- School of Social Development and Public Policy, Beijing Normal University, Beijing, China
Objective: The purpose of this study was to investigate the association between smoking and health-related quality of life among Chinese individuals aged 40 years and older.
Method: Using a stratified multistage sampling method, data from 1,543 adults aged 40 years and older were obtained from a household survey conducted in eight provinces in China. The health-related quality of life was quantified based on the utility index obtained using a standardized instrument entitled “The European Five-Dimensional Health Scale (EQ-5D-5L).” Descriptive statistics were used to summarize the demographic characteristics and social factors of the sample according to smoking status. An instrumental variable (IV) probit model was used to estimate the association between smoking status and health-related quality of life.
Results: Of the 1,543 participants, 485 (31.43%) were smokers and 1,058 (68.57%) were non-smokers. Smoking was negatively associated with the probability of having a higher quality of life (p < 0.01). For smokers, the average probability of having a higher quality of life was 11.65% lower than when they did not smoke.
Conclusions: These findings suggest that smoking reduces health-related quality of life among Chinese individuals aged 40 years and older. Anti-smoking programs should consider this factor.
Introduction
The tobacco epidemic is the greatest but preventable risk factor for human health. Approximately 8 million people worldwide die from smoking each year, and more than 80% of the 1.3 billion tobacco users worldwide live in low- and middle-income countries (1). According to the 2018 Global Adult Tobacco Survey (GATS), there are more than 300 million smokers in China, with 52.9% of Chinese male adults smoking (2). China's health, society, and economy are suffering due to tobacco consumption. More than 1 million people die from tobacco-related deaths in China each year. This number will continue to grow—to ~3 million by 2,050 if China does not act effectively to control its smoking epidemic (3).
In addition to health threats, smoking can also directly affect health-related quality of life (HRQoL) (4–7). As a comprehensive health evaluation index, quality of life is a self-assessment, that measures people's self-report of their physical state, mental function, social ability, and personal overall condition based on certain socioeconomic and cultural backgrounds and values.
It seems to be a common belief that smoking can help relieve stress and promote relaxation, thus creating the illusion that smokers have a much higher quality of life than non-smokers. However, accumulating evidence suggests that HRQoL is better among non-smokers and former smokers than among current smokers (8–10). The negative association between smoking and HRQoL has been demonstrated in several cross-sectional studies (11–13). Their results were further confirmed by longitudinal studies focusing on the association between smoking status and changes in HRQoL (14–17).
The association between smoking and HRQoL may have different manifestations in different countries, where the cultural context may be at play. Most related studies have been conducted in western countries, including European countries (18–21), the United States (22), and a few other countries (23–26). Although China is the largest tobacco producer and consumer in the world, few studies have systematically examined the association between smoking and HRQoL among Chinese individuals. Besides, smoking is a continuous behavior, and its process of causing harm to human health is long-term and chronic (27). As a result, smoking-related side effects may be more easily perceived in middle-aged and older adults than in younger adults. Therefore, while the current mainstream literature shows that smoking is negatively related to quality of life, it is still necessary to evaluate the impact of smoking on the quality of life of the Chinese population aged 40 years and above.
The challenges in studying the association between smoking status and HRQoL are sample self-selection and sampling bias. However, the possible endogeneity of the relationship between smoking status and quality of life has rarely been considered. Whether to smoke is a self-selective behavior that can be influenced by many factors. The omitted variables that may affect both smoking and HRQoL will make the results less credible.
Therefore, the objective of this study was to explore the association between smoking and HRQoL among Chinese individuals aged 40 years and older using an instrumental variable (IV) probit model.
Materials and Methods
Participants
Participants (N = 1,543) were Chinese individuals aged 40 years and older recruited in a household survey conducted in China between November 1, 2019, and October 30, 2020. A stratified multistage sampling method was used to select participants from 24 primary health care facilities. These 24 primary health care facilities were selected as follows: firstly, 8 provinces were selected in the east, middle, and west of China: Hebei, Heilongjiang, Shandong, Henan, Hubei, Sichuan, Guizhou, and Shaanxi. Then 2–4 primary health care institutions, including township health centers and community health service centers, were randomly selected in each province. From the areas of 24 primary health care facilities, ~100 households were randomly selected. To be eligible, participants from the 100 households had to live in local communities for at least 6 months, have a minimum age of 40 years, and be willing to participate in this study.
Data Collection
Based on informed consent, the data were collected using anonymous paper and pencil tests. Participants completed questionnaires entitled “Questionnaire on the health of people over 40 years old and its influencing factors.” The validated interviewer-administered questionnaire mainly included (1) general household information, including household type, total household income, and expenditure; (2) basic personal information of household members, including gender, age, and education level; (3) smoking, smoking-related knowledge and chronic diseases of household members; and (4) self-care ability and quality of life of household members.
In this study, the investigators were designated by each investigation unit, and then the investigators were uniformly trained by the research team. The means of household inquiries were adopted by the investigators. Besides, each survey unit identified a contact person who was responsible for survey organization, implementation, quality control, and unified reporting to the subject group. Finally, the research team organized and coded the questionnaires in a unified manner. This study was approved by the ethics committee of the Capital Institute of Pediatrics, Beijing (ID: SHERLL2020017). And the study was conducted following the ethical principles of the Declaration of Helsinki.
Measures
Dependent Variables
The dependent variable was “quality of life utility index.” The HRQoL was quantified based on the utility index obtained using a standardized instrument entitled “The European Five-Dimensional Health Scale (EQ-5D-5L).” The EQ-5D is easy to operate and easy to understand by the survey subject and has good reliability and validity. Therefore, it has been widely used in various research fields in many countries (28) and has become one of the widely used tools for measuring HRQoL. The EQ-5D survey includes five dimensions: mobility, self-care, usual activities, pain or discomfort, and anxiety or depression. An approved Chinese version of the EQ-5D-5L was used, and each level contained five possible responses indicating “no problems,” “slight problems,” “moderate problems,” “severe problems” and “unable to/extreme problems.” If “no problems” were reported for a given level, it was marked as level 1, whereas “unable to/extreme problems” was marked as level 5. The eq5d command in STATA (StataCorp, College Station, Texas, USA) computes an index value from individual responses to the EQ-5D-5L quality-of-life instrument. The EQ-5D index has an upper bound equal to 1 that indicates full health (as evidenced by “no problem” in all domains), whereas 0 represents death (29). To facilitate analysis, we dichotomized the EQ-5D index according to its mean value.
Independent Variable
The measure of smoking status came from responses to the following question: “Do you smoke now?” In the current study, the concept of smoking was defined as “having smoked at least 1 day in the past 30 days.” Response options were (1) No, (2) Yes, and (3) Have quit smoking. To facilitate statistical analysis, smoking status was dummy coded: (1) smoking: participants who smoke now; (2) non-smoking: participants who had never smoked or had quit smoking.
Covariates
Based on prior knowledge (30), covariates included age, gender, educational level, marital status, logarithm of household income, occupation, family size, health status, and province.
Instrumental Variable
Whether the increase in cigarette prices reduced the number of cigarettes smoked (PRS) was used as an instrumental variable.
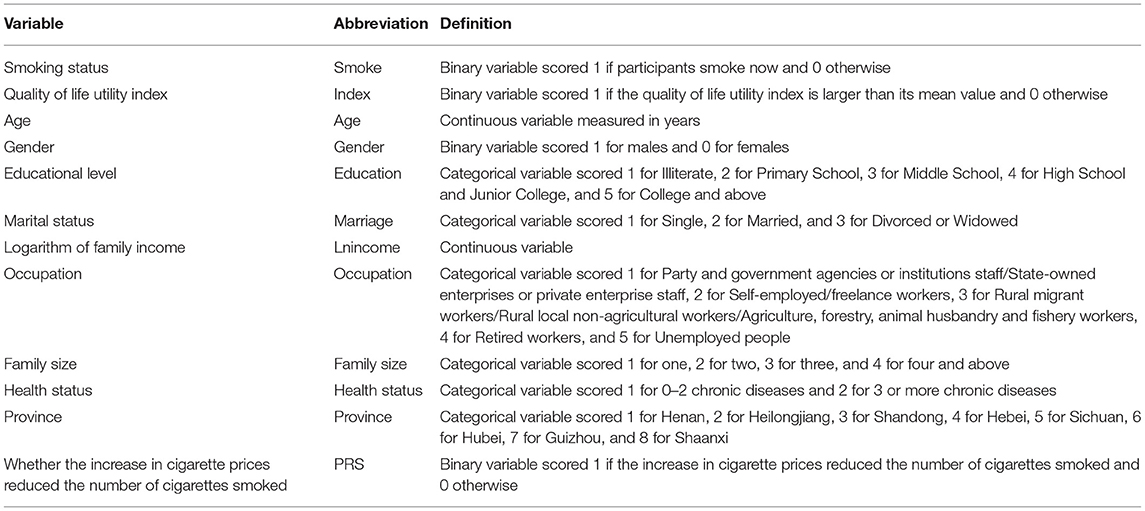
The variables used in the regression analysis are listed and defined in Table 1.
Data Analysis
Descriptive Analysis
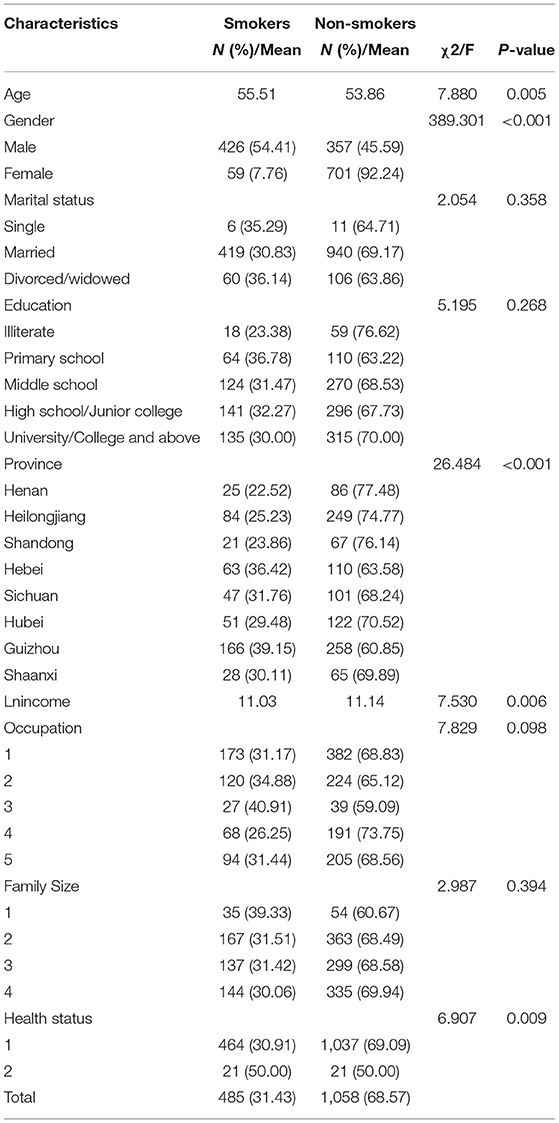
Descriptive statistics were used to summarize the demographic characteristics and social factors of the sample by smoking status. Characteristics of smokers were compared with those of non-smokers using chi-square tests for categorical variables and Kruskal–Wallis one-way ANOVA tests for continuous variables. Descriptive data are presented as the mean for continuous variables and as percentages for categorical variables.
Effect Estimation
To investigate the association between smoking status and HRQoL, an instrumental variable (IV) probit model was used to control for potential endogeneity problems. Whether the increase in cigarette prices had an effect on the number of cigarettes smoked (PRS) was used as an instrumental variable. It was chosen because it is expected to be correlated with smoking behavior but not directly affect quality of life, thus satisfying the instrumental variable exogeneity requirement. Covariates included age, gender, educational level, marital status, logarithm of annual household income, occupation, family size, health status, and province. The province variable was entered into the model as a dummy variable to give the province a specific intercept to capture sample clustering.
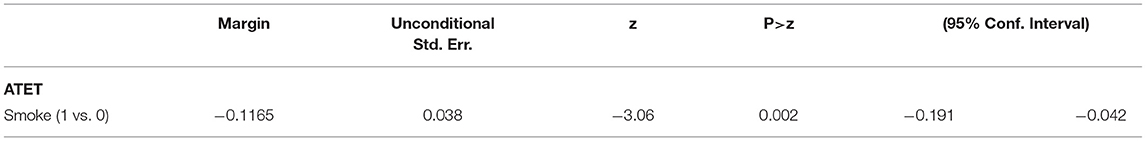
The parameter estimates from the IV probit were further used by marginal analysis to estimate the average treatment effect on the treated (ATET) of smoking on HRQoL. ATET is the estimated average difference of the treatment and control potential outcomes in the treated population. ATET is useful when there is interest in the quantification of the treatment effect in observational studies in which no definite parameter can be used. Therefore, ATET was calculated to obtain more intuitive and practical results.
The instrumental variable (IV) probit model is constructed below as:
Here, Indexi refers to the quality of life utility index of the respondents and represents the latent variable of the quality of life utility index in Equation (1). Smokei, the independent variable of interest, is binary. β1 is the coefficient of interest, which provides the estimated effect of smoking on HRQoL. Z is a vector of demographic and socioeconomic variables. I represents the instrumental variable. γ, π1 and π2 are the vectors of parameters for the control variables that need to be estimated. μi and αi are normally distributed error terms in the equation and i denotes an individual respondent.
All statistical analyses were performed using Stata (version 16.0; StataCorp, College Station, Texas, USA). Values of p < 0.05 were considered statistically significant.
Results
Sample Characteristics
The characteristics of subjects are summarized in Table 2. Of the 1,543 participants, 485 (31.43%) were smokers, and 1,058 (68.57%) were non-smokers. The average age of smokers was 55.51, whereas that of non-smokers was 53.86 (p = 0.005). The proportion of smokers among males was 54.41%, whereas the proportion among females was 7.76% (p < 0.001). The mean value of the logarithm of family income for smokers was 11.03 compared to 11.14 for non-smokers (p = 0.006). There was no significant difference concerning educational status (p = 0.268), marital status (p = 0.358), occupations (p = 0.098), and family size (p = 0.394) between smokers and non-smokers, whereas there were significant differences in the distribution of provinces (p < 0.001). Among the participants with two or fewer chronic diseases, 30.91% were smokers and 69.09% were non-smokers (p = 0.009).
The Association Between Smoking and HRQoL
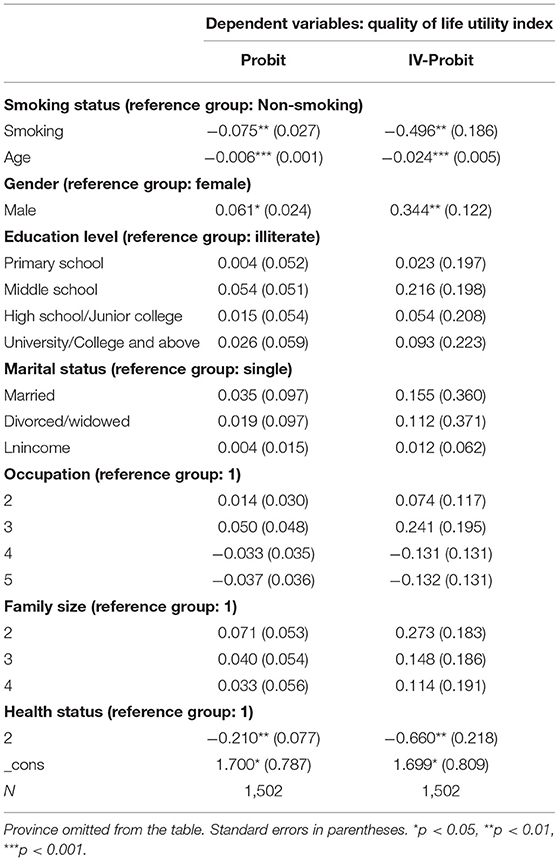
The middle column in Table 3 shows the average marginal effects of the probit regression model. The sign of the smoke variable was negative and statistically significant. Smoking decreases the probability of having a higher quality of life by 7.50 percent.
The right column in Table 3 presents the estimated results of the IV probit regression model. As expected, the results show that smoking was negatively correlated with the probability of having a higher quality of life (p < 0.01). As shown in Table 4, the estimated ATET of −0.1165 implies that for those who smoked, the average probability of having a higher quality of life would be 11.65 percent lower than it would be if they had not smoked. This result is higher than the 7.50 percent obtained by the probit regression model.
In Table 3, from the estimated results of the explanatory variables in the IV probit model, the effects of age and gender on HRQoL were significant at the 0.1 and 1% levels, respectively. The coefficient for age indicates that increases in age lower the probability of having a higher quality of life. If the subject was male, the probability of his having a higher quality of life was greater. Among the province variables, the effects of Shandong, Hebei, and Shaanxi on HRQoL were significant at the 1, 5, and 5% levels, respectively.
Discussion
Our study indicated that smoking led to a lower probability of having a higher quality of life. For smokers, the average probability of having a higher quality of life was 11.65 percent lower than when they did not smoke.
These compelling findings confirm previous findings reported from other countries such as the UK (31, 32), USA (22), Spain (19, 33), Canada (4) and Turkey (8). The consistent findings when using different tools to measure HRQoL reinforces the conclusion that smoking is negatively associated with HRQoL (11, 34, 35). According to Toghianifar et al. (36), smokers scored lower than non-smokers in terms of general health, social functioning, role-emotional and mental health, whereas recent quitters had significantly improved role-emotional and mental health than those who had continued smoking or those who became smokers.
The reasons for the observed negative association between smoking and HRQoL can be attributed to the following aspects. First, smoking increases the risk of non-communicable diseases, including cancers and cardiovascular and respiratory diseases (37). Adults with more health diseases have worse quality of life (26). Second, smoking was found to be associated with increased odds of depression (38) and more clinically significant fatigue (39). Third, the substances inhaled in cigarettes are related to muscle weakness and decreased vitality (40). Forth, the EQ-5D used in the present study is a comprehensive measurement of HRQoL in terms of mobility, self-care, usual activities, pain or discomfort, and anxiety or depression. In the long term, smoking would affect the five dimensions of the EQ-5D, thereby reducing HRQoL (14).
Besides smoking status that was previously discussed, age and gender were found to be independent variables of a lower HRQoL. This finding suggests that smoking intervention programs might be targeted for specific populations, such as men in particular age groups who are current smokers, in order to better improve HRQoL.
Popular belief has it that quitting will decrease HRQoL—because individuals believe it interferes with relationships or produces a loss of smoking related pleasure (such as reducing stress or promoting relaxation). However, the current study indicated that smoking did not improve HRQoL as one would expect. This result contributes to the knowledge of the association between smoking and HRQoL. Knowledge of this association is useful for two reasons: (1) to assist the economic evaluation of cessation programs by providing a more direct measure of health outcomes than the cessation itself; (2) to provide a good reason for individuals to quit smoking.
The strengths of this study are as follows. First, it was based on a large and nationally representative sample of middle-aged and older Chinese individuals. We were able to examine the association between smoking and HRQoL and control many potential confounding factors. The large sample size enabled sufficient power for statistical inference. Second, we used the IV probit regression model to address selection bias. The estimated results of the IV probit regression model were higher than the estimated results of the probit regression model, indicating that the probit model might underestimate the effect of smoking on HRQoL because of selection bias.
There are several limitations to the present study. First, we relied on self-report measures, which may be subject to recall bias and social desirability effects. Second, the study was cross-sectional in design, thus making it hard to obtain any conclusions regarding exact cause-and-effect relationships. Longitudinal data may be needed to further explore the causal relationship between smoking and HRQoL. Third, the generalizability of our results to other populations is limited because we focused on China, and other countries may be different due to ethnic differences.
Conclusion
Findings from the current study suggest that for smokers, the average probability of having a higher quality of life was 11.65% lower than when they did not smoke. Emphasizing that smoking will lead to a lower quality of life may help guide smokers to consciously quit smoking. Therefore, it is necessary for anti-smoking campaigns to clearly point out the negative effect of tobacco use on HRQoL.
Data Availability Statement
The datasets presented in this article are not readily available because data involves personal privacy issues. Requests to access the datasets should be directed to Xi Cheng, 15107100093@163.com.
Author Contributions
XC: conceptualization, data curation, writing - original draft, and writing - review & editing. CJ: conceptualization, funding acquisition, investigation, supervision, and writing - review & editing. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. WHO. Tobacco (2020). Available online at: https://www.who.int/en/news-room/fact-sheets/detail/tobacco (accessed May 6, 2021).
2. WHO. Global Adult Tobacco Survey 2018 (2020). Available online at: https://extranet.who.int/ncdsmicrodata/index.php/catalog/803/related-materials (accessed January 11, 2022).
3. WHO. Smoke-Free Policies in China: Evidence of Effectiveness and Implications for Action (2015). Available online at: http://www.wpro.who.int/china/tobacco_report_20151019_en.pdf (accessed December 9, 2021).
4. Cui Y, Forget EL, Torabi M, Oguzoglu U, Ohinmaa A, Zhu Y. Health-related quality of life and economic burden to smoking behaviour among Canadians. Can J Public Health Rev Canad De Sante Publique. (2019) 110:533–41. doi: 10.17269/s41997-019-00244-x
5. Heikkinen H, Jallinoja P, Saarni SI, Patja K. The impact of smoking on health-related and overall quality of life: a general population survey in Finland. Nicot Tobacco Res. (2008) 10:1199–207. doi: 10.1080/14622200802163142
6. Tillmann M, Silcock J. A comparison of smokers' and ex-smokers' health-related quality of life. J Public Health Med. (1997) 19:268–73. doi: 10.1093/oxfordjournals.pubmed.a024629
7. Unsal A, Ayranci U, Tozun M. Frequency of smoking among males and its impact on the quality of life. Pakistan J Med Sci. (2010) 26:163–7.
8. Cakmakci Karadogan D, Onal O, Say Sahin D, Yazici S, Kanbay Y. Evaluation of school teachers' sociodemographic characteristics and quality of life according to their cigarette smoking status: a cross-sectional study from the eastern Black Sea region of Turkey. Tuberkuloz Ve Torak Tuberculosis Thorax. (2017) 65:18–24. doi: 10.5578/tt.48618
9. Davila EP, Zhao W, Byrne M, Hooper MW, Messiah A, Caban-Martinez A, et al. Health-related quality of life and nicotine dependence, Florida 2007. Am J Health Behav. (2011) 35:280–9. doi: 10.5993/AJHB.35.3.3
10. Sarna L, Bialous SA, Cooley ME, Jun HJ, Feskanich D. Impact of smoking and smoking cessation on health-related quality of life in women in the nurses' health study. Qual Life Res. (2008) 17:1217–27. doi: 10.1007/s11136-008-9404-8
11. Gasperini B, Barbadoro P, Cherubini A, Pierri F, D'Errico MM, Di Stanislao F, et al. The earlier the better: health-related quality of life is inversely related to age of smoking cessation in older former Italian smokers. Aging Clin Exp Res. (2017) 29:655–63. doi: 10.1007/s40520-016-0608-4
12. Joseph S, Pascale S, Georges K, Mirna W. Cigarette and waterpipe smoking decrease respiratory quality of life in adults: results from a national cross-sectional study. Pulmon Med. (2012) 2012:868294. doi: 10.1155/2012/868294
13. Kahraman T, Ozdogar AT, Abasiyanik Z, Ozakbas S, Multiple Sclerosis Res G. Associations between smoking and walking, fatigue, depression, and health-related quality of life in persons with multiple sclerosis. Acta Neurol Belgica. (2020) 121:1199–1206. doi: 10.1007/s13760-020-01341-2
14. Chen P.-C., Kuo R. N.-C., Lai C.-K.-T., Lee Y.-C., et al. The relationship between smoking status and health-related quality of life among smokers who participated in a 1-year smoking cessation programme in Taiwan: a cohort study using the EQ-5D. Bmj Open. (2015) 5:Article e007249. doi: 10.1136/bmjopen-2014-007249
15. Danson SJ, Rowland C, Rowe R, Ellis S, Crabtree C, Horsman JM, et al. The relationship between smoking and quality of life in advanced lung cancer patients: a prospective longitudinal study. Supp Care Cancer. (2016) 24:1507–16. doi: 10.1007/s00520-015-2928-x
16. Holahan CK, Holahan CJ, North RJ, Hayes RB, Powers DA, Ockene JK. Smoking status, physical healthrelated quality of life, and mortality in middle-aged and older women. Nicot Tobacco Res. (2013) 15:662–9. doi: 10.1093/ntr/nts182
17. Quezada SM, Langenberg P, Cross RK. Cigarette smoking adversely affects disease activity and disease-specific quality of life in patients with Crohn's disease at a tertiary referral center. Clin Exp Gastroenterol. (2016) 9:307–10. doi: 10.2147/CEG.S104652
18. de Lossada A, Rejas J. Quit smoking is associated with better health-related quality of life in the spanish general population. Quality Life Res. (2014) 23:159.
19. de Lossada A, Rejas J. Health-related quality-of-life in the smoking general population of Spain: an approach from the national health survey [Calidad de vida relacionada con la salud en la poblacion general espanola fumadora: una aproximacion desde la Encuesta Nacional de Salud.]. Semergen. (2016) 42:431–9. doi: 10.1016/j.semerg.2015.09.003
20. Rachiotis G, Behrakis PK, Vasiliou M, Yfantopoulos J. Quality of life and smoking among industrial workers in Greece. La Med Lavoro. (2006) 97:44–50.
21. Rajabi A, Arefnezhad M, Erfanpoor S, Esmaeilzadeh F, Arefnezhad M, Hasani J. Cigarette smoking and health-related quality of life in the general population of iran: independent associations according to gender. Int J Prev Med. (2019) 10:Article 188. doi: 10.4103/ijpvm.IJPVM_526_17
22. Ostbye T, Taylor DH. The effect of smoking on years of healthy life (YHL) lost among middle-aged and older Americans. Health Serv Res. (2004) 39:531–51. doi: 10.1111/j.1475-6773.2004.00243.x
23. Balfour L, Cooper C, Kowal J, Tasca GA, Silverman A, Kane M, et al. Depression and cigarette smoking independently relate to reduced health-related quality of life among Canadians living with hepatitis C. Can J Gastroenterol Hepatol. (2006) 20:81–6. doi: 10.1155/2006/469761
24. Londhe J, Brashier B, Iyer N, Madas S, Juvekar S, Salvi S, et al. Comparison of quality of life in smoking and non-smoking COPD patients in India using St. George's respiratory questionnaire and COPD assessment test. Eur Res J. (2013) 42:4908.
25. Tan NC, Ngoh SHA, Teo SSH, Swah TS, Chen Z, Tai BC. Impact of cigarette smoking on symptoms and quality of life of adults with asthma managed in public primary care clinics in Singapore: a questionnaire study. Primary Care Resp J. (2012) 21:90–3. doi: 10.4104/pcrj.2012.00003
26. Viana DA, Andrade FCD, Martins LC, Rodrigues LR, dos Santos Tavares DM. Differences in quality of life among older adults in Brazil according to smoking status and nicotine dependence. Health Quality Life Outcomes. (2019) 17:Article 1. doi: 10.1186/s12955-018-1072-y
27. WHO. WHO Report on the Global Tobacco Epidemic 2019: Offer Help to Quit Tobacco Use (2019). Available online at: https://EconPapers.repec.org/RePEc:cdl:ctcres:qt1g16k8b9 (accessed January 21, 2022).
28. Rabin R, Charro FD. EQ-SD: a measure of health status from the EuroQol Group. Ann Med. (2001) 33:337–43. doi: 10.3109/07853890109002087
29. Ramos-Goni JM, Rivero-Arias O. eq5d: A command to calculate index values for the EQ-5D quality-of-life instrument. Stata J. (2011) 11:120–5. doi: 10.1177/1536867X1101100108
30. Li X, Li Q, Dong L, Sun B, Chen J, Jiang Y, et al. Risk factors associated with smoking behaviour in recreational venues: findings from the international tobacco control (ITC) China survey. Tobacco Control. (2010) 19 (Supple. 2):i30. doi: 10.1136/tc.2009.031336
31. Kind P, Dolan P, Gudex C, Williams A. Variations in population health status: results from a United Kingdom national questionnaire survey. BMJ. (1998) 316:736–41. doi: 10.1136/bmj.316.7133.736
32. Vogl M, Wenig CM, Leidl R, Pokhrel S. Smoking and health-related quality of life in English general population: implications for economic evaluations. Bmc Public Health. (2012) 12:Article 203. doi: 10.1186/1471-2458-12-203
33. Guiterrez-Bedmar M, Segui-Gomez M, Gomez-Gracia E, Bes-Rastrollo M, Martinez-Gonzalez MA. Smoking status, changes in smoking status and health-related quality of life: findings from the SUN (“Seguimiento Universidad de Navarra”) Cohort. Int J Environ Res Public Health. (2009) 6:310–20. doi: 10.3390/ijerph6010310
34. Perelman NL, Kolosov VP, Perelman JM, Naryshkina SV. The influence of smoking on health related quality of life in asthmatics. Eur Res J. (2015) 46:5026. doi: 10.1183/13993003.congress-2015.PA5026
35. Uchoa Sales MP, Oliveira MI, Mattos IM, Sampaio Viana CM, Barros Pereira ED. The impact of smoking cessation on patient quality of life. J Brasil De Pneumol. (2009) 35:436–41. doi: 10.1590/S1806-37132009000500008
36. Toghianifar N, Najafian J, Pooya A, Rabiei K, Eshrati B, Anaraki J, et al. Association of smoking status with quality of life in a cross-sectional population-based sample of iranian adults: isfahan healthy heart program. Asia Pacific J Public Health. (2012) 24:786–94. doi: 10.1177/1010539511403800
37. Glantz S, Gonzalez M. Effective tobacco control is key to rapid progress in reduction of non-communicable diseases. Lancet. (2012) 379:1269–71. doi: 10.1016/S0140-6736(11)60615-6
38. Mckay KA, Tremlett H, Fisk JD, Patten SB, Fiest K, Berrigan L, et al. Adverse health behaviours are associated with depression and anxiety in multiple sclerosis: a prospective multisite study. Mult Scl. (2016) 22:685–93. doi: 10.1177/1352458515599073
39. Weiland TJ, Jelinek GA, Marck CH, Hadgkiss EJ, van der Meer DM, Pereira NG, et al. Clinically significant fatigue: prevalence and associated factors in an international sample of adults with multiple sclerosis recruited via the internet. PLoS ONE. (2015) 10:e0115541. doi: 10.1371/journal.pone.0115541
Keywords: smoking, health-related quality of life, adult smoking, quality of life, association
Citation: Cheng X and Jin C (2022) The Association Between Smoking and Health-Related Quality of Life Among Chinese Individuals Aged 40 Years and Older: A Cross-Sectional Study. Front. Public Health 10:779789. doi: 10.3389/fpubh.2022.779789
Received: 19 September 2021; Accepted: 28 January 2022;
Published: 24 February 2022.
Edited by:
Samer A. Kharroubi, American University of Beirut, LebanonReviewed by:
Iffat Elbarazi, United Arab Emirates University, United Arab EmiratesJunling Gao, Fudan University, China
Copyright © 2022 Cheng and Jin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chenggang Jin, cgjin2005@126.com
 Xi Cheng
Xi Cheng Chenggang Jin
Chenggang Jin