imaging was unacceptable in seven patients. Instead of making a confident diagnosis of a hemangiomas the radiologist should have ordered repeated imaging. In the remaining seven patients with acceptable image quality, the interpretation had been inaccurate. Similarly, in the study by Portolani et al., 75% of the incorrect diagnoses were made at low volume centers. A high-volume center was “characterized by the availability of an interdisciplinary group for the management of liver disease, by a tertiary-level or an academic hospital, or by the certification of almost 40 liver resections per year” (16).
The published literature and the cases reported here lead us to point out the following:
1- A proper contrast-enhanced CT/MRI examination with a state-of-the art apparatus is mandatory for proper characterization of liver lesions, particularly in patients with chronic viral hepatitis (22–25). According to recent data, an MRI examination with a hepatocyte-specific agent is preferred (26, 27).
2- Even the most specific examination method may fail in rare situations (27), especially outside academic centers. The suggestion stated by Portolani et al. (16) to repeat the imaging examination 4–6 months later is a practical safeguard.
3- The clinician should avoid the misconception that “conservative follow up” is always “safe.” Although the radiologist makes the imaging diagnosis, the “overall” diagnosis and responsibility of the patient rests on the clinician.
4- Follow up may be conducted at the same institution (e.g., patients with chronic viral hepatitis) or coordinated with the referring institution or family physician (patients with no or modifiable risk factors such as obesity for chronic liver disease).
A theoretically possible confounding factor is the development of imaging technology during the 15-year study period. However, as reported in Table 1, this may have been the case in at most eight cases (one-third of the patients) in whom inadequate MRI images were the causes of the initial error. Still, the misdiagnosis could be identified at our institution after contrast-enhanced dynamic MRI. In the remaining two-thirds of the patients, reliance on USG only or inadequate interpretation of the available CT or MRI images were implicated.
A limitation of this study is that the data does not allow us to calculate the frequency of misdiagnosis. The patients reported here belong to part of the numerator (there may be other misdiagnosed patients at the initial institutions; the denominator (the total number of patients who received a diagnosis of liver hemangioma at the initial institutions during a particular period) is unknown.
Conclusion
A multidisciplinary team approach at an experienced center is recommended for a reliable baseline assessment of a liver mass, especially in patients with chronic liver conditions.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author's Note
A preliminary report was presented at the 13th Turkish National Congress of HPB Surgery, November 1–4, 2017, Antalya, Turkey.
Author Contributions
MY, MG, and AP: collecting data and writing. İO: design of study, writing, supervision, and last control of study. YT, Cİ, and BA: supervision. İŞ: collecting analysis data. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Belghiti J, Dokmak S, Vilgrain V, Paradis V. Benign liver lesions. In: Jarnagin WR, Blumgart LH, editors. Blumgart's Surgery of the Liver, Biliary Tract, and Pancreas. Saunders: Elsevier (2012). p. 1250–67.
2. Farlow DC, Little JM, Gruenewald SM, Antico VF, O'Neill P. A case of metastatic malignancy masquerading as a hepatic hemangioma on labeled red blood cell scintigraphy. J Nucl Med. (1993) 34:1172–4.
3. Ji EK, Ryu JS, Kang GH, Moon DH, Auh YH, Lee HK. Pelioid-type hepatocellular carcinoma masquerading as a hepatic hemangioma on technetium-99m red blood cell scintigraphy. Clin Nucl Med. (2001) 26:33–5. doi: 10.1097/00003072-200101000-00008
4. Kawasaki T, Kudo M, Inui K, Ogawa C, Chung H, Minami Y. Hepatocellular carcinoma mimicking cavernous hemangioma on angiography and contrast enhanced harmonic ultrasonography. A case report. Hepatol Res. (2003) 25:202–12. doi: 10.1016/S1386-6346(02)00249-8
5. Lacout A, El Hajjam M, Julie C, Lacombe P, Pelage JP. Liver metastasis of a mucinous colonic carcinoma mimicking a haemangioma in T2-weighted sequences. J Med Imaging Radiat Oncol. (2008) 52:580–2. doi: 10.1111/j.1440-1673.2008.02014.x
6. Kim J, Han HS, Yoon YS, Cho JY, Ahn KS, Kwon Y. Outcomes of the patients who were postoperatively diagnosed as malignancy after laparoscopic distal pancreatectomy. Surg Laparosc Endosc Percutaneous Tech. (2012) 22:467–70. doi: 10.1097/SLE.0b013e3182632833
7. Okano A, Sonoyama H, Masano Y, Taniguchi T, Ohana M, Kusumi F, et al. The natural history of a hepatic angiosarcoma that was difficult to differentiate from cavernous hemangioma. Intern Med. (2012) 51:2899–904. doi: 10.2169/internalmedicine.51.7994
8. Yang K, Cheng YS, Yang JJ, Jiang X, Guo JX. Primary hepatic neuroendocrine tumor with multiple liver metastases: a case report with review of the literature. World J Gastroenterol. (2015) 21:3132–8. doi: 10.3748/wjg.v21.i10.3132
9. Tan H, Xu L, Liu X, Si S, Sun Y, Liu L, et al. Hepatocellular carcinoma in nonalcoholic fatty liver disease mimicking benign hemangioma: two case reports and literature review. Int J Clin Exp Pathol. (2015) 8:15350–5.
10. Aumpansub P, Chaiteerakij R, Geratikornsupuk N, Thanapirom K, Sanpavat A, Chaopathomkul B, et al. Atypical image of hepatocellular carcinoma mimicking hemangioma. ACG Case Rep J. (2016) 3:e119. doi: 10.14309/crj.2016.92
11. Garcia AR, Ribeiro J, Gervásio H, Castro E, Sousa F. Hepatic angiosarcoma masquerading as hemangioma: a challenging differential diagnosis. Acta Med Port. (2017) 30:750–3. doi: 10.20344/amp.8593
12. Arçay A, Kintrup GT, Gelen MT, Arslan G, Karayalçin B. Hepatoblastoma mimicking hemangioma in labeled red blood cell scintigraphy. Clin Nucl Med. (2019) 44:229–31. doi: 10.1097/RLU.0000000000002418
13. Ansari-Gilani K, Modaresi Esfeh J. Unusual MRI appearance of a well differentiated hepatocellular carcinoma, mimicking a cavernous hemangioma: a case report. Radiol Case Rep. (2019) 14:885–8. doi: 10.1016/j.radcr.2019.04.002
15. Mamone G, Di Piazza A, Carollo V, Cannataci C, Cortis K, Vicenzo Bartolotta T, et al. Imaging of hepatic hemangioma: from A to Z. Abdom Radiol. (2020) 45:672–91. doi: 10.1007/s00261-019-02294-8
16. Portolani N, Baiocchi G, Gheza F, Molfino S, Grazioli L, Olivetti L, et al. Impact on liver cancer treatment of a first erroneous diagnosis of hemangioma. World J Surg. (2014) 38:2685–91. doi: 10.1007/s00268-014-2643-7
17. Leifer DM, Middleton WD, Teefey SA, Menias CO, Leahy JR. Follow-up of patients at low risk for hepatic malignancy with a characteristic hemangioma at US. Radiology. (2000) 214:167–72. doi: 10.1148/radiology.214.1.r00ja09167
18. Gibney RG, Hendin AP, Cooperberg PL. Sonographically detected hepatic hemangiomas: absence of change over time. AJR Am J Roentgenol. (1987) 149:953–7. doi: 10.2214/ajr.149.5.953
19. Moody AR, Wilson SR. Atypical hepatic hemangioma: a suggestive sonographic morphology. Radiology. (1993) 188:413–7. doi: 10.1148/radiology.188.2.8327687
20. Vilgrain V, Boulos L, Vullierme MP, Denys A, Terris B, Menu Y. Imaging of atypical hemangiomas of the liver with pathologic correlation. Radiographics. (2000) 20:379–97. doi: 10.1148/radiographics.20.2.g00mc01379
21. Mathew RP, Sam M, Raubenheimer M, Patel V, Low G. Hepatic hemangiomas: the various imaging avatars and its mimickers. Radiol Med. (2020) 125:801–15. doi: 10.1007/s11547-020-01185-z
22. van Leeuwen MS, Noordzij J, Feldberg MA, Hennipman AH, Doornewaard H. Focal liver lesions: characterization with triphasic spiral CT. Radiology. (1996) 201:327–36. doi: 10.1148/radiology.201.2.8888219
23. Duran R, Ronot M, Kerbaol A, Van Beers B, Vilgrain V. Hepatic hemangiomas: factors associated with T2 shine-through effect on diffusion-weighted MR sequences. Eur J Radiol. (2014) 83:468–78. doi: 10.1016/j.ejrad.2013.11.023
24. Kudo M, Matsui O, Izumi N, Iijima H, Kadoya M, Imai Y, et al. Surveillance and diagnostic algorithm for hepatocellular carcinoma proposed by the liver cancer Study Group of Japan: 2014 Update. Oncology. (2014) 87(Suppl. 1):7–21. doi: 10.1159/000368141
25. Semelka RC, Nimojan N, Chandana S, Ramalho M, Palmer S, DeMulder D, et al. MRI features of primary rare malignancies of the liver: a report from four university centres. Eur Radiol. (2018) 28:1529–39. doi: 10.1007/s00330-017-5102-7
26. Kim YY, Park MS, Aljoqiman KS, Choi JY, Kim MJ. Gadoxetic acid-enhanced magnetic resonance imaging: hepatocellular carcinoma and mimickers. Clin Mol Hepatol. (2019) 25:223–33. doi: 10.3350/cmh.2018.0107
Keywords: hemangioma, atypical hemangioma, misdiagnosis, liver malignancy, malign mass
Citation: Yıldırım MB, Şahiner İT, Poyanlı A, Acunaş B, Güllüoǧlu M, İbiş C, Tekant Y and Özden İ (2021) Malignant Tumors Misdiagnosed as Liver Hemangiomas. Front. Surg. 8:715429. doi: 10.3389/fsurg.2021.715429
Received: 26 May 2021; Accepted: 19 July 2021;
Published: 11 August 2021.
Edited by:
Hakan Kulacoglu, Ankara Hernia Center, TurkeyReviewed by:
Ali Coskun, Izmir Bozyaka Training and Research Hospital, TurkeyBariş Saylam, Ankara City Hospital, Turkey
Copyright © 2021 Yıldırım, Şahiner, Poyanlı, Acunaş, Güllüoǧlu, İbiş, Tekant and Özden. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Murat Baki Yıldırım, dr.mbyildirim@gmail.com
†Present address: Murat Baki Yıldırım İbrahim Tayfun Şahiner, Faculty of Medicine, Hitit University, Çorum, Turkey
‡ORCID: Murat Baki Yıldırım orcid.org/0000-0001-9176-1160
İbrahim Tayfun Şahiner orcid.org/0000-0002-3921-7675
Arzu Poyanlı orcid.org/0000-0002-8851-1109
Bülent Acunaş orcid.org/0000-0003-4695-6043
Mine Güllüoǧlu orcid.org/0000-0002-3967-0779
Cem İbiş orcid.org/0000-0002-5602-375X
Yaman Tekant orcid.org/0000-0001-8926-7948
İlgin Özden orcid.org/0000-0001-7360-628X
 Murat Baki Yıldırım
Murat Baki Yıldırım İbrahim Tayfun Şahiner1,†,‡
İbrahim Tayfun Şahiner1,†,‡