- 1Department of Public Health, Sarab Faculty of Medical Sciences, Sarab, Iran
- 2Department of Nursing, Sarab Faculty of Medical Sciences, Sarab, Iran
- 3Research Center of Psychiatry and Behavioral Sciences, Tabriz University of Medical Sciences, Tabriz, Iran
Background: Vaccination is one of the most influential and cost-effective health interventions for preventing and reducing COVID-19 diseases. Unfortunately, the majority of the world's population is deprived of vaccination. Health Literacy (HL) and Media Literacy (ML) are essential to the COVID-19 vaccination. The present study investigates the barriers to COVID-19 vaccine uptake, focusing on classification and the roles of HL and ML.
Methods: A cross-sectional study was conducted among people 18–65 years old in Sarab City, located in East Azerbaijan, Iran, between September to October 2020. Multistage cluster sampling was employed to recruit 298 people from Health Care Services Centers (HCCs).
Results: The results of this research demonstrated that about 32.6% of participants reported that they have fully injected COVID-19 vaccines. Also, HL was positively associated with ML (r = 0.214, p < 0.05). Barriers of COVID-19 vaccine uptake were classified into personal, interpersonal, group and organizational, society and decision-making factors. Besides, barriers to the COVID-19 vaccine were significantly correlated with HL (r = −0.298, p < 0.05) and ML (r = 0.266, p < 0.05). Additionally, in the hierarchical regression model, demographic characteristics accounted for 8.2% of the variation in barriers to the COVID-19 vaccine (F = 4.34; p = 0.001), that monthly income (ß = −0.237; p < 0.05) and marriage statues (ß = 0.131; p < 0.05) were statistically associated with low barriers. HL as predictor variables explained an additional 14.4% of variation in barriers of COVID-19 vaccine (F = 53.84; p < 0.001) and ML explained an extra 9.2% of the variation (F = 38.83; p < 0.001). In total, demographic characteristics, HL dimensions and ML were able to explain 31.8% of the variation in barriers to COVID-19 vaccine.
Conclusions: According to the findings, various strategies are needed to increase the COVID-19 vaccination uptake. This is due to the fact that barriers to COVID-19 vaccination uptake are multifactorial. These facts can help health policymakers and healthcare providers design media-based interventions to reduce barriers to COVID-19 vaccination uptake among adults. Enhancing vaccine HL and ML for adults and improving vaccine confidence are of high priority.
1. Introduction
The COVID-19 pandemic has led to significant changes in people's daily lives worldwide (1). Since the COVID-19 outbreak, many precautions have been implemented, including quarantines, lockdowns, wearing mandatory face masks in public, and social isolation (2, 3). Vaccination is one of the most crucial and cost-effective health interventions (4) for achieving herd immunity and halting the COVID-19 pandemic (1). At least 80% of the population must be vaccinated for herd immunity (5). However, there are some perceived barriers to achieving the desired vaccination coverage. According to a systematic review, worldwide acceptance rates for the COVID-19 vaccine ranged from 97% to 23.6%, with the lowest rate reported in the Middle East (6).
According to the health belief model, perceived barriers can directly lead to non-participation in preventive behavior (5). The literature has shown that insufficient information about vaccines and their side effects, mistrust in the source of the vaccine (6), concern and mistrust about the vaccine's efficacy and safety, and belief in natural immunity (7) are perceived barriers to COVID-19 vaccination. Studies with similar results have also been conducted in Iran (8–10). In this regard, Jahanshahi-Amjazi et al. found that 58% of Iranians faced barriers to receiving the COVID-19 vaccine (8). Khankeh et al. (9) identified insufficient trust in the healthcare system, vaccine safety, and adverse effects as primary barriers to vaccine acceptance. Many perceived barriers to COVID-19 vaccination can be influenced by insufficient knowledge and misinformation about the vaccine and poor HL (11).
Misinformation has spread as quickly as the development of the vaccine, primarily through social media (12). Misinformation spreads faster than correct information, and more audiences are exposed to it (13). The World Health Organization (WHO), in response to the rapid expansion and high volume of false information published via digital social media, has coined the term “infodemic” to describe “too much information, including false or misleading information, in digital and physical environments during a disease outbreak” (14). False and misleading information about the COVID-19 vaccine can be challenging for people with insufficient HL and ML and cause them to hesitate or refuse vaccination (11). That is why WHO has requested all countries to fight the infodemic (15).
HL is “the degree to which individuals can obtain, process, understand, and communicate health-related information needed to make informed health decisions” (16). Various personal, demographic, social and informational factors such as gender, language, ethnicity, health education, physical condition, marital status, place of residence, and access to information sources can influence HL level (14, 17, 18). Inadequate HL is associated with adverse health outcomes and less use of preventive services (11). It is considered one of the essential psychosocial factors in the formation of health behaviors (19). According to studies, people with low HL have less intention to receive the COVID-19 vaccine or are hesitant about it (11, 20).
Due to the critical conditions caused by the COVID-19 pandemic and the urgent need for mass vaccination, COVID-19 vaccines were produced and distributed at an unprecedented speed (11). The rapid production and distribution of vaccines caused various information sources, such as social media, to publish information about the inefficacy and non-safety of vaccines (21). Much of this information may need to be revised (21). Therefore, if people cannot evaluate and understand this information, they will be confused, hesitant, and refuse to get the vaccine (12). Recent studies showed that social media play a role in public vaccination refusal (22), indicating the necessity to enhance public ML to analyze media contents related to COVID-19 vaccination (20). The WHO considered ML one of the top five literacy skills (12). ML means thinking about and retrieving correct information and determining its accuracy and correctness for personal or collective use (12). Given the proliferation of anti-vaccination conspiracy theories through social media, ML is undoubtedly a vital tool for public health (23).
According to the background mentioned, studying HL and ML as factors affecting barriers to COVID-19 vaccine uptake can be important for several reasons. By studying HL and ML, we can understand how people access and process information about vaccines, which can influence their decision-making process to uptake (12). As such, considering the rapid dissemination of misinformation and vaccine-related myths through diverse media platforms, comprehending Media Literacy (ML) has a crucial role. By understanding ML, we can effectively identify and combat misinformation, empowering individuals to make informed choices based on credible evidence regarding the COVID-19 vaccination (12). Identifying Health Literacy (HL) and Media Literacy (ML) as factors influencing barriers to COVID-19 vaccine uptake holds significant potential in developing targeted interventions, enhancing communication strategies, and combatting misinformation. These endeavors are crucial for fostering vaccine acceptance and safeguarding public health. The results of this research can effectively gain valuable insights that can guide effective measures in promoting widespread vaccination. Hence, this study aimed to investigate barriers to COVID-19 vaccine uptake by examining the classification and roles of HL and ML.
2. Methods
2.1. Study design and participants
We conducted a cross-sectional study on 298 participants aged 18–65 in Sarab, East Azerbaijan, Iran, between February to May 2023. The sample size was calculated based on information from a similar study (24) and a confidence level of %95, Z = 1.96, SD = 2.89, Mean = 6.74, 283 samples. Finally, considering the possibility of dropping samples, 300 people were included in the study, of which 293 completed the questionnaires completely. Multistage cluster sampling was employed to recruit the participants from Healthcare Services Centers (HSCs). The city of Sarab includes four health centers, each of which was considered a cluster. Then, in the first sampling stage, each HSCs were considered a cluster. In the second stage, participants were randomly selected from the four HSCs (75 people from each HSCs) according to their health records. Respondents were invited to participate in the survey by phone, informed about the research objectives, and signed a formal informed consent form. Participants answered the questionnaire items in a consultation room at the health center. Because of the nature of the study questions and the culture of the study population, all interviews were performed by two trained interviewers to make participants feel at ease. Individuals aged 18–65 with consent to participate in the study were required for inclusion. Exclusion criteria amounted to failing to complete the questionnaire completely and correctly.
2.2.Measure
Published instruments were applied to collect the following data. A brief description of the questionnaire is as follows:
2.2.1. Demographic information questionnaire
Demographic information includes participants' gender, age, marital status, job status, education level, and income status.
2.2.2. Health literacy for iranian adults (HELIA)
We used the validated Health Literacy for Iranian Adults (HELIA) (25). This questionnaire consists of 47 items and five dimensions: (1) Reading health information (4 items) is measured using a five-interval Likert scale, ranging from 1 (completely difficult) to 5 (completely easy). The total score ranged from 4 to 20. The higher scores represented a high level of reading health information. (2) Understanding health information (7 items) was rated on a 5-point scale ranging from 1 (completely difficult) to 5 (completely easy). The scores for understanding items ranged from 7 to 35. The higher scores determined the better condition for understanding; (3) Appraisal of health information (4 items), rated on a 5-point scale ranging from 1 (never) to 5 (always). The total scores for this dimension ranged from 4 to 20. The high level of scores indicated an increased ability to appraise health information; (4) Ability to access health information (6 items) was scored based on a five-interval Likert scale (always = 5, most of the time = 4, sometimes = 3, seldom = 2, and never = 1). The scores ranged between 6 and 30, and a higher score indicated a better ability to access health information; (5) Decision making (12 items) was measured on a five-interval Likert scale (always = 5, most of the time = 4, sometimes = 3, seldom = 2 and never = 1). The scores for decision-making items ranged from 12 to 60; the higher scores indicated a better condition. Cronbach's alpha for all of the dimensions of the questionnaire was >0.7 (0.72–0.89).
2.2.3. Media literacy scale
A validated and reliable scale was used to assess participants' ML (26). The Cronbach's α of this scale was between 0.75 and 0.8. The questionnaire consists of 20 items with five subscales: “understanding the contents of a media message”, “realizing the hidden objectives of a media message”, “deliberate choices of media messages”, “critical view on media messages”, and “analysis of media messages”. The items were rated using a five-point Likert scale (1 = strongly disagree, 2 = slightly disagree, 3 = not sure, 4 = slightly agree, 5 = strongly agree). The overall score ranged between 20 and 100.
2.2.4. Barriers of COVID-19 vaccine
A researcher-made questionnaire assessed barriers to COVID-19 Vaccine uptake. The questionnaire was prepared by reviewing other questionnaires applied in similar studies (7, 24, 27–30). The validity of the questionnaires was assessed by an expert panel (four health educationists, a socialist, and an epidemiologist). To assess reliability, a pilot study was performed on 25 people not included in the final sample. Finally, the version of the scale included 33 items with four dimensions as follows: intrapersonal factors (15 items; α = 0.87), Interpersonal factors (3 items; α = 0.77), Group and organization factors (5 items; α = 0.79), and Society and Policy-making factors (10 items; α = 0.76). For all dimensions, the items were rated on a 5-point Likert-type scale ranging from 1 to 5 (5 = totally agree through 1 = totally disagree). The total score ranges from 33 to 165; the higher score indicates more barriers to COVID-19 vaccine uptake by the participants. The Cronbach's α for all questionnaire, was measured 0.92.
2.2.5. COVID-19 vaccine uptake
Two questions were used to evaluate participants' performance in taking the COVID-19 vaccine [i.e., did you get the COVID-19 vaccine? (Yes or No)]; How many doses of the COVID-19 vaccine did you take? (1 dose; two doses and more).
2.3. Data analysis
We conducted all analyses using SPSS 21 (SPSS Inc, Chicago, IL, USA). The data were presented as mean (SD) for quantitative variables and frequency (percent) for qualitative variables. To assess normality, we utilized the Kolmogorov-Smirnov test. We employed the independent sample t-test and one-way ANOVA for bivariate comparisons of quantitative variables. Additionally, the relationship between HL and ML with barriers to the COVID-19 vaccine was measured using Pearson correlation.
In three steps, we applied Hierarchical Linear Regression analysis for barriers to the COVID-19 vaccine. The demographic variables, including age, gender, education level, job, income and marriage, were entered in the first step. HL was involved in the second step, along with the demographic variables, and in the third step, we entered the demographic variables and HL with ML in the analysis. To determine the percentage of variance characterized by barriers, we assessed the adjusted R2 change following the insertion of each block. The threshold for significance was fixed at = 0.05. The significance level was set to α = 0.05.
3. Results
The demographics of the participants are presented in Table 1. Among the 298 participants, 41.6 % were in the age group of 30 to 39 years. Most participants were male (55%), with an education level of diploma or under (51.7%). More than half of the participants were undergraduates (6.88% freshmen, 46.50% sophomores, 25.13% juniors, and 9.93% seniors). Over 37% of participants reported a monthly family income between 150 and 200 dollars or more. About 32.6% of participants reported that they had been fully injected with COVID-19 vaccines.
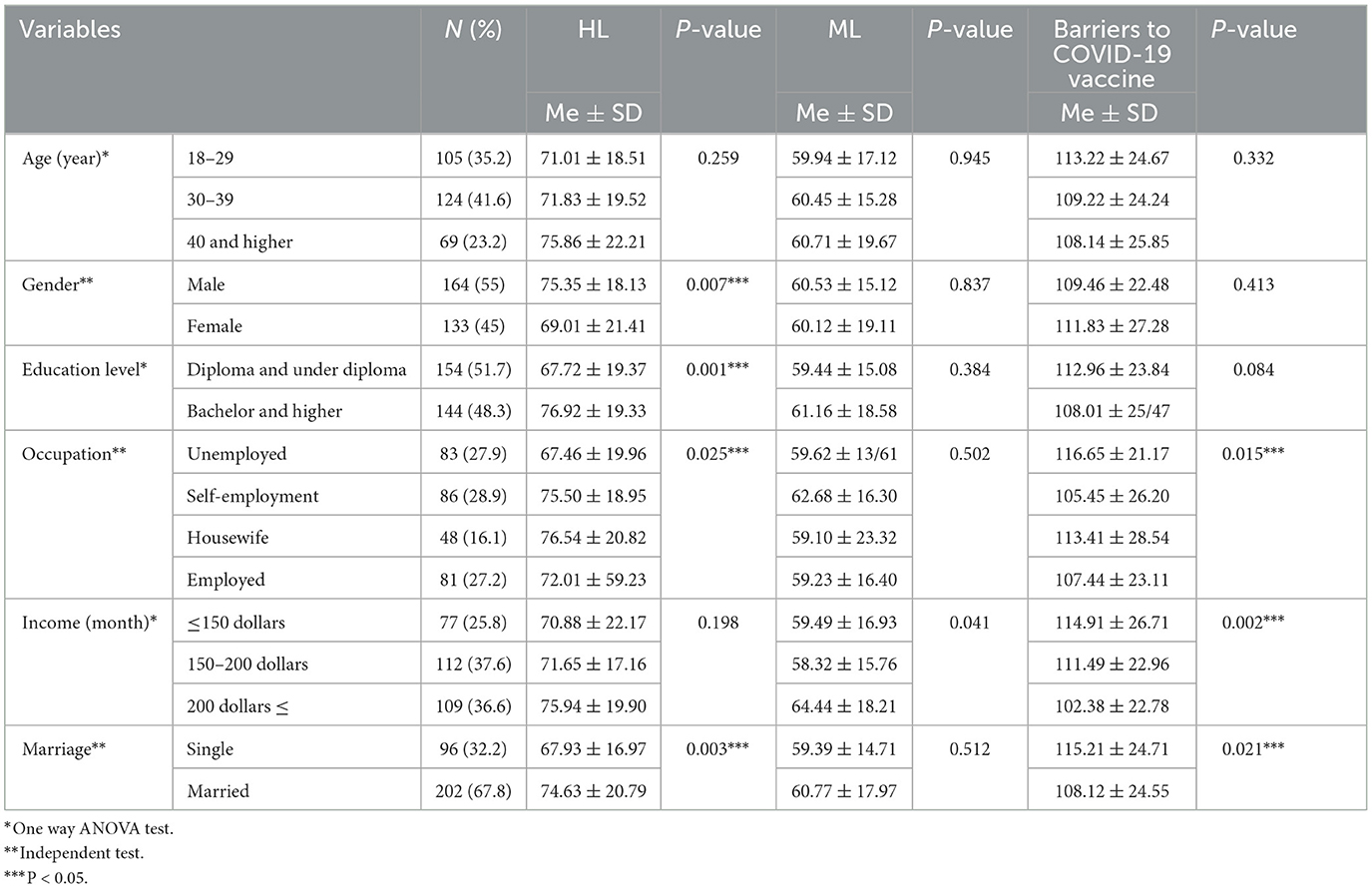
Table 1. Relationship between HL, ML, and barriers to the COVID-19 vaccine and some of the demographic characteristics.
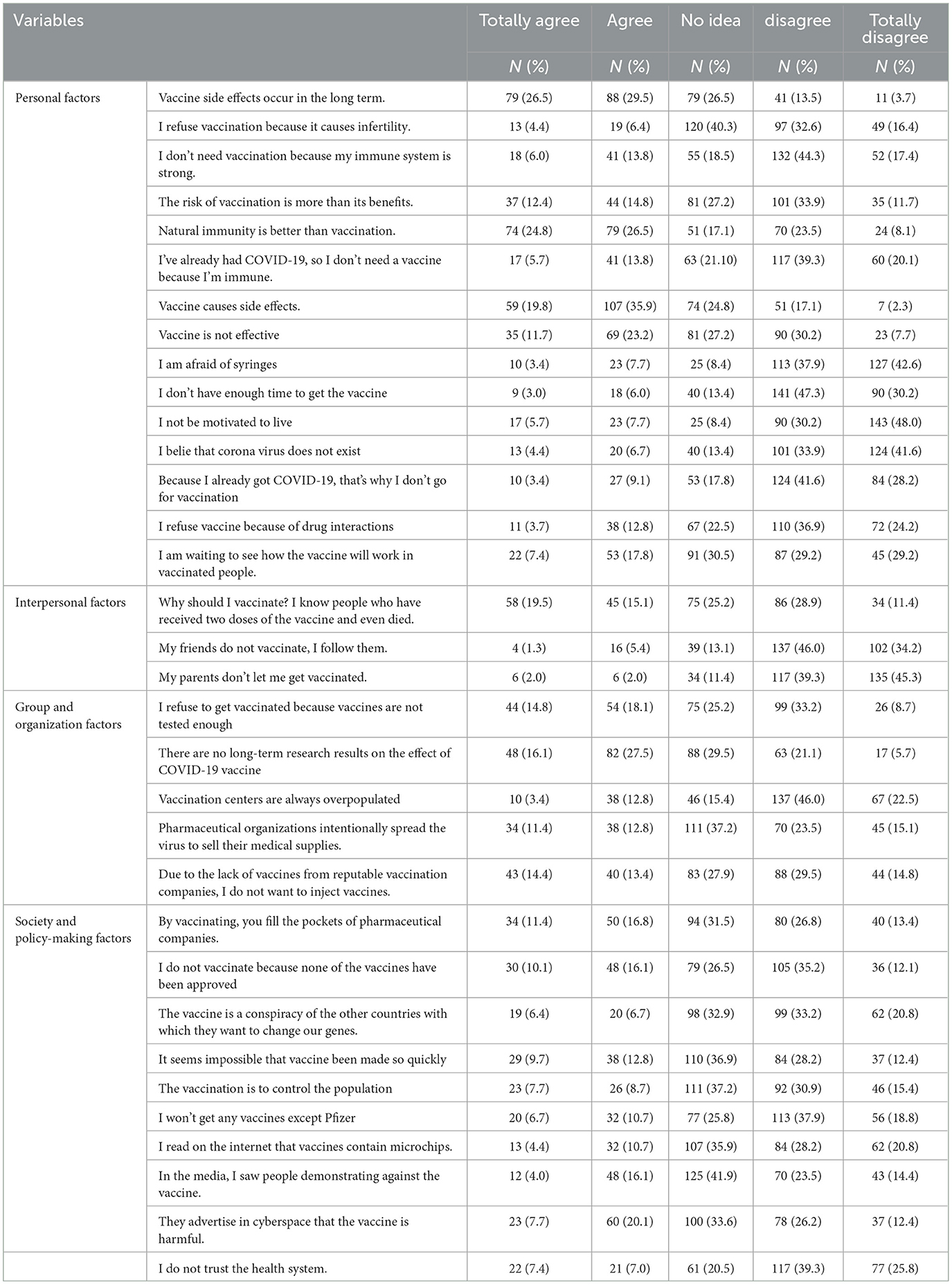
This study established that barriers to COVID-19 vaccination uptake were categorized as personal, interpersonal, group and organizational, societal, and decision-making factors. Questions related to barriers to COVID-19 vaccine uptake are shown in Table 2; of the most important barriers to COVID-19 vaccine uptake by the participants can be pointed to “vaccine side effects” and “belief in better natural immunity than vaccine immunity”.
Table 3 indicates that HL and ML scores were higher among participants with a history of COVID-19 vaccine uptake (p < 0.05). Also, individuals with a history of COVID-19 vaccine uptake experienced fewer barriers.
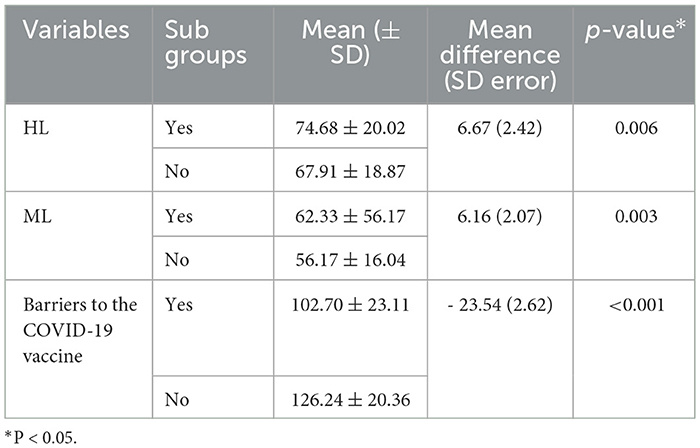
Table 3. Comparison of HL and ML variables and barriers to the COVID-19 vaccine between vaccinated and unvaccinated individuals.
Table 4 displays the variables' mean scores and standard deviations and the correlation matrix of all the variables in the mediation model. HL was positively associated with ML (r = 0.214, p < 0.05). Barriers to the COVID-19 vaccine had a significant correlation with HL (r = −0.298, p < 0.05) and ML (r = 0.266, p < 0.05).
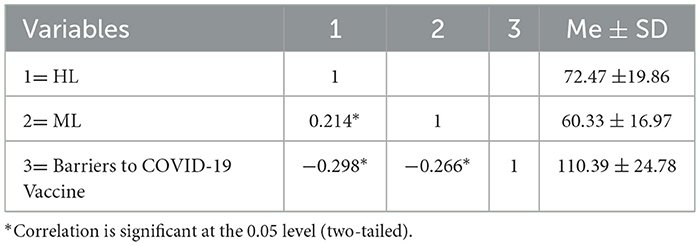
Table 4. Bivariate correlation matrix of the relationship among HL and ML and barriers to COVID-19 vaccine uptake.
We used the hierarchical regression model to examine the effects of demographic characteristics, HL, and ML on barriers to the COVID-19 vaccine. In step 1, demographic characteristics accounted for 8.2% of the variation in barriers to the COVID-19 vaccine (F = 4.34; p = 0.001); that is, approximately 8.6% of the variation in barriers to the COVID-19 vaccine is explained by the demographic variables. Table 4 displays that monthly income (ß = −0.237; p < 0.05) and marital status (ß = 0.131; p < 0.05) were statistically associated with low barriers. HL as predictor variables (step 2) explained an additional 14.4% of the barriers to the COVID-19 vaccine (F = 53.84; p < 0.001). In step 3, ML was added, which explained an additional 9.2% of the variation (F = 38.83; p < 0.001). In total, demographic characteristics, HL dimensions, and ML were able to explain 31.8% of the variation in barriers to the COVID-19 vaccine (Table 5).
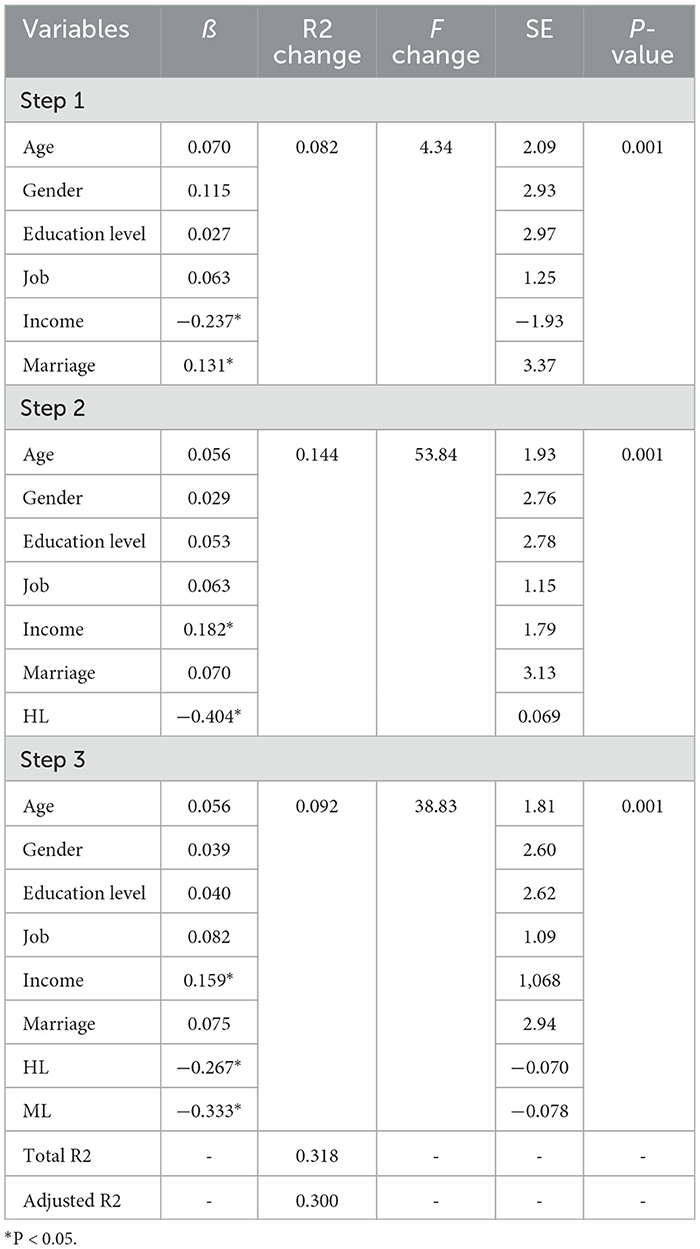
Table 5. Hierarchical linear regression for prediction of barriers to COVID-19 vaccine uptake through demographic characteristics, HL, and ML.
4. Discussion
The present research investigated barriers to COVID-19 vaccine uptake and the role of HL and ML in public vaccine refusal. About 32.6% of participants reported that they had been fully injected with COVID-19 vaccines. A similar study revealed that 26.5% and 26% of low-concern states and municipalities, respectively, received full vaccinations (23). Another study by Li et al. (31) in China indicated that 41.2% of medical students had vaccine hesitancy. Wirawan et al. found that Indonesia's COVID-19 booster vaccine acceptance rate was 56.3% (32). Various studies have reported the relationship between vaccination and hesitancy. In a systematic review in 2021, the range of COVID-19 vaccine acceptance rates was reported to be between 97% and 23.6% globally, with the lowest rate in the Middle East (33). Due to new strains of the COVID-19 virus, vaccine uptake hesitancy could be a significant problem in efforts to control the COVID-19 pandemic. Hence, identifying the barriers to vaccine uptake and designing media-based interventions can help improve this situation.
There was a relationship between gender, education level, occupation, marital status, and HL, but ML was not associated with demographic characteristics. Previous studies revealed that age, gender, education level, occupational status, income, and marital status had statistically significant associations with e-HL and HL in adults (34, 35). During pandemics, it is essential to improve HL based on socioeconomic status so that people can use accurate information to adopt preventive behaviors. ML may enhance health-related information more publicly than HL; therefore, ML was not associated with socioeconomic status.
The founding of this study demonstrated that barriers to COVID-19 vaccine uptake were classified into personal, interpersonal, group and organizational, societal, and decision-making factors. In terms of vaccination side effects, 35.9% of the participants agreed, 19.8% completely agreed, and 29.5% agreed that these side effects were seen in the long term. Also, 26.5% and 24.8% of adults reported that they agreed and totally agreed, respectively, that natural immunity was better than vaccine immunity. Consistent with our finding, the study of Merkelbach et al. implied that fear of side effects (38.1%) and fear of needles (23.6%) were the most common and strongest barriers in terms of COVID-19 vaccination (36). It is better to provide adults with additional information through the media about vaccination effects on mortality rates to decrease barriers to COVID-19 vaccine uptake. In a study, a high prevalence of vaccine hesitancy was associated with fear of the serious consequences of vaccination and its side effects (31).
In terms of interpersonal factors, 25.2% of participants had no idea, and 15.1% stated that they knew people who had been vaccinated twice yet became ill with COVID-19 disease and died. A lack of long-term studies on the barriers to COVID-19 vaccination (group and organizational variables) was reported by 27.5% of participants. When considering societal and decision-making considerations, 20.1% of people agreed with the statement, “It is advertised in cyberspace that the vaccine is harmful.” The classification of COVID-19 vaccine obstacles reveals that to overcome them, all these elements must be considered, not just individual opinions. The low rate of complete COVID-19 vaccination could be a warning sign that other factors are being overlooked. Additionally, policymakers and affiliated organizations can facilitate COVID-19 vaccination.
Barriers to COVID-19 vaccination are also associated with occupation, income, and marital status. These findings are consistent with the other studies (37, 38). A study showed that socioeconomic status was a determinant of actual COVID-19 booster vaccine acceptance (32). Therefore, in order to increase the COVID-19 vaccination rate, it is necessary to focus on socioeconomic factors and individuals with low socioeconomic status.
In this study, those who had previously received the COVID-19 immunization had higher HL and ML scores. Those who had previously gotten the COVID-19 vaccine also encountered fewer obstacles. This is likely because those who have suffered from deadly infectious diseases are more likely to be motivated to adopt preventive behaviors, such as getting the vaccine. Such individuals can contribute valuable insight to help make health programs even better.
Importantly, HL was positively associated with ML. Barriers to the COVID-19 vaccine were significantly correlated with HL and ML. Previous studies demonstrated that health beliefs, social media influence, HL, and trusting invalid information sources were predictors for planned and actual booster COVID-19 vaccine acceptance (11, 32, 39). Wong et al. (30) showed that positive attitudes toward social media were associated with lower levels of vaccine hesitation in regards to the COVID-19 vaccine booster. Therefore, improved HL and ML can aid in making sense of social media content and boosting the uptake of the COVID-19 vaccination. A study's findings suggested that misinformation and vaccine safety perceptions influenced people's willingness to get the COVID-19 vaccine (29), highlighting the need to trust the information provided by the media. These findings contribute new evidence of the relationship between HL and ML and barriers to COVID-19 vaccine uptake, which could be a guideline for enhancing HL and ML as a necessity for COVID-19 vaccine acceptance and COVID-19 disease control. Importantly, in order to control epidemics and pandemics, in the information and technology era, the role of HL and ML should not be ignored.
The result of our study indicated that demographic characteristics accounted for 8.2% of the variation in barriers to the COVID-19 vaccine; that is, the demographic variables explain 8.6% of the variation in barriers to the COVID-19 vaccine. Monthly income and marital status were statistically associated with low barriers. HL as predictor variables explained an additional 14.4% of the variation in barriers to the COVID-19 vaccine, and ML explained an extra 9.2%. In total, demographic characteristics, HL dimensions, and ML were able to explain 31.8% of the variation in barriers to the COVID-19 vaccine. These results are consistent with those of a study conducted in the United States that found a correlation between vaccine reluctance and factors such as gender, race (particularly African-American and American Indian/Alaska Native), smoking, socioeconomic status, regular use of social media, food insecurity, and lack of access to healthcare (40). Researchers found that people's knowledge of the COVID-19 vaccine was linked to their vaccination history, age, level of education, and even, maybe, gender (41). According to another American study, HL serves as a source of wealth when dealing with a pandemic since it allows for the speedy acquisition of accurate knowledge, the comprehension of social hazards, and the adoption of restrictive government laws and protective behaviors (42). It appears that concentrating on the demographic characteristics of adults, enhancing HL and ML, and developing media-based programs can assist in overcoming barriers and gaining control of COVID-19. The success of health and disease prevention programs depends on considering all the factors identified and effective in the spread of diseases and health problems.
4.1. Study limitations
There were some limitations in this research. This research was a cross-sectional study. Hence, it cannot show causal relationships between variables. The barriers to COVID-19 vaccine uptake were investigated in Iran and it may be limited generalizability to other countries. In addition to, these barriers it may not be all the barriers to COVID-19 vaccine uptake. Therefore, it is suggested to be conducted the more studies in the future.
4.2. Implications for future research and strengths
One of the strengths of this study is the classification of various barriers to receiving the COVID-19 vaccine in adults, which can be a guideline for policymakers and healthcare providers to design targeted programs. To overcome the barriers to COVID-19 vaccine uptake, it is necessary to address all these factors, not just individual factors and beliefs. In addition, the role and relationship between HL and ML, which were determinants of vaccine uptake barriers, have been assessed. Notably, the results of this study can assist government policies in responding to crises induced by infectious diseases and pandemics.
5. Conclusion
The results of the present study revealed that the full COVID-19 vaccination rate was low among Iranian adults. This can be a critical factor hindering efforts to control the COVID-19 pandemic in Iran. In addition, the findings indicate that diverse strategies are required to increase COVID-19 vaccination rates due to the multifactorial nature of the barriers to vaccination, which include personal, interpersonal, group, organizational, societal, and policy-making factors. These findings are required for health policymakers and healthcare providers to design community-based interventions to reduce barriers to adult COVID-19 vaccination. There was a significant correlation between COVID-19 vaccine barriers and the prevalence of HL and ML. Enhancing vaccine HL and ML education for adults and increasing vaccine confidence are crucial.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Sarab Faculty of Medical Sciences (IR.SARAB.REC.1401.003). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SR and TB conceptualized and designed the study and drafted the initial manuscript. SP carried out the statistical analysis. KMC drafted the initial manuscript and reviewed the manuscript. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Funding
This study was supported by the Sarab Faculty of Medical Science (grant number: 401000005).
Acknowledgments
We express our gratitude to our colleagues in Center for clinical research development, Razi Psychiatric Hospital, Tabriz University of Medical sciences.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wu Y, Kuru O, Kim DH, Kim S. COVID-19 news exposure and vaccinations: a moderated mediation of digital news literacy behavior and vaccine misperceptions. Int J Environ Res Public Health. (2023) 20:1. doi: 10.3390/ijerph20010891
2. Alqudeimat Y, Alenezi D, AlHajri B, Alfouzan H, Almokhaizeem Z, Altamimi S, et al. Acceptance of a COVID-19 vaccine and its related determinants among the general adult population in Kuwait. Med Princ Pract. (2021) 30:262–71. doi: 10.1159/000514636
3. WHO. Coronavirus (COVID-19). Geneva: WHO. (2022). Available online at: https://www.who.int/health-topics/coronavirus#tab=tab_2
4. Kafadar AH, Tekeli GG, Jones KA, Stephan B, Dening T. Determinants for COVID-19 vaccine hesitancy in the general population: a systematic review of reviews. Zeitschrift fur Gesundheitswissenschaften. (2022) 2022:1–17. doi: 10.1007/s10389-022-01753-9
5. Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q. (1988) 15:175–83. doi: 10.1177/109019818801500203
6. Saied SM, Saied EM, Kabbash IA, Abdo SAE. Vaccine hesitancy: Beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J Med Virol. (2021) 93:4280–91. doi: 10.1002/jmv.26910
7. Bolatov AK, Seisembekov TZ, Askarova AZ, Pavalkis D. Barriers to COVID-19 vaccination among medical students in Kazakhstan: development, validation, and use of a new COVID-19 vaccine hesitancy scale. Hum Vaccin Immunother. (2021) 17:4982–92. doi: 10.1080/21645515.2021.1982280
8. Jahanshahi-Amjazi R, Rezaeian M, Abdolkarimi M, Nasirzadeh M. Predictors of the intention to receive the COVID 19 vaccine by Iranians 18–70 year old: application of health belief model. J Educ Health Promot. (2022) 11:175. doi: 10.4103/jehp.jehp_647_21
9. Khankeh HR, Farrokhi M, Khanjani MS, Momtaz YA, Forouzan AS, Norouzi M, et al. The barriers, challenges, and strategies of COVID-19 (SARS-CoV-2) vaccine acceptance: a concurrent mixed-method study in Tehran City, Iran. Vaccines. (2021) 9:11. doi: 10.3390/vaccines9111248
10. Nakhostin-Ansari A, Zimet GD, Khonji MS, Aghajani F, Teymourzadeh A, Rastegar Kazerooni AA, et al. Acceptance or rejection of the COVID-19 vaccine: a study on iranian people's opinions toward the COVID-19 vaccine. Vaccines (Basel). (2022) 10:670. doi: 10.3390/vaccines10050670
11. Song I, Lee SH. COVID-19 vaccine refusal associated with health literacy: findings from a population-based survey in Korea. BMC Public Health. (2023) 23:255. doi: 10.1186/s12889-023-15182-0
12. Nemati-Anaraki L, Azimi A, Abdolahi L, Gafari S. The relation between Media Literacy and COVID-19 Vaccination. Med J Islam Repub Iran. (2021) 35:200. doi: 10.47176/mjiri.35.200
13. Shaw J, Anderson KB, Fabi RE, Thompson CA, Harris M, Aljabbarin N, et al. COVID-19 vaccination intention and behavior in a large, diverse, U. S. refugee population. Vaccine. (2022) 40:1231–7. doi: 10.1016/j.vaccine.2022.01.057
14. Xu L-m, Xie L-f, Li X, Wang L, Gao Y. A meta-analysis of factors influencing health literacy among Chinese older adults. J Public Health. (2022) 30:1889–900. doi: 10.1007/s10389-021-01638-3
15. Marzo RR, Su TT, Ismail R, Htay MNN, Essar MY, Chauhan S, et al. Digital health literacy for COVID-19 vaccination and intention to be immunized: A cross sectional multi-country study among the general adult population. Front. Public Health. (2022) 10:998234. doi: 10.3389/fpubh.2022.998234
16. Berkman ND, Davis TC, McCormack L. Health literacy: what is it? J Health Commun. (2010) 15:9–19. doi: 10.1080/10810730.2010.499985
17. Uysal N, Ceylan E, Koç A. Health literacy level and influencing factors in university students. Health Soc Care Community. (2019) 28:505–11. doi: 10.1111/hsc.12883
18. Saei M, Hosseini Moghaddam M, Basirian Jahromi H. Assessment of health literacy of tehranian and the factors affecting it. Communic Res. (2019) 26:113–47. doi: 10.22082/cr.2019.112855.1908
19. Zhang H, Li Y, Peng S, Jiang Y, Jin H, Zhang F. The effect of health literacy on COVID-19 vaccine hesitancy among community population in China: the moderating role of stress. Vaccine. (2022) 40:4473–8. doi: 10.1016/j.vaccine.2022.06.015
20. Montagni I, Ouazzani-Touhami K, Mebarki A, Texier N, Schück S, Tzourio C, et al. Acceptance of a Covid-19 vaccine is associated with ability to detect fake news and health literacy. J Public Health. (2021) 43:695–702. doi: 10.1093/pubmed/fdab028
21. Pourrazavi S, Fathifar Z, Sharma M, Allahverdipour H. COVID-19 vaccine hesitancy: a systematic review of cognitive determinants. Health Promot Perspect. (2023) 13:21–35. doi: 10.34172/hpp.2023.03
22. Liu PL, Zhao X, Wan B. COVID-19 information exposure and vaccine hesitancy: the influence of trust in government and vaccine confidence. Psychol Health Med. (2021) 28:27–36. doi: 10.1080/13548506.2021.2014910
23. Mokhtari H, Mirzaei A. The tsunami of misinformation on COVID-19 challenged the health information literacy of the general public and the readability of educational material: a commentary. Public Health. (2020) 187:109–10. doi: 10.1016/j.puhe.2020.08.011
24. Shahrour G, Jaradat D. Dardas LAJ. Barriers related to COVID-19 testing intention. Public Health Nurs. (2021) 38:978–83. doi: 10.1111/phn.12950
25. Montazeri A, Tavousi M, Rakhshani F, Azin SA, Jahangiri K, Ebadi M, et al. Health Literacy for Iranian adults (HELIA): development and psychometric properties. BMC Public Health. (2014) 13:589–99. doi: 10.1186/s12889-020-08787-2
26. First National Conference on Media, Communication and Citizenship Education. The study of relation between media literacy and life style (a case study):young adult high school students between the age of 15 to 18 years old in 6th district of Tehran. In: First National Conference on Media, Communication and Citizenship Education. (2015). Available online at: www.civilica.com/Paper-MCCE01-MCCE01_005.html (accessed October 26, 2020).
27. Moghaddam HR, Khan FR, Bazyar H. Aghamohammadi VJJoE, Promotion H. Reasons for not getting COVID-19 vaccine in Ardabil, a Northwestern province in Iran: Based on an ecological approach. J Educ Health Promot. (2023) 12:111. doi: 10.4103/jehp.jehp_1074_22
28. Fisk RJJGHJ. Barriers to vaccination for coronavirus disease 2019 (COVID-19) control: experience from the United States. Glob Health J. (2021) 5:51–5. doi: 10.1016/j.glohj.2021.02.005
29. Embrett M, Sim SM, Caldwell HA, Boulos L, Yu Z, Agarwal G. et al. Barriers to and strategies to address COVID-19 testing hesitancy: a rapid scoping review. BMC Public Health. (2022) 22:1–10. doi: 10.1186/s12889-022-13127-7
30. Burke PF, Masters D. Massey GJV. Enablers and barriers to COVID-19 vaccine uptake: An international study of perceptions and intentions. Vaccine. (2021) 39:5116–28. doi: 10.1016/j.vaccine.2021.07.056
31. Li M, Zheng Y, Luo Y, Ren J, Jiang L, Tang J, et al. Hesitancy toward COVID-19 vaccines among medical students in Southwest China: a cross-sectional study. Hum Vaccin Immunother. (2021) 17:4021–7. doi: 10.1080/21645515.2021.1957648
32. Wirawan GBS, Harjana NPA, Nugrahani NW, Januraga PP. Health beliefs and socioeconomic determinants of COVID-19 booster vaccine acceptance: an Indonesian cross-sectional study. Vaccines. (2022) 10:724. doi: 10.3390/vaccines10050724
33. Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines. (2021) 9:160. doi: 10.3390/vaccines9020160
34. Rezakhani Moghaddam H, Ranjbaran S, Babazadeh T. The role of e-health literacy and some cognitive factors in adopting protective behaviors of COVID-19 in Khalkhal residents. Front Public Health. (2022) 10:916362. doi: 10.3389/fpubh.2022.916362
35. Ranjbaran S, Chollou KM, Babazadeh T. Assessment of health literacy and health promoting behaviors among the urban adult population. Ethiop J Health Sci. (2022) 32:985–92. doi: 10.4314/ejhs.v32i5.14
36. Merkelbach I, Magnee T, Sana S, Kollmann J, Kocken P, Denktas S. Using the health belief model to explain COVID-19 vaccination hesitancy in Dutch urban citizens under thirty. PLoS ONE. (2023) 18:e0279453. doi: 10.1371/journal.pone.0279453
37. Kricorian K, Civen R, Equils O. COVID-19 vaccine hesitancy: misinformation and perceptions of vaccine safety. Hum Vaccin Immunother. (2022) 18:1950504. doi: 10.1080/21645515.2021.1950504
38. Wang R, Qin C, Du M, Liu Q, Tao L, Liu J. The association between social media use and hesitancy toward COVID-19 vaccine booster shots in China: a web-based cross-sectional survey. Hum Vaccin Immunother. (2022) 18:2065167. doi: 10.1080/21645515.2022.2065167
39. Turhan Z, Dilcen HY, Dolu I. The mediating role of health literacy on the relationship between health care system distrust and vaccine hesitancy during COVID-19 pandemic. Curr Psychol. (2022) 41:8147–56. doi: 10.1007/s12144-021-02105-8
40. Moon I, Han J, Kim K. Determinants of COVID-19 vaccine hesitancy: California health interview survey preventive medicine reports. Prev Med Rep. (2020) 2023:102200. doi: 10.1016/j.pmedr.2023.102200
41. Biasio LR, Zanobini P, Lorini C, Monaci P, Fanfani A, Gallinoro V, et al. COVID-19 vaccine literacy: a scoping review. Hum Vaccin Immunother. (2023) 19:2176083. doi: 10.1080/21645515.2023.2176083
Keywords: barriers, COVID-19, vaccine, Health Literacy, Media Literacy, Iran
Citation: Ranjbaran S, Chollou KM, Pourrazavi S and Babazadeh T (2023) Barriers to COVID-19 vaccine uptake: classification and the role of Health Literacy and Media Literacy. Front. Public Health 11:1238738. doi: 10.3389/fpubh.2023.1238738
Received: 13 June 2023; Accepted: 09 October 2023;
Published: 08 November 2023.
Edited by:
Christiane Stock, Institute of Health and Nursing Science, GermanyReviewed by:
Satyajit Kundu, North South University, BangladeshOzden Gokdemir, İzmir University of Economics, Türkiye
Copyright © 2023 Ranjbaran, Chollou, Pourrazavi and Babazadeh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Towhid Babazadeh, towhid.babazadeh@gmail.com
 Soheila Ranjbaran
Soheila Ranjbaran Khalil Maleki Chollou
Khalil Maleki Chollou Sara Pourrazavi
Sara Pourrazavi Towhid Babazadeh
Towhid Babazadeh