- 1Department of Pharmacology, Riphah International University, Lahore, Pakistan
- 2Department of Pharmacology and Toxicology, University of Veterinary and Animal Sciences, Lahore, Pakistan
- 3Department of Botany, Division of Science and Technology, University of Education, Lahore, Pakistan
- 4Department of Parasitology, University of Veterinary and Animal Sciences, Lahore, Pakistan
The emergence of a pathogen responsible for a mysterious respiratory disease was identified in China and later called a novel coronavirus. This disease was named COVID-19. The present study seeks to determine the epidemiological and clinical characteristics of COVID-19 in Pakistan. This report will exhibit a linkage between epidemiology and clinical aspects which in turn can be helpful to prevent the transmission of the virus in Pakistan. A retrospective, multiple center study was performed by collecting the data from patients' with their demographics, epidemiological status, history of co-morbid conditions, and clinical manifestations of the disease. The data was collected from 31 public-sector and 2 private hospitals across Pakistan by on-field healthcare workers. A Chi-square test was applied to assess the relationship between categorical data entries. A total of 194 medical records were examined. The median age of these patients was found to be 34 years. A total of 53.6% active cases were present including 41.2% males and 12.4% females till the end of the study. Adults accounted for most of the cases (94.3%) of COVID-19. Fever (86.60%), cough (85.05%), fatigue (36.60%), dyspnea (24.74%), and gastrointestinal discomfort (10.31%) were among the most frequently reported signs and symptoms by the patients. However, 4.12% of the total patient population remained asymptomatic. The median duration of hospital stay was found to be 14 (0–19) days. The earliest source of the spread of the virus may be linked to the foreigners traveling to Pakistan. Spread among men was more as compared to women. A few cases were found to be positive, due to the direct contact with pets or livestock. Hypertension (7.73%), diabetes (4.64%), cardiovascular conditions (2.58%) were the most common co-morbidities. The percentage mortality was 2.50% with the highest mortality among elders.
Introduction
In December 2019, an event of respiratory disease due to an unknown cause with similarities to that of pneumonia was identified in China (1). Later, the World Health Organization (WHO) acknowledged it to be the sixth emergency service of public health on January 30, 2020 (2) and declared it as a global pandemic in March 2020 (3, 4). On February 11, 2020, the WHO named this viral pneumonia as Corona Virus Disease-19 (COVID-19) (5). The metagenomics analysis was performed through the samples of bronchoalveolar lavage taken from the infected patients (6) and the newly identified pathogen was named as 2019 novel coronavirus (2019-nCoV) by the United States Center for Disease Control and Prevention (CDC) (7). The COVID-19 had almost 88% genetic resemblance to the severe acute respiratory syndrome (SARS). Two SARS viruses were bat-derived coronaviruses bat-SL-CoVZXC21 and bat-SL-CoVZC45 (8). The receptor for the COVID-19 virus is the same as that of SARS-CoV, i.e., angiotensin-converting enzyme-2, ACE-2 receptor (9). The novel corona virus is now listed as the 7th member of the coronavirus family (10).
Multiple epidemiological studies reported that the COVID-19 is identified in Wuhan, China on December 8, 2019 (2, 11–13). This disease later spread worldwide including Iran, Europe, India, United Kingdom (UK), and Pakistan, and officially became a pandemic on March 11, 2020 (13, 14). In Pakistan, the first incidence of this disease was identified at the end of February 2020 (15, 16). COVID-19 is extremely contagious and its spread takes place via human-to-human transmissions (17). As of February 15, 2021, the total reported cases in Pakistan were 564,077, while total deaths were around 12,333 and the total recovered were 525,277, as per the data released by the Government of Pakistan (https://covid.gov.pk/).
The coronavirus is encased with an exceptionally huge positive-sense strand of the RNA genome, which mutates very rapidly due to errors in the RNA (10, 18). Pertaining to its continuous mutation, it is highly contagious and may be identified in several animals (19–21). In one of the Indian analysis, the prediction was floated that the cases of COVID-19 will keep on increasing with higher transmission rates as well as with seasonal occurrences (22, 23). Several mathematical models have suggested that the spread of the virus may be retarded by taking precautionary measures including social distancing, isolation, and contact tracing (24, 25). In humans, some patients may remain asymptomatic or may be a carrier of the disease (26–29).
In Pakistan, some patients were reported to be asymptomatic which may serve as a carrier to other people, if not managed properly (30, 31). The purpose of this study is to assess heedfully the epidemiological and clinical characteristics of COVID-19 in Pakistan. This study will exhibit a linkage between epidemiology and clinical aspects which in turn can be helpful to prevent the transmission of the virus in Pakistan.
Materials and Methods
A retrospective, multiple center study was performed by collecting the patient's demographics, epidemiological status, history of co-morbid conditions, and assessment of clinical manifestations. The data were collected from 33 hospitals (31 public sector hospitals and 2 private sector hospitals) with the help of in-field healthcare workers i.e., doctors, nurses, or pharmacists of the respective hospitals involved in the medical care of these patients. The diagnosis of COVID-19 was made either by taking a specimen from a throat swab and then performing a Real Time-Polymerase Chain Reaction (RT-PCR) in a laboratory setting or by evaluating the clinical symptoms to ascertain the diagnosis. There were 189 lab-confirmed cases; on the other hand, five patients were diagnosed with definitive travel history, signs, and symptoms of COVID-19.
Data collection was initiated on March 16, 2020, and the follow-up of the study was made on April 14th, 2020. Whereas, the data of a few patients were also collected by the end of April 2020. The confirmed 194 cases of the disease through either RT-PCR or clinical diagnosis were considered. A total of 192 cases were confirmed by RT-PCR whereas 2 cases were diagnosed based on clinical manifestations.
Ethical Approval was conferred from Riphah International University, Lahore, Pakistan (Letter No. RCVETS-701). Efforts were made to ensure data collection from different provinces of Pakistan including Punjab, Sindh, Khyber Pakhtunkhwa, Gilgit Baltistan, Islamabad, and Azad Jammu and Kashmir (AJK), a self-governing state under the constitution of Pakistan.
Statistical Analysis
The data were analyzed by using Statistical Package for Social Sciences version 21 (SPSSv21). Frequency, percentages, median, ranges, and interquartile ranges were used to display data. Mann-Whitney U-test was used for comparison across the groups. A Chi-square test was applied to assess the relationship between categorical data entries.
Results
As of April 14, 2020, epidemiological data of 194 patients were collected including 10 (5.15%) patients from the Sindh province, 157 (80.93%) from Punjab, 2 (1.03%) from Islamabad, 3 (1.55%) patients from Gilgit-Baltistan (GB), 6 (3.09%) patients from Khyber Pakhtunkhwa (KPK), and 16 (8.25%) from AJK. The team was unable to collect any data from the province of Baluchistan, the least populated province, due to limited resources. Figure 1A depicts the locations and the amount of patient data collected from that facility. On the other hand, Figure 1B represents the official data by the Government of Pakistan (http://covid.gov.pk/stats/pakistan) of all the patients throughout the country as of April 13, 2020, at 0530 h.
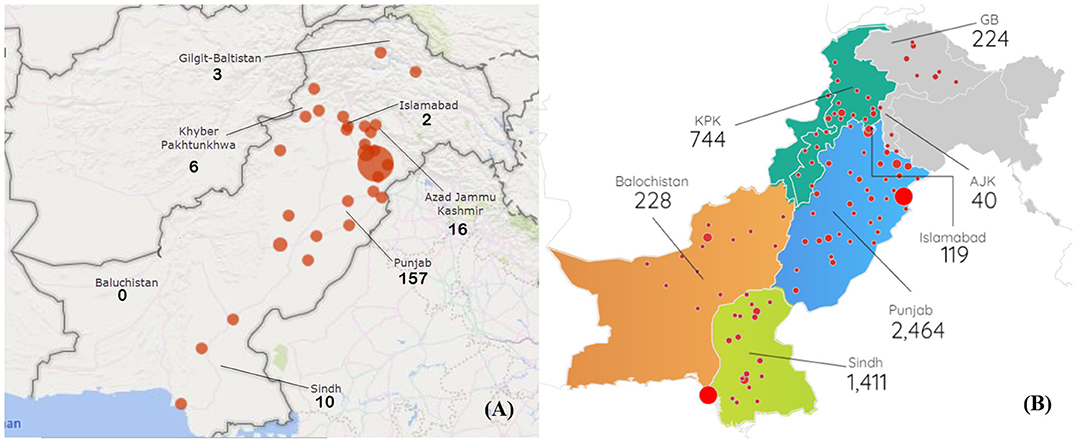
Figure 1. (A) Depicts the sample data distribution throughout the country. (B) Represents the population data generated by Government of Pakistan. The size red dots represents the number of the patient data collected from each district in (A) whereas, the red dots in (B) represents the number of active patients. The values below each province name represents the number of patients.
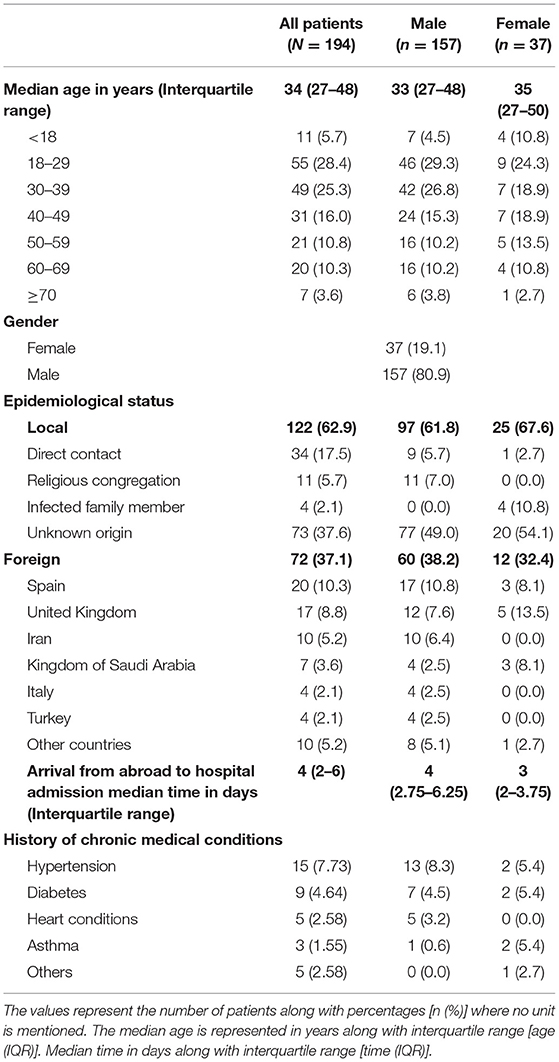
A total of 194 patients' medical records were examined. The median age of these patients was found to be 34 years with an interquartile range (IQR) of 27–48 years. The youngest patient was 6 months old, whereas the oldest one was 87 years of age. Adults accounted for most of the active cases of COVID-19 with 55 (28.4%) patients in 18–29 years of age, 49 (25.3%), 31 (16.0%), and 21 (10.8%) patients were found to be in the age ranges of 30–39, 40–49, and 50–59 years, respectively. The study also included 27 older patients altogether as per locally accepted criterion of old aged individuals. 11 (5.7%) of young patients were also infected.
The distribution of infected males and females were found to be 157 (80.9%) and 37 (19.1%), respectively (Table 1). One of the females was pregnant and tested positive for COVID-19 although, she remained asymptomatic with no reported complications.
The earliest hospital admission of our sample dates was back on February 26, 2020, of a patient who had a recent prior visit to Iran. However, this patient presented to the hospital after 20 days of arrival in Pakistan. Most of the earlier cases were found to be amongst the foreigners. A total of 72 (37.1%) patients had a recent travel history abroad and local transmission comprised 122 patients (62.9%) in this study. Among patients with travel history, 20 (10.3%) patients were from Spain, 17 (8.8%) from the United Kingdom, 10 (5.0%) from Iran, and 7 (3.6%) were from the Kingdom of Saudi Arabia. For most of the patients, the transmission was found to be of unknown origin (37.6%) since they did not have a substantial travel history and were unaware of any contact that could have infected them. 34 (17.5%) individuals had direct contact with the already infected patients of COVID-19. Paramedical staff and doctors are at great risk due to a lack of proper PPE and safety equipment. Among the data collected from different hospitals, most of the patients got infected by direct contact from healthcare providers, including 12 physicians and five paramedical staff. Besides, it was observed that individuals with more public exposure were part of our study, including an epidemiologist, a religious scholar, a lawyer, and a news reporter.
Hypertension was observed to be the most prevalent co-morbidity affecting 15 (7.73%) patients of the total sample. This was followed by diabetes (4.64%), heart conditions (2.58%), asthma (1.55%), and other minor co-morbidities (2.58%) (Table 1).
Clinical Manifestations
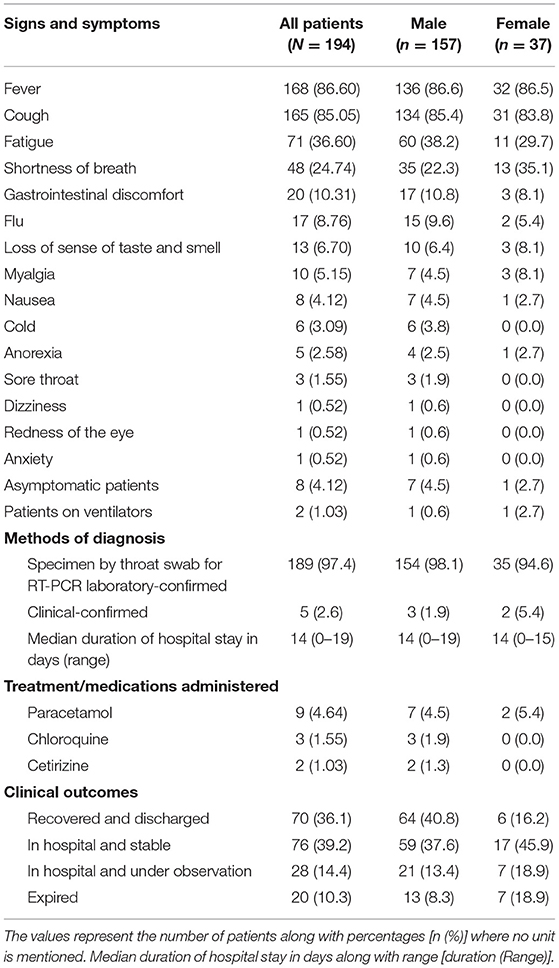
The signs and symptoms of the patients were recorded, and 168 (86.60%) patients exhibited fever. The cough was the second most frequent sign and was experienced by 165 (85.05%) of the patients. 71 (36.60%) patients' complaints of having fatigue. Dyspnea or shortness of breath was the next most occurring symptom (24.74%). Some of the patients also (10.31%) reported gastrointestinal discomfort. 17 (8.76%) patients had the flu, whereas six patients had a cold. Surprisingly, a considerable number of patients (6.70%) also reported a loss of sense of smell and taste. Myalgia, nausea, anorexia, and sore throat were reported by 10 (5.15%), 8 (4.12%), 5 (2.58%), and 3 (1.55%) of patients, respectively. Redness of eyes, dizziness, and anxiety was also observed in 0.52% of the patients. Conversely, 8 (4.12%) patients were asymptomatic. Two patients were put on ventilators; however, both patients expired.
The median duration of hospitalization for COVID-19 patients was found to be 14 days with a stay range of as low as 0 days and as high as 43 days. Paracetamol was the most prescribed medicine (4.64%), followed by chloroquine (1.55%) and cetirizine (1.03%).
Clinical outcomes were evaluated in the last section of data collection. As of April 14, 2020, a total of 70 (36.1%) patients were recovered and discharged. On the other hand, 20 (10.3%) of the deaths were reported. The rest of the patients were still in the hospital, 76 (39.2%) of them were stable and more likely to be discharged in a few days, while 28 (14.4%) patients were still under observation out of which 23 (11.8%) patients recovered and 5 (2.5%) died as per data collected by the end of April 2020. A total of 53.6% active cases were present including 41.2% males and 12.4% females till the end of the study (Table 2).
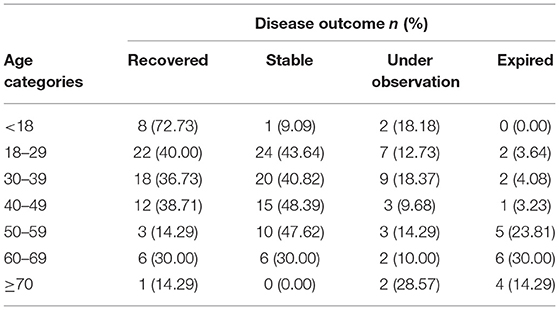
Mann-Whitney U-test was applied to evaluate the clinical outcomes of the disease against the patients' age. It was observed that the patients who were recovered had an average age of 33.66 years. The patients who were kept in hospital but were stable had an average age of 37.51 years; those under observation had an average age of 38.61 years. Patients who expired were having an average age of 55.30 years (P < 0.05). The highest recovery percentage (72.73%) was among young patients with ages <18 years whereas; the highest mortality percentage was among older patients with an age range of 60–69 years (Table 3).
Discussion
As of April 11, 2020, the COVID-19 attained over 1.6 million cases as per WHO, claiming nearly a hundred thousand lives (32). Recent data presents that COVID-19 cases have been increased and crossed over 80 million globally by February 2021, according to WHO. Pakistan is also amongst the countries affected most by this pandemic with estimated cases of over 0.5 million by February 2021 and a mortality rate of 1.7% (33).
The median age of infected individuals was 34 years. The adult age group (19–59 years) was more affected by the infection. The population demographics of the country, according to the 1998 census, suggesting that nearly 40% of the country's population comprises adults whereas, 53% of the total population is under 19 years of age. 5.54% of the total population is above 60 years of age (34). The occurrence of the infection in females (19.1%) is less as compared to the male (80.9%) population. Our results bear similarity to a recent study in China, where the percentage of the infected females was lesser as compared to the males (26, 35). A previous study also suggested that male mice were more susceptible to the SARS-CoV and MERS-CoV as compared to the female mice (36). Currently, there is no reliable evidence regarding the influence of sex on the susceptibility of the infection. Hence, further studies are required to ascertain this behavior.
The earliest source of the spread of the virus may be linked to the foreigners entering Pakistan from Iran. The disease outbreak in Iran was reported in late January 2020, but the first cases of COVID-19 were identified in late February 2020 (37). Therefore, the dissemination of the virus in Pakistan may be firstly linked to Iran. The travelers from Spain contributed to the highest number of infected patients. According to our data, the local transmission of the virus was massive in the province of Punjab, which is one of the most populated provinces of Pakistan (38). There is already strong evidence of human-to-human transmission of the disease (39). Our study also confirms that individuals with more public exposure are at a higher risk of acquiring the disease. Furthermore, the religious congregations held in March also led to an increased number of cases. Therefore, social distancing must be encouraged to avoid the exponential dissemination of the disease (40, 41).
Another alarming situation observed in our study was the fact that 17 (8.76%) healthcare workers including physicians and paramedics were found to be infected (42, 43). They were also affected by stress and anxiety during the pandemic (44, 45). During the recent coronavirus outbreak in China, a substantial number of healthcare workers acquired the infection (43, 46). A study from China reported that 3.8% of healthcare workers were affected by the disease (47). Another publication discussed the mortality of 23 healthcare workers along with two physicians in China bringing in light the risk these health workers deal with within their daily routine (48). However, in our study, this percentage is quite higher as compared to the reported studies. The lack of personal protective equipment (PPE), prolonged exposure to patients, and inadequate knowledge of the disease transmission among the healthcare providers may have increased such incidents (49, 50). Increased awareness of self-protection, adequate supplies of PPE, and a prompt response may aid in decreased susceptibility of infection among healthcare workers (46, 51, 52).
The most prevalent comorbidities in our study were hypertension, diabetes, cardiovascular conditions, and asthma. A similar pattern was also found in different studies where hypertension was the most prevalent co-morbidity followed by diabetes, heart diseases, and respiratory illnesses (53–55). Some other studies revealed the same pattern as mentioned earlier, with hypertension, diabetes, and cardiovascular diseases as the prime co-morbidities (56, 57).
Fever, cough, fatigue, dyspnea, and gastrointestinal discomfort were among the most frequently reported signs and symptoms by the patients (58). The clinical symptoms of 100 patients admitted to a hospital in Karachi included dry cough, fever, lethargy, fatigue, dyspnea, myalgia, vomiting, nausea, and diarrhea (59). A single-center study from Pakistan has depicted a similar trend of clinical symptoms as our study (60). Other studies have reported a similar set of signs and symptoms (61–63). However, 4.12% of the total patient population remained asymptomatic. This trend is also like the other studies (62, 64, 65). Surprisingly, 6.70% of the patients reported a loss of sense of smell and taste which along with other symptoms, is a strong predictor of COVID-19 infection (66–69). Moreover, flu, myalgia, nausea, cold, anorexia, sore throat, dizziness, redness of the eyes, and anxiety were also reported (45, 63, 70).
Paracetamol, chloroquine, and cetirizine were the most frequently prescribed medicines during the early days of the COVID-19 pandemic in Pakistan (71–74). However, the current data is insufficient to assess the effect of medications on the outcome of the disease. Paracetamol was the most prescribed medicine as it is the safest drug for managing the COVID-19 symptoms in place of ibuprofen (75), followed by chloroquine which is being imagined as a miracle drug (76). Altogether, 20 deaths were reported in our study 104 (53.61%) patients were still hospitalized, with 76 patients in stable condition, and the rest 28 patients were still under observation. Complete recovered patients 70 (36.1%) and were discharged from the hospital. Out of 28 patients, 23 (11.8%) patients recovered and 5 (2.5%) died by the end of April 2020.
There might be a link between COVID-19 with the human population and animals. Some zoo animals were also reported positive for SARS-CoV-2, however, under experimental conditions, chicken and ducks were not affected with COVID-19 (77). Inter-specie transmission of COVID-19 was very recent and must be addressed after conducting different research studies. Different experimental trials suggest that pets (cats, dogs) might also be susceptible to SARS-CoV-2 from humans (19, 78).
The present study has some limitations since 53.61% of the sample patients were still hospitalized, and the recovery of these patients was not ascertained. The data collected was not evenly distributed throughout the country. Moreover, remained unable to investigate more clinical indicators such as complete blood count, CT scans, or chest X-rays since there were a limited number of tests performed by the hospitals. The non-availability of data such as the date of onset of symptoms had prevented us from evaluating more factors such as the incubation period of the virus. The current study is amongst one of the first studies to portray the epidemiological picture of COVID-19 in Pakistan. Being a lower-middle-income country, Pakistan is facing many challenges from inadequate health facilities to poor socioeconomic conditions. Our study may help in identifying and developing a response that may alleviate the rapid onset of disease.
Conclusions
The earliest source of the spread of the virus may be linked to the foreigners traveling Pakistan. Spread among men was more as compared to females. Fever, cough, fatigue, dyspnea are the most common symptoms. A few positive cases were found to be directly in contact with pets or livestock. Hypertension, diabetes, cardiovascular conditions are the most common co-morbidities. The percentage mortality was 2.50% with the highest mortality among elders.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Ethics Committee (IEC) of Riphah College of Veterinary Sciences. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
MA and BB conceived the idea and did a write-up of the manuscript. SR did the critical appraisal of findings with literature search. SA, AM, and RM did the acquisition of patient data and drafting of the article. SM did the analysis and interpretation of the data. MH and MR did general supervision of the research group and final approval of the version to be published. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. (2020) 382:1199–207. doi: 10.1056/NEJMoa2001316
2. Bilgin S, Kurtkulagi O, Kahveci GB, Duman TT, Tel BMA. Millennium pandemic: a review of coronavirus disease (COVID-19). Exp Biomed Res. (2020) 3:117–25. doi: 10.30714/j-ebr.2020259176
3. Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. (2020) 91:157–60. doi: 10.23750/abm.v91i1.9397
4. Tam PCK, Ly KM, Kernich ML, Spurrier N, Lawrence D, Gordon DL, et al. Detectable severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in human breast milk of a mildly symptomatic patient with coronavirus disease 2019 (COVID-19). Clin Infect Dis. (2021) 72:128–30. doi: 10.1093/cid/ciaa673
5. Rodriguez-Morales AJ, Bonilla-Aldana DK, Tiwari R, Sah R, Rabaan AA, Dhama K. COVID-19, an emerging coronavirus infection: current scenario and recent developments-an overview. J Pure Appl Microbiol. (2020) 14:5–12. doi: 10.22207/JPAM.14.1.02
6. Wu Y, Wang T, Guo C, Zhang D, Ge X, Huang Z, et al. Plasminogen improves lung lesions and hypoxemia in patients with COVID-19. QJM. (2020) 113:539–45. doi: 10.1093/qjmed/hcaa121
7. Paules CI, Marston HD, Fauci AS. Coronavirus infections—more than just the common cold. JAMA. (2020) 323:707–8. doi: 10.1001/jama.2020.0757
8. Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. (2020) 395:565–74. doi: 10.1016/S0140-6736(20)30251-8
9. Kumar A, Narayan RK, Kumari C, Faiq MA, Kulandhasamy M, Kant K, et al. SARS-CoV-2 cell entry receptor ACE2 mediated endothelial dysfunction leads to vascular thrombosis in COVID-19 patients. Med Hypotheses. (2020) 145:1–5. doi: 10.1016/j.mehy.2020.110320
10. Barua R, Datta S, Roychowdhury A, Datta P. The study of the epidemiology and clinical features of the novel coronavirus (COVID-19). In: Taukeni SG, editor. Epidemiological Research Applications for Public Health Measurement and Intervention. IGI Global (2021). p. 25–39.
11. COVID C, Team R. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:343–6. doi: 10.15585/mmwr.mm6912e2
12. Khan S, Siddique R, Bai Q, Shabana, Liu Y, Xue M, et al. Coronaviruses disease 2019 (COVID-19): causative agent, mental health concerns, and potential management options. J Infect Public Health. (2020) 13:1840–4. doi: 10.1016/j.jiph.2020.07.010
13. Waris A, Atta UK, Ali M, Asmat A, Baset A. COVID-19 outbreak: current scenario of Pakistan. New Microbes New Infect. (2020) 35:1–6. doi: 10.1016/j.nmni.2020.100681
14. Weber A, Ianelli F, Goncalves S. Trend analysis of the COVID-19 pandemic in China and the rest of the world. arXiv preprint arXiv:200309032. (2020). doi: 10.1101/2020.03.19.20037192
15. Mehmood K, Bao Y, Abrar MM, Petropoulos GP, Saifullah, Soban A, et al. Spatiotemporal variability of COVID-19 pandemic in relation to air pollution, climate and socioeconomic factors in Pakistan. Chemosphere. (2021) 271:1–11. doi: 10.1016/j.chemosphere.2021.129584
16. Baloch GM, Sundarasen S, Chinna K, Nurunnabi M, Kamaludin K, Khoshaim HB, et al. COVID-19: exploring impacts of the pandemic and lockdown on mental health of Pakistani students. PeerJ. (2021) 9:1–15. doi: 10.7717/peerj.10612
17. Pongpirul WA, Pongpirul K, Ratnarathon AC, Prasithsirikul W. Journey of a Thai taxi driver and novel coronavirus. N Engl J Med. (2020) 382:1067–8. doi: 10.1056/NEJMc2001621
18. Drexler JF, Gloza-Rausch F, Glende J, Corman VM, Muth D, Goettsche M, et al. Genomic characterization of SARS-related coronavirus in European bats and classification of coronaviruses based on partial RNA-dependent RNA polymerase gene sequences. J. Virol. (2010) 84:11336–49. doi: 10.1128/JVI.00650-10
19. Shi J, Wen Z, Zhong G, Yang H, Wang C, Huang B, et al. Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS–coronavirus 2. Science. (2020) 368:1016–20. doi: 10.1126/science.abb7015
20. Liu H, Zhang Q, Wei P, Chen Z, Aviszus K, Yang J, et al. The basis of a more contagious 501Y.V1 variant of SARS-COV-2. bioRxiv [Preprint]. (2021) 1–25. doi: 10.1101/2021.02.02.428884
21. Zahradnik J, Marciano S, Shemesh M, Zoler E, Chiaravalli J, Meyer B, et al. SARS-CoV-2 RBD in vitro evolution follows contagious mutation spread, yet generates an able infection inhibitor. bioRxiv [Preprint]. (2021) 1–41. doi: 10.1101/2021.01.06.425392
22. Khajanchi S, Sarkar K. Forecasting the daily and cumulative number of cases for the COVID-19 pandemic in India. Chaos. (2020) 30:071101–16. doi: 10.1063/5.0016240
23. Khajanchi S, Sarkar K, Mondal J, Perc M. Dynamics of the COVID-19 pandemic in India. arXiv preprint arXiv:200506286. (2020). doi: 10.21203/rs.3.rs-27112/v1
24. Samui P, Mondal J, Khajanchi S. A mathematical model for COVID-19 transmission dynamics with a case study of India. Chaos Solitons Fractals. (2020) 140:1–11. doi: 10.1016/j.chaos.2020.110173
25. Sarkar K, Khajanchi S, Nieto JJ. Modeling and forecasting the COVID-19 pandemic in India. Chaos Solitons Fractals. (2020) 139:1–16. doi: 10.1016/j.chaos.2020.110049
26. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
27. Al-Qahtani M, AlAli S, AbdulRahman A, Salman Alsayyad A, Otoom S, Atkin SL. The prevalence of asymptomatic and symptomatic COVID-19 in a cohort of quarantined subjects. Int J Infect Dis. (2021) 102:285–8. doi: 10.1016/j.ijid.2020.10.091
28. Smalley DL, Cisarik PM, Grantham J, Cloud W, Neil RB, DePriest P. Impact of pool testing in detection of asymptomatic patients with COVID-19. Lab Med. (2021) 52:e15–6. doi: 10.1093/labmed/lmaa094
29. Kronbichler A, Kresse D, Yoon S, Lee KH, Effenberger M, Shin JI. Asymptomatic patients as a source of COVID-19 infections: a systematic review and meta-analysis. Int J Infect Dis. (2020) 98:180–6. doi: 10.1016/j.ijid.2020.06.052
30. Haqqi A, Awan UA, Ali M, Saqib MAN, Ahmed H, Afzal MS. COVID-19 and dengue virus coepidemics in Pakistan: a dangerous combination for an overburdened healthcare system. J Med Virol. (2021) 93:80–2. doi: 10.1002/jmv.26144
31. Gao Z, Xu Y, Sun C, Wang X, Guo Y, Qiu S, et al. A systematic review of asymptomatic infections with COVID-19. J Microbiol Immunol Infect. (2021) 54:12–6. doi: 10.1016/j.jmii.2020.05.001
35. Guan W-j, Ni Z-y, Hu Y, Liang W-h, Ou C-q, He J-x, et al. Clinical characteristics of 2019 novel coronavirus infection in China. MedRxiv [Preprint]. (2020) 1–30.
36. Channappanavar R, Fett C, Mack M, Ten Eyck PP, Meyerholz DK, Perlman S. Sex-based differences in susceptibility to severe acute respiratory syndrome coronavirus infection. J Immunol. (2017) 198:4046–53. doi: 10.4049/jimmunol.1601896
37. Tuite AR, Bogoch II, Sherbo R, Watts A, Fisman D, Khan K. Estimation of coronavirus disease 2019 (COVID-19) burden and potential for international dissemination of infection from Iran. Ann Intern Med. (2020) 172:699–701. doi: 10.7326/M20-0696
38. Saeed U, Sherdil K, Ashraf U, Mohey-Ud-Din G, Younas I, Butt HJ, et al. Identification of potential lockdown areas during COVID-19 transmission in Punjab, Pakistan. Public Health. (2021) 190:42–51. doi: 10.1016/j.puhe.2020.10.026
39. Shereen MA, Khan S, Kazmi A, Bashir N, Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res. (2020) 24:91–8. doi: 10.1016/j.jare.2020.03.005
40. Dalton CB, Corbett SJ, Katelaris AL. Pre-emptive low cost social distancing and enhanced hygiene implemented before local COVID-19 transmission could decrease the number and severity of cases. Med J Austral. (2020) 212:1–10. doi: 10.2139/ssrn.3549276
41. Carriere J, Shafi H, Brehon K, Pohar Manhas K, Churchill K, Ho C, et al. Utilizing AI and NLP to assist with healthcare and rehabilitation during the COVID-19 pandemic: a perspective. Front Artif Intell. (2021) 4:613637. doi: 10.3389/frai.2021.613637
42. Gómez-Ochoa SA, Franco OH, Rojas LZ, Raguindin PF, Roa-Díaz ZM, Wyssmann BM, et al. COVID-19 in health-care workers: a living systematic review and meta-analysis of prevalence, risk factors, clinical characteristics, and outcomes. Am J Epidemiol. (2021) 190:161–75. doi: 10.1093/aje/kwaa191
43. Chen T, Li G, Liu H, Wan W, Zheng H, Chen C. Clinical characteristics of 132 healthcare worker cases with COVID-19: a retrospective study from a single center in Wuhan, China. J Med Virol. (2021) 93:1631–8. doi: 10.1002/jmv.26511
44. Akman C, Cetin M, Toraman C. The analysis of emergency medicine professionals' occupational anxiety during the COVID-19 pandemic. Signa Vitae. (2021) 17:1–15. doi: 10.22514/sv.2021.023
45. Liu Y, Chen H, Zhang N, Wang X, Fan Q, Zhang Y, et al. Anxiety and depression symptoms of medical staff under COVID-19 epidemic in China. J Affect Disord. (2021) 278:144–8. doi: 10.1016/j.jad.2020.09.004
46. Wang J, Zhou M, Liu F. Exploring the reasons for healthcare workers infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect. (2020) 30101–8. doi: 10.1016/j.jhin.2020.03.002
47. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. (2020) 1239–42. doi: 10.1001/jama.2020.2648
48. Ing EB, Xu QA, Salimi A, Torun N. Physician deaths from corona virus (COVID-19) disease. Occup Med. (2020) 70:370–4. doi: 10.1093/occmed/kqaa088
49. Jackson D, Anders R, Padula WV, Daly J, Davidson PM. Vulnerability of nurse and physicians with COVID-19: monitoring and surveillance needed. J Clin Nurs. (2020) 29:3584–7. doi: 10.1111/jocn.15347
50. Sun S, Xie Z, Yu K, Jiang B, Zheng S, Pan X. COVID-19 and healthcare system in China: challenges and progression for a sustainable future. Global Health. (2021) 17:1–8. doi: 10.1186/s12992-021-00665-9
51. Cobb N, Papali A, Pisani L, Schultz MJ, Ferreira JC, For The Covid-Lmic Task F. Pragmatic recommendations for infection prevention and control practices for healthcare facilities in low- and middle-income countries during the COVID-19 pandemic. Am J Trop Med Hyg. (2021) 104:25–33. doi: 10.4269/ajtmh.20-1009
52. Gohel KH, Patel PB, Shah PM, Patel JR, Pandit N, Raut A. Knowledge and perceptions about COVID-19 among the medical and allied health science students in India: an online cross-sectional survey. Clin Epidemiol Global Health. (2021) 9:104–9. doi: 10.1016/j.cegh.2020.07.008
53. Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis. (2020) 1–14. doi: 10.1016/j.ijid.2020.03.017
54. Naveed M, Naeem M, ur Rahman M, Hilal MG, Khel MAK, Ali G, et al. Who is a potential risk groups to coronavirus disease 2019 (COVID-19) a-review. New Microbes New Infect. (2021) 100849. doi: 10.1016/j.nmni.2021.100849
55. Emami A, Javanmardi F, Akbari A, Kojuri J, Bakhtiari H, Rezaei T, et al. Survival rate in hypertensive patients with COVID-19. Clin Exp Hypertens. (2021) 43:77–80. doi: 10.1080/10641963.2020.1812624
56. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. (2020) 382:1708–20. doi: 10.1056/NEJMoa2002032
57. Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. (2020) 75:1730–41. doi: 10.1111/all.14238
58. Schettino M, Pellegrini L, Picascia D, Saibeni S, Bezzio C, Bini F, et al. Clinical characteristics of COVID-19 patients with gastrointestinal symptoms in Northern Italy: a single-center cohort study. Am J Gastroenterol. (2021) 116:306–10. doi: 10.14309/ajg.0000000000000965
59. Asghar MS, Kazmi SJH, Khan NA, Akram M, Khan SA, Rasheed U, et al. Clinical profiles, characteristics, and outcomes of the first 100 admitted COVID-19 patients in Pakistan: a single-center retrospective study in a tertiary care Hospital of Karachi. Cureus. (2020) 12:c34. doi: 10.7759/cureus.c34
60. Khan M, Khan H, Khan S, Nawaz M. Epidemiological and clinical characteristics of coronavirus disease (COVID-19) cases at a screening clinic during the early outbreak period: a single-centre study. J Med Microbiol. (2020) 69:1114. doi: 10.1099/jmm.0.001231
61. Qian GQ, Yang NB, Ding F, Ma AHY, Wang ZY, Shen YF, et al. Epidemiologic and clinical characteristics of 91 hospitalized patients with COVID-19 in Zhejiang, China: a retrospective, multi-centre case series. QJM. (2020) 113:474–81. doi: 10.1093/qjmed/hcaa089
62. Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. Features, evaluation and treatment coronavirus (COVID-19). In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing (2020).
63. Weng LM, Su X, Wang XQ. Pain symptoms in patients with coronavirus disease (COVID-19): a literature review. J Pain Res. (2021) 14:147–59. doi: 10.2147/JPR.S269206
64. Bai Y, Yao L, Wei T, Tian F, Jin DY, Chen L, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. (2020) 323:1406–7. doi: 10.1001/jama.2020.2565
65. Imran T, Naz HA, Khan H, Bangash AH, Khan LB, Khan H. Joint CBC-ICT Interpretation for the pre-surgical screening of COVID 19 asymptomatic cases: a cross-sectional study. Nature. (2020) 1–8:1037–40. doi: 10.1101/2020.07.16.20138354
66. Menni C, Valdes A, Freydin MB, Ganesh S, Moustafa JE-S, Visconti A, et al. Loss of smell and taste in combination with other symptoms is a strong predictor of COVID-19 infection. medRxiv [Preprint]. (2020) 26. doi: 10.1101/2020.04.05.20048421
67. Callejon-Leblic MA, Moreno-Luna R, Del Cuvillo A, Reyes-Tejero IM, Garcia-Villaran MA, Santos-Peña M, et al. Loss of smell and taste can accurately predict COVID-19 infection: a machine-learning approach. J Clin Med. (2021) 10:570. doi: 10.3390/jcm10040570
68. Hjelmesæth J, Skaare D. Loss of smell or taste as the only symptom of COVID-19. Tidsskrift for Den norske legeforening (2020). doi: 10.4045/tidsskr.20.0287
69. Elangovan S. Acute loss of smell or taste without nasal blockage should raise suspicion for COVID-19 infection. J Evid Based Dental Prac. (2021) 21:101525. doi: 10.1016/j.jebdp.2020.101525
70. Paredes MR, Apaolaza V, Fernandez-Robin C, Hartmann P, Yanez-Martinez D. The impact of the COVID-19 pandemic on subjective mental well-being: the interplay of perceived threat, future anxiety and resilience. Pers Individ Dif. (2021) 170:110455. doi: 10.1016/j.paid.2020.110455
71. Hassan SM, Sohail H, Iftikhar A, Rathore R, Fatima Q. Pharmacologic agents for the management of COVID-19: a review. Int J Commun Med Public Health. (2021) 8:446. doi: 10.18203/2394-6040.ijcmph20205735
72. Gasmi A, Peana M, Noor S, Lysiuk R, Menzel A, Gasmi Benahmed A, et al. Chloroquine and hydroxychloroquine in the treatment of COVID-19: the never-ending story. Appl Microbiol Biotechnol. (2021) 105:1333–43. doi: 10.1007/s00253-021-11094-4
73. Goscianska J, Olejnik A, Ejsmont A, Galarda A, Wuttke S. Overcoming the paracetamol dose challenge with wrinkled mesoporous carbon spheres. J Colloid Interface Sci. (2021) 586:673–82. doi: 10.1016/j.jcis.2020.10.137
74. Faria CGF, Weiner L, Petrignet J, Hingray C, Santamaria ÁRDP, Villoutreix BO, et al. Antihistamine and cationic amphiphilic drugs, old molecules as new tools against the COVID-19? Med Hypotheses. (2021) 110508.
75. Day M. Covid-19: Ibuprofen Should Not Be Used for Managing Symptoms, Say Doctors and Scientists. London: British Medical Journal Publishing Group (2020).
77. McNamara T, Richt JA, Glickman L. A critical needs assessment for research in companion animals and livestock following the pandemic of COVID-19 in humans. Vector Borne Zoonotic Dis. (2020) 20:393–405. doi: 10.1089/vbz.2020.2650
Keywords: epidemiology, COVID-19, clinical characteristics, diagnosis, treatment, Pakistan
Citation: Ahmad M, Beg BM, Majeed A, Areej S, Riffat S, Rasheed MA, Mahmood S, Mushtaq RMZ and Hafeez MA (2021) Epidemiological and Clinical Characteristics of COVID-19: A Retrospective Multi-Center Study in Pakistan. Front. Public Health 9:644199. doi: 10.3389/fpubh.2021.644199
Received: 20 December 2020; Accepted: 15 March 2021;
Published: 14 April 2021.
Edited by:
Susan Christina Welburn, University of Edinburgh, United KingdomReviewed by:
Guoqing Qian, Ningbo First Hospital, ChinaSubhas Khajanchi, Presidency University, India
Muhammad Salman, University of Lahore, Pakistan
Copyright © 2021 Ahmad, Beg, Majeed, Areej, Riffat, Rasheed, Mahmood, Mushtaq and Hafeez. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mian Abdul Hafeez, abdul.hafeez@uvas.edu.pk
 Mehmood Ahmad
Mehmood Ahmad Bilal Mahmood Beg
Bilal Mahmood Beg Arfa Majeed
Arfa Majeed Sadaf Areej
Sadaf Areej Sualeha Riffat1
Sualeha Riffat1 Muhammad Adil Rasheed
Muhammad Adil Rasheed