Finding Goal Focus With People With Severe Traumatic Brain Injury in a Person-Centered Multi-Component Community Connection Program (M-ComConnect)
- 1Living With Disability Research Centre, La Trobe University, Melbourne, VIC, Australia
- 2The Summer Foundation, Melbourne, VIC, Australia
Background and Objectives: Loss of social connections in the community is a common consequence of severe traumatic brain injury (TBI), resulting in reduced well-being and quality of life. M-ComConnect is an individualized multi-component community connection intervention with the key objectives of increasing social activity, developing social relationships, and supporting community participation following severe TBI. As part of the M-ComConnect approach, semi-structured initial interviews were conducted to develop a holistic understanding of each participant and their goal focus for the project. In this paper we describe how clinicians worked with participants to identify a desired community-based social activity in which to participate.
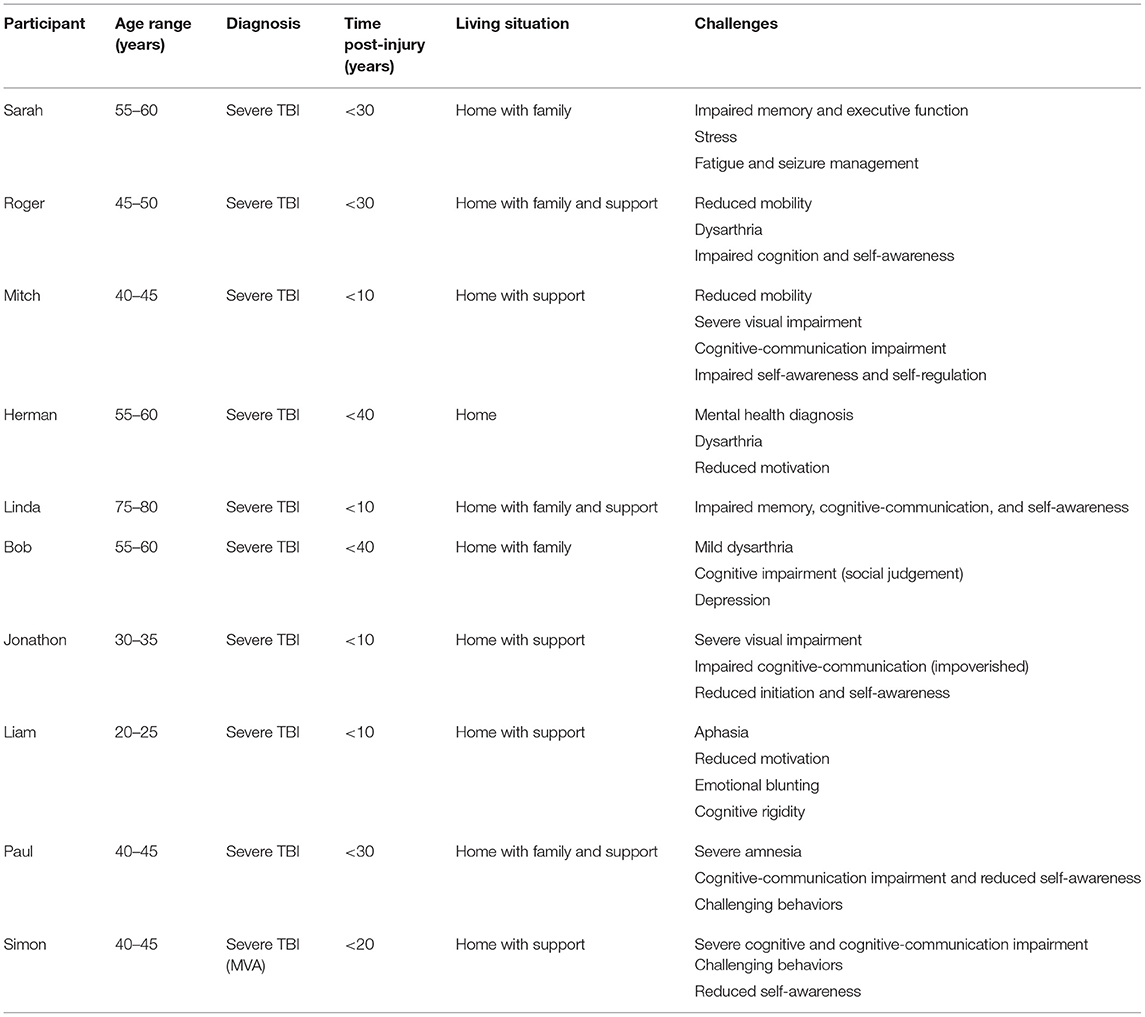
Method: Transcripts of initial interviews between participant and clinician were analyzed using the phases of reflexive thematic analysis developed by Braun and Clarke. Participants were ten individuals aged between 24 and 75 with severe TBI. All were living in the community and reported reduced social connections since their TBI. The aim of the analysis was to evaluate the skills and strategies used by clinicians in their interactions with participants to derive goal focus for the program.
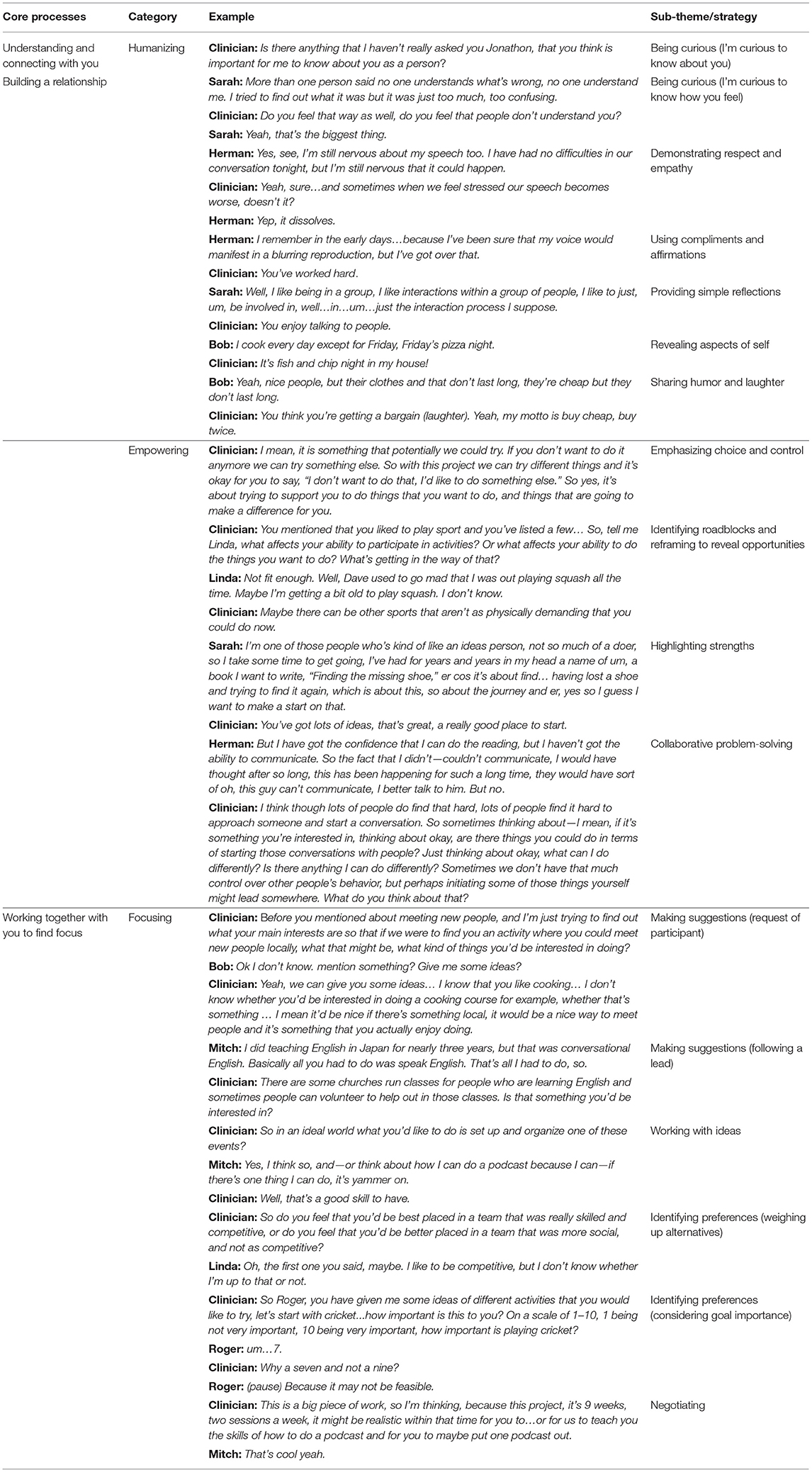
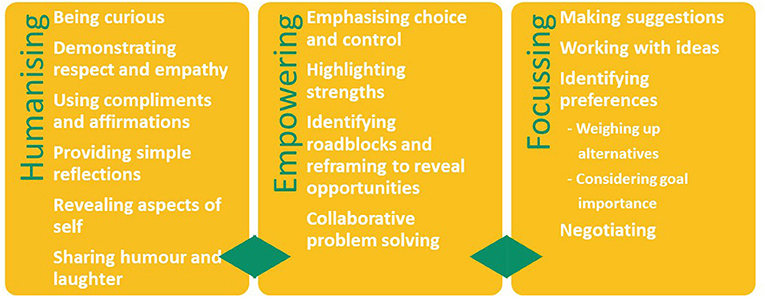
Results: Thematic analysis of initial interview data revealed three main categories and fourteen sub-categories of clinical strategies. These were: (1) Humanizing (curiosity; demonstrating respect and empathy; providing compliments and affirmations; simple reflections; revealing aspects of self; and humor and laughter), (2) Empowering (emphasizing choice and control; highlighting strengths; identifying roadblocks and reframing to reveal opportunities; and collaborative problem solving), and (3) Focusing (making suggestions; identifying preferences; working with ideas; and negotiating). These strategies aligned with the program's relational approach and supported the core processes of the goal-focussing framework, namely understanding and connecting with you, building a relationship, and working together with you to find focus.
Conclusion: The goal-focusing framework and clinical strategies outlined provide guidance for clinicians working with people with TBI in the community and is a promising way to engage clients when focusing on individualized social activity-based goals.
Introduction
The impact of traumatic brain injury (TBI) on a person's ability to maintain social connections and participate meaningfully in the community is well-documented (1–6). Despite the importance of leisure and recreational activity as a means of connecting with others, people with TBI are consistently found to have diminished social activity levels after injury (6, 7). Given the strong evidence linking social participation and social connection to health, wellbeing and quality of life (8, 9), it follows that supporting people with TBI to participate in social leisure and recreational activities is a priority for clinicians working in community rehabilitation settings. Identifying activities and interventions that reflect and support an individual's interests and preferences and are grounded in their sense of self demands an understanding of their unique circumstances (8).
How we view ourselves affects our relationship with the world. In turn, our life experiences and interactions with others impact on how we view ourselves (10). William James famously coined the term “social self” in describing the way an individual conceptualizes the reaction of others to him or her (11). According to the symbolic interactionist perspective, the individual and the context in which they exist are inseparable and mutually constructed through the unfolding of social interactions (10). This dynamic process has far-reaching consequences for individuals after TBI, whose sense of self undergoes profound change in accordance with their altered abilities and roles. Without congruence between the rehabilitation program and one's sense of self, “rehabilitation efforts…are likely to be at best ineffective and at worst, counter-productive…” [(12), p. 715], particularly when facing the challenge of establishing and maintaining social connections after TBI. Understanding an individual's concept of themselves can therefore be viewed as an essential step in the design of effective person-centered goals and interventions following TBI.
Douglas (8) proposed a “describe, strive, achieve, and appraise” therapy framework based on the results of a qualitative exploration into how 20 adults with severe to very severe TBI conceptualized themselves several years after injury. The framework places therapy in the context of self: “who I am,” encompassing attributes (describe) and goals (strive), and “how I feel about myself,” involving outcomes (achieve) and attitude (appraise). Accordingly, the characteristics or attributes of the individual from that individual's perspective must be understood to collaboratively formulate self-relevant goals to guide the work of therapy. The multi-component community connection program (M-ComConnect) developed from Douglas' previous research is an individualized intervention program for people with severe TBI (13). M-ComConnect was specifically developed to meet the needs of adults with severe brain injury and complex needs who are socially isolated and participate in minimal community activity. It is designed around 3 personal domains (components): functioning, relationships and social connections, and community participation.
1. Functioning focusses on the person's skills and behaviors as they participate in their community.
2. Relationships and social connections emphasizes all types of connections relevant to the individual including those with family, friends, and members of the community more generally (e.g., service providers, co-participants in community-based group activities, and programs)
3. Community participation involves becoming an active participant in a community based interactive activity (i.e., with other people) in which the individual is interested and wants to participate.
In a recently completed feasibility trial, M-ComConnect was delivered on twenty-five occasions over three phases in varying community contexts with adults with severe TBI. Statistically significant changes post-intervention consistent with large positive effects were demonstrated on core measures of quality of life, wellbeing and community integration and maintained at 3-months post-intervention (13).
At the core of the M-ComConnect approach was the partnership and collaboration between client and clinician, and the recognition that participants' unique input and self-knowledge were fundamental to the process of identifying, participating in and succeeding in their chosen activity. M-ComConnect's person-centered approach was consistent with elements of person-centered frameworks described in the literature. Jesus et al. (14) for example, provide a model of thinking about how rehabilitation services can be delivered with as opposed to for the individual. Most pertinent to this paper are the five attributes identified within the person-professional dyad: (i) respectful of and tailored to the person—beyond individualized interventions for the patient, (ii) reflexive and adaptive to the situation at hand—not script based, (iii) nurtures a supportive relationship—compassionate, trustful, and caring, (iv) focused on meaning, hope, and strength—beyond addressing deficits, and (v) collaborative, empowering, and enabling—co-constructed rehabilitation. McCormack and McCance's (15) Person-centered Practice Framework can be applied to a wide range of healthcare contexts and disciplines and comprises four domains: (1) prerequisites (attributes of the staff), (2) the practice environment (the context in which healthcare is experienced), (3) the person-centered process (focusing on ways of engaging that create connections between persons), and (4) the outcome (the result of effective person-centered practice). For clinicians to work in a way that centralizes clients' perspectives and self-concepts, they must begin with a sound theoretical understanding of person-centered care and an awareness of their own approach and behaviors that shape the interactions.
The person-professional relationship, also known as the therapeutic or working alliance, has received considerable attention in the brain injury literature (16–22). Therapeutic working alliance has historically been defined as comprising three key elements: (a) the interpersonal bond between the therapist and the client; (b) agreement on the tasks to be completed in therapy; and (c) agreement on the goals for therapy [(23, 24); in (25)]. In a qualitative exploration of how allied health clinicians established and maintained working alliance with people with stroke-related communication impairment, interpersonal processes coalesced under the following themes: enabling interaction, being responsive, building relationship capital, and building credibility (26). Relational practices such as everyday conversations and the use of humor were also seen to be important in building therapeutic alliance. With regards to setting goals for therapy, Prescott et al. (27) identified client-centeredness and collaboration as the most common guiding principles. Other authors have highlighted key ingredients such as communication (28), active and reflective listening (29, 30), and the practitioner's self-awareness (30). Bright et al. (31) further highlighted how engagement in goal-setting is a co-constructed and dynamic process between the client and practitioner.
Setting goals that are truly collaborative and co-constructed with people with TBI can be complex and challenging. Issues such as lack of motivation, reduced self-awareness and cognitive impairment may impact on a person's ability to set realistic goals (32–34). Severe cognitive impairments may impact on an individual's ability to generate goals or indeed conceptualize what Markus and Narius (35) termed “possible selves.” Perhaps due to these challenges, research into best practice regarding goal-setting or goal-planning approaches for people with acquired brain injury (ABI) in clinical practice lacks consensus and consistency (14, 27, 36). A range of goal-setting frameworks have been described in the literature. Ylvisaker et al. (12), for example, proposed an identity-oriented goal setting approach, utilizing metaphoric identity mapping to develop personally meaningful goals. Others have looked at the efficacy of specific tools, such as the Values in Action Inventory of Strengths (VIA-IS) that links goals to personal values (37). Prescott et al. (27) conducted a systematic scoping review examining goal-setting approaches specific to people of working age with ABI. They found that formal goal setting approaches such as Goal Attainment Scaling (38) and the Canadian Occupational Performance Measure (39) were used frequently in research but <14% of the time in clinical practice. Following on from this research, Prescott et al. (36) developed a framework to explain how clinicians support community-dwelling clients to actively engage in goal-setting in routine practice. The framework incorporated three phases, including needs identification, goal operationalization, and intervention. Building rapport was considered a core strategy, and clients with self-awareness impairments benefitted from additional metacognitive strategies to participate in goal setting.
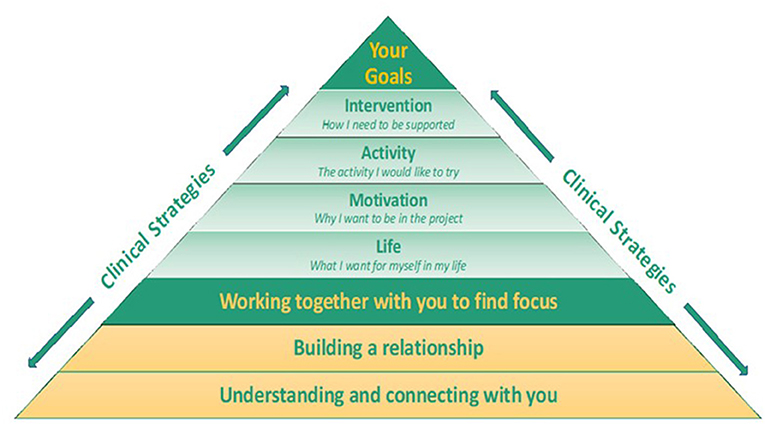
The M-ComConnect program goal-focusing framework was developed from a combination of theoretically driven rehabilitation constructs (8, 40) and evaluation of program outcomes (13). The framework consisted of three core processes deemed essential for finding goal focus. These were “understanding and connecting with you,” “building a relationship,” and “working together with you to find focus.” The program aimed to derive goal focus with participants across four domains: (1) life (what the person wants for themselves in their life), (2) motivation (what they wanted to achieve in the project), (3) activity (the activity they wanted to try), and (4) intervention (the supports they required to achieve their goals). These domains were based on processes identified within Douglas' (8) “describe, strive achieve, and appraise” framework that emerged from the conceptualizing self and maintaining social connection grounded theory model proposed by Douglas (8, 40).
In this paper, we aim to describe the skills and strategies used by clinicians to find social activity goal focus with people with severe TBI in the M-ComConnect program. Transcripts of initial interviews between participants and research clinicians provided the material from which key themes were derived.
Methods
Design
Phase one of the M-ComConnect study consisted of 10 single-case experimental design (SCED) studies (A-B-A with multiple probes), forming part of a larger study (n = 25). The program was evaluated using primary outcome measures customized for each individual, and standardized secondary outcome measures encompassing community integration, well-being, and quality of life.
Semi-structured interviews were conducted with participants prior to engaging in the program. This interview process aimed to build a sense of collaboration and partnership, to gather important information about the person, and to determine a desirable leisure/recreation activity. For participants with severe cognitive or communication impairment, family members, and/or support workers participated in the initial interview process.
Participants
Ten participants (eight males and two females) with severe TBI enrolled in phase one of the study (see Table 1). Mean age at enrolment in the project was 47.1 years (range 24–75 years) and mean time post injury was 17.5 years (range 2–36 years). Nine participants were living in their own home, either independently, with family or with high levels of support. One participant lived in specialized supported accommodation. Criteria for referral to the program were: (i) the person must have acquired a severe TBI (post traumatic amnesia > 14 days) and (ii) be experiencing challenges with community connection. The latter was defined as difficulty participating in social activities and getting to know others in the local area. Level of disability was indexed pre-intervention using the Care and Needs Scale (41). This ranged from level 1 (can live alone but needs intermittent contact) to level 7 (cannot be left alone). In order to protect the identity of participants, pseudonyms have been used throughout the manuscript.
Five clinicians including four speech pathologists and one neuropsychologist were involved in the initial interview process. The speech pathologists had between 7 and 25 years experience working with people with ABI in rehabilitation and community settings. The neuropsychologist had <1 year of experience.
Procedure
Approval to conduct the study and associated analyses were obtained from the university ethics committee. Participants were recruited through various channels including community seminars, community providers, relevant newsletters and word of mouth.
The study was explained, questions answered, and informed consent obtained in an initial meeting with participants. Initial interviews occurred either at participants' homes or in a community setting, and were audio recorded. Family members or support workers attended initial interview sessions for five participants. Questions were directed toward and answered by the participant where possible. Cognitive and communication impairments prevented only one participant (Simon) from engaging meaningfully in the interview process, and in this instance the interviewer interacted with the participant's mother and support worker, including the participant where possible.
A semi-structured interview approach provided guidance yet allowed participants to speak freely about topics of their choosing. Whilst key questions were pre-determined, the questioning style was flexible and non-formulaic. Each interview was therefore unique, with clinicians responding to the individual needs and communication styles of participants. Formal assessments and checklists were not used in the initial interview process. Information about abilities and challenges was provided by participants and gathered through clinical observation. For some, additional background information was provided by family members or treating allied health professionals.
The initial interview was conducted over two sessions for eight participants, and completed in one session for two participants. Eighteen initial interviews were recorded in total. Length of interviews varied from 60 to 120 minutes. Interview questions were broadly organized around gathering personal information (“Tell me about yourself/your story”); their experience of living with TBI (“Tell me a bit about your brain injury and how it's affected you; what sort of things do you find challenging?”); interests and attributes (“What sort of things do you enjoy doing?” “How would you describe yourself in three words?” “How would others describe you?”); participants' social and psychological being (“Tell me about the people in your life”; “How have you been feeling in the last 3 months?”); how they imagined their future (“What's missing from your life right now?”; “Is there anything that you are not doing that you would like to be doing?”), and questions relating to community connection (“How do you like to exist within your community?”; “What does being connected to your community mean to you?”).
Following completion of the intervention, follow-up interviews were conducted with participants to gain an understanding of their experiences. These follow-up interviews were conducted by a research clinician who was not involved in the delivery of the M-ComConnect program for that individual. Nine participants participated in post-intervention interviews independently and four support workers were interviewed separately.
Analytic Strategy
Braun and Clarke's (42, 43) six-phase analysis process was used to identify emergent themes. This process followed the six recommended steps of coding and analysis, including: (i) familiarization with the data, (ii) coding, (iii) generating initial themes, (iv) reviewing themes, (v) defining and naming themes, and (vi) writing up (42, 43).
NVivo software was used to support open and focused coding of themes. Coding involved selection and labeling of small to large segments of text considered relevant to understanding the process of finding goal focus for people with severe TBI in the M-ComConnect program. As the general aims of the interview process were pre-established (to get to know the person, to build a relationship and establish a social activity that the person wanted to participate in) the clinician's approach and interview questions were naturally directed to this focus.
Interviews were coded independently by the first and second author and a high degree of similarity of text extracts and coding occurred. As the data from each successive interview were compared and contrasted in an iterative process, codes became increasingly focused. Further analysis of coded data resulted in expansion of some codes. For example “curiosity” contained quotes that were sub-divided into “I'm curious to know about you” and “I'm curious to know how you think.” Other codes were merged, for example, quotes in themes of “identifying roadblocks” and “reframing to reveal opportunities” were combined, as roadblocks (perceived barriers) usually occurred in longer conversations focused on identifying a solution. Sub-themes were discussed, combined and re-named until consensus was achieved between all three authors on final themes and subthemes.
Following this agreement, themes were assigned to one of three emergent categories depending on their function: humanizing, empowering or focusing strategies. Humanizing strategies supported relationship building and recognition of the uniqueness of the person (44), empowering strategies promoted confidence and autonomy, and focusing strategies supported themes that honed conversations toward goal focus.
Relationship Between Themes
Overlap of themes across categories was evident. For example, quotes within “providing compliments and affirmation” (humanizing strategy) overlapped with “highlighting strengths” (empowering strategy). Similarly, “making suggestions” (focusing strategies) may also have been coded as “being curious” (humanizing strategy). The primary function of the quote was taken into consideration when coding. For example, in the section of text below the question is followed by a suggestion and was therefore coded as “making a suggestion” rather than “being curious.”
Clinician: Is there anything else that you'd like to do?
Roger: Such as?
Clinician: Singing at church…being in a choir at church.
Quality
Questions regarding quality of the analytic approach were applied to interpretations of the data throughout the analysis process (43). The coding approach was collaborative and reflexive. In recognition of the role of the researcher as a participant in the research process, the authors/researchers acknowledged the influence of their own expectations and experience as clinicians who had worked for many years with people with TBI. Therefore, careful attention was paid to ensure that this experience did not unduly color the data analysis process. Further, memo writing was used extensively to provide an audit trail throughout the research process from data collection through to theme identification. In addition, first the codes, themes and then later the categories that resulted from data analysis were reviewed and discussed by the team to develop a richer more nuanced reading of the data. Where differences occurred, original transcripts of interviews, fieldnotes and coding memos were reviewed and the code, category or theme under consideration was discussed until consensus about meaning was reached. Memos were used to ensure that data analysis decisions were documented. Finally, core themes and categories were reviewed against the original transcripts to ensure that they maintained the voice of the participants and were anchored in the skills and strategies used by clinicians in their interactions with participants to derive goal focus for the program.
Relationship With the M-ComConnect Goal-Focusing Model
The relationship of the strategies to the M-ComConnect goal-focusing model was discussed by the three authors. The strategies validated and supported the three core processes (understanding and connecting with you, building a relationship, and working together with you to find focus).
Results
Table 2 illustrates the core processes, themes and sub-themes (strategies) that emerged from thematic analysis of the initial interviews with each participant. Excerpts from interviews are used to exemplify the nature and content of the interchange between the clinicians and participants that contributed to the analysis. Figure 1 outlines humanizing, empowering, and focusing strategy themes and sub-themes.
Clinical Strategies
Humanizing Strategies
Humanizing strategies aligned with M-ComConnect's relational approach and served both to promote an understanding of the person and build the relationship.
1. Curiosity allowed for genuine enquiry into the participants sense of self, their worlds, thoughts and feelings. Two sub-themes emerged: I'm curious to know about you, and I'm curious to know how you feel.
2. Demonstrating respect and empathy was evident throughout, particularly when participants spoke about their personal stories and challenges.
3. Providing compliments and affirmations was used to focus on strengths and served to make the participant feel validated and valued.
4. Simple reflections occurred frequently during conversations with all participants. Reflections demonstrated understanding of the person's thoughts and encouraged further exploration.
5. Revealing aspects of self acted to humanize the interaction, create an equal partnership and a bond. Self-disclosures were not highly personal and frequently overlapped with humor and laughter.
6. Humor and laughter were features of both the participants' and clinicians' contributions within the interview discourse. This reciprocity of humor served to build the interpersonal connection.
Empowering Strategies
Empowering strategies supported all three core processes by emphasizing to the person that the project was about them and their lives. Perceived barriers were discussed, and emphasis was placed on collaborative problem-solving to achieve the desired outcome.
1. Emphasizing choice and control. All participants were made aware that they were in control of decisions made in the project. Their control in decision making was both explicitly explained and evident in statements such as “It's up to you?” and “What do you think?”
2. Highlighting strengths was considered an empowering strategy and was also embedded within other humanizing, empowering and focusing strategies, for example, when “using compliments and affirmations.” Highlighting strengths was evident following statements where the participant questioned their own ability, or through direct questions such as “What's the thing that you are best at?”
3. Identifying roadblocks and reframing to reveal opportunities. Participants were specifically asked about barriers to participation. This provided an opportunity to identify perceived roadblocks and explore other potential opportunities.
4. Collaborative problem solving. When participants' beliefs potentially impacted on their ability to think forward and see a future self, the clinician challenged these beliefs gently and respectfully to engage the participant in conversations that supported collaborative solutions.
Focusing Strategies
The aim of understanding and connecting with the person and building a relationship was to derive goal focus for a social activity that was realistic within the context and timeframe of the project. A phase occurred in the interview process, that involved more focused conversations and questioning toward finding the participants' activity goal focus.
1. Making suggestions. Suggestions of activities were put forward by the clinician regardless of the participants' activity goal certainty i.e., whether they had no, one, or several ideas about activities. Suggestions of activities were either made following a lead from the individual or at the request of the participant.
2. Working with ideas. During the initial interview, all ideas put forward by participants were recognized as being valid and the clinician worked toward feasibility.
3. Identifying preferences. Throughout the interviews, participants gave information that indicated their preferences, for example Simon's mother said, “He likes concerts, we bought Lionel Richie tickets.” However, identifying preferences in this category related more specifically to honing in, with two sub-themes emerging, weighing up alternatives and assessing goal importance using a rating scale.
4. Negotiating involved firstly pinpointing the person's true preference (identifying preferences) followed by placing their preference within the context of what may be achievable in the timeframe of the project.
Informally, the intensity of focusing strategies was noted to vary across individual participants. For example, the focusing strategy “making suggestions” was particularly observable for participants with reduced ideas or cognitive inflexibility. For these participants, several activities were not only suggested but also trialed, allowing for further deepening of the process of “understanding and connecting with you” and ensuring that the chosen activity aligned with the person's sense of self. The focusing strategy “negotiating” was more often employed with participants who proposed multiple ideas, or ideas outside the realm of feasibility for the context and timeframe of the project. For participants who presented with greater negativity about their lives and challenges, identifying roadblocks and reframing to reveal opportunities, highlighting strengths and collaborative problem-solving featured more prominently.
Multi-Level Goal Focusing Framework
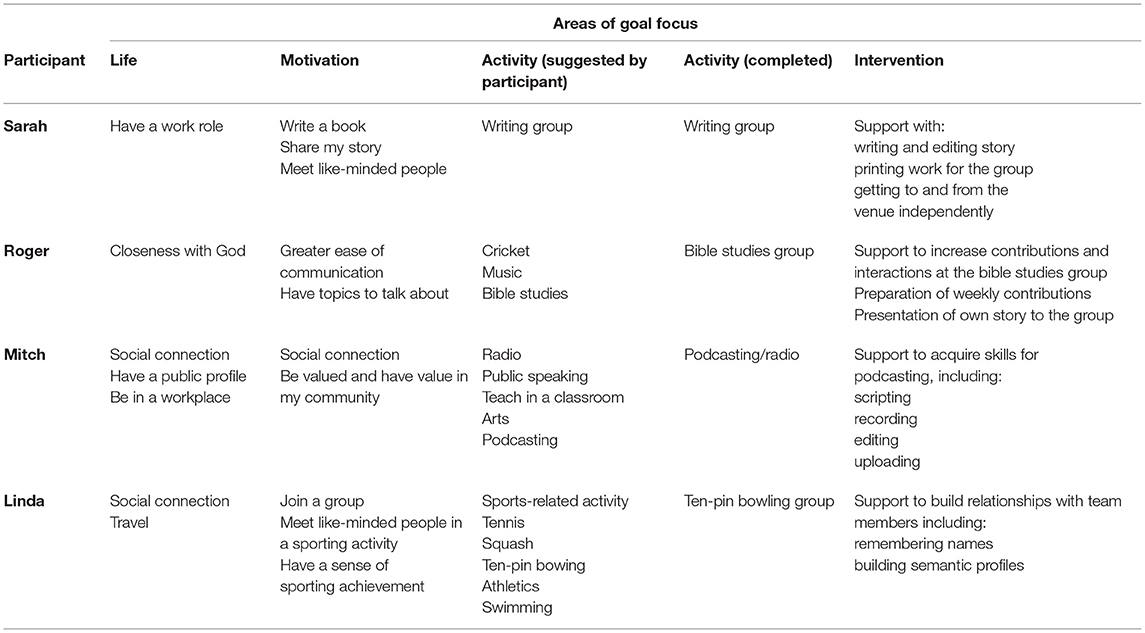
The M-ComConnect goal focusing framework incorporated multiple interrelated processes. The core processes understanding and connecting with you, building a relationship, and working together with you to find focus underpinned the framework (see Figure 2). The role of the clinician and use of clinical strategies were instrumental in the establishment of these processes that aimed to find social activity goal focus with the participant. The information gathering and relationship building that occurred during the initial interview process were fundamental to finding social recreation/leisure activities that were personally meaningful to the participant and aligned with their life goals (what's important for them in their lives) and their motivation goals (what they want to achieve by being in the project). Furthermore, the person's intervention goal focus (the supports they required to achieve their goals) were informed by these areas of goal foci (see Table 3 for examples of participants areas of goal foci). This resulted in participants engaging in social recreation/leisure activities that were personally meaningful to them and aligned with their concept of self across multiple levels.
Table 3 presents examples of participants' goal foci across life, motivation, activity, and intervention domains.
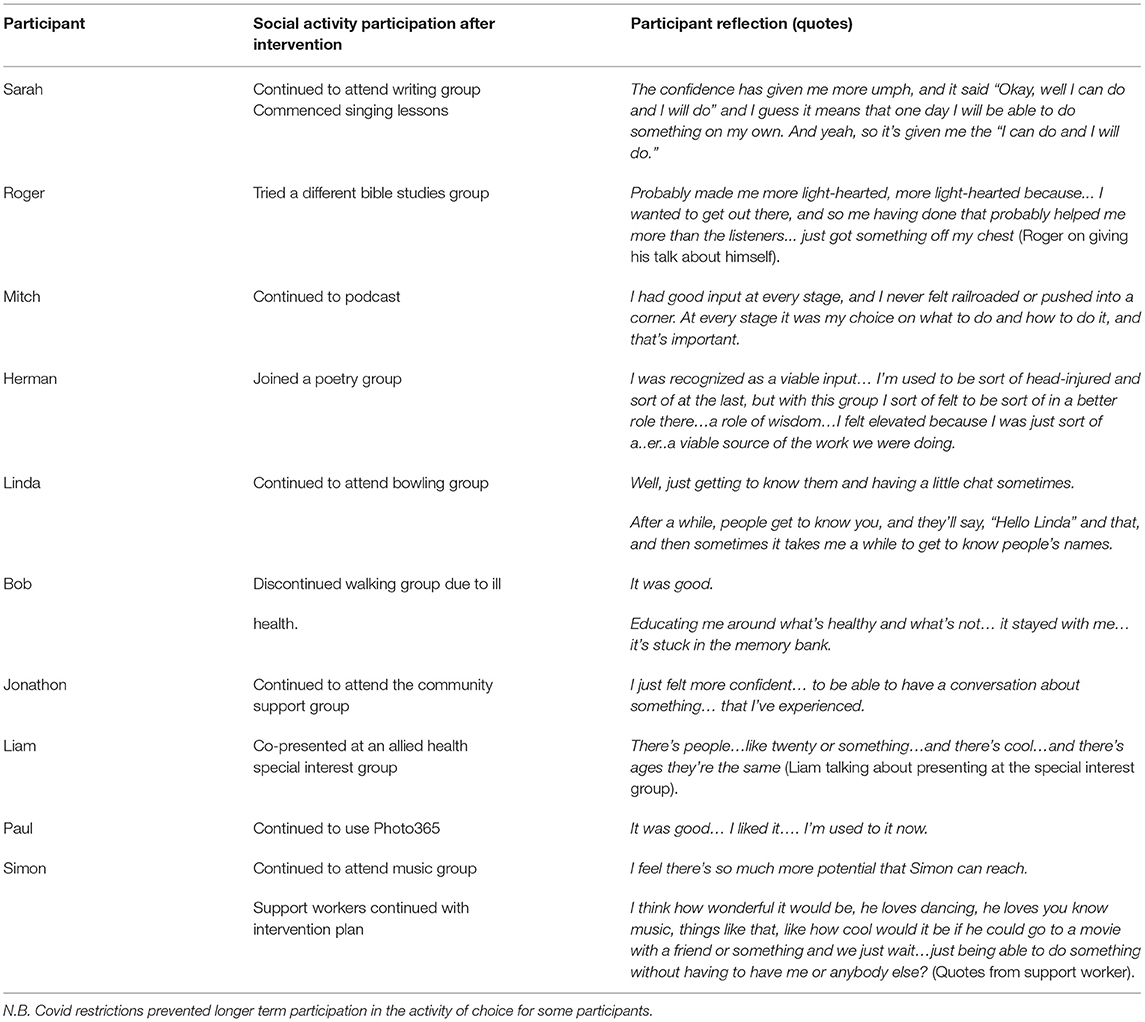
Finally, it is noteworthy that 9 of the 10 participants in phase one of the project continued to participate in community social activity following the conclusion of this phase. Six participants continued with their phase one social activity, three participants moved on to different social activities and one discontinued due to ill health. Table 4 presents the social participation outcomes for participants and illustrates their experience of the intervention through quotes from their post intervention interviews. These quotes reflect the range of outcomes reported by participants including increased confidence, having personal choice and control, being in a valued role, developing new knowledge and having opportunities to make friends.
Discussion
Many researchers, clinicians and people with TBI view community integration and social connection as the ultimate goal of rehabilitation (2, 45–48) and yet there is little research looking at how to find activities and interventions that support community integration. The overall aim of the M-ComConnect project was to support people with severe TBI to participate in social leisure/recreation activities that enhanced social connection and integration into their community. The aim of this paper was to analyze how social activity goal focus was derived with participants in the project by analyzing strategies used by clinicians in the initial interview process.
The semi-structured interview process allowed exploration of all aspects of the person's self-concept, their social worlds, interests, preferences, beliefs and so on. Information gathered resulted in an understanding about that person across multiple layers of goal foci: life (what the person wants in their life), motivation (what the person wants to achieve in the project), and activity goal focus (the activity they want to try.) Intervention goal focus (the supports they need to achieve their goals) was subsequently informed by these domains of goal foci. Thematic analysis of initial interview data revealed three main categories of clinical strategies: humanizing, empowering and focusing. These clinical strategies aligned with the program's relational approach and supported the goal-focusing framework's core processes: understanding and connecting with you, building a relationship, and working together with you to find focus. The social leisure/recreation activity and intervention goal foci that emerged were inherently aligned with motivational and life goals where possible. Goals were therefore not just personally relevant for the person in the context of the project, but within the context of their lives. It is proposed that this alignment across the four areas of goal foci contributed to the success of the program, with 90% of participants in phase one of the study continuing with their chosen activity or engaging in other extended social activity. Participants also recognized their positive experiences within the program as evidenced by comments made in their post-intervention interviews.
The clinical strategies that emerged (humanizing, empowering, and focusing) offer a unique insight into how we develop connections and build relationships with people, how confidence can be built through empowering strategies and how social activity goal focus can be found through focusing strategies. The importance of the therapeutic relationship in developing a partnership with clients and family members to support engagement in goal setting is well-documented (28, 32, 49, 50). Similarly, theoretical frameworks of person-centered rehabilitation practice recognize the importance of clinician attributes in building relationships and connecting with others. As described earlier, Jesus et al. (14) identified five relational attributes in the person-professional dyad, and McCormack and McCance (15) emphasized the importance of professional attributes such as interpersonal skills and knowing “self” in their framework of person-centered care. Given the experience and training of the clinicians involved in the M-ComConnect project, these attributes were likely inherent in the choice and use of specific clinical strategies during the interview process. Our analysis contributes to research on person-centered models of rehabilitation by providing a clinical illustration on how therapeutic relationships are developed and how goal focus can be derived through our interactions, thereby bridging the gap between theory and practice.
Humanizing strategies (curiosity, respect and empathy, use of reflections, affirmations and compliments, revealing aspects of self and use of humor) are well-documented in counseling, psychotherapy, motivational interviewing, and working alliance literature (25, 26, 51, 52). There is also strong, consistent evidence demonstrating a positive relationship between therapeutic alliance and outcomes in psychotherapy literature (53). This supports our hypothesis that the relationship and connection between the person and clinician contributed to the success of the program. Empowering strategies have also received attention in the literature. Focusing on strengths, for example, emerged from the field of positive psychology, and is recognized as being an important construct for personal growth (54), as well as having a positive impact on rapport building and rehabilitation outcomes (37). Equally, empowering strategies such as client's self-determination and choice and control over decision-making have received much attention in mental health practices, intellectual disability literature and rehabilitation literature (55–57). A growing body of evidence suggest that self-determination and choice-offering increases satisfaction with services, improves social functioning, and adherence to interventions (58, 59). In the context of this study, the use of the empowering strategy “emphasizing choice and control” was made explicit. Participants were given choices and reminded that they were in control, and clinicians worked collaboratively with the person to identify roadblocks and reveal potential opportunities. The success of empowering strategies was evident in post-intervention interviews. Mitch, for example, said, “She (the clinician) really did make me feel that I had good input at every stage and I never felt railroaded or pushed into a corner. At every stage it was my choice on what to do and how to do it and that's important.”
Acknowledging that people with TBI may have challenges with goal planning and identifying realistic goals due to cognitive impairment and reduced self-awareness (32, 34) one further strength of our approach was its application to all participants regardless of their individual challenges. A social leisure/recreation activity goal focus was collaboratively derived for all participants. Participants in this study presented with varying degrees of impairment in cognition, communication, and self-awareness. The advantage of the M-ComConnect approach was the capacity to “understand and connect” with the person, “build a relationship,” and “find focus” regardless of their individual challenges. The range of strategies described was observed across all participant interviews, however the intensity with which they were utilized was determined by the individual's unique presentation. Flexibility and responsiveness were therefore key.
Strengths, Limitations, and Future Research
The analysis presented in this paper provided a lens through which to view what unfolded during person-clinician interactions in real time. Rather than offering a theoretical perspective on principles of a person-centered approach, it distilled a range of clinical strategies that were used to understand and connect with the person, build the relationship, and find focus with the person for engagement in a social activity that reflected their sense of self.
The majority of participants continued with their activity and/or started other new activities. Whilst multiple factors invariably contribute to the success of such a program, it was hypothesized that the relational approach was integral, and this was supported by themes that emerged in post-intervention interviews.
Participants in the M-ComConnect project were aware of the project aims prior to becoming involved, and were included in the study based on their recognized desire and motivation to find social activities in which to engage. The interview process was therefore deliberately geared toward this outcome, and there was already a focus in the minds of the clinicians and participants, potentially influencing the aim/outcome of the interactions. This focus may impact on translation of the framework into clinical practice where clinicians are working with clients who may not be so motivated to participate in social leisure/recreation activities. One point for consideration, therefore, is how this goal-focusing framework could be utilized in a clinical setting. Working within a framework that provides structure and strategies to support the client to find their social activity goal focus would be beneficial in a community rehabilitation setting where funding is limited. However, reconsideration as to how funding resources are allocated may well be required. This paper highlights the value of factoring in sufficient time for getting to know the person and building a relationship so that interventions are personally-relevant and person-centered, thereby maximizing the potential for success.
Further research into translating this framework in clinical practice is required. Evaluation of its impact from multiple perspectives including, people with TBI and their close others, allied health clinicians and funding bodies is also necessary to inform ongoing development.
Conclusion
A distinct set of strategies used by clinicians in this project enabled them to understand and connect with the person, build a relationship and work together with them to find focus. The derived social leisure/recreation activity was therefore personally meaningful and grounded in the person's sense of self. This sense of self was further enhanced through social participation in the leisure/recreation activity that was supported by individualized interventions aligned with their individual characteristics and goal foci. This increased self-confidence and facilitated successful continuation of social activity participation. Through engagement in this program, the person experienced situation-specific positive outcomes (attending an activity/ increased community integration) and person-specific outcomes (increased confidence and well-being). The M-ComConnect approach to finding goal focus shows promise as a community-based rehabilitation framework for people with severe TBI and complex presentations.
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by University Human Ethics Committee, La Trobe University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
This work was produced as part of a research project funded by the Transport Accident Commission directly (TAC project T032) and via the Institute for Safety Compensation and Recovery Research (ISCRR Project 155).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank the participants and clinicians who made a significant contribution to the project.
References
1. Bertram T, Togher L, Power E, Douglas J. The maintenance of friendships after severe traumatic brain injury. Brain Impairment. (2020) 22:79–91. doi: 10.1017/BrImp.2020.13
2. Douglas J. Loss of friendship following traumatic brain injury: a model grounded in the experience of adults with severe injury. Neuropsychol Rehabil. (2020) 30:1277–302. doi: 10.1080/09602011.2019.1574589
3. Finset A, Dyrnes S, Krogstad JM, Berstad J. Self-reported social networks and interpersonal support 2 years after severe traumatic brain injury. Brain Injury. (1995) 9:141–50. doi: 10.3109/02699059509008187
4. Kreutzer JS, Wehman P. Community Integration Following Traumatic Brain Injury. Baltimore: Brookes (1990).
5. Ownsworth T, Fleming J. Community adjustment and re-engagement. In: Levin H, Shum D, Chan R, editors. Understanding Traumatic Brain Injury: Current Research and Future Directions. Oxford: Oxford University Press (2014). p. 235–54.
6. Wise EK, Mathews-Dalton C, Dikmen S, Temkin N, Machamer J, Bell K, et al. Impact of traumatic brain injury on participation in leisure activities. Arch Phys Med Rehabil. (2010) 91:1357–62. doi: 10.1016/j.apmr.2010.06.009
7. Fleming J, Braithwaite H, Gustafsson L, Griffin J, Collier AM, Fletcher S. Participation in leisure activities during brain injury rehabilitation. Brain Injury. (2011) 25:806–18. doi: 10.3109/02699052.2011.585508
8. Douglas JM. Conceptualizing self and maintaining social connection following severe traumatic brain injury. Brain Injury. (2013) 27:60–74. doi: 10.3109/02699052.2012.722254
9. Tate RL, Wakim D, Sigmundsdottir L, Longley W. Evaluating an intervention to increase meaningful activity after severe traumatic brain injury: a single-case experimental design with direct inter-subject and systematic replications. Neuropsychol Rehabil. (2020) 30:641–72. doi: 10.1080/09602011.2018.1488746
10. Douglas J, Drummond M, Knox L, Mealings M. Chapter 8: Rethinking social-relational perspectives in rehabilitation: traumatic brain injury as a case study. In: McPherson K, Gibson BE, Leplege A, editors. Rethinking Rehabilitation Theory. Boca Raton, FL: CRC Press (2015). p. 137–62.
12. Ylvisaker M, Mcpherson K, Kayes N, Pellett E. Metaphoric identity mapping: Facilitating goal setting and engagement in rehabilitation after traumatic brain injury. Neuropsychol Rehabil. (2008) 18:713–41. doi: 10.1080/09602010802201832
13. Douglas J, Leeson R, Collins M, Bigby C. Maximizing Social Connection and Building Relationships in the Community: Evaluation of a Multi-Component Community Connection Program (M-ComConnect) for People With Severe TBI. Final Report TAC Project No: T032 (2021).
14. Jesus TS, Papadimitriou C, Bright FA, Kayes NM, Pinho CS, Cott CA. The Person-Centered Rehabilitation Model: Framing the concept and practice of person-centered adult physical rehabilitation based on a scoping review and thematic analysis of the literature. Arch Phys Med Rehabil. (2021). doi: 10.1016/j.apmr.2021.05.005
15. McCormack B, McCance T, . Person-Centred Practice in Nursing and Health Care: Theory and Practice. Chichester: Wiley Blackwell (2017).
16. Evans CC, Sherer M, Nakase-Richardson R, Mani T, Irby JW Jr. Evaluation of an interdisciplinary team intervention to improve therapeutic alliance in post-acute brain injury rehabilitation. J Head Trauma Rehabil. (2008) 23:329–38. doi: 10.1097/01.HTR.0000336845.06704.bc
17. Klonoff PS, Lamb DG, Henderson SW. Outcomes from milieu-based neurorehabilitation at up to 11 years post-discharge. Brain Injury. (2001) 15:413–28. doi: 10.1080/02699050010005968
18. Lustig DC, Strauser DR, Weems GH, Donnell CM, Smith LD. Traumatic brain injury and rehabilitation outcomes: does the working alliance make a difference? J Appl Rehabil Counsel. (2003) 34:30–7. doi: 10.1891/0047-2220.34.4.30
19. Giles GM, Manchester D. Two approaches to behavior disorder after traumatic brain injury. J Head Trauma Rehabil. (2006) 21:168–78. doi: 10.1097/00001199-200603000-00009
20. Prigatano GP. Disturbances of self-awareness and rehabilitation of patients with traumatic brain injury: a 20-year perspective. J Head Trauma Rehabil. (2005) 20:19–29. doi: 10.1097/00001199-200501000-00004
21. Prigatano GP, Klonoff PS, O'Brien KP, Altman I, Amin K, Chiapello DA, et al. Productivity after neuropsychologically oriented, milieu rehabilitation. J Head Trauma Rehabil. (1994) 9:91–102. doi: 10.1097/00001199-199403000-00011
22. Schönberger M, Humle F, Zeeman P, Teasdale TW. Working alliance and patient compliance in brain injury rehabilitation and their relation to psychosocial outcome. Neuropsychol Rehabil. (2006) 16:298–314. doi: 10.1080/09602010500176476
23. Bordin E. The generalizability of the psychoanalytic concept of the working alliance. Psychother Theory Res Pract. (1979) 16:252–60. doi: 10.1037/h0085885
24. Bordin E. Theory and research on the therapeutic working alliance: new directions. In: Horvath AO, Greenberg LS, editors. The Working Alliance: Theory, Research and Practice. New York, NY: Wiley and Sons Inc. (1994). p. 13–37.
25. Horvath AO. The therapeutic alliance: concepts, research and training. Aust Psychol. (2001) 36:170–6. doi: 10.1080/00050060108259650
26. Stagg K, Douglas J, Iacono T. The perspectives of allied health clinicians on the working alliance with people with stroke-related communication impairment. Neuropsychol Rehabil. (2021) 31:1390–409. doi: 10.1080/09602011.2020.1778491
27. Prescott S, Fleming J, Doig E. Goal setting approaches and principles used in rehabilitation for people with acquired brain injury: a systematic scoping review. Brain Injury. (2015) 29:1515–29. doi: 10.3109/02699052.2015.1075152
28. Sugavanam T, Mead G, Bulley C, Donaghy M, van Wijck F. The effects and experiences of goal setting in stroke rehabilitation - a systematic review. Disabil Rehabil. (2013) 35:177–90. doi: 10.3109/09638288.2012.690501
29. D'Cruz K, Howie L, Lentin P. Client-centered practice: perspectives of persons with a traumatic brain injury. Scand J Occup Ther. (2016) 23:30–8. doi: 10.3109/11038128.2015.1057521
30. Cameron LJ, Somerville LM, Naismith CE, Watterson D, Maric V, Lannin NA. A qualitative investigation into the patient-centered goal-setting practices of allied health clinicians working in rehabilitation. Clin Rehabil. (2018) 32:827–40. doi: 10.1177/0269215517752488
31. Bright FAS, Kayes NM, Worrall L, McPherson KM. A conceptual review of engagement in healthcare and rehabilitation. Disabil Rehabil. (2015) 37:643–54. doi: 10.3109/09638288.2014.933899
32. Doig E, Fleming J, Cornwell PL, Kuipers P. Qualitative exploration of a client-centered, goal-directed approach to community-based occupational therapy for adults with traumatic brain injury. Am J Occup Therapy. (2009) 63:559–68. doi: 10.5014/ajot.63.5.559
33. Fischer S, Gauggel S, Trexler LE. Awareness of activity limitations, goal setting and rehabilitation outcome in patients with brain injuries. Brain Injury. (2004) 18:547–62. doi: 10.1080/02699050310001645793
34. Turner BJ, Ownsworth TL, Turpin M, Fleming JM, Griffin J. Self-identified goals and the ability to set realistic goals following acquired brain injury: a classification framework. Aust Occup Ther J. (2008) 55:96–107. doi: 10.1111/j.1440-1630.2007.00660.x
35. Markus H, Nurius P. Possible selves. Am Psychol. (1986) 41:954–69. doi: 10.1037/0003-066X.41.9.954
36. Prescott S, Fleming J, Doig E. Rehabilitation goal setting with community dwelling adults with acquired brain injury: a theoretical framework derived from clinicians' reflections on practice. Disabil Rehabil. (2018) 40:2388–99. doi: 10.1080/09638288.2017.1336644
37. Wainman-Lefley J, Goudie N, Richardson M, Evans J. A pilot feasibility study of a randomized controlled trial of goal setting using the values in action inventory of strengths following brain injury. Neuropsychol Rehabil. (2020) 1–19. doi: 10.1080/09602011.2020.1823428. [Epub ahead of print].
38. Kiresuk TJ, Smith A, Cardillo JE, Lougaris IA, Ejournal Library. Goal Attainment Scaling: Applications, Theory, and Measurement. Hoboken: Taylor and Francis (2014).
39. Law MC, Baptiste S, Carswell A, McColl M, Polatajko HJ, Pollock N, Canadian Occupational Performance Measure. Canadian Occupational Performance Measure, 5th Edition-Revised. Ottawa: CAOT publications ACE (2019).
40. Douglas J. Elizabeth Usher Memorial Lecture: Placing therapy in the context of the self and social connection. Int J Speech Lang Pathol. (2015) 17:199–210. doi: 10.3109/17549507.2015.1016113
41. Tate RL. Assessing support needs for people with traumatic brain injury: the care and needs scale (CANS). Brain Injury. (2004) 18:445–60. doi: 10.1080/02699050310001641183
42. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
43. Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health. (2019) 11:589–97. doi: 10.1080/2159676X.2019.1628806
44. Todres L, Galvin K, Holloway I. The humanization of healthcare: a value framework for qualitative research. Int J Qual Stud Health Well-being. (2009) 4:68–77. doi: 10.1080/17482620802646204
45. Doig E, Fleming J, Tooth T. Patterns of community integration 2-5 years post-discharge from brain injury rehabilitation. Brain Injury. (2001) 15:747–62. doi: 10.1080/02699050110034343
46. Douglas J. ‘The things that help, the things that get in the way': Working together to improve outcome following acquired brain injury, presidential address. Brain Impairment. (2018) 19:258–69. doi: 10.1017/BrImp.2018.17
47. McColl MA, Carlson P, Johnston J, Minnes P, Shue K, Davies D, et al. The definition of community integration: perspectives of people with brain injuries. Brain Injury. (1998) 12:15–30. doi: 10.1080/026990598122827
48. Minnes P, Carlson P, Ann Mccoll M, Lou Nolte M, Johnston J, Buell K. Community integration: a useful construct, but what does it really mean? Brain Injury. (2003) 17:149–59. doi: 10.1080/02699050301828
49. Lefebvre H, Pelchat D, Swaine B, Gélinas I, Levert MJ. The experiences of individuals with a traumatic brain injury, families, physicians and health professionals regarding care provided throughout the continuum. Brain Injury. (2005) 19:585–97. doi: 10.1080/02699050400025026
50. Holliday RC, Ballinger C, Playford ED. Goal setting in neurological rehabilitation: Patients' perspectives. Disabil Rehabil. (2007) 29:389–94. doi: 10.1080/09638280600841117
51. Cormier LS, Hackney H. Counseling Strategies and Interventions, 8th Edn. Upper Saddle River, NJ: Pearson (2012).
52. Rollnick S, Miller WR, Butler C, ProQuest NetLibrary Inc., Ejournal Library. Motivational Interviewing in Health Care: Helping Patients Change Behavior. New York, NY: Guilford Press (2008).
53. Horvath A, Del Re A, Fluckiger C, Symonds D, Flueckiger A. Alliance in individual psychotherapy. Psychotherapy. (2011) 48:9–16. doi: 10.1093/acprof:oso/9780199737208.003.0002
54. Sheldon KM, Houser-Marko L. Self-concordance, goal attainment, and the pursuit of happiness: can there be an upward spiral? J Pers Soc Psychol. (2001) 80:152–65. doi: 10.1037/0022-3514.80.1.152
55. Pilnick A, Clegg J, Murphy E, Almack K. Questioning the answer: questioning style, choice and self-determination in interactions with young people with intellectual disabilities. Sociol Health Illness. (2010) 32:415–36. doi: 10.1111/j.1467-9566.2009.01223.x
56. Sheldon KM, Williams GC, Joiner T. Self-Determination Theory in the Clinic Motivating Physical and Mental Health. Newhaven: Yale University Press (2003).
57. Douglas J, Bigby C. Development of an evidence-based practice framework to guide decision making support for people with cognitive impairment due to acquired brain injury or intellectual disability. Disabil Rehabil. (2020) 42:434–41. doi: 10.1080/09638288.2018.1498546
58. Stanhope V, Barrenger SL, Salzer MS, Marcus SC. Examining the relationship between choice, therapeutic alliance and outcomes in mental health services. J Pers Med. (2013) 3:191–202. doi: 10.3390/jpm3030191
Keywords: traumatic brain injury, activity, social participation, goal-setting, clinical strategies
Citation: Leeson R, Collins M and Douglas J (2021) Finding Goal Focus With People With Severe Traumatic Brain Injury in a Person-Centered Multi-Component Community Connection Program (M-ComConnect). Front. Rehabilit. Sci. 2:786445. doi: 10.3389/fresc.2021.786445
Received: 30 September 2021; Accepted: 22 November 2021;
Published: 17 December 2021.
Edited by:
Brendan McCormack, Queen Margaret University, United KingdomReviewed by:
Alessandro Giustini, Istituto di Riabilitazione Santo Stefano, ItalyJaana Paltamaa, JAMK University of Applied Sciences, Finland
Sylwia Górska, Queen Margaret University, United Kingdom
Copyright © 2021 Leeson, Collins and Douglas. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jacinta Douglas, J.Douglas@latrobe.edu.au
†ORCID: Rebecca Leeson orcid.org/0000-0003-3851-0367
Michelle Collins orcid.org/0000-0002-9801-3648
Jacinta Douglas orcid.org/0000-0003-0940-6624
 Rebecca Leeson
Rebecca Leeson Michelle Collins1†
Michelle Collins1†  Jacinta Douglas
Jacinta Douglas