Designing healthcare for human use: Human factors and practical considerations for the translational process
- 1Graduate Program in Translational Biology, Medicine and Health, Virginia Tech, Blacksburg, VA, United States
- 2Department of Psychology, Virginia Tech, Blacksburg, VA, United States
- 3Systems Science and Industrial Engineering, SUNY Binghamton University, Vestal, NY, United States
- 4Human Factors, Carilion Clinic, Roanoke, VA, United States
- 5Department of Human Nutrition, Foods, and Exercise, Virginia Tech, Blacksburg, VA, United States
- 6Department of Health Systems and Implementation Science, Virginia Tech Carilion School of Medicine, Roanoke, VA, United States
- 7Fralin Biomedical Research Institute at VTC, Roanoke, VA, United States
In recent years, the focus of implementation science (IS) shifted to emphasize the influence of contextual factors on intervention adaptations in clinical, community, and corporate settings. Each of these settings represent a unique work system with varying contexts that influence human capabilities, needs, and performance (otherwise known as “human factors”). The ease of human interaction with a work system or an intervention is imperative to IS outcomes, particularly adoption, implementation, and maintenance. Both scientific approaches consider the “big picture” when designing interventions for users and stakeholders to improve work and health outcomes. IS and human factors are therefore complementary in nature. In this paper, the authors will (1) provide perspective on the synergistic relationship between human factors and IS using two illustrative and applied cases and (2) outline practical considerations for human factors-based strategies to identify contextual factors that influence intervention adoption, implementation, and maintenance dimensions of the RE-AIM framework. This article expands on recent research that developed user- and human-centered design strategies for IS scientists to use. However, defining the complementary relationship between IS and human factors is a necessary and valuable step in maximizing the effectiveness of IS to transform healthcare. While IS can complement practitioners' identification of intervention adaptations, human interaction is a process in the work system often overlooked throughout implementation. Further work is needed to address the influence that organizational endorsement and trust have on intervention adaptations and their translation into the work system.
Introduction
Billions of tax dollars are spent on health services research annually (1), but the adoption and maintenance of evidence-based interventions lag (2). Issues with the uptake of an intervention are noted throughout the history of medicine (3). Given this lag in translation and uptake, solely determining the effectiveness of a clinical innovation is not sufficient to ensure its routine use but addressing the challenges of implementing an intervention could bridge this gap (3). In the late 1990s and early 2000s, implementation science (IS) developed as a discipline with methods for testing the integration of interventions in practice settings (4). While the evidence of the effectiveness of an intervention does contribute to some adoption rates, mediating contextual issues, such as different disciplines, appropriate outcomes, and usability of the intervention itself, are also highly influential (5).
According to the International Ergonomics Association, human factors developed during the 1940s and is a “scientific discipline concerned with the understanding of interactions among humans and other elements of a system, and the profession that applies theory, principles, data, and methods to design in order to optimize human well-being and overall system performance” (6). Typically, the study of human factors takes place in high-risk work settings, such as aviation or nuclear power; however, over the last two decades, human factors have become further integrated into the delivery of healthcare to reduce errors and improve efficiency (7). Simply stated, the basic tenets of human factors are: (1) that the system influences how individuals interact within it, (2) that there are experimentally tested and consistent findings demonstrating that humans have inherent capabilities and limitations, and (3) that the design of a work system can account for these capabilities and limitations to support human performance (8).
The tenets of human factors complement those of IS and could further facilitate practical applications for IS interventions (9). IS has methods to understand the intervention, the implementation strategy, and the outcomes of interest (10). A large body of literature, ranging from human-computer interactions to mental health services, suggests the human-centeredness of interventions and the design of the work system also heavily influence translation (11–14). If humans do not perform to an expected standard, it is likely that the failure stems from a mismatch between the system and human capabilities to function within that system (15–18).
It is possible that gaps in translation, specifically implementation, adoption, and maintenance, are related to the discordance between the intervention of interest, the design of the “work” or intervention of interest, implementation strategy, and human capabilities (19). Applying this perspective to IS in both health and healthcare, the human-centeredness of the design of interventions (based on understanding the capabilities of the end users) could heavily influence their translation (11, 12). The aim of this paper is to use part of the reach, effectiveness, adoption, implementation, and maintenance (RE-AIM) framework to outline where human factors strategies can complement the translational process (20–23). Specifically, this paper will focus on applications of human factors methodology and principles to improve adoption, implementation, and maintenance activities. To this end, the authors leverage the recent work of members of the authorship team (MJ, SHP) in infection prevention for illustrative purposes.
Based on findings from the field of human factors and practical considerations for the dimensions of the RE-AIM framework, the authors suggest an opportunity for integrating methods where applicable in the translational process. In this article, authors strategically chose two case studies to elucidate the interactivity of human factors and IS: (1) the complexity of hand sanitizing practices in the context of outpatient dialysis and (2) how human factors practices contributed to the development of ergonomic personal protective equipment (PPE) (face shields) during the COVID-19 pandemic response. Each case study offers a complex IS issue, explored through the lens of human factors. Although both cases are related to infection prevention the goal is to provide insight beyond this issue, to better understanding how implementation is impacted by work system design. In the discussion, the authors will categorize human factors strategies, according to the adoption, implementation, and maintenance dimensions of the RE-AIM framework.
Case study #1: considering human factors in the design of hand sanitizing stations in outpatient dialysis clinics
Patients with chronic kidney disease are particularly vulnerable to infections, and infections are the second leading cause of death in outpatient dialysis patients (24, 25). When receiving dialysis in an outpatient facility, patients are susceptible to infection because their personal dialysis connection site (either catheter or fistula/graft) is exposed during their dialysis procedure. Interventions such as appropriate hand hygiene and specific wound cleaning techniques have been established as a protection against infection (26). However, infections in these settings remain, even though a best practice for prevention is well established (26).
Members of the authorship team (MJ, SHP) used a macroergonomic approach in inpatient dialysis to better understand the human factors contributions to non-adherence to infection prevention evidence. For the purposes of this article, the authors will focus on one evidence-based best practice, hand sanitizing, and how the design of the system impacted implementation. An in-depth description of the overall methods and analysis can be found elsewhere (27). The Systems Engineering Initiative for Patient Safety (SEIPS) model was used to identify “work system inputs, care processes, and their influence on outcomes related to the patient and provider” in inpatient dialysis clinics (28, 29). The study identified factors related to the individual providers (e.g., the impact of disruptions on cognitive processes), the physical layout of the space, the technology and tools, and the organization (e.g., scheduling) were related to whether hand sanitizing was implemented properly.
There was wide variation in facility layout, with focus group feedback indicating that the location of hand sanitizing stations was often inconvenient for the work processes. In observations, individuals would go outside of normal walking paths to use hand sanitizing stations. Interruptions and alarms were frequent, occurring at a rate of 19% and 50.6% of all patient encounters respectively. Interruptions frequently resulted in additional hand sanitizing needs, as they were often caused by the machine and had to be silenced by physically touching an unclean surface. These findings illustrate how the design of the work system is impacting the action of engaging in a best practice (i.e., hand sanitizing).
Patient scheduling was observed to be rigidly timed, and limited flexibility in turnover time was observed at multiple centers. Although intervening events such as patient transportation delays, treatment interruptions for patients' needs, difficulty with needle insertion or delayed clotting were routinely observed, extra time was not routinely allotted for such occurrences. Dialysis connection and disconnection activities often overlapped. While there is not a direct correlation to hand hygiene, the context of the work is influencing how individuals engage with hand sanitizing stations.
This is an example of how successful implementation of an established intervention (i.e., hand sanitizing to prevent infection) is entangled with the design of the work system, and the human factors of the individual workers (e.g., forgetting or making mistakes when rushing or multitasking) within the work system. Designing the implementation of hand sanitizing stations to match the human capabilities and limitations may help facilitate adoption.
Case study #2: inclusion of human factors in the design and implementation of face shields during COVID-19
During the COVID-19 pandemic, healthcare supply chains experienced a shortage of medical equipment. An Emergency Use Authorization allowed frontline staff to wear improvised PPE to protect themselves from contact with bodily fluids during patient care (30). In the early phases of the pandemic, while there was significant concern over the contagious nature of SarsCoV-2 (the virus that causes COVID-19), face shields were recommended (31, 32).
The benefits of properly wearing face shields are well-known (33); however, uncomfortable, or poorly designed equipment can lead to staff non-compliance. This issue is critical to resolve for both staff safety and to help limit cross contamination. To better understand why an individual might be non-compliant with face shielding best practices, members of the authorship team (MJ, SHP) conducted an iterative design process with frontline providers and human factors experts. By contrast to the previously presented case study, this study was focused only on individuals and the context for face shielding, not on a broad macroergonomic perspective. MJ, SHP, and others attempted to use human factors principles, particularly around hardware usability, and user feedback to drive the study.
Key elements for design were identified from 1,648 survey responses such as the ability to adjust tension, anti-fogging, ventilation, and durability (34). A 3-phase iterative, randomized trial was then conducted with frontline providers. To measure the success of the design iterations, Kurtz et al. (2022) conducted a repeat survey after each phase, identifying common issues. The final design was able to meet the design criteria and limit or eliminate the common issues (see Figure 1 in reference 34).
This is an example of how the implementation of a best practice that benefits frontline providers as well as patients, can potentially be augmented by good design at the individual level. Where the previous example examined the broader work system contributions to implementation, this example illustrates individual requirements for implementing an evidence-based practice (i.e., wearing a face shield to prevent infection).
Discussion
These two case studies illustrate the benefit of integrating human factors principles into intervention design and are applicable to the implementation of other evidence-based practices. Identifying linkages between the principles, tools, and methods of both human factors and IS may improve adoption, implementation, and maintenance of evidence-based practices like hand sanitizing in outpatient dialysis clinics and wearing face shields in hospital departments. Notably, the authorship team has expertise in human factors and IS, but do not claim to be experts in infection prevention. In future investigations, the goal is to use both disciplines to maximize human-centeredness and uptake of interventions, given the interdependent contextual factors and human capabilities (21, 23).
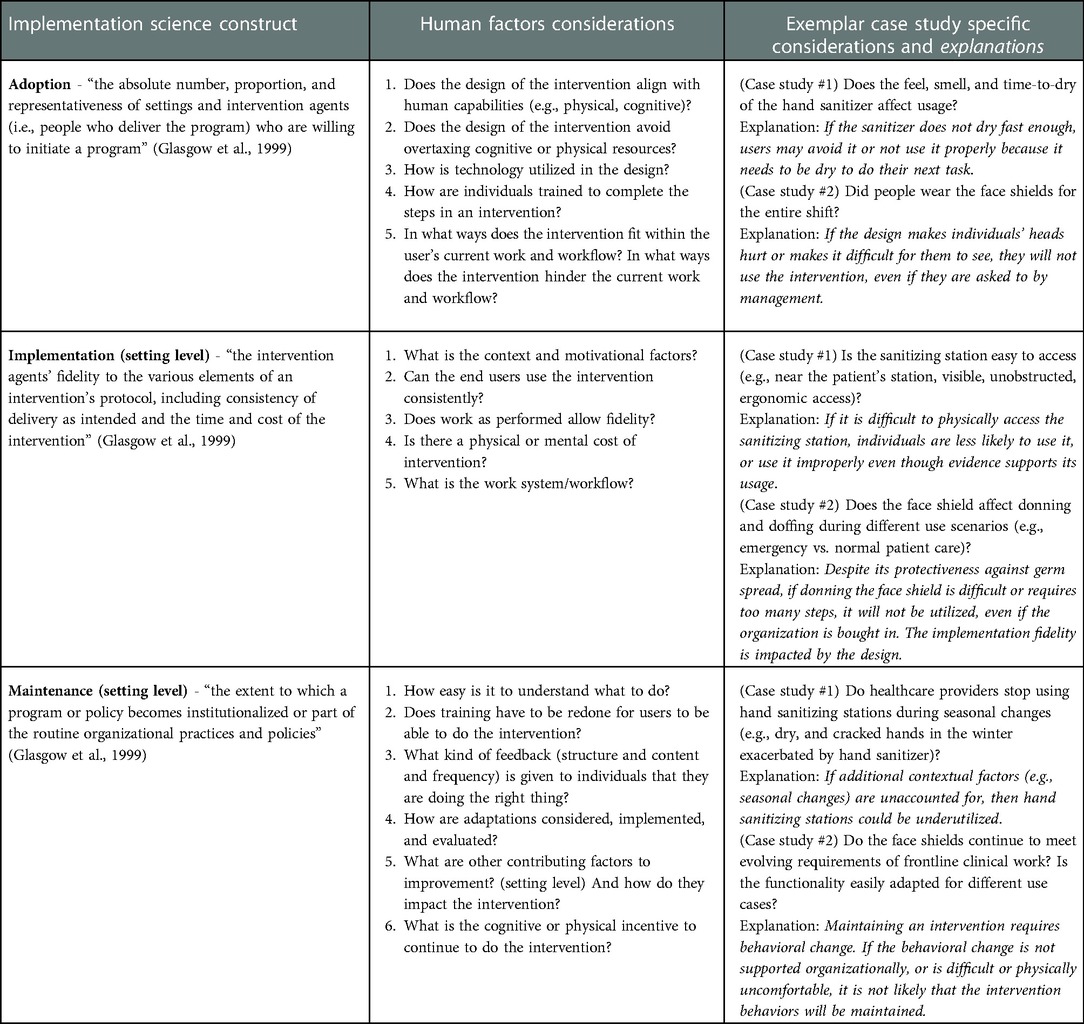
To further illustrate the associations between human factors and IS, the authors use the three dimensions of the RE-AIM framework that are associated with IS outcomes of staff and setting levels: adoption, implementation, and maintenance; then further articulate the human factors considerations for each construct with the two exemplar case studies (Table 1).
This work is a novel contribution to the IS literature and expands on recent efforts to identify human-centered implementation strategies (11, 35–37). Researchers and practitioners may find some strategies more helpful than others including task analysis, co-creation sessions, workflow analysis, and iterative prototyping (11, 35, 36). The design of an intervention, including the structure of delivery, hardware or software that can facilitate delivery, and training for target populations (care providers and patients/clients), is highly influential to how and whether and for how long the interventions are adopted and whether the setting's infrastructure can maintain them. Ultimately, the design of both the intervention and the work system are very likely to impact translation as well as implementation of an intervention.
The case studies have integrated both observations of normal work (i.e., hand sanitizing) to develop interventions, and a near real-time iterative process for integrating feedback (i.e., designing a face shield). Documentation of the iterative process is helpful to others that are attempting to implement an intervention in their own setting. From some of the authors' experience (STJ, MJ, SHP), the method of gathering iterative feedback is domain agnostic and ultimately translatable to other clinical settings, whereas the exact findings are contextual and often highly local. Information gathered in real-time informs the perspective of work as performed realistically, providing insight into how an intervention might be integrated. Questions relevant to adoption, (e.g., does the design of the intervention align with human capabilities? How do you avoid overtaxing physical or cognitive resources? Table 1), can address contextual factors that would limit adoption of interventions like hand sanitizing stations and face shields in high-risk work environments. For example, the real-time information gathering revealed that a hand sanitizer which does not dry quickly or has an uncomfortable texture (e.g., gritty, slippery, etc.) may limit uptake. Similarly, face shield uptake is dependent on the ability of the device to fit seamlessly within normal work duties and certainly cannot cause physical discomfort and should not make performing job functions more difficult.
Contextual factors influence every aspect of implementation. Systematically identifying contextual issues, including human performance issues, results in a better intervention design, and a higher likelihood of uptake (11, 35, 36, 38, 39). The field of human factors has much to offer on this point. To facilitate use in IS, the authors developed a list of implementation questions (Table 1). In these examples, the relevant implementation questions are centered around the consistent use of the intervention and whether work as performed allows for fidelity to the intervention. For example, an important contextual issue to consider while implementing the sanitizing stations is whether they are easy to access (e.g., accessible, visible, unobstructed, etc.). Logically, if a sanitizing station is difficult to access, then individuals may be less likely to use it. This conceptualization extends to donning and doffing of face shields: does the poor design of face shields interfere with consistent use of the intervention? If so, the design of an intuitive and ergonomic face shield becomes imperative because an individual is less likely to wear a face shield if it is cumbersome and poorly designed.
Stakeholders are critical at all phases of both human factors and IS (39–41). In human factors, the primary stakeholders of concern are frontline users of a product, device, or process. Including the frontline users in research discussions elevates the feedback from the individuals who know what may or may not be successful for their daily work. Frontline workers, otherwise, the end-users, can help researchers and implementation science practitioners understand the workflow in a particular setting. For example, including frontline users in the layout of hand sanitizing stations could possibly increase uptake and buy-in. A frontline user can identify the (1) critical times hand sanitizing must be performed, (2) paths in the workflow that do not burden task completion, and (3) accessible locations. This idea extends beyond hand sanitizing and face shield donning and doffing but can be used to identify promising strategies for implementing an intervention at multiple points of human interaction in a work system. In IS, stakeholders are also often organizational leaders or other individuals. While these individuals are critical to the resources needed to develop and implement an intervention, they are not the actual “doers” of the activity, and therefore, may have complementary insight into the daily work of frontline staff. A dichotomy stating that human factors consider frontline users and IS does not or IS considers organizational stakeholders and human factors does not, would be false. Each discipline is beneficial to the other in terms of designing for implementation success.
Conclusion
In this paper, the authors suggest that incorporating strategies from a human factor's perspective is a minor but pivotal shift within an implementation study. As illustrated in the two applied case studies, infection prevention in outpatient dialysis clinics and hospital departments that require face shields is more likely to succeed if human interactions within a work system are carefully considered in the design and implementation process. The authors attempted to articulate the linkages between IS and human factors and organize strategies according to the interdependent dimensions of the RE-AIM framework. The authors used two case studies as examples that required both an IS mindset and human factors design principles to promote adoption, implementation, and maintenance. It is the authors' belief that both disciplines are complementary of the other, and by integrating principles from each, the implementation of evidence-based practices like hand sanitizing and face shielding are strengthened.
In the field of IS, it is prudent to design an intervention with considerations for its use in the work system. Additionally, including insights from other fields, such as industrial and organizational psychology may prove useful when examining the interactions across levels of organizations. For example, the satisfaction and motivation of employees, and the extent to which the leadership endorses the intervention may affect its adoption and maintenance within the organization.
As demonstrated by the two applied case studies, the consideration of human factors complements the implementation process and likely improves use of an intervention. Consequently, the authors believe that the identification of human factors in an implementation study could substantially improve adoption, implementation, and maintenance.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author/s.
Author contributions
FE, VZ, STJ, MJ, SMH, and SHP have all contributed equally to this manuscript. All authors came up with the idea of the manuscript together. FE led the writing, while all authors contributed to additional writing and editing. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Davio K. Report: US medical health research spending on the rise, but for how long. AJMC Managed Markets Network, AJMC (2017).
2. Hull L, Goulding L, Khadjesari Z, Davis R, Healey A, Bakolis I, et al. Designing high-quality implementation research: development, application, feasibility and preliminary evaluation of the implementation science research development (ImpRes) tool and guide. Implement Sci. (2019) 14(1):80. doi: 10.1186/s13012-019-0897-z
3. Bauer MS, Kirchner J. Implementation science: what is it and why should I care? Psychiatry Res. (2020) 283:112376. doi: 10.1016/j.psychres.2019.04.025
4. Eccles MP, Mittman BS. Welcome to implementation science. Implementation Sci. (2006) 1:1. doi: 10.1186/1748-5908-1-1
5. Ferlie E, Fitzgerald L, Wood M, Hawkins C. The nonspread of innovations: the mediating role of professionals. Acad Manage J. (2005) 48(1):117–34. doi: 10.5465/amj.2005.15993150
6. Carayon P, Xie A, Kianfar S. Human factors and ergonomics as a patient safety practice. BMJ Qual Saf. (2014) 23(3):196–205. doi: 10.1136/bmjqs-2013-001812
7. Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, Hundt AS, Hoonakker P, Holden R, et al. Human factors systems approach to healthcare quality and patient safety. Appl Ergon. (2014) 45(1):14–25. doi: 10.1016/j.apergo.2013.04.023
8. Smith TJ. Core principles of human factors science. In: Proceedings of the human factors and ergonomics society annual meeting. Sage CA: Los Angeles, CA: SAGE Publications (1994). p. 536–40 (Vol. 38, No. 9). doi: 10.1177/154193129403800917
9. Rabin BA, Brownson RC, Haire-Joshu D, Kreuter MW, Weaver NL. A glossary for dissemination and implementation research in health. J Public Health Manag Pract. (2008) 14(2):117–23. doi: 10.1097/01.PHH.0000311888.06252.bb
10. Brownson RC, Colditz GA, Proctor EK. (Eds). Dissemination and implementation research in health: translating science to practice. New York, New York: Oxford University Press (2017). doi: 10.1093/oso/9780190683214.001.0001
11. Eisman AB, Kim B, Salloum RG, Shuman CJ, Glasgow RE. Advancing rapid adaptation for urgent public health crises: using implementation science to facilitate effective and efficient responses. Front Public Health. (2022) 10. doi: 10.3389/fpubh.2022.959567
12. Lyon AR, Brewer SK, Areán PA. Leveraging human-centered design to implement modern psychological science: return on an early investment. Am Psychol. (2020) 75(8):1067–79. doi: 10.1037/amp0000652
13. Norman DA, Draper SW. User centered system design: new perspectives on human-computer interaction. Hillsdale, New Jersey: Lawrence Erlbaum Associates, Inc. (1986). ISBN-10: 0898598729.
14. Wheelock A, Bechtel C, Leff B. Human-centered design and trust in medicine. JAMA. (2020) 324(23):2369–70. doi: 10.1001/jama.2020.21080
15. Carayon PASH, Hundt AS, Karsh BT, Gurses AP, Alvarado CJ, Smith M, et al. Work system design for patient safety: the SEIPS model. BMJ Qual Saf. (2006) 15(suppl 1):i50–8. doi: 10.1136/qshc.2005.015842
16. Reason J. Human error. Cambridge: Cambridge University Press (1990). doi: 10.1017/CBO9781139062367
17. Shappell S, Wiegmann D. A methodology for assessing safety programs targeting human error in aviation. Int J Aviat Psychol. (2009) 19(3):252–69. doi: 10.1080/10508410902983904
18. Xie A, Carayon P. A systematic review of human factors and ergonomics (HFE)-based healthcare system redesign for quality of care and patient safety. Ergonomics. (2015) 58(1):33–49. doi: 10.1080/00140139.2014.959070
19. McCreight MS, Rabin BA, Glasgow RE, Ayele RA, Leonard CA, Gilmartin HM, et al. Using the practical, robust implementation and sustainability model (PRISM) to qualitatively assess multilevel contextual factors to help plan, implement, evaluate, and disseminate health services programs. Transl Behav Med. (2019) 9(6):1002–11. doi: 10.1093/tbm/ibz085
20. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. (1999) 89(9):1322–7. doi: 10.2105/ajph.89.9.1322
21. Glasgow RE, Harden SM, Gaglio B, Rabin B, Smith ML, Porter GC, et al. RE-AIM planning and evaluation framework: adapting to new science and practice with a 20-year review. Front Public Health. (2019) 7:64. doi: 10.3389/fpubh.2019.00064
22. RE-AIM. Improving public health relevance and population impact. (2022). Available at: https://re-aim.org/ (Accessed June 11, 2022).
23. Holtrop JS, Estabrooks PA, Gaglio B, Harden SM, Kessler RS, King DK, et al. Understanding and applying the RE-AIM framework: clarifications and resources. J Clin Trans Sci. (2021) 5(1):E126. doi: 10.1017/cts.2021.789
24. Fisher M, Golestaneh L, Allon M, Abreo K, Mokrzycki MH. Prevention of bloodstream infections in patients undergoing hemodialysis. Clin J Am Soc Nephrol. (2020) 15(1):132–51. doi: 10.2215/CJN.06820619
25. Johansen KL, Gilbertson DT, Wetmore JB, Peng Y, Liu J, Weinhandl ED. Catheter-Associated bloodstream infections among patients on hemodialysis: progress before and during the COVID-19 pandemic. Clin J Am Soc Nephrol. (2022) 17(3):429–33. doi: 10.2215/CJN.11360821
26. Centers for Disease Control and Prevention (CDC). Dialysis safety: guidelines, recommendations and resources. Centers for Disease Control and Prevention (2017). Available at: https://www.cdc.gov/dialysis/guidelines/index.html (Accessed May 20, 2022).
27. Parker SH, Jesso MN, Wolf LD, Leigh KA, Booth S, Gualandi N, et al. A systems approach to understanding infection prevention in outpatient hemodialysis centers: Understanding the human factors contribution (in prep).
28. Wooldridge AR, Carayon P, Hundt AS, Hoonakker PL. SEIPS-based process modeling in primary care. Appl Ergon. (2017) 60:240–54. doi: 10.1016/j.apergo.2016.11.010
29. Holden RJ, Carayon P, Gurses AP, Hoonakker P, Hundt AS, Ozok AA, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics. (2013) 56(11):1669–86. doi: 10.1080/00140139.2013.838643
30. U.S. Food & Drug Administration. Personal protective equipment EUAs. U.S. Food & Drug Administration. Available at: https://www.fda.gov/medical-devices/coronavirus-disease-2019-covid-19-emergency-use-authorizations-medical-devices/personal-protective-equipment-euas Updated March 7, 2022. (Accessed May 20, 2022).
31. Centers for Disease Control and Prevention (CDC). Infection control guidance. Centers for Disease Control and Prevention (2019). Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html Updated February 2, 2022. (Accessed May 20, 2022).
32. World Health Organization. Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages: interim guidance, 6 April 2020 (No. WHO/2019-nCov/IPC_PPE_use/2020.3). World Health Organization (2020).
33. Verbeek JH, Rajamaki B, Ijaz S, Sauni R, Toomey E, Blackwood B, et al. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst Rev. (2020) 4:CD011621. doi: 10.1002/14651858.CD011621.pub4
34. Kurtz CE, Peng Y, Jesso M, Sanghavi H, Kuehl DR, Parker SH. Using a human factors-centric approach to development and testing of a face shield designed for health care workers: a COVID-19 case study for process and outcomes. Am J Infect Control. (2022) 50(3):306–11. doi: 10.1016/j.ajic.2021.10.033
35. Dopp AR, Parisi KE, Munson SA, Lyon AR. A glossary of user-centered design strategies for implementation experts. Transl Behav Med. (2019) 9(6):1057–64. doi: 10.1093/tbm/iby119
36. Dopp AR, Parisi KE, Munson SA, Lyon AR. Aligning implementation and user-centered design strategies to enhance the impact of health services: results from a concept mapping study. Implement Sci Comm. (2020) 1(1):1–13. doi: 10.1186/s43058-020-00020-w
37. Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the expert recommendations for implementing change (ERIC) project. Implement Sci. (2015) 10(1):21. doi: 10.1186/s13012-015-0209-1
38. Barwick M, Dubrowski R, Damschroder L. Factors associated with effective implementation: research and practical implications. Implement Sci. (2020):81–100. doi: 10.1007/978-3-030-03874-8_4
39. Lyon AR, Koerner K. User-centered design for psychosocial intervention development and implementation. Clin Psychol Sci Pract (2016) 23(2):180. doi: 10.1111/cpsp.12154
Keywords: adoption, contextual factors, face shield, infection prevention, maintenance, re-aim, work system, adaptations
Citation: Edwards III GF, Zagarese V, Tulk Jesso S, Jesso M, Harden SM and Parker SH (2023) Designing healthcare for human use: Human factors and practical considerations for the translational process. Front.Health Serv. 2:981450. doi: 10.3389/frhs.2022.981450
Received: 29 June 2022; Accepted: 12 December 2022;
Published: 6 January 2023.
Edited by:
Marina McCreight, VA Eastern Colorado Health Care System, Veterans Health Administration, United StatesReviewed by:
Ashley M Hughes, University of Illinois at Chicago, United States© 2023 Edwards, Zagarese, Tulk Jesso, Jesso, Harden and Parker. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Franklin Edwards gfedward@vt.edu
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Implementation Science, a section of the journal Frontiers in Health Services
 G. Franklin Edwards III
G. Franklin Edwards III Vivian Zagarese2,†
Vivian Zagarese2,†  Stephanie Tulk Jesso
Stephanie Tulk Jesso Samantha M. Harden
Samantha M. Harden Sarah Henrickson Parker
Sarah Henrickson Parker