- 1Department of Counseling Psychology and Human Services, University of Oregon, Eugene, OR, United States
- 2Prevention Science Institute, University of Oregon, Eugene, OR, United States
- 3Department of Special Education and Clinical Sciences, University of Oregon, Eugene, OR, United States
- 4Department of Global Studies, Center for Global Health, University of Oregon, Eugene, OR, United States
- 5Institute of Ecology and Evolution, University of Oregon, Eugene, OR, United States
- 6Presidential Initiative in Data Science, University of Oregon, Eugene, OR, United States
Background: Latinx communities are disproportionately affected by COVID-19 compared with non-Latinx White communities in Oregon and much of the United States. The COVID-19 pandemic presents a critical and urgent need to reach Latinx communities with innovative, culturally tailored outreach and health promotion interventions to reduce viral transmission and address disparities. The aims of this case study are to (1) outline the collaborative development of a culturally and trauma-informed COVID-19 preventive intervention for Latinx communities; (2) describe essential intervention elements; and (3) summarize strengths and lessons learned for future applications.
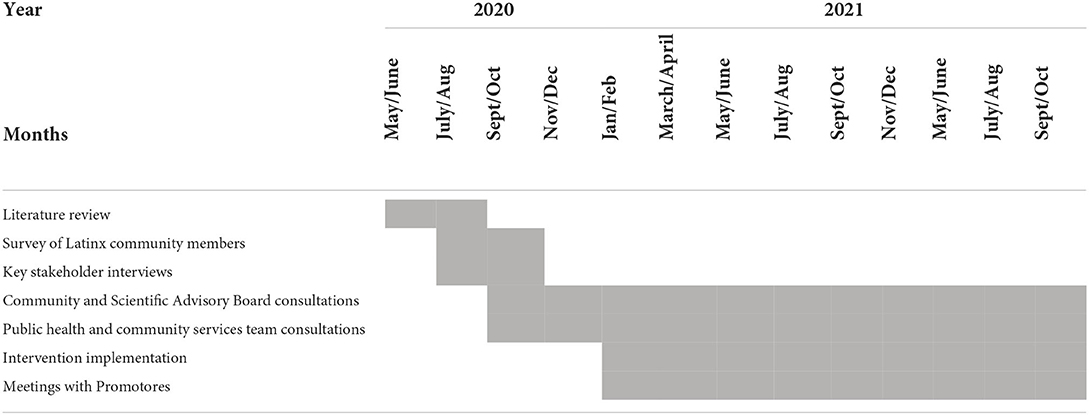
Methods: Between June 2020 and January 2021, a multidisciplinary team of researchers and Latinx-serving partners engaged in the following intervention development activities: a scientific literature review, a survey of 67 Latinx residents attending public testing events, interviews with 13 leaders of community-based organizations serving Latinx residents, and bi-weekly consultations with the project's Public Health and Community Services Team and a regional Community and Scientific Advisory Board. After launching the intervention in the field in February 2021, bi-weekly meetings with interventionists continuously informed minor iterative refinements through present day.
Results: The resulting intervention, Promotores de Salud, includes outreach and brief health education. Bilingual, trauma-informed trainings and materials reflect the lived experiences, cultural values, needs, and concerns of Latinx communities. Interventionists (21 Promotores) were Latinx residents from nine Oregon counties where the intervention was delivered.
Conclusions: Sharing development and intervention details with public health researchers and practitioners facilitates intervention uptake and replication to optimize the public health effect in Oregon's Latinx communities and beyond.
Introduction
U.S. born and immigrant Hispanic/Latino/a/x [henceforth referred to as Latinx; (1)] persons have been disproportionately affected by the COVID-19 pandemic (2, 3). In the early months, Latinx and Spanish-speaking individuals were both less likely to get tested, and more likely to test positive for SARS-CoV-2 — the virus that causes COVID-19 (4, 5). Latinx residents constitute 13.9% of the population in Oregon (6), but in Mid-May of 2020 accounted for 31.7% of the state's COVID-19 cases (7). By July of 2020, weekly cases for Oregon's Latinx residents were 174.7 per 100,000, and only 28.1 per 100,000 for non-Latinx Whites (8). The mortality rate was also higher for Latinx residents even though Oregon's Latinx population is much younger than the non-Latinx White population (e.g., median age of 24 vs. 41 years, respectively) (9, 10). Testing for SARS-CoV-2 is critical to prevention and control (11). This case study describes the development and essential elements of an innovative culturally and trauma-informed intervention designed to increase SARS-CoV-2 testing, and decrease transmission, among Latinx communities in Oregon.
Background and rationale
The need for tailored interventions for Latinx community members
The Latinx population of Oregon has grown by 31% since 2010 and is the largest ethnically minoritized group in the state (6). The majority (85%) are of Mexican origin, and 70% speak a language other than English at home (10), predominantly Spanish, but also including 0.6% who speak Mam, Mixtec, Tzotzil, or another indigenous language of Mexico or Central America (12). Oregon's Latinx residents are much more likely to live in poverty, lack health insurance, and experience food insecurity than non-Latinx Whites (10, 13). Oregon's undocumented immigrants, 77% of whom are Latinx (14), are often employed in what the Department of Homeland Security deemed “critical infrastructure” roles — such as agriculture and food processing — and these workers have been disproportionately affected by job loss, contagion, and death during the pandemic (15) but are not eligible for federal pandemic stimulus benefits (16, 17). Lack of health insurance, pre-existing health conditions, employment as essential workers, lack of access to protective gear, and language barriers increase vulnerability to COVID-19 (18). Efforts to mitigate SARS-CoV-2 spread among Latinx communities must account for these factors and provide access to testing (2, 4, 5, 19, 20).
Ongoing inequities in healthcare and education (2), chronic stress associated with anti-immigration policies (21), and trauma from the disproportionate effects of COVID-19 including inadequate workplace protections from the virus, sudden job loss, hospitalization, and death combine with sociopolitical histories of oppression to decrease trust in government authorities and programs and necessitate trauma-informed approaches to engage Latinx communities in SARS-CoV-2 testing and prevention efforts (2, 17, 21). Trauma-informed approaches to behavioral health services recognize the prevalence of trauma, how it is manifested, and its multifaceted effects on individuals and communities, emphasize physical, psychological, and emotional safety for both users and providers of the services, promote and support user agency, and utilize practices and procedures that minimize the likelihood of re-traumatization (22). We developed and delivered our innovative health promotion intervention using a trauma-informed approach, as recommended but little researched with Latinx communities (23).
Case study purpose
Disparities in SARS-CoV-2 testing and contagion showed that Oregon Latinx communities were not being served by standard outreach and health promotion practices. Our team aimed to develop an innovative culturally tailored and trauma-informed intervention to increase SARS-CoV-2 testing and engagement in preventive behaviors among Oregon Latinx communities. A community-based participatory research (CBPR) approach was followed as much as possible by soliciting and incorporating experiences, ideas, and feedback from community stakeholders, who were members of the communities we aimed to serve, at every step of the intervention development and refinement process to promote knowledge transfer, ownership of the intervention's success, and sustainability (24–26). The purpose of this case study is to describe intervention development activities and the resulting Promotores de Salud intervention to facilitate replication and optimize potential public health effects. Integrated throughout are the items from the GUIDED (GUIDance for the rEporting of intervention Development) checklist by Duncan and colleagues (27) and Smith, Levkoff and Ory's (28) list of key components of a community case study.
Methods
This project, entitled Oregon Saludable: Juntos Podemos, was part of a national effort to increase SARS-CoV-2 testing among underserved populations funded through the National Institutes of Health Rapid Acceleration of Diagnostics for Underserved Populations (RADx-UP) initiative. The request for RADx-UP proposals was made in June 2020 and notice of award in September 2020. Community leaders who later became members of the Community and Scientific Advisory Board (CSAB) or Public Health and Community Services Team provided input on the study design and approach. A multidisciplinary team of researchers from public health, language and communication sciences, counseling psychology, prevention science, and sociocultural anthropology at the University of Oregon led the intervention development and implementation in close collaboration with a multi-sector team that spanned the state, including researchers, community-based organizations (CBOs), local and state health departments, and a CSAB. The design of the larger study included random assignment of testing sites within counties to intervention or outreach-as-usual conditions. Primary intervention development activities were informed by CDC recommended community assessment methods for promoting health equity, including reviewing existing data and evidence and conducting surveys and interviews (29). These primary intervention development activities occurred between June 2020 and January 2021 (Table 1). The intervention was launched in the field in February 2021, and refinement continues with input from our stakeholder groups. All study activities that involved human subjects were approved by the University of Oregon Institutional Review Board (IRB).
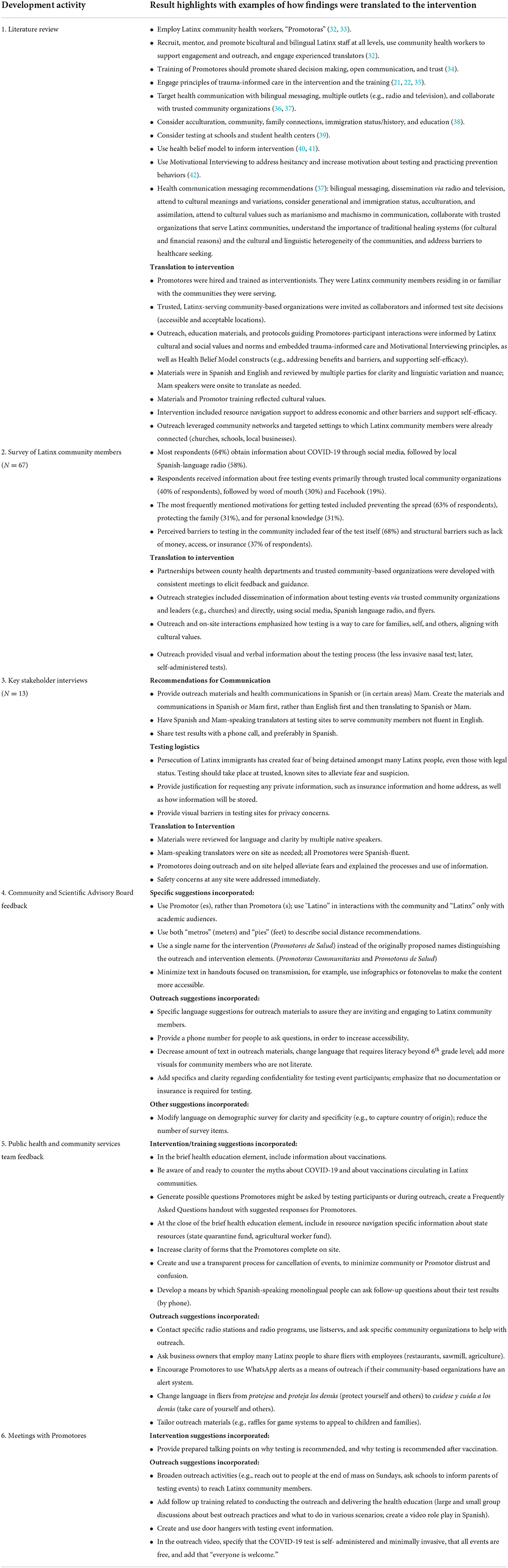
Activity 1: Literature review
In Summer 2020, the first author and two research assistants conducted a review of the scientific literature between 2005–2020 on culturally tailored public health and medical interventions for Latinx patients or communities in the United States. The following MeSH terms were included in PubMed and Google Scholar searches: Hispanic or Latino, United States, prevention and control, cultural competency. Reports on best public health or medical practices among Hispanic or Latino/a/x individuals by organizations such as the CDC, U.S. Department of Health and Human Services Office of Minority Health, and American Psychiatric Association were also included in the review. Research assistants created an annotated bibliography focusing on evidence-supported intervention and outreach practices related to caring for and reaching Latinx community members and noted theoretical frameworks that informed this literature.
Activity 2: Survey of Latinx community members
Between July and October 2020, a researcher on the CSAB and a research assistant visited all nine SARS-CoV-2 testing events, organized by the Lane County (Oregon) Public Health Department, that targeted Latinx and Spanish speaking community members through outreach in Spanish and through Latinx-serving CBOs. Using convenience sampling, community members were approached while they waited in line for testing. If a family was in line together, the researcher asked if one of the adults would be interested in hearing about the survey. The survey purpose and procedure were explained in the preferred language (Spanish or English) expressed by the community member. If interest was expressed, community members' eligibility was confirmed (≥ 18 years and identified as Hispanic or Latino/a/x) and they were consented and surveyed after they completed SARS-CoV-2 testing. Approximately five eligible adults who were approached about the study declined to participate. No incentives were provided for participation. Sixty-seven Latinx community members completed the 3–5-min survey using the Epicollect5 (https://five.epicollect.net) app. The final sample size was the maximum number of eligible adults the investigator was able to invite to the participate, given the time it took to conduct each informed consent and survey, minus the individuals who declined across visited testing events.
The 11-question survey was informed by the Health Belief Model (e.g., perceived benefits, barriers, and threat), feedback from local health department practitioners, and questions/concerns expressed by community members through the local COVID-19 public hotline. The survey assessed: how participants heard about the testing events; from what sources they obtain COVID-19 information; reasons for seeking testing; perceptions of why others in their community may be reluctant to seek testing; ways the pandemic had affected themselves and their families; the industry in which they primarily work; and whether participants had health insurance, were employed, had lost a job due to the pandemic, were exposed to COVID-19 risks at their job, and were aware of state financial resources available to those who had lost a job or had been adversely affected by the pandemic. The researcher chose not to collect additional socio-demographic information in the survey in order to receive the fastest possible IRB review and approval. This trade-off allowed for the data collection at these limited-time events but prohibited any assessment of who is or is not represented in the sample beyond that participants were all adults, Latinx, and opted to participate in Spanish.
Activity 3: Key stakeholder interviews
Between July and September 2020, key community stakeholders (defined as leaders of CBOs that predominantly serve Latinx community members in Lane County) were purposely selected and invited to participate in interviews. The purpose of these interviews was to inform COVID-19 testing event protocols and related communications to maximize acceptability, feasibility, and reach among Latinx community members. Participating stakeholders underwent informed consent and completed a 45–60-min, one-on-one interview via Zoom. Informed by Guest, Namey, and Chen's (16) recommendations, the study team determined that thematic saturation was reached within the 13 completed interviews. Three research assistants, trained and supervised by the first-and sixth author, carried out all informed consent processes, interviews, and analyses in English.
The semi-structured interview guide included 44 questions informed by the Elaboration Likelihood Model of Persuasion (30). First, demographic information was assessed on the stakeholders and community members they serve. Then, stakeholders' feedback on three primary domains was gathered, including (1) testing event messaging and communication channels for promoting testing events; (2) on-site testing event logistics, protocols, and staff; and (3) methods for sharing of test results. Stakeholders responded to each interview question, first reflecting their own preferences, and then reflecting those of the community members they serve. Importantly, the latter questions aimed to learn from the stakeholders' expertise in serving Latinx community members, rather than serving as a proxy for Latinx community members' voices.
The interviews were audio-recorded and transcribed using Zoom, transcriptions were edited by research assistants, and analyzed using a conventional content analytic approach, starting with the interview guide questions as an a priori framework (31). After achieving consensus on the identified themes, a final review of transcripts was conducted to identify any potential additional themes that were distinct from or counter to existing themes; none were identified.
Activity 4: Community and Scientific Advisory Board consultations
To provide guidance on the community, cultural, and linguistic responsiveness of the research study, a CSAB was established in September 2020. The CSAB met monthly via Zoom, from September 2020 to the present, to review and provide feedback on study operations and materials. CSAB consisted of eight individuals with expertise in COVID-19 public health response at the state and county levels, inclusive of members of Oregon's Health Equity Committee, research investigators who specialize in Latinx populations, and members of CBOs and behavioral health organizations with experience working with immigrant and Latinx families. By design, CSAB members had high levels of Spanish proficiency, included young and middle-aged adults, had work and/or lived experiences with Latinx communities across different regions of Oregon, and had heritages in various Latin American countries. At least one investigator and staff person from the research team also attended the CSAB meetings. Examples of agenda items included review of intervention materials and Promotores' training materials.
Activity 5: Public health and community services team consultations
October 2020 through August 2021, 2–3 members of the research team met weekly with a group of 5–8 Lane County Latinx-serving social services providers, including individuals from a local CBO and from the local health department's Latinx Outreach Team. These professionals were Spanish-English bilingual and identified as Latinx. Meetings took place over Zoom and followed an agenda co-established at the beginning of each meeting. Initial meetings focused on the purpose of the intervention, constraints and resources associated with the project, and the initial vision for the intervention. As the intervention evolved, the associated materials, trainings, content, and scripts were presented iteratively to this team and feedback was incorporated.
Activity 6: Meetings with Promotores
From February 2021 through present, approximately two interventionists (Promotores) in each of nine counties were hired to deliver the intervention. The research team contracted with partner CBOs, and CBOs hired the Promotores. Although the research team offered hiring guidelines (connected to local community, bicultural, Spanish and English-speaking), CBOs hired Promotores independent of the research team. Because these CBOs were well-established and predominately served local Latinx community members, they had experience hiring employees responsive to community members' needs. All Promotores identified as Hispanic or Latino/a/x and were connected to their counties' Latinx communities, largely by residence and/or employment. Approximately 44% of the Promotores had a high school diploma or GED, 19% had a college degree, 13% had some college, 6% did not report; annual income ranged from $4,500–$60,000 (M = $27,375, SD = $14,160); 50% were born in the United States; 20% had a parent born in the United States; 25% reported Spanish as their primary language, 31%, English, and 44% both English and Spanish equivalently. Promotores participated in bi-weekly meetings via Zoom, facilitated by several investigators on the research team, in order to continuously refine the intervention for optimal implementation and effectiveness. During these meetings, investigators solicited interventionists' feedback on barriers and facilitators to intervention delivery, and possible adaptations, clarifications, or additional materials that would improve intervention delivery and/or better serve the needs of the Latinx residents in their counties. These meetings also offered a space to collaboratively review intervention materials, practice and receive feedback on Promotores' delivery of the intervention, and receive support related to implementation challenges. Promotores also had the opportunity to reflect on ways in which their own stress, traumas, and lived experiences more generally might impact them in their role when engaging with community members. Additional check-ins provided space for Promotores to share in a smaller group setting and address more county and Promotor-specific issues. In addition, research team members reached out to each partner CBO and affiliated Promotores at least bi-weekly via email or Zoom to answer questions, help problem solve, and exchange ideas.
Results
Table 2 summarizes the key findings generated by each activity reported in the Methods section and how the information informed the Promotores de Salud intervention. The first three activities (the literature review, survey of Latinx community members, and interviews with key stakeholders), were conducted prior to initiating development of the intervention. The latter three activities (CSAB consultations, Public Health and Community Services Team consultations, and Promotores meetings) reflect ongoing iterative processes through which feedback was sought and incorporated over time as the intervention was implemented in the field. While the survey and interview data were collected among residents of Lane County, continuous input from Promotores and CSAB members ensured that intervention development was sensitive to contextual differences across counties. Promotores de Salud was associated with three and a half more Latinx community members engaged in testing compared with outreach-as-usual sites, representing a medium-to-large effect size (0.70). Evaluation results and how testing sites were selected to optimize convenience and familiarity to Latinx communities are reported elsewhere (43, 44). Details of the implementation approach, guiding frameworks, and findings will be outlined in forthcoming articles.
Essential elements of the intervention
The Promotores de Salud intervention had two essential elements: outreach and brief health education. Both elements reflected culturally tailored, evidence- and trauma-informed strategies generated by intervention development activities described above. The intervention elements were delivered by bicultural, Spanish and English-speaking Promotores, similar to community health workers (36). The majority of the 21 Promotores lived in the county in which they served and were intricately connected to the local Latinx community (45), and were hired by partner CBOs that predominantly serve Latinx community members. Employing members of the local Latinx community is a CDC recommended strategy for effective health education (32, 46–48), and Promotores help facilitate the trust and respect necessary for effective study recruitment (48–50). Promotores can be highly effective at recruitment for health-related interventions among all ages of Latinx people (51). Distinct from typical community health worker models, Promotores were only trained on COVID-19 prevention and control, rather than multiple public health topics, and were trained through the research study rather than a standardized training program, such as a state certification (52). Additionally, Promotores tracked data on the reach and fidelity of intervention delivery. Each Promotores de Salud element is outlined next, followed by an overview of the training and description of how trauma-informed care and motivational interviewing practices were embedded.
The purposes of the outreach element were to build relationships with Latinx community members and with predominately Latinx-serving CBOs and to advertise and promote participation in the SARS-CoV-2 testing events. Promotores shared outreach materials including Spanish and English flyers, door hangers, radio announcements, WhatsApp telephone application messages, and social media messages (e.g., Facebook, Instagram) among Latinx community members directly and through well-established Latinx serving organizations (see Supplementary materials for example). These organizations included grocery stores and Mexican markets, churches, schools, community mental health centers, the regional farmworkers union, and the Women, Infant, and Children program. When relevant, Promotores would ask organizational leaders (e.g., priest, principal) to aid in promoting the testing events among their constituents. Outreach materials included logistical information about when and where testing would occur, that testing was free, and that documentation status was not relevant. Promotores determined the optimal outreach strategies to use in their communities. Promotores verbally reinforced the information on the outreach materials and provided additional details about the testing process (e.g., anterior nares swab vs. nasopharyngeal swab) and what information would (e.g., name and date of birth, contact information) and would not be requested of them (e.g., proof of citizenship or health insurance). Outreach materials and interactions reflected constructs of the Health Belief Model (40, 41) by emphasizing Latinx community values supportive of testing engagement, acknowledging that Latinx people are hard workers, often essential workers, whose employment necessitates interaction with others, and that testing contributes to collective welfare and provides information to help keep families and the community safe (42).
The purposes of the brief health education element of the intervention were to promote COVID-19 preventive behaviors and to help sustain testing rates of Latinx community members over time. This health education element also reflected the Health Belief Model including perceived barriers, benefits, threat, self-efficacy and cues to action (40, 41). Typically, a Promotor greeted community members who drove up to the testing event, then asked whether the person was willing to hear a 5-min overview of COVID-19 preventive behaviors while waiting in the line of cars to get tested. If the community member was interested, the Promotor offered verbal instruction on effective mask wearing, hand washing, physical distancing, repeated testing, as well as the benefits of practicing these behaviors. After vaccines began to be widely available (approximately May 2021), the benefits of getting vaccinated was a fifth preventive behavior added to the health education element. During the verbal instruction, the Promotor presented a flier in the community member's preferred language with illustrations and brief explanations for each behavior (see Supplementary materials). Participants were invited to ask questions and share any concerns or hesitations. They were given a flier to take home and encouraged to bring a friend or family member to the next testing event.
The brief health education element closed with offering resources, and navigation support as needed, in recognition of the multifaceted barriers faced by Latinx community members in accessing services (2, 19). Materials for this resource navigation support included a customized list of local and state resources (e.g., food banks, social services, and information regarding funds for agricultural workers who missed work due to quarantine or positive test results) and informational handouts focused on how to prevent further viral spread if they or a family member tested positive.
Prior to launching the training of Promotores, a pilot test of the intervention was conducted at two testing events, with members of the research team serving as proxy Promotores. These experiences informed the scope and content of the Promotor training, as well as the order of operations at testing events. For example, the research team began by offering the health education after community members were tested, but at that point most community members had accomplished what they came for and declined the additional education in order to be on their way. When the research team changed to delivering the health education prior to community members getting tested, (thereby taking advantage of the time they were waiting in line to be tested), receptivity to the health education improved substantially.
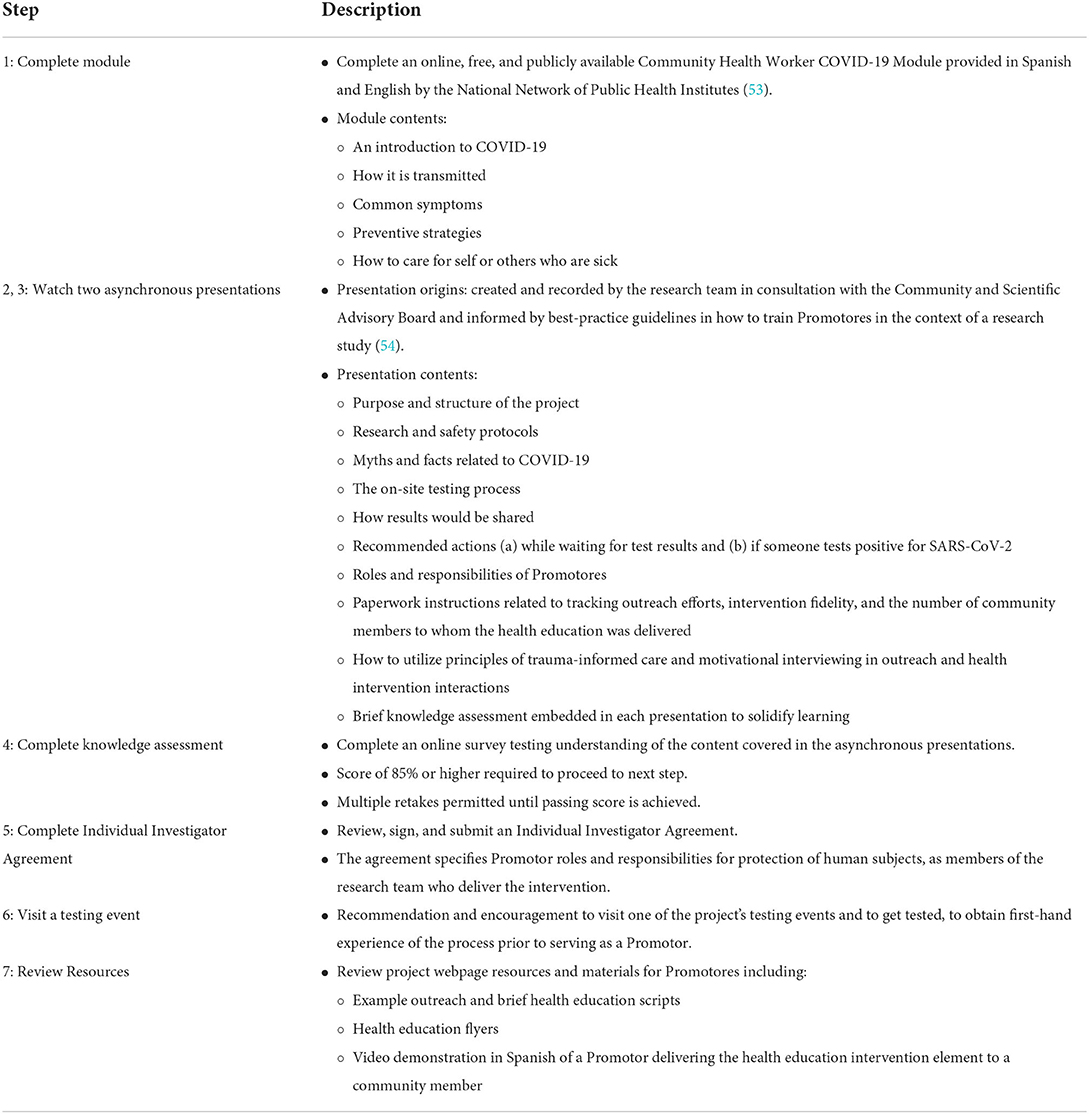
Promotor training
Over the course of the project, partner CBOs hired a total of 21 Promotores who met qualifications such as proficiency in Spanish and English, interpersonal skills, knowledge of cultural norms and community resources, access to internet and email, and computer literacy. Upon being hired, Promotores were directed to the project website for instructions on how to complete their seven-step training (see Table 3), which totaled approximately 6 hours of (paid) time. The Promotor training reviewed effective communication practices consistent with principles of trauma-informed care including safety, trustworthiness, transparency, collaboration, empowerment and intersectionality (3). These principles guided the design of the Promotores de Salud intervention, the processes at the testing events, the research team's ongoing interactions with Promotores, and how Promotores were trained to interact with community members. For example, safety was prioritized, with protocols to keep Promotores and community members safe from COVID-19 as well as from negative community responses to Promotores or the presence of Immigration and Customs Enforcement at a testing event. Trustworthiness and transparency were enhanced by working with community partners embedded in Latinx communities, being explicit in outreach materials that testing events were for all Latinx community members regardless of immigration status, and by excluding any questions about immigration status to minimize risk in a potential breach of confidentiality to testing registration data (55). Potential risks to Promotores (e.g., possible SARS-CoV-2 exposure) and testing participants (e.g., potential risk of breach of confidentiality) were reviewed in advance in the individual's preferred language. To further foster trust and collaboration with partners across sectors, the research team regularly acknowledged the limitations of their resources and knowledge base and expressed appreciation, warmth, and concern for collaborators, many of whom were spread very thin across professional and personal domains as they managed the pandemic. Each Promotor meeting highlighted the hard work, positive attitude, and/or creative problem-solving of Promotores, their CBOs, or the project as a whole.
The principle of collaboration was enacted through regular meetings with the CSAB, public health and community services team, and Promotores, ensuring on-going feedback loops that further refined the intervention. Intervention modifications suggested during these meetings were carefully considered, and a rationale provided for any suggestions not incorporated (e.g., such a change would be contrary to the study design specifications of the grant) or delayed (e.g., required modification to the IRB plan). Empowerment was supported by prioritizing the value of lived experience and community knowledge in the hiring of Promotores, and by trusting Promotores to select the outreach strategies and talking points that they deemed most effective for their communities. Promotores were also trained to honor community members' choices during outreach and brief health education interactions. Lastly, the principle of intersectionality was engaged by consistently acknowledging the structural and systemic constraints affecting Latinx communities and their experience of the pandemic, attending to heterogeneity of Oregon Latinx communities, and by respecting the importance of variation in how the intervention was deployed across communities regarding outreach strategies, community partners, talking points, languages spoken and written materials, and resources shared.
Promotors were trained in how to use motivational interviewing (MI) (56) in the context of their outreach and when delivering the brief health education. MI has demonstrated strong positive effects as a behavior change intervention among Latinx populations and in the context of health promotion interventions (57–59). Training addressed the relational elements, or the “spirit,” of MI as well as how Promotores could apply MI principles and core skills in their role (60). Training in the relational elements of MI emphasized the importance of approaching interactions with a compassionate, non-judgmental, and collaborative stance. For example, in response to ambivalence or resistance to getting tested, Promotores were trained to evoke change by exploring the person's ambivalence to get tested through open-ended follow-up questions, such as eliciting pros and cons of getting tested. Similarly, when delivering health education, Promotores were trained to refrain from pushing back on resistance to mask-wearing, and instead to explore this perspective and ask for permission to share information with the participant about the value of mask-wearing. Promotores engaged in these interactions using core MI skills, such as open-ended questions, affirmations regarding the person's current COVID-19 mitigating behaviors and their self-efficacy for change, reflective listening, and summarizing to convey empathy and compassion. Promotores training highlighted the importance of responding in accord with participants' readiness for testing, mask wearing, and other key COVID-19 preventive behaviors (61).
Discussion
Guided by Duncan et al.'s (27) and Smith, Levkoff and Ory's (28) checklists, this community case study of the Promotores de Salud intervention development and delivery is shared here for the purposes of transparency, replicability, and furthering public health impact by facilitating intervention uptake among Latinx communities. Project strengths, lessons learned for future applications, and additional recommendations are highlighted below.
Strengths
The intervention development process exemplified effective research-community partnerships. Namely, multi-disciplinary researchers, county and state public health practitioners, and leaders from Latinx-serving CBOs pooled their time, resources, connections, and methodological and substantive expertise to accomplish the shared goal of developing a culturally and trauma-informed intervention to promote SARS-CoV-2 testing and preventive behaviors among Oregon's Latinx communities. This project demonstrates how the spirit of CBPR can be infused throughout a public health intervention in spite of the challenges posed by time pressure and constraints of the funding mechanism. The continuous influence of our community social service and public health partners, advisory board, and Promotores greatly enhanced the quality of cultural tailoring, supported learning, and promoted shared ownership of the intervention's success (13).
Another strength was infusing trauma-informed care principles into this project beyond the development of the intervention and training of the Promotores. The pandemic itself was a source of trauma, generating a sense of fear and uncertainty across all communities, causing death and illness, interrupting and constraining daily activities, and restricting access to valuable social supports (62, 63). The strain of these conditions was amplified in Latinx communities but was, nonetheless, palpable across the entire project team. Such a context made it all the more important to curate a team of people who are kind, gracious, and non-defensive. Further, given the long history of research-community partnerships in which value is extracted from the community by researcher-experts, it was paramount that Latinx community members and leaders from Latinx-serving CBOs were upheld as the experts on their communities and their guidance was sought and trusted. Trusting builds trust. The research team acted more as facilitators of the work—synthesizing extant and newly collected data, drafting intervention elements and materials, arranging for on-going solicitation of feedback and direction from these community experts, and incorporating their feedback. Transparency and support for the autonomy of collaborators built safety. Inviting critique and responding with openness and humility increased the likelihood and quality of subsequent feedback. A research team member took diligent notes at all meetings with community partners. These notes, shared after each meeting, documented feedback, recommendations, and adaptations and tracked communication and responsivity over time, which also helped coordinate and communicate these efforts across a large project team. Prior to ending a meeting, a research team member took responsibility for following up on any questions or concerns that could not be addressed during the meeting. The project was a true partnership with a shared sense of urgency and mission.
Responsiveness to Promotores was prioritized, highlighting the critical value of their community knowledge and first-hand experiences delivering the intervention in the community. For example, within and outside of meetings, suggestions and ideas for enhancing outreach and education efforts were responded to promptly and the group was engaged in collaborative problem-solving of the challenges that arose on the ground. A warm relational climate was built in which Promotores and other partners felt comfortable sharing ideas and concerns. Gratitude and respect for their contributions to the project were consistently expressed.
Another strength was the robust representation of Latinx, bicultural, and/or bilingual researchers, professionals, and community members on the research team and CSAB. Leadership with intimate cultural knowledge, relevant lived experience, and Spanish-English language skills was instrumental in fostering trusting partnerships and effectively developing the Promotores de Salud intervention in a relatively short period of time. Meetings with some county CBOs and Promotores were conducted in Spanish, and in response to suggestions from Promotores, meeting minutes were disseminated in both English and Spanish.
Finally, sustainability was an important goal of the project. The partnerships and new lines of communication we established across entities and counties can facilitate greater responsivity to future community health concerns and endeavors in Oregon Latinx communities. The CSAB has expressed enthusiasm for continued service focused on other Latinx health projects. The Promotores de Salud intervention has utility beyond the work of this project. This intervention could accompany testing or vaccination events delivered by public health or other entities. Currently, for example, the intervention is being used at vaccination and testing events hosted by Oregon's Mexican Consulate. The elements of the Promotores de Salud intervention are also well poised for adapting to other community-wide disease prevention and control efforts focused on, for example, influenza or chronic diseases such as heart disease or type 2 diabetes.
Lessons learned for future applications
Although the research-community partnership was a strength, it also presented challenges, often deriving from the rigorous and sometimes lengthy protocols that accompany federally grant-funded and human subjects research. For example, frustration sometimes arose when logical and valuable suggestions from partners could not be incorporated because of grant-related limitations (e.g., funds could not support vaccination efforts), requirements associated with human subjects research (e.g., approval of intervention changes), or research design (e.g., Promotores could not be deployed to all testing sites until completion of the data collection period for evaluating the wait-list control trial). We learned the importance of frequent meetings with CSAB, CBOs, and Promotores that allowed researchers opportunities to respond to frustration and provide the rationale and constraints of the research process. These regular channels of communication supported transparency and helped to increase understanding and patience among the groups.
The fast-paced nature of the project in the context of a pandemic also made it impossible for some of the partner CBOs to take on tasks or processes to the extent initially envisioned, even though financial resources were available. The partner CBOs were actively involved in the delivery of an array of services to their communities (e.g., proving economic resources, health and legal services, childcare, employment support). The increasing demand for these services and staffing shortages as a result of the pandemic stretched the already limited human resources of CBOs. This posed some challenges to supporting the readiness and capacity of CBOs, as well as the Promotores who worked for these CBOs, to deliver the intervention independent of the research team's involvement (13). As such, research team members took on additional, unanticipated aspects of the project in order to continue moving forward. In this context, the intervention development was well suited for a research-community partnership in which the university had substantial human resources to contribute.
We learned to adjust timelines for adaptations to intervention materials and/or Promotores training. Prompted by changing CDC guidelines or state ordinances regarding COVID-19 preventive behaviors, adaptations required drafting, obtaining feedback on, and translating new health education and training content, obtaining IRB approval, and then training CBOs and Promotores on new health education material. Moreover, even after training, Promotores' adoption of new health education content took time and often required review and re-review at the twice-monthly Promotores meetings. Similarly, when vaccines became available and testing rates declined, adaptation of the materials to emphasize the continued importance of SARS-CoV-2 testing took time.
Because of social distancing requirements and the physical dispersion of the project across nine counties, it was necessary to rely almost entirely on technology to communicate with each other and community partners. This was a particular challenge among those Promotores who were less comfortable engaging with the project's website. Ultimately, we found Zoom and email to be the best means of communication and resource sharing. Within the University research team, Zoom and Microsoft Teams were most used. We learned, although remote formats can make forming relationships challenging, it also offered the possibility to meet safely and regularly with people across the state.
Additional recommendations
In order to more fully prioritize the suggestions and timelines of the community partners, we recommend that funding agencies interested in the use of CBPR build in flexibility into study aims to better reflect the priorities of community collaborators, especially in times of public health emergency when community contexts and needs can quickly change. We also recommend that research teams work with their IRB in the grant proposal stage to arrange a fast-track review of any study protocol adjustments for the duration of the study to minimize implementation delays. Despite the accelerated pace of RADx-UP funding timeline (4 months from request for proposals to notification of award), it was about a year between Oregon's shelter-in-place order (March 2020) and the implementation of Promotores de Salud in the community (February 2021). Funding agencies could consider an emergency mechanism for dispersing awards immediately to CBOs that serve vulnerable communities toward hiring additional personnel (even if remote employees) and toward research-community collaborations to facilitate faster acting CBPR-led public health responses.
The heterogeneity of Latinx communities means that local adaptations should be on-going, and we recommend close attention to language and literacy. We recommend not only bicultural and bilingual staff but Spanish native speakers' involvement in the creation and/or review of materials to produce accurately written messages that are culturally and linguistically responsive. We were unable to recruit a Mam-speaking Promotor and arranged for translators at testing sites where Mam-speaking community members were expected. Our written materials were not translated into Mam due to low Mam literacy rates in the community. Further, our materials adhered to a 6th-grade reading level for English and Spanish and incorporated visual cues, but still relied on textual information for certain aspects of outreach, health education, and resource navigation support. An agency specializing in multi-language audio and visual outreach services was contracted to create videos in Spanish and Mam. However, these products did not come to fruition due to agency staffing limitations. These conditions made our verbal outreach efforts (radio announcements and in-person presence at community locations) critical.
The Promotores de Salud intervention will also need ongoing adaptation as SARS-CoV-2 and its variants continue to change and scientific understanding of COVID-19 prevention and control evolves. We recommend generating the critical feedback for necessary adaptations via partnerships with public health practitioners, Latinx-serving CBOs, and Promotores in the communities where the intervention will be implemented. Evidence that this intervention resulted in significantly higher participation of Latinx community members in testing events (43) is very promising, warranting replication and continued evaluation.
Conclusion
In response to disproportionate COVID-19 burden experienced among Latinx communities in Oregon, we collaboratively developed a trauma-informed and culturally tailored Promotores de Salud intervention to increase SARS-CoV-2 testing and preventive behaviors among Oregon's Latinx communities. This case study presents details of the development and refinement processes, the intervention itself, and the strengths and lessons learned of such public health field work to benefit future research-community partnerships and to facilitate replication of the Promotores de Salud intervention toward eliminating COVID-19 disparities among Latinx communities nationwide.
Data availability statement
The de-identified data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by University of Oregon Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
All authors made substantial contributions to the conception or design of the work. EB, CC, KY, AJ, and HT contributed substantially to the data acquisition, analysis, and interpretation. EM, SD, AM, MM, AN, KV, JG, OSJP CSAB, WC, DD, and LL contributed substantially to the data interpretation. EB, EM, SD, AM, KY, AJ, and HT drafted the work and CC, OSJP CSAB, and LL substantively revised it. All authors read and approved the final manuscript and agree to be accountable for the content of the work.
Funding
Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number P50 DA048756-02S2 (MPIs: LL, WC, and DD). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funding body had no role in the design of the study and collection, analysis, and interpretation of data or in writing the manuscript.
Acknowledgments
We are grateful for the tremendous contributions and collaborative spirits of our partner CBOs, Promotores, and local and state health departments throughout this project. CSAB members include JG (Chair), Lisandra Guzman, Juan Diego Ramos, Kristin Yarris, Maria Castro, Jacqueline McCall, Abe Vega, and Oscar Becerra. Thank you also to Jen Volpi for her assistance with formatting and Christabelle Dragoo, Ashley Easter, and Akhila Nekkanti for their contributions to the literature review and stakeholder interviews.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.962862/full#supplementary-material
Data Sheet 1. Example outreach card.
Data Sheet 2. Health education flier in Spanish.
Data Sheet 3. Health education flier in English.
References
1. del Río-González AM. To Latinx or not to Latinx: a question of gender inclusivity vs. gender neutrality. Am J Public Health. (2021) 111:1018–21. doi: 10.2105/AJPH.2021.306238
2. Fortuna LR, Tolou-Shams M, Robles-Ramamurthy B, Porche MV. Inequity and the disproportionate impact of COVID-19 on communities of color in the United States: the need for a trauma-informed social justice response. Psychol Trauma. (2020) 12:443–5. doi: 10.1037/tra0000889
3. Rodriguez-Diaz CE, Guilamo-Ramos V, Mena L, Hall E, Honermann B, Crowley JS, et al. Risk for COVID-19 infection and death among Latinos in the United States: examining heterogeneity in transmission dynamics. Ann Epidemiol. (2020) 52:46–53 e2. doi: 10.1016/j.annepidem.2020.07.007
4. Ahmed F, Ahmed Ne, Pissarides C, Stiglitz J. Why inequality could spread COVID-19. Lancet Public Health. (2020) 5:e240. doi: 10.1016/S2468-2667(20)30085-2
5. Kim HN, Lan KF, Nkyekyer E, Neme S, Pierre-Louis M, Chew L, et al. Assessment of disparities in COVID-19 testing and infection across language groups in Seattle, Washington. JAMA Netw Open. (2020) 3:e2021213. doi: 10.1001/jamanetworkopen.2020.21213
6. U.S. Census Bureau. Racial and Ethnic Diversity in the United States 2010 and 2020. (2021). Available online at: https://www.census.gov/library/visualizations/interactive/racial-and-ethnic-diversity-in-the-united-states-2010-and-2020-census.html (accesed April 1, 2022).
7. Oregon Health Authority. COVID-19 Weekly Report: Oregon's Weekly Surveillance Summary- May 19, 2020. (2020). Available online at: https://www.oregon.gov/oha/PH/DISEASESCONDITIONS/DISEASESAZ/Emerging%20Respitory%20Infections/COVID-19-Weekly-Report-2020-05-19-FINAL.pdf (accesed September 10, 2021).
8. Oregon Health Authority. COVID-19 Weekly Report: Oregon's Weekly Urveillance Summary- July 15, 2020. (2020). Available online at: https://www.oregon.gov/oha/PH/DISEASESCONDITIONS/DISEASESAZ/Emerging%20Respitory%20Infections/COVID-19-Weekly-Report-2020-07-22-FINAL.pdf (accesed September 10, 2021).
9. Centers for Disease Control Prevention. COVID Data Tracker: Trends in Cases and Deaths By Race/Ethnicity, Age, and Sex. (2020). Available online at: https://covid.cdc.gov/covid-data-tracker/#demographicsovertime (accesed September 12, 2021).
10. Oregon Community Foundation. Latinos in Oregon Report. (2016). Available online at: https://oregoncf.org/community-impact/research/latinos-in-oregon-report/ (accesed September 14, 2021).
11. Centers for Disease Control Prevention. COVID-19 Testing: What You Need To Know. (2022). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/testing.html (accesed April 25, 2022).
12. U.S. Census Bureau. American Community Survey 5-Year Estimates Subject Tables: Languages Spoken at Home: S1601. (2019). Available online at: https://data.census.gov/cedsci/table?tid=ACSST5Y2019.S1601&g=0400000US41 (accesed December 10, 2021).
13. Edwards RW, Jumper-Thurman P, Plested BA, Oetting ER, Swanson L. Community readiness: research to practice. J Community Psychol. (2000) 28:291–307. doi: 10.1002/(SICI)1520-6629(200005)28:3<291::AID-JCOP5>3.0.CO;2-9
14. Migration Policy Institute. Profile of the Unauthorized Population: Oregon. (2019). Available online at: https://www.migrationpolicy.org/data/unauthorized-immigrant-population/state/OR (accesed July 08, 2022).
15. Bauer J. Oregon's Undocumented Workers Endure Pandemic Without Economic Aid Offered to Others Oregon Center for Public Policy. (2021). Available online at: https://www.ocpp.org/2021/06/15/oregon-undocumented-workers-pandemic/ (accesed April 14, 2022).
16. Guest G, Namey E, Chen M. A simple method to assess and report thematic saturation in qualitative research. PLoS ONE. (2020) 15:e0232076. doi: 10.1371/journal.pone.0232076
17. Liu SR, Modir S. The outbreak that was always here: racial trauma in the context of COVID-19 and implications for mental health providers. Psychol Trauma. (2020) 12:439–42. doi: 10.1037/tra0000784
18. Thakur N, Lovinsky-Desir S, Bime C, Wisnivesky JP, Celedon JC. The structural and social determinants of the racial/ethnic disparities in the US COVID-19 pandemic What's our role? Am J Respir Crit Care Med. (2020) 202:943–9. doi: 10.1164/rccm.202005-1523PP
19. Capps R, Gelatt J. Barriers to COVID-19 Testing Treatment: Immigrants Without Health Insurance Coverage in the U.S.: Migration Policy Institute. (2020). Available online at: https://www.migrationpolicy.org/research/covid-19-testing-treatment-immigrants-health-insurance (accesed November 13, 2021).
20. Kerr JR, Schneider CR, Recchia G, Dryhurst S, Sahlin U, Dufouil C, et al. Correlates of intended COVID-19 vaccine acceptance across time and countries: results from a series of cross-sectional surveys. BMJ Open. (2021) 11:e048025. doi: 10.1136/bmjopen-2020-048025
21. Garcini LM, Domenech Rodíguez MM, Mercado A, Paris M. A tale of two crises: the compounded effect of COVID-19 and anti-immigration policy in the United States. Psychol Trauma. (2020) 12:S230–2. doi: 10.1037/tra0000775
22. Substance Abuse and Mental Health Services Administration. Trauma-Informed Care in Behavioral Health Services. Rockville, MD: SMA (2014). p. 13–4801. Contract No.: HHS.
23. Meléndez Guevara AM, Lindstrom Johnson S, Elam K, Hilley C, McIntire C, Morris K. Culturally responsive trauma-informed services: a multilevel perspective from practitioners serving Latinx children and families. Community Ment Health J. (2021) 57:325–39. doi: 10.1007/s10597-020-00651-2
24. Collins SE, Clifasefi SL, Stanton J, The The Leap Advisory B, Straits KJE, Gil-Kashiwabara E. Community-based participatory research (CBPR): towards equitable involvement of community in psychology research. Am Psychol. (2018) 73:884–98. doi: 10.1037/amp0000167
25. Trickett EJ. Community-based participatory research as worldview or instrumental strategy: is it lost in translation(al) research? Am J Public Health. (2011) 101:1353–5. doi: 10.2105/AJPH.2011.300124
26. Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. (2010) 100:S40–6. doi: 10.2105/AJPH.2009.184036
27. Duncan E, O'Cathain A, Rousseau N, Croot L, Sworn K, Turner KM, et al. Guidance for reporting intervention development studies in health research (GUIDED): an evidence-based consensus study. BMJ Open. (2020) 10:e033516. doi: 10.1136/bmjopen-2019-033516
28. Smith ML, Levkoff SE, Ory MG. Community case study article type: criteria for submission and peer review. Front Public Health. (2016) 4:56. doi: 10.3389/fpubh.2016.00056
29. Brennan Ramirez LK, Baker EA, Metzler M. Promoting Health Equity: A Resource to Help Communities Address Social Determinants of Health. National Center for Chronic Disease Prevention and Health Promotion (US) (2008).
30. Petty RE, Cacioppo JT. The elaboration likelihood model of persuasion. In: Berkowitz L, editor. Advances in Experimental Social Psychology. Orlando, FL: Academic Press (1986). p. 123–205.
31. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. (2005) 15:1277–88. doi: 10.1177/1049732305276687
32. Calzada E, Suarez-Balcazar Y. Enhancing cultural competence in social service agencies: a promising approach to serving diverse children and families. OPRE Report. (2014) 31:1–8.
33. Logan RI, Castaneda H. Addressing health disparities in the rural United States: advocacy as caregiving among community health workers and promotores de salud. Int J Environ Res Public Health. (2020) 17:9223. doi: 10.3390/ijerph17249223
34. Oakley LP, Harvey SM, Lopez-Cevallos DF. Racial and ethnic discrimination, medical mistrust, and satisfaction with birth control services among young adult Latinas. Womens Health Issues. (2018) 28:313–20. doi: 10.1016/j.whi.2018.03.007
35. Bowen EA, Murshid NS. Trauma-informed social policy: a conceptual framework for policy analysis and advocacy. Am J Public Health. (2016) 106:223–9. doi: 10.2105/AJPH.2015.302970
36. Centers for Disease Control Prevention. Community Health Worker (CHW) Toolkit. (2019). Available online at: https://www.cdc.gov/dhdsp/pubs/toolkits/chw-toolkit.htm (accesed October 12, 2021).
37. Centers for Disease Control Prevention Office of the Associate Director for Communication. Cultural Insights; Communication With Hispanics/Latinos. (2012). Available online at: https://stacks.cdc.gov/view/cdc/13183
38. APA Presidential Task Force on Immigration. Crossroads: the psychology of immigration in the new century. J Lat Psychol. (2013) 1:133–48. doi: 10.1037/lat0000001
39. López-Cevallos DF, Harvey SM, Warren JT. Medical mistrust, perceived discrimination, and satisfaction with health care among young-adult rural Latinos. J Rural Health. (2014) 30:344–51. doi: 10.1111/jrh.12063
40. Janz NK, Champion VL, Strecher VJ. The health belief model. In: Glanz K, Rimer BK, Lewis FM, editors. Health Behavior and Health Education. San Francisco: Jossey-Bass (2002). p. 45–66.
41. Strecher VJ, Champion VL, Rosenstock IM. The health belief model and health behavior. In: Gochman DS, editor. Handbook of Health Behavior Research: Personal and Social Determinants. New York, NY: Plenum Press (1997). p. 71–91.
42. Añez LM, Silva MA, Paris M, Bedregal LE. Engaging Latinos through the integration of cultural values and motivational interviewing principles. Prof Psychol Res Pr. (2008) 39:153–9. doi: 10.1037/0735-7028.39.2.153
43. DeGarmo DS, De Anda S, Cioffi CC, Tavalire HF, Searcy JA, Budd EL, et al. Effectiveness of a COVID-19 testing outreach intervention for Latinx communities: a clustered randomized clinical trial. JAMA Netw Open. (2022) 5:e2216796. doi: 10.1001/jamanetworkopen.2022.16796
44. Searcy J, Cioffi CC, Tavalire HF, Budd EL, Cresko WA, DeGarmo DS, et al. Reaching Latinx Communities With Algorithmic Optimization for SARS-CoV-2 Testing Locations. In press.
45. Olaniran A, Smith H, Unkels R, Bar-Zeev S, van den Broek N. Who is a community health worker? - a systematic review of definitions. Glob Health Action. (2017) 10:1272223. doi: 10.1080/16549716.2017.1272223
46. Brown LD, Vasquez D, Salinas JJ, Tang X, Balcazar H. Evaluation of Healthy Fit: A community health worker model to address Hispanic health disparities. Prev Chronic Dis. (2018) 15:E49. doi: 10.5888/pcd15.170347
47. Centers for Disease Control Prevention. Promotores de Salud/Community health workers: Office of Minority Health & Health Equity. (2019). Available online at: https://www.cdc.gov/minorityhealth/promotores/index.html
48. García AA, Zuniga JA, Lagon C. A personal touch: the most important strategy for recruiting Latino research participants. J Transcult Nurs. (2017) 28:342–7. doi: 10.1177/1043659616644958
49. Vincent D, McEwen MM, Hepworth JT, Stump CS. Challenges and success of recruiting and retention for a culturally tailored diabetes prevention program for adults of Mexican descent. Diabetes Educ. (2013) 39:222–30. doi: 10.1177/0145721713475842
50. Zuñiga JA, Munoz S, Johnson MZ, Garcia AA. Mexican American men's experience of living with tuberculosis on the US-Mexico border Am J Mens Health. (2016) 10:32–8. doi: 10.1177/1557988314555359
51. Barnett ML, Gonzalez A, Miranda J, Chavira DA, Lau AS. Mobilizing community health workers to address mental health disparities for underserved populations: a systematic review. Adm Policy Ment Health. (2018) 45:195–211. doi: 10.1007/s10488-017-0815-0
52. Oregon Department of Human Services. Community Health Worker Certification. Available online at: https://www.oregon.gov/dhs/SENIORS-DISABILITIES/HCC/PSW-HCW/Pages/Community-Health-Worker.aspx (accesed July 28, 2020).
53. National Network of Public Health Institutes. Community Health Worker COVID-19 Training Module. (2020). Available online at: https://www.phlearningnavigator.org/training/community-health-worker-training-covid-19-module (accesed July 29, 2020).
54. Gutierrez Kapheim M, Campbell J. Best Practice Guidelines for Implementing and Evaluating Community Health Worker Programs in Health Care Settings. Sinai Urban Health Institute (2014).
55. Doran KM, Castelblanco DG, Mijanovich T. Undocumented Latino immigrants and research: new challenges in changing times. J Health Care Poor Underserved. (2018) 29:645–50. doi: 10.1353/hpu.2018.0048
56. Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. 3rd Ed. New York, NY: The Guilford Press (2012).
57. Brandford A, Adegboyega A, Combs B, Hatcher J. Training community health workers in motivational interviewing to promote cancer screening. Health Promot Pract. (2019) 20:239–50. doi: 10.1177/1524839918761384
58. Elder JP, Haughton J, Perez LG, Martinez ME. De la Torre CL, Slymen DJ, et al. Promoting cancer screening among churchgoing Latinas: fe en Accion/faith in action. Health Educ Res. (2017) 32:163–73. doi: 10.1093/her/cyx033
59. Portillo EM, Vasquez D, Brown LD. Promoting Hispanic immigrant health via community health workers and motivational interviewing. Int Q Community Health Educ. (2020) 41:3–6. doi: 10.1177/0272684X19896731
60. Miller WR, Moyers TB. Eight stages in learning motivational interviewing. J Teach Addict. (2006) 5:3–17. doi: 10.1300/J188v05n01_02
61. Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol. (2005) 1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833
62. Park AL, Velez CV, Kannan K, Chorpita BF. Stress, functioning, and coping during the COVID-19 pandemic: Results from an online convenience sample. Behav Ther. (2020) 42:210–6. doi: 10.31234/osf.io/jmctv
Keywords: COVID-19 testing, Hispanic Americans, health promotion, minority health, health status disparities, Latinx
Citation: Budd EL, McWhirter EH, De Anda S, Mauricio AM, Mueller MV, Cioffi CC, Nash A, Van Brocklin K, Yarris K, Jackson A, Terral H, García JIR, Juntos Podemos Community and Scientific Advisory Board, Cresko WA, DeGarmo DS and Leve LD (2022) Development and design of a culturally tailored intervention to address COVID-19 disparities among Oregon's Latinx communities: A community case study. Front. Public Health 10:962862. doi: 10.3389/fpubh.2022.962862
Received: 06 June 2022; Accepted: 05 September 2022;
Published: 23 September 2022.
Edited by:
Kevin Dadaczynski, Fulda University of Applied Sciences, GermanyReviewed by:
Mario Cruz-Gonzalez, Harvard Medical School, United StatesMariano Kanamori, University of Miami, United States
Copyright © 2022 Budd, McWhirter, De Anda, Mauricio, Mueller, Cioffi, Nash, Van Brocklin, Yarris, Jackson, Terral, García, Juntos Podemos Community and Scientific Advisory Board, Cresko, DeGarmo and Leve. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elizabeth L. Budd, ebudd@uoregon.edu
 Elizabeth L. Budd
Elizabeth L. Budd Ellen Hawley McWhirter
Ellen Hawley McWhirter Stephanie De Anda
Stephanie De Anda Anne Marie Mauricio
Anne Marie Mauricio Maryanne V. Mueller1,2
Maryanne V. Mueller1,2 Camille C. Cioffi
Camille C. Cioffi Heather Terral
Heather Terral David S. DeGarmo
David S. DeGarmo Leslie D. Leve
Leslie D. Leve