- 1School of Public Health, Weifang Medical University, Weifang, China
- 2Department of Cardiology, Affiliated Hospital of Jining Medical University, Jining, China
- 3School of Management, Weifang Medical University, Weifang, China
Background: Atrial fibrill ation (AF) is a predominant public health concern in older adults. Therefore, this study aimed to explore the global, regional, and national burden of AF in older adults aged 60–89 between 1990 and 2019.
Methods: The morbidity, mortality, disability-adjusted life years (DALYs), and age-standardized rates of AF were refined from the Global Burden of Diseases study 2019. The epidemiological characteristics were assessed based on numerical values, age-standardized rates per 100,000 person-years, and estimated annual percentage changes (EAPC).
Results: Globally, a total of 33.31 million AF cases, 219.4 thousand deaths, and 65.80 million DALYs were documented in 2019. There were no appreciable changes in EAPC from 1990 to 2019. The disease burden of AF differed significantly across different territories and countries. At the national level, China exhibited the highest number of incident cases [818,493 (562,871–1,128,695)], deaths [39,970 (33,722–46,387)], and DALYs [1,383,674 (1,047,540–1,802,516)]. At the global level, high body mass index (BMI) and high systolic blood pressure (SBP) were two predominant risk factors contributing to the proportion of AF-related deaths.
Conclusion: AF in older adults remains a major public health concern worldwide. The burden of AF varies widely at both national and regional levels. From 1990 to 2019, the cases of incidences, deaths, and DALYs have shown a global increase. The ASIR, ASMR, and ASDR have declined in the high-moderate and high SDI regions; however, the burden of AF increased promptly in the lower SDI regions. Special attention should be paid to the main risk factors for high-risk individuals with AF, which can help control systolic blood pressure and body mass index within normal limits. Over all, it is necessary to illustrate the features of the global AF burden and develop more effective and targeted prevention and treatment strategies.
Introduction
Atrial fibrillation (AF) is a common cardiac arrhythmia (1), affecting more than 33 million people. Globally, it is a primary cause of coronary heart disease and mortality (2). Relevant research indicates that the incidence and prevalence of AF have been going up in Europe and North America from the 1970's to the early twenty-first century (3). The prevalence of AF is expected to rise in the next 30–50 years (4, 5). Hence, AF has become a worldwide public health problem and strained the healthcare system. Understanding the pattern of AF incidence and the temporal trends can facilitate the development of more well-directed preventive measures.
The Global Burden of Disease (GBD) study estimates the AF burden in 204 countries and territories worldwide, providing an excellent opportunity to comprehend the picture of AF (6). Recent studies have assessed the prevalence, disability-adjusted life years (DALYs), and AF-related mortality in all age groups using the data derived from the GBD (7, 8). However, of all cardiovascular diseases, AF commonly causes heart failure (9), imposing a substantial disease burden, especially on older adults. The overall health of older adults declines with age, and multimorbidity is prevalent, especially in cardiovascular disease. Therefore, it is necessary to pay particular attention to older adults. A cohort study found a significant increase in the prevalence of AF in older adults over 60 years of age (10). In addition, the proportion of the older population over 90 years old is only 2%. Therefore, we selected 60–89-year-olds as the research subjects. Based on the GBD Study 2019 data, the purpose of this study was to explore the burden of AF and its risk factors among older adults aged 60–89 years at global, regional, and national levels from 1990 to 2019. Our outcomes can act as a crucial supplement and expansion to previous research while also contributing to the formulation of AF prevention measures targeting various countries.
Methods
Data sources
We collected corresponding data from the Global Health Data Exchange (GHDx) query tool (http://ghdx.healthdata.org/gbd-results-tool) (11), an online tool of the Global Burden of Diseases (GBD), Etiologies, Injuries, and Risk Factors Study. The quality of statistics has been recognized internationally, and the approaches employed in the GBD have been illustrated elsewhere. The GBD 2019 database consisted of epidemiological data (i.e., deaths, prevalence, incidence, and DALYs) for 204 countries and territories worldwide. Then, these countries and territories were divided into five regions in accordance with the sociodemographic index (SDI) (2). The regions ranged from high to low as follows: high SDI, high-middle SDI, middle SDI, low-middle SDI, and low SDI.
Furthermore, the world was geographically divided into 21 regions, such as Australasia and Eastern Europe. The Human Development Index (HDI) data were available for extraction from Human Development Reports (http://hdr.undp.org/en/data). It was a composite measure index of three elementary aspects of human development: life expectancy, education, and per capita income. In our research, HDI was assembled and utilized to match GBD data. The secondary analysis data in the present article did not require ethical agreement or approval from the ethics committee or the institutional review board.
Statistical analysis
The burden of AF was expressed in terms of number, age-standardized incidence rates (ASIRs), age-standardized mortality rates (ASMRs), age-standardized DALY rates (ASDRs), and estimated annual percentage change (EAPC) with a confidence interval of 95%. The ASRs were counted using a standardized global aging structure, which is necessary when comparing populations in different locations or sample groups over a period of time (12).
In the present study, we calculated the EAPC in the age-standardized rates of AF to further assess the burden of the disease. EAPC was a generalization and extensively used weighing measure for ASR's tendency within a specified interval. It was calculated using the referring regression line: Y = α + βX + ε, where Y referred to ln (age-standardized rate), X presented the calendar year, β influenced the active or passive trends in ASR and ε meant error value. The EAPC can be given by the following formula: 100 × [exp (β) – 1], and its 95% confidence interval (CI) could be obtained from the linear regression model (12). There are three situations: (1) if the 95% CI and EAPC assessment were both <0, the ASRs were regarded as a descending trend, (2) if the 95% CI and EAPC were both >0, the ASRs were regarded as an increasing trend. (3) If not, the ASRs were regarded as a steady trend. The statistical analysis in the present study was accomplished using the R program (Version 4.1.2). If the p-value was <0.05, it was deemed to be statistically significant.
Results
Global burden of AF
At the global level, a total of 3,331,144 (2,342,510–4,489,654) cases of AF were reported in 2019. The morbidity in both sexes increased by 1.1% from 1,583,024 (1,094,531–2,166,439) in 1990 to 3,331,144 (2,342,510–4,489,654) in 2019. Moreover, the ASIR fluctuated slightly by 0.05% from 58.54 (44.92–74.24) to 57.09 (44.07–71.9) during the past 30 years. Similarly, the mortality rate increased by 1.36% from 92,801 (82,995–111,456) in 1990 to 219,437 (190,526–249,642) in 2019. The ASMR demonstrates a mild increase of 0.04%, from 4.29 (3.73–5.09) in 1990 to 4.38 (3.7–5.05) in 2019 per 100,000 population. AF caused 6,579,978 (5,241,696–8,321,653) DALYs in 2019 worldwide, which was a 1.16% increase from 3,044,717 (2,363,647–3,900,467) in 1990. With regard to age-standardized rates, in 1990, the ASDR of AF was 110 (87.66–139.16) per 100,000 population, which slightly decreased to 107.13 (86.18–133.73) in 2019 (Table 1, Figure 1A).

Table 1. Incident cases, death, and DALYs of cardiomyopathy and myocarditis and ASRs per 10,000 population from 1990 and 2019 by Global Burden of Disease.
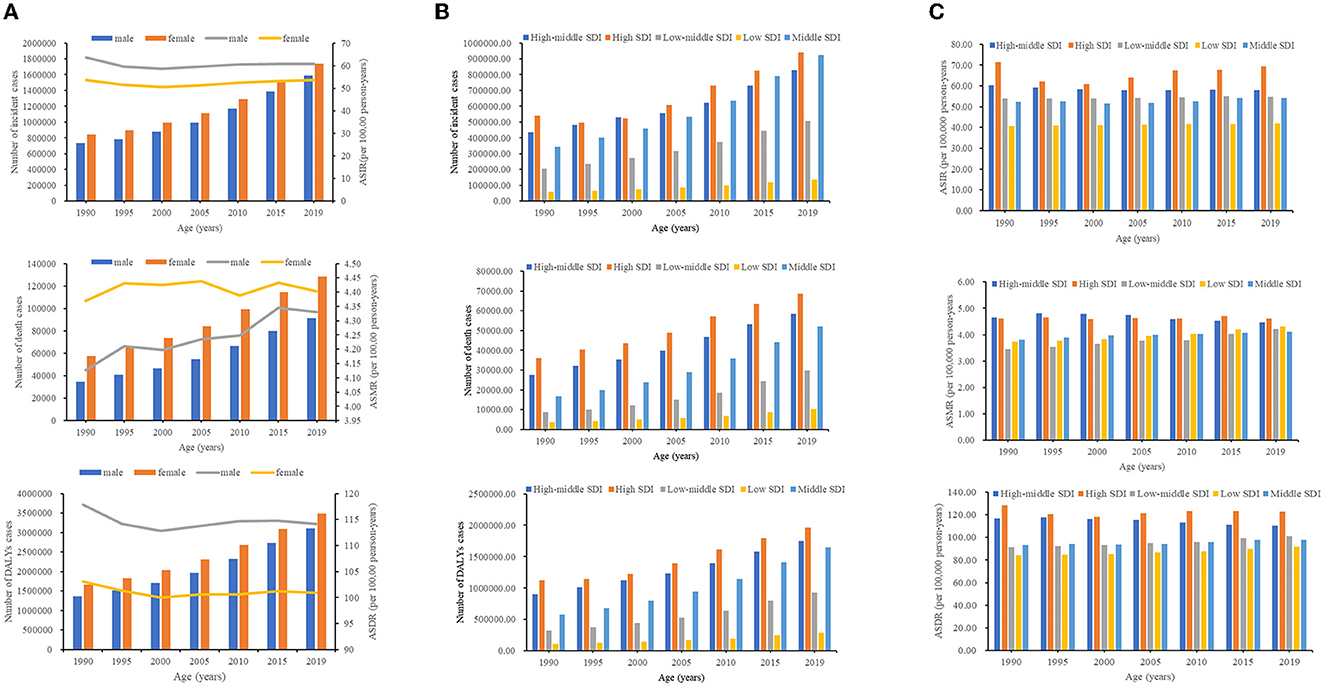
Figure 1. The number of cases and ASRs of AF from 1990 to 2019. (A) The number of cases of AF caused by global, from 1990 to 2019. (B) The number of cases of AF caused by SDI regions from 1990 to 2019. (C) The ASRs of AF caused by SDI regions from 1990 to 2019. SDI, sociodemographic index.
Regional burden of AF
For SDI regions, the number of AF cases showed an upward trend in the five SDI countries from 2009 to 2019 (Table 1, Figure 1B). Interestingly, the higher the SDI region, the higher the morbidity and mortality. From 1990 to 2019, the number of incidences and DALY cases of AF rose most dramatically in the middle SDI. However, the number of deaths increased most substantially in low-middle SDI (Table 1, Figure 1B). Only high-middle SDI recorded a decreasing AF ASR, including ASIR (−0.12; 95% CI: −0.15 to −0.09), ASMR (−0.25; −0.32 to −0.18), and ASDR (−0.25; −0.28 to −0.23) of the EAPC (Table 1, Figure 1C, Supplementary Figure 1). Regarding the rest of the 21 GBD regions, the highest ASIR due to AF has occurred in high-income North America [108.53 (87.59–131.44)] since 2019 (Table 1, Supplementary Figure 2A). Similarly, the ASMR and ASDR of AF for men and women in Australasia were 6.86 (5.45–8.33) and 168.28 (132.54–214.32), respectively, which placed Australia in the top rank for AF related-mortality in 2019 (Table 1, Supplementary Figures 2B, C). It is also worth noting that the most prominent increases in the ASIR and ASDR were in high-income North America. Additionally, the most significant increases in the ASMR were exhibited in Central Asia, followed by southern sub-Saharan Africa, Southeast Asia, and high-income North America. During the research period, the most pronounced decrease in the ASIR, ASMR, and ASDR was reported, all in high-income Asia Pacific (Table 1, Supplementary Figure 3).
National burden of AF
In 2019, China presented the highest morbidity [818,493 (562,871–1,128,695)], mortality [39,970 (33,722–46,387)], and DALYs [1,383,674 (1,047,540–1,802,516)]. Coincidentally, all three accounted for approximately a quarter of the global caseload (Supplementary Tables 1–3). The United States of America exhibited the highest ASIR [109.52 (88.97–131.92)]; Montenegro showed the highest ASMR [14.38 (11.31–19.38)] and ASDR [250.62 (205.82–313.72)]. Conversely, Bolivia (Plurinational State of) had the lowest ASIR [14.41 (10.71–18.68)]; Singapore had the lowest ASMR [1.97 (1.44–2.37)] and ASDR [51.94 (40.06–67.04)] owing to AF (Supplementary Tables 1–3, Figure 2A). As for the percentage change, the most remarkable rise was in Qatar from 1990 to 2019, with a 7.91% increase in AF incidences; the most conspicuous rise was in Bahrain during the 30 years, with an 8.82% increase in deaths and a 6.51% increase in DALYs (Supplementary Tables 1–3, Figure 2B). Furthermore, the most apparent increase in ASIR was in the United States of America [1.51 (1.07–1.95)] from 1990 to 2019; the most significant rise in ASMR was in Uzbekistan [4.58 (4.23–4.94)]; the most demonstrable increases in the ASDR were in Bahrain [2.71(2.27–3.14)] and Uzbekistan [2.32 (2.17–2.47)] (Supplementary Tables 1–3, Figure 2C). By comparison, Japan displayed significant decreases in the ASIR and ASDR; Guam exhibited the most pronounced decline in the ASMR (Supplementary Tables 1–3, Figure 2C).

Figure 2. The national burden of AF for both sexes in 204 countries and territories. (A) The relative ASRs of AF between 1990 and 2019. (B) The relative changes of AF between 1990 and 2019. (C) The relative EAPCs of AF between 1990 and 2019.
The influential factors for EAPC
Figure 3 shows that ASR (in 2019) and HDI (in 2019) seem to be particularly associated with EAPC. The ASMR of AF implies a healthy life expectancy from disease onset to eventual death. Meanwhile, HDI can be considered a metric to measure the accessibility and level of medical treatment. A significant positive relationship was observed between EAPCs and ASMR. Remarkably, a significant positive association was observed between EAPC and HDI when the HDI was restricted to <0.6. However, when the HDI was above 0.6, the countries with a higher HDI experienced a sharper decrease in EAPC of atrial fibrillation from 1990 to 2019 (Figure 3).
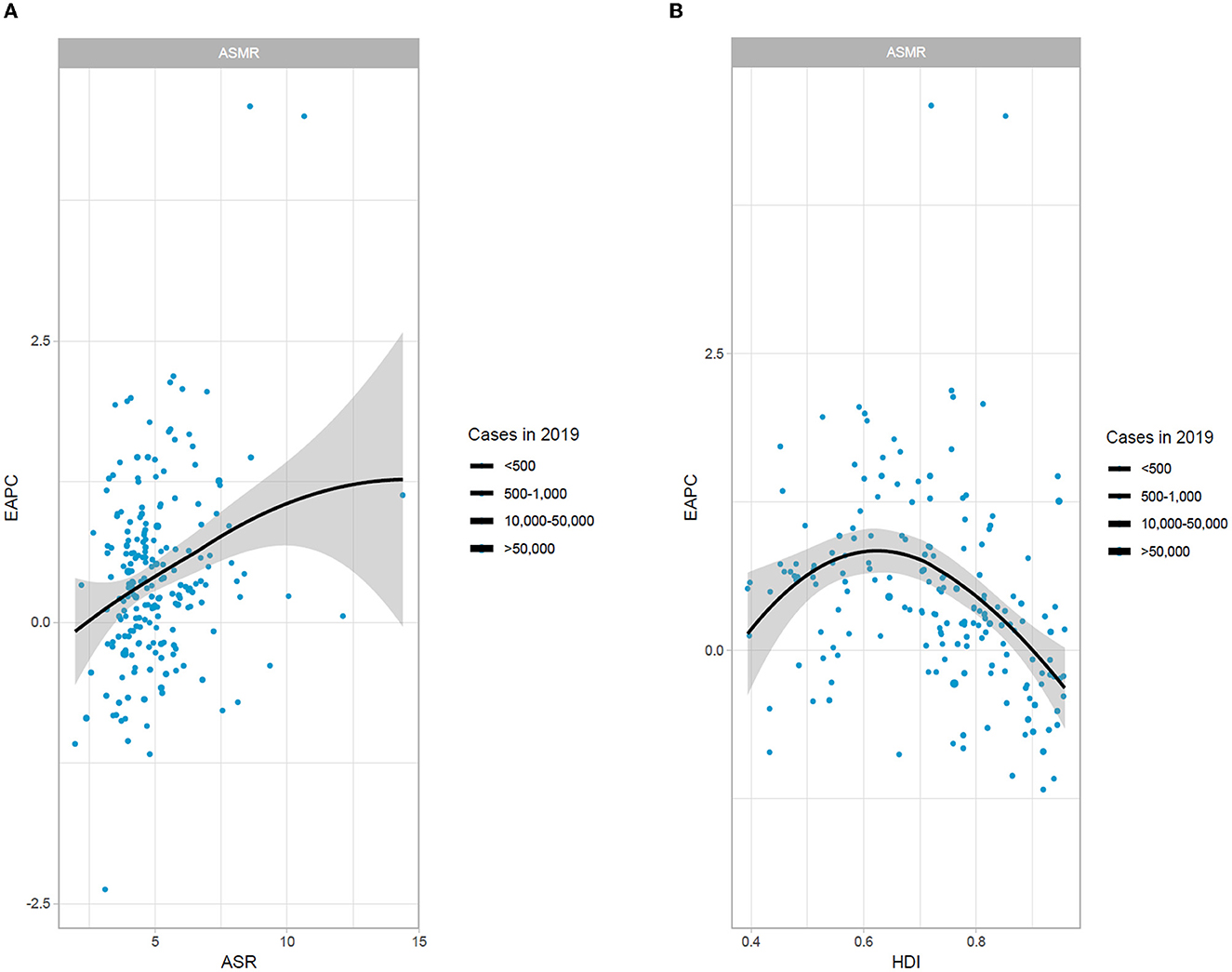
Figure 3. The association between EAPC and ASMR in 2019 and HDI in 2019. (A) The association between EAPC and ASMR in 2019. (B) The association between EAPC and HDI in 2019. EAPC, estimated annual percentage change; ASMR, age-standardized mortality rate; HDI, human development index.
Relationship of ASRs with SDI
A non-linear association was investigated between SDI and ASIR in global and 21 regions. The highest ASIR was found in high-income North America, with an SDI of 0.86. The ASIR was lowest in the Andean-Latin America area when the SDI was 0.53. At the region level, the ASIR values of 10 areas based on SDI in 2019 were higher than the global level, consisting of high-income North America, Australasia, Central Europe, Eastern Europe, Western Europe, Central Asia, Southeast Asia, South Asia, Oceania, and East Asia (Figure 4). The biggest ASMR and ASDR both appeared in Australasia, with SDI values of 0.77 and 0.74, respectively.
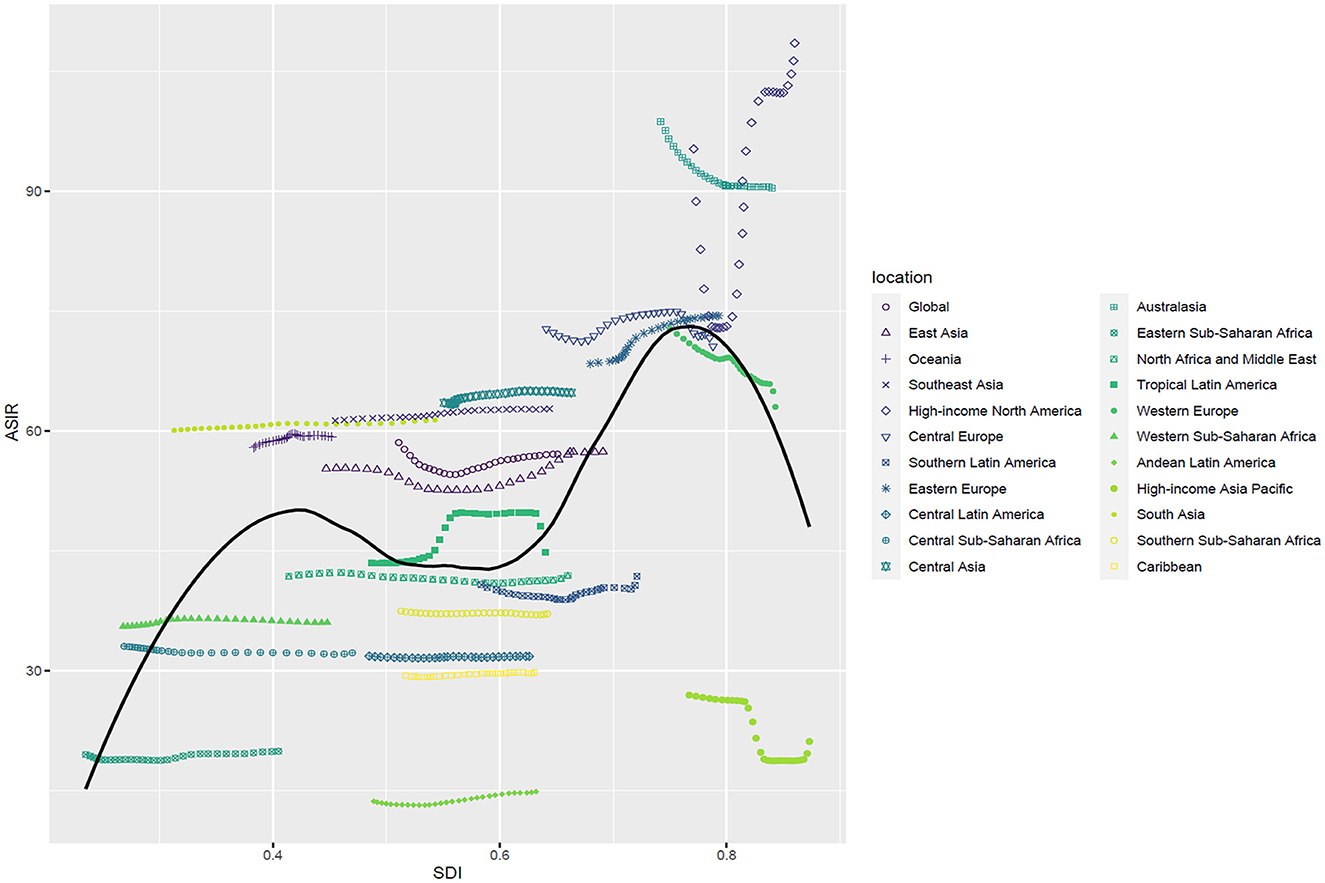
Figure 4. ASIR of AF in the global and 21 regions by SDI, 1990–2019. ASIR, age-standardized incidence rate; SDI, sociodemographic index.
At the national level, we explored the relationship between ASIR and SDI values, which were complex and non-linear in 2019. Further analysis revealed that the ASIR in 204 countries and territories was positively correlated with the SDI. The largest ASIR was in the United States of America, followed by Canada and Greenland, according to the SDI. The ASIR was larger than the anticipated level in a number of territories. Nevertheless, Bolivia (the Plurinational State of), Peru, Ecuador, Eritrea, Somalia, and numerous other countries held a smaller ASIR than the expected SDI (Figure 5). Non-linear relationships among the SDI, ASMR, and ASDR of atrial fibrillation were also surveyed. The highest ASMR and ASDR were both noted in Montenegro when the SDI value was 0.79. However, the lowest ASMR and ASDR occurred in Singapore, with an SDI value of 0.86. And the majority of countries had lower ASMR and ASDR levels than expected, such as Japan, Kuwait, and the Republic of Korea. Intriguingly, burden estimates experienced an upward trend with increasing SDI, yet ASDR had a higher rise than ASMR (Supplementary Figures 4A, B).
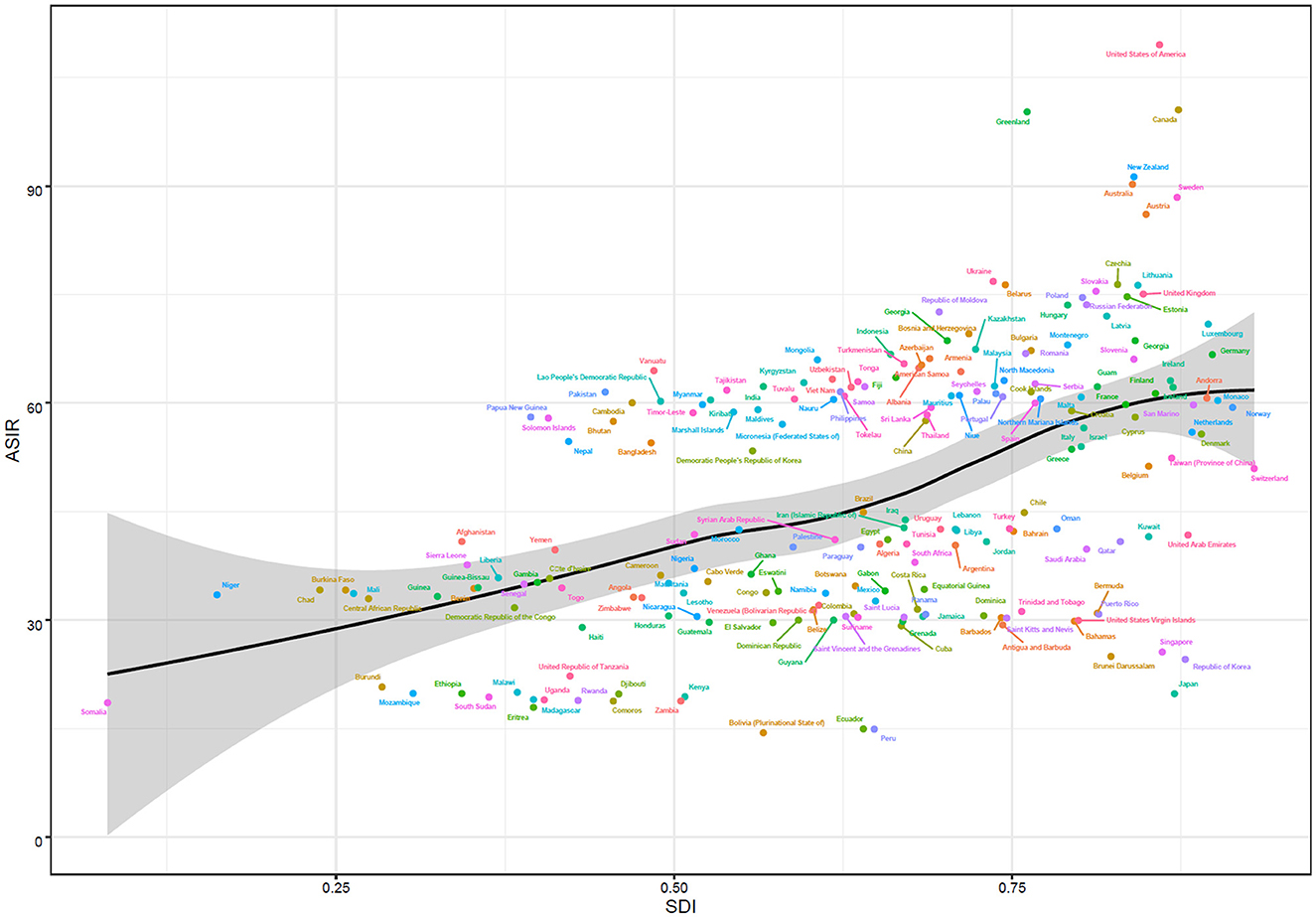
Figure 5. ASIR of AF in 204 countries by SDI, 1990–2019. ASIR, age-standardized incidence rate; SDI, sociodemographic index.
Risk factors for AF
Globally, 219,437 (190,526–249,642) individuals have died from AF. The mortality of AF in 2019 may be attributed to the referring risk factors evaluated by GBD: alcohol use, behavioral risks, a diet high in sodium, a high body mass index (BMI), high systolic blood pressure (SBP), lead exposure, metabolic risks, and smoking. Among them, the two main risk factors were a high BMI and a high SBP. The above risk factors displayed different percentages depending on the sexes at the regional level. For instance, the highest percentage of deaths due to smoking was detected in Central Europe, 52% for males. Simultaneously, the lowest percentage of deaths due to smoking was in High-income Asia Pacific, with 36% for females. In Central Europe, men (37%) and women (14%) had the highest mortality rates due to behavioral risks. Regarding high systolic blood pressure (SBP), the highest proportion of deaths occurred in southern sub-Saharan Africa (men, 41%; women, 43%) (Figure 6).
Discussion
This is the first study to estimate the global burden and trends of AF in older adults aged 60–89 years and to recognize the associated risk factors. The results indicated that the burden of AF is gradually increasing globally, with an ~1.1-fold increase in incidences and an ~1.4-fold increase in deaths from 1990 to 2019. It may be attributable to improved survival with chronic diseases and the global population rising and aging (4, 13, 14). Moreover, the ASIR was higher in high-income North America, Australasia, Eastern Europe, and Central Europe; it was lower in Andean-Latin America, Eastern Sub-Saharan Africa, and high-income Asia Pacific, which was in accordance with the prevalence of AF (13). However, it was worth noting that the rate of increase in the prevalence of AF was extraordinarily rapid in high-income North America and surrounding areas. This observation may be due to the rapidly evolving regional economy, the Westernization tendency of personal diet, and the higher morbidity of cardiovascular problems and metabolic disorders (15).
Our findings also revealed that the degree of disease burden in AF differed between men and women. In general, the number of incident cases was higher in women, but the result of the age-standardized incidence rate was completely opposite, which was consistent with the perspectives of IHME (16). It may be related to our selection of older adults aged 60–89 years as our research subjects. An original research article demonstrated that the incidence rate of AF in women has increased significantly since the age of 60 (10). Longevity in women may be another reason for the increased morbidity of AF (10).
Furthermore, several studies have been conducted to show that estrogen plays a protective role against AF by prolonging the effective refractory period and reducing atrial pressure, which could profoundly interpret the increase in susceptibility to AF in post-menopausal women (17, 18). Andrade et al. also observed a higher prevalence of age-adjusted AF in men than in women (19), which may be partially explained by the lower lifetime risk of AF in women (20, 21). As for mortality, female patients with AF had a higher mortality rate, which may be due to the risk of thromboembolism (22). Previous studies have found female gender to be a major independent risk factor for thromboembolism in patients with AF (23, 24).
At the global level, the values of ASIR and ASDR were far higher than ASMR. Patients with AF were at higher risk for concurrent stroke, heart failure, hypertension, and other cardiovascular diseases than those without arrhythmias (25). In clinical practice, complications and co-morbidities have been documented as the leading cause of death in patients with AF (26). As a result, the actual number of deaths caused by AF may be hard to count, and the estimated disease burden of AF-related deaths is lower than the actual number of deaths. Our analysis also revealed characteristics in incidence, mortality rates, and DALYs in distinct SDI territories. In 2019, both morbidity and mortality were highest in high SDI regions, while the lowest morbidity and mortality occurred in low SDI and middle SDI regions, respectively. However, the most dramatic growth can be discerned in the low and low-middle SDI regions. From 1990 to 2019, ASIR, ASMR, and ASDR showed a decreasing trend in both high SDI and high-moderate SDI quintiles. In addition, the results reflected that the ASIR, ASMR, and ASDR were positively correlated with SDI, which signified that the higher the SDI region, the higher the burden of disease in older adults. These findings were roughly consistent with the research of other scholars (22, 27). Groups with higher access to health care, educational qualifications, and greater health awareness would focus more on their health (28–30). Therefore, AF was more likely to be discovered and reported in areas with a higher SDI. The effective and proven tactics used to manage the burden associated with AF in high SDI regions, such as the United States of America, may serve as a valuable source of policy inspiration for other regions with relatively low SDI quintiles.
Furthermore, we explored the association between ASMR, EAPC, and HDI. HDI is a meaningful indicator to evaluate the level of national social and economic development (31). There was an inverted U-shaped relationship diagram: mid-HDI regions had a higher EAPC of deaths than high-HDI regions. It implied that the ASMR of AF in high HDI areas experienced a decrease while low HDI areas experienced an increase. This may be attributed to the more powerful medical and health services, higher resource allocation, and residents' more aggressive attitude to prevent and treat AF and its complications (32). It was clear from the current study that the disease burden of AF is an urgent concern and an issue that needs to be addressed in less economically developed regions at present and in the future. Hence, it was imperative to establish health- and economic-based AF prevention initiatives for relevant national departments and regional health authorities.
Eventually, we explored the influencing risk factors of AF in older adults based on the GBD database, involving alcohol use, smoking, a diet high in sodium, a high BMI, a high SBP, lead exposure, and metabolic risks. The relationship between AF and the first six risk factors has already been identified (8, 33). Our analysis confirmed that high SBP and high BMI were principal considerations in the burden of AF. Credible evidence has demonstrated that high blood pressure (HBP) is an independent risk element for AF (34–36). A systematic review showed a 50% higher relative risk of AF in patients with HBP compared to those without HBP (37). Each 20 mm Hg increase in systolic blood pressure was associated with a 19% corresponding increase in the risk of atrial fibrillation (38). A few clinical mechanisms might account for the elevated risk of AF in people with HBP. Higher blood pressure leads to an increased risk of coronary artery disease and myocardial infarction (39), which can induce AF (4, 40, 41). Predictable epidemiological findings have demonstrated that increased blood pressure triggers inflammation in myocardial cells, contributing to fibrillation and an enlarged left ventricle (42, 43), which in turn raises the risk of suffering from AF (4, 44).
Furthermore, chronic hypertensive patients may experience impaired left ventricular hypertrophy and left ventricular contraction-diastolic function, which increase atrial pressure and eventually worsen atrial contraction (45). Experts believe controlling blood pressure within the normal range is conducive to reducing the occurrence of AF (46, 47). It is essential to adopt a low-salt diet and engage in home self-monitoring of blood pressure in daily life to prevent the occurrence of hypertension. High SBP and AF often co-exist, and the effect of obesity on AF should not be ignored. A former report highlighted that obesity elevated the risk of AF occurring by ~50% (48). Moreover, every 1 kg/m2 higher BMI was correlated with a 6% increase in risk (49), which was perceived as an independent predictor of incident AF (48, 50). Obesity exerted a proximate effect on cardiac muscle structure through enhanced exposure to oxidative strain (51). AF may be caused by electroanatomic remodeling in patients with a high BMI (52). Additionally, the role of BMI in generating the incidence of AF changed as age advanced. After the age of 60, alterations in physical components, such as increased fat mass and redistribution, may explain the increased influence of a high BMI on the risk of AF with age (53). As for the prognosis for patients with AF, a high BMI would increase the recurrence rate of AF (54) and the risk of paroxysmal atrial fibrillation developing into permanent atrial fibrillation (55). Therefore, weight control and physical exercise play a positive role in improving the prognosis and preventing the worsening of AF. In the future, both doctors and heart specialists are expected to incorporate recommendations on diet and lifestyle improvements, especially for obese older adults, into regular medical care. Moreover, metabolic syndrome may increase susceptibility to AF by activating significant oxidative stress signaling pathways and an inflammatory response (56). Metabolic syndrome is a kind of cardiovascular and metabolic disease that includes elevated blood pressure, overweight, hyperlipidemia, and insulin resistance (57). In the section above, we described the effects of high SBP and high BMI on AF, which contributed most to the increased risk of AF among the components of the metabolic syndrome (58). Considering the important impact of the metabolic syndrome on AF, a low-fat, low-sugar diet and regular monitoring of blood glucose and lipids are essential for formulating targeted AF prevention strategies in older adults. Additionally, we can create prevention and monitoring precautions according to the risk factors in different regions and by gender. For example, South Asia has higher mortality rates due to lead exposure than other regions, so avoiding lead exposure and reducing environmental lead concentrations could be used for AF prevention in South Asia. It was worth mentioning that the attribution proportions for smoking and alcohol consumption were significantly higher for men than for women. For men, quitting smoking and limiting alcohol to prevent the occurrence of AF should be valued.
Based on the findings above, we can conclude that our research is valuable in developing a worldwide strategy for effectively for screening AF in certain groups. More precisely, screening programs targeting risk factors are more effective. First, we should pay special attention to the older female population. Regular electrocardiogram examinations are necessary for them. Second, high SBP and high BMI have the greatest impact on AF. Thus, blood pressure and weight measurements must be included in the screening programs. Finally, we can establish screening plans for other risk factors. Smoking, alcohol consumption, a high-salt diet, and chronic lead exposure are key populations for AF screening, especially in males. In other words, high-risk individuals with AF need to undergo regular medical check-ups in specialized medical institutions with the goal of early screening, timely treatment planning, and delaying the progression of AF.
The current study has several limitations. First, our analysis was impacted by deficiencies in the 2019 GBD study methodology, which have been documented in previous literature (59–61). Insufficient and untimely registration of AF in some underdeveloped regions resulted in the underestimation of patients as well as misdiagnosis or under diagnosis owing to the lack of adequate medical resources. Overall, the data from some countries were not integral, which affected the precision and reliability of the results. Second, the GBD research did not meticulously classify AF into first-diagnosed AF, paroxysmal AF, persistent AF, and so on, based on clinical characteristics. Third, other pathological factors, such as rheumatic heart disease, hyperthyroidism, and pre-excitation syndrome, were not considered. Finally, the outbreak and prevalence of COVID-19 have had a serious impact on the burden of AF (62), and more evidence is urgently needed to compare changes in AF during the epidemic.
Conclusion
In conclusion, AF in older adults is a major public health concern worldwide. The burden of AF varies widely at both national and regional levels. From 1990 to 2019, the cases of AF incidences, deaths, and DALYs have shown a global increase. The ASIR, ASMR, and ASDR have declined in the high-moderate and high SDI regions. However, the burden of AF increased promptly in the lower SDI regions. Moreover, it is necessary to consider the predominant risk factors for AF, such as high BMI and SBP, to encourage individuals with a high risk of AF to perform health management and early screening. By interpreting the burden of AF at different regional and national levels, our research illustrates the features of the global AF burden in pursuit of more effective and targeted prevention and treatment strategies.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
MJ, CL, and QG conducted a statistical analysis of the data. MJ drafted the manuscript. AM and QG conceptualized and designed the research and revised the manuscript. YL and YW collected and sorted the data. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1137230/full#supplementary-material
Supplementary Figure 1. The EAPCs of AF ASRs from 1990 to 2019, both sexes by SDI. SDI, sociodemographic index.
Supplementary Figure 2. The regional burden of AF for both sexes in 2019. (A) ASIR in regions, 1990–2019; (B) ASMR in regions, 1990–2019; (C) ASDR in regions, 1990–2019. ASIR, age-standardized incidence rate; ASMR, age-standardized mortality rate; ASDR, age-standardized DALYs rate.
Supplementary Figure 3. The EAPCs of AF at the regional level, from 1990 to 2019.
Supplementary Figure 4. ASRs of AF in 204 countries by SDI, 1990–2019. (A) ASMR in 204 countries and territories, 2019; (B) ASDR in 204 countries and territories, 2019. ASMR, age-standardized mortality rate; ASDR, age-standardized DALYs rate; SDI, sociodemographic index.
Supplementary Table 1. The incidence of atrial fibrillation between 1990 and 2019 at national level.
Supplementary Table 2. The deaths of atrial fibrillation between 1990 and 2019 at national level.
Supplementary Table 3. The disability-adjusted life years (DALYs) of atrial fibrillation between 1990 and 2019 at national level.
References
1. Fang MC, Chen J, Rich MW. Atrial fibrillation in the older adults. Am J Med. (2007) 120:481–7. doi: 10.1016/j.amjmed.2007.01.026
2. Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. (2017) 70:1–25. doi: 10.1016/j.jacc.2017.04.052
3. Guez D, Boroumand G, Ruggiero NJ, Mehrotra P, Halpern EJ. Automated and manual measurements of the aortic annulus with ECG-gated cardiac CT angiography prior to transcatheter aortic valve replacement: Comparison with 3D-transesophageal echocardiography. Acad Radiol. (2017) 24:587–93. doi: 10.1016/j.acra.2016.12.008
4. Schnabel RB, Yin X, Gona P, Larson MG, Beiser AS, McManus DD, et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: A cohort study. Lancet. (2015) 386:154–62. doi: 10.1016/S0140-6736(14)61774-8
5. Lippi G, Sanchis-Gomar F, Cervellin G. Global epidemiology of atrial fibrillation: An increasing epidemic and public health challenge. Int J Stroke. (2021) 16:217–21. doi: 10.1177/1747493019897870
6. Murray CJ, Lopez AD. Measuring the globalburden of disease. N Engl J Med. (2013) 369:448–57. doi: 10.1056/NEJMra1201534
7. Wang L, Ze F, Li J, Mi L, Han B, Niu H, et al. Trends of global burden of atrial fibrillation/flutter from Global Burden of Disease Study 2017. Heart. (2021) 107:881–7. doi: 10.1136/heartjnl-2020-317656
8. Li H, Song X, Liang Y, Bai X, Liu-Huo WS, Tang C, et al. Global, regional, and national burden of disease study of atrial fibrillation/flutter, 1990-2019: Results from a global burden of disease study, 2019. BMC Public Health. (2022) 22:2015. doi: 10.1186/s12889-022-14403-2
9. Osorio J, Mansour M, Melby D, Imhoff RJ, Hunter TD, Maccioni S, et al. Economic evaluation of contact force catheter ablation for persistent atrial fibrillation in the United States. Heart Rhythm O2. (2022) 3:647–55. doi: 10.1016/j.hroo.2022.09.011
10. Magnussen C, Niiranen TJ, Ojeda FM, Gianfagna F, Blankenberg S, Njølstad I, et al. Sex differences and similarities in atrial fibrillation epidemiology, risk factors, and mortality in community cohorts: Results from the BiomarCaRE Consortium (Biomarker for Cardiovascular Risk Assessment in Europe). Circulation. (2017) 136:1588–97. doi: 10.1161/CIRCULATIONAHA.117.028981
11. Global Burden of Disease Collaborative Network. Global Burden ofDisease Study 2016 (GBD 2016) Results. Seattle, United States: Institutefor Health Metrics and Evaluation (IHME) (2017). Available from http://ghdx.healthdata.org/gbd-results-tool.
12. Liu Z, Jiang Y, Yuan H, Fang Q, Cai N, Suo C, et al. The trends in incidence of primary liver cancer caused by specific etiologies: Results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. J Hepatol. (2019) 70:674–83. doi: 10.1016/j.jhep.2018.12.001
13. Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, et al. Worldwide epidemiology of atrial fibrillation: A Global Burden of Disease 2010 Study. Circulation. (2014) 129:837–47. doi: 10.1161/CIRCULATIONAHA.113.005119
14. Fordyce CB, Roe MT, Ahmad T, Libby P, Borer JS, Hiatt WR, et al. Cardiovascular drug development: Is it dead or just hibernating? J Am Coll Cardiol. (2015) 65:1567–82. doi: 10.1016/j.jacc.2015.03.016
15. Bhagavathula AS, Shehab A, Ullah A, Rahmani J. The burden of cardiovascular disease risk factors in the Middle East: A systematic review and Meta-analysis focusing on primary prevention. Curr Vasc Pharmacol. (2021) 19:379–89. doi: 10.2174/1573406416666200611104143
16. Institute for Health Metrics Evaluation. GBD Compare Data Visualization. Seattle, WA: IHME, University of Washington (2018). Available online at: http://vizhub.healthdata.org/gbd-compare (accessed June 3, 2020).
17. Tse HF, Oral H, Pelosi F, Knight BP, Strickberger SA, Morady F. Effect of gender on atrial electrophysiologic changes induced by rapid atrial pacing and elevation of atrial pressure. J Cardiovasc Electrophysiol. (2001) 12:986–9. doi: 10.1046/j.1540-8167.2001.00986.x
18. Westerman S, Wenger N. Gender differences in atrial fibrillation: A review of epidemiology, management, and outcomes. Curr Cardiol Rev. (2019) 15:136–44. doi: 10.2174/1573403X15666181205110624
19. Andrade JG, Deyell MW, Lee AYK, Macle L. Sex differences in atrial fibrillation. Can J Cardiol. (2018) 34:429–36. doi: 10.1016/j.cjca.2017.11.022
20. Ko D, Rahman F, Schnabel RB, Yin X, Benjamin EJ, Christophersen IE. Atrial fibrillation in women: Epidemiology, pathophysiology, presentation, and prognosis. Nat Rev Cardiol. (2016) 13:321–32. doi: 10.1038/nrcardio.2016.45
21. Alonso A, Agarwal SK, Soliman EZ, Ambrose M, Chamberlain AM, Prineas RJ, et al. Incidence of atrial fibrillation in whites and African-Americans: The Atherosclerosis Risk in Communities (ARIC) study. Am Heart J. (2009) 158:111–7. doi: 10.1016/j.ahj.2009.05.010
22. Zhang J, Johnsen SP, Guo Y, Lip GYH. Epidemiology of atrial fibrillation: Geographic/ecological risk factors, age, sex, genetics. Card Electrophysiol Clin. (2021) 13:1–23. doi: 10.1016/j.ccep.2020.10.010
23. Fang MC, Singer DE, Chang Y, Hylek EM, Henault LE, Jensvold NG, et al. Gender differences in the risk of ischemic stroke and peripheral embolism in atrial fibrillation: the AnTicoagulation and risk factors in atrial fibrillation (ATRIA) study. Circulation. (2005) 112:1687–91. doi: 10.1161/CIRCULATIONAHA.105.553438
24. Lip GYH, Nieuwlaat R, Pisters R, Lane DA, Crijns HJGM. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: The euro heart survey on atrial fibrillation. Chest. (2010) 137:263–72. doi: 10.1378/chest.09-1584
25. Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: A report from the American Heart Association. Circulation. (2020) 141:e139–596. doi: 10.1161/CIR.0000000000000757
26. Deshpande S, Catanzaro J, Wann S. Atrial fibrillation: Prevalence and scope of the problem. Card Electrophysiol Clin. (2014) 6:1–4. doi: 10.1016/j.ccep.2013.10.006
27. Freedman B, Hindricks G, Banerjee A, Baranchuk A, Ching CK, Du X, et al. World heart federation roadmap on atrial fibrillation—A 2020 update. Glob Heart. (2021) 16:41. doi: 10.5334/gh.1023
28. Zhang Y, Su D, Chen Y, et al. Effect of socioeconomic status on the physical and mental health of the older adults: The mediating effect of social participation. BMC Public Health. (2022) 22:605. doi: 10.1186/s12889-022-13062-7
29. Lövdén M, Fratiglioni L, Glymour MM, Lindenberger U, Tucker-Drob EM. Education and cognitive functioning across the life span. Psychol Sci Public Interest. (2020) 21:6–41. doi: 10.1177/1529100620920576
30. Ding D, Zhao Q, Wu W, Xiao Z, Liang X, Luo J, et al. Prevalence and incidence of dementia in an older Chinese population over two decades: The role of education. Alzheimers Dement. (2020) 16:1650–62. doi: 10.1002/alz.12159
31. Veisani Y, Jenabi E, Khazaei S, Nematollahi S. Global incidence and mortality rates in pancreatic cancer and the association with the Human Development Index: Decomposition approach. Public Health. (2018) 156:87–91. doi: 10.1016/j.puhe.2017.12.015
32. Chugh SS, Roth GA, Gillum RF, Mensah GA. Global burden of atrial fibrillation in developed and developing nations. Glob Heart. (2014) 9:113–9. doi: 10.1016/j.gheart.2014.01.004
33. Xu S, Chen Y, Lin R, Huang W, Zhou H, Lin Y, et al. Burden of atrial fibrillation and its attributable risk factors from 1990 to 2019: An analysis of the Global Burden of Disease study 2019. Front Cardiovasc Med. (2022) 9:997698. doi: 10.3389/fcvm.2022.997698
34. Wingerter R, Steiger N, Burrows A, Estes NAM. Impact of lifestyle modification on atrial fibrillation. Am J Cardiol. (2020) 125:289–97. doi: 10.1016/j.amjcard.2019.10.018
35. Morin DP, Bernard ML, Madias C, Rogers PA, Thihalolipavan S. The state of the art: Atrial fibrillation epidemiology, prevention, and treatment. Mayo Clin Proc. (2016) 91:1778–810. doi: 10.1016/j.mayocp.2016.08.022
36. Manolis AJ, Rosei EA, Coca A, Cifkova R, Erdine SE, Kjeldsen S, et al. Hypertension and atrial fibrillation: Diagnostic approach, prevention and treatment. Position paper of the Working Group “Hypertension Arrhythmias and Thrombosis” of the European Society of Hypertension. J Hypertens. (2012) 30:239–52. doi: 10.1097/HJH.0b013e32834f03bf
37. Cameron A, Cheng HK, Lee R-P, Doherty D, Hall M, Khashayar P, et al. Biomarkers for atrial fibrillation detection after stroke: Systematic review and meta-analysis. Neurology. (2021) 97:e1775–89. doi: 10.1212/WNL.0000000000012769
38. Nazarzadeh M, Pinho-Gomes A-C, Bidel Z, Canoy D, Dehghan A, Byrne KS, et al. Genetic susceptibility, elevated blood pressure, and risk of atrial fibrillation: A Mendelian randomization study. Genome Med. (2021) 13:38. doi: 10.1186/s13073-021-00849-3
39. Rapsomaniki E, Timmis A, George J, Pujades-Rodriguez M, Shah AD, Denaxas S, et al. Blood pressure and incidence of twelve cardiovascular diseases: Lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet. (2014) 383:1899–911. doi: 10.1016/S0140-6736(14)60685-1
40. Alonso A, Krijthe BP, Aspelund T, Stepas KA, Pencina MJ, Moser CB, et al. Simple risk model predicts incidence of atrial fibrillation in a racially and geographically diverse population: The CHARGE-AF consortium. J Am Heart Assoc. (2013) 2:e000102. doi: 10.1161/JAHA.112.000102
41. Khurshid S, Choi SH, Weng L-C, Wang EY, Trinquart L, Benjamin EJ, et al. Frequency of cardiac rhythm abnormalities in a half million adults. Circ Arrhythm Electrophysiol. (2018) 11:e006273. doi: 10.1161/CIRCEP.118.006273
42. Cao X, Broughton ST, Waits GS, Nguyen T, Li Y, Soliman EZ. Interrelations between hypertension and electrocardiographic left ventricular hypertrophy and their associations with cardiovascular mortality. Am J Cardiol. (2019) 123:274–83. doi: 10.1016/j.amjcard.2018.10.006
43. Soliman EZ, Byington RP, Bigger JT, Evans G, Okin PM, Goff DC, et al. Effect of intensive blood pressure lowering on left ventricular hypertrophy in patients with diabetes mellitus: Action to control cardiovascular risk in diabetes blood pressure trial. Hypertension. (2015) 66:1123–9. doi: 10.1161/HYPERTENSIONAHA.115.06236
44. Ogunmoroti O, Michos ED, Aronis KN, Salami JA, Blankstein R, Virani SS, et al. Life's Simple 7 and the risk of atrial fibrillation: The Multi-Ethnic Study of Atherosclerosis. Atherosclerosis. (2018) 275:174–81. doi: 10.1016/j.atherosclerosis.2018.05.050
45. Gumprecht J, Domek M, Lip GYH, Shantsila A. Invited review: Hypertension and atrial fibrillation: epidemiology, pathophysiology, and implications for management. J Hum Hypertens. (2019) 33:824–36. doi: 10.1038/s41371-019-0279-7
46. Chen C, Liu L, Yu Y, Shen G, Huang J, Huang Y, et al. Association of systolic blood pressure with atrial fibrillation among treated hypertensive patients. Ann Palliat Med. (2020) 9:1752–63. doi: 10.21037/apm-19-649
47. Kim D, Yang P-S, Kim T-H, Jang E, Shin H, Kim HY, et al. Ideal blood pressure in patients with atrial fibrillation. J Am Coll Cardiol. (2018) 72:1233–45. doi: 10.1016/j.jacc.2018.05.076
48. Wanahita N, Messerli FH, Bangalore S, Gami AS, Somers VK, Steinberg JS. Atrial fibrillation and obesity—Results of a meta-analysis. Am Heart J. (2008) 155:310–5. doi: 10.1016/j.ahj.2007.10.004
49. Zhao M, Song L, Zhao Q, Chen Y, Li B, Xie Z, et al. Elevated levels of body mass index and waist circumference, but not high variability, are associated with an increased risk of atrial fibrillation. BMC Med. (2022) 20:215. doi: 10.1186/s12916-022-02413-1
50. Korantzopoulos P, Kolettis TM. Obesity and the risk of new-onset atrial fibrillation. J Am Med Assoc. (2004) 292:2471–7. doi: 10.1001/jama.292.20.2471
51. Vincent HK, Powers SK, Stewart DJ, Shanely RA, Demirel H, Naito H. Obesity is associated with increased myocardial oxidative stress. Int J Obes Relat Metab Disord. (1999) 23:67–74. doi: 10.1038/sj.ijo.0800761
52. Lavie CJ, Pandey A, Lau DH, Alpert MA, Sanders P. Obesity and atrial fibrillation prevalence, pathogenesis, and prognosis: Effects of weight loss and exercise. J Am Coll Cardiol. (2017) 70:2022–35. doi: 10.1016/j.jacc.2017.09.002
53. Senoo K, Nakata M, Teramukai S, Yamamoto T, Nishimura H, Matoba S. Age-specific association between body mass index and the incidence of atrial fibrillation in Japanese men. Circ Rep. (2020) 2:466–70. doi: 10.1253/circrep.CR-20-0067
54. Guglin M, Maradia K, Chen R, Curtis AB. Relation of obesity to recurrence rate and burden of atrial fibrillation. Am J Cardiol. (2011) 107:579–82. doi: 10.1016/j.amjcard.2010.10.018
55. Tsang TSM, Barnes ME, Miyasaka Y, Cha SS, Bailey KR, Verzosa GC, et al. Obesity as a risk factor for the progression of paroxysmal to permanent atrial fibrillation: A longitudinal cohort study of 21 years. Eur Heart J. (2008) 29:2227–33. doi: 10.1093/eurheartj/ehn324
56. Tadic M, Ivanovic B, Cuspidi C. What do we currently know about metabolic syndrome and atrial fibrillation? Clin Cardiol. (2013) 36:654–62. doi: 10.1002/clc.22163
57. Yu S, Guo X, Li G, Yang H, Zheng L, Sun Y. Gender discrepancies in predictors for newly onset cardiovascular events and metabolic syndrome in older adults patients from rural China. Front Cardiovasc Med. (2022) 9:995128. doi: 10.3389/fcvm.2022.995128
58. Watanabe H, Tanabe N, Watanabe T, Darbar D, Roden DM, Sasaki S, et al. Metabolic syndrome and risk of development of atrial fibrillation: the Niigata preventive medicine study [published correction appears in Circulation. 2010 Aug 17;122:e433]. Circulation. (2008) 117:1255–60. doi: 10.1161/CIRCULATIONAHA.107.744466
59. GBD 2016 Mortality Collaborators. Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. (2017) 390:1084–150. doi: 10.1016/S0140-6736(17)31833-0
60. GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. (2017) 390:1211–59. doi: 10.1016/S0140-6736(17)32154-2
61. GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. (2017) 390:1151–210. doi: 10.1016/S0140-6736(17)32152-9
Keywords: atrial fibrillation, aging, Global Burden of Disease, risk factors, older adults
Citation: Jiao M, Liu C, Liu Y, Wang Y, Gao Q and Ma A (2023) Estimates of the global, regional, and national burden of atrial fibrillation in older adults from 1990 to 2019: insights from the Global Burden of Disease study 2019. Front. Public Health 11:1137230. doi: 10.3389/fpubh.2023.1137230
Received: 04 January 2023; Accepted: 12 May 2023;
Published: 12 June 2023.
Edited by:
Edwin Van Teijlingen, Bournemouth University, United KingdomReviewed by:
Shilpa Gaidhane, Datta Meghe Institute of Medical Sciences, IndiaGuglielmo M. Trovato, University of Catania, Italy
Cosmin Mihai Vesa, University of Oradea, Romania
Copyright © 2023 Jiao, Liu, Liu, Wang, Gao and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anning Ma, man@wfmc.edu.cn; Qianqian Gao, wfgaoqq@163.com
†These authors have contributed equally to this work
 Min Jiao
Min Jiao Chenglin Liu2†
Chenglin Liu2† Yongwen Liu
Yongwen Liu Qianqian Gao
Qianqian Gao Anning Ma
Anning Ma