- 1Department of Obstetrics and Gynecology, Nanjing Maternity and Child Health Care Hospital, Women's Hospital of Nanjing Medical University, Nanjing, China
- 2Department of Public Health, Nanjing Maternity and Child Health Care Hospital, Women's Hospital of Nanjing Medical University, Nanjing, China
- 3Department of Women Health Care, Nanjing Maternity and Child Health Care Hospital, Women's Hospital of Nanjing Medical University, Nanjing, China
Objective: Several studies have evaluated the association of cadmium exposure with the risk of gestational diabetes mellitus (GDM). However, the findings among these studies have been inconsistent. To further investigate the relationship, we carried out a meta-analysis to clarify the relationship between cadmium exposure and GDM risk.
Methods: Five databases (Scopus, PubMed, Web of Science, Cochrane, and CNKI) were searched for eligible studies until September 09, 2021. The quality of eligible studies was evaluated using the Newcastle–Ottawa quality assessment scale (NOS). The summary odds ratios (ORs) and 95% confidence intervals (CIs) were calculated by random-effects models due to high heterogeneity. Sensitivity analysis was performed to explore the robustness of the results. Publication bias was evaluated by Egger's test and Begg's test. We also conducted meta-regression analysis and subgroup analysis to assess the potential sources of heterogeneity.
Results: A total of 10 studies with 32,000 participants related to our issue were included. Comparing the highest vs. lowest categories of cadmium exposure, no significant association was observed between cadmium exposure and the risk of GDM (OR = 1.16, 95% CI = 0.92–1.46, and P = 0.206). No publication bias was found in Begg's and Egger's tests (all P > 0.05). Meta-regression suggested that publication year was the potentially heterogeneous source (P = 0.034). Subgroup analysis of publication year showed that the OR of studies before the year of 2016 was 4.05 (95% CI = 1.87–8.76, P < 0.001), and prospective cohort studies showed a borderline increased GDM risk (OR = 1.15, 95% CI = 0.99–1.33, and P = 0.061).
Conclusion: Our results indicated no significant association between cadmium exposure and GDM risk. Further high-quality prospective studies, especially those using standard analytic methods for cadmium exposure, are warranted to confirm the results.
Introduction
Gestational diabetes mellitus (GDM) is the initial occurrence of abnormal glucose tolerance during pregnancy and has a worldwide prevalence ranging from 1 to >30%, indicating that GDM is a relatively prevalent disease during pregnancy (1). The maternal and fetal consequences of GDM have been well-explored. The common complications of GDM include preeclampsia, polyhydramnios, operative delivery, shoulder dystocia, fetal overgrowth, neonatal hypoglycemia, jaundice, and perinatal mortality (2). Moreover, mothers and their offspring have a tendency to develop type 2 diabetes and obesity in the long term (3).
Epidemiological studies have confirmed a series of risk factors contributing to GDM, such as advanced maternal age, geography, ethnicity, and lifestyle factors. However, emerging risk factors, such as environmental pollutants and endocrine disruptors, have also attracted more attention (4, 5). As a result, it is vital to take emerging risk factors into account for the prevention and management of GDM. Cadmium, recognized as a toxic heavy metal distributed widely in our environment, has a large number of negative effects on humans. An unhealthy diet and tobacco smoking are the major sources of cadmium exposure in humans. Absorbed cadmium accumulates mainly in the kidneys and is ultimately excreted through the urine (6). The carcinogenicity and damage to the kidneys caused by cadmium have been reported in some studies (7, 8). Moreover, there is abundant evidence indicating a strong association between cadmium exposure and type 2 diabetes. The diabetogenic effect of cadmium may be involved in the dysfunction of insulin secretion from glucose-stimulated β-cells (9, 10).
Considering the increased risk of diabetes resulting from cadmium, we hypothesized that cadmium exposure may also increase the risk of GDM by similar mechanisms. Several studies found significant evidence to prove the relationship between cadmium and the risk of GDM. However, others found negative results, which may be due to differences in study populations, regions, sample types, and study methods. To explore the association more deeply, we conducted a meta-analysis to synthesize the data from existing studies and to analyze the likely relationship between cadmium and the risk of GDM.
Methods
Search Strategies
A systematic search for published studies that reported the relationship between cadmium and GDM risk was conducted using the following five databases from the date of database inceptions to September 09, 2021: Scopus, PubMed, Web of Science, Cochrane, and Chinese National Knowledge Infrastructure (CNKI). As for PubMed, the search was designed to seek articles that reported the effect of cadmium on GDM risk in English databases by combining MeSH terms and free-text terms: (((((((Diabetes, Gestational[MeSH Terms]) OR Diabetes, Pregnancy-Induced) OR Diabetes, Pregnancy Induced) OR Pregnancy-Induced Diabetes) OR Gestational Diabetes) OR Diabetes Mellitus, Gestational) OR Gestational Diabetes Mellitus) AND ((metals [MeSH Terms]) OR cadmium). In other English databases, the keywords used for the search were (((Gestational Diabetes) OR Pregnancy-Induced Diabetes) OR Gestational Diabetes Mellitus) AND (metals OR cadmium). Regarding the CNKI, we used the terms gestational diabetes mellitus, metals, and cadmium in Chinese and then combined the terms “gestational diabetes mellitus” and “metals or cadmium” to search for potential articles. The search strategy of each database is presented in Supplementary Figure 1.
Inclusion and Exclusion Criteria
The participants, interventions, comparison, outcomes, and study design (PICOS) strategy was used to guide our eligibility criteria (Supplementary Table 1). Studies were included if they reported the association between cadmium exposure and the risk of GDM. The criteria required for eligibility were as follows: (1) The diagnostic criteria of GDM were cautiously defined according to standard criteria; (2) proper and reasonable measurements were used to describe the cadmium concentrations in pregnant women; (3) cadmium exposures in pregnancy or prior to pregnancy were all considered; and (4) the odds ratios (ORs) or relative ratios (RRs) and 95% confidence intervals (CIs) or other statistics could be inverted into odds ratios and 95% CIs. The exclusion criteria were as follows: (1) duplicated reports; (2) animal studies, reviews, news, and abstracts; (3) ecological studies; (4) inadequate data or incorrect statistical analysis; and (5) articles that focused on diabetes rather than GDM.
Data Extraction and Quality Assessment
Two investigators independently extracted the following information regarding the eligible studies: (1) First author and timing of publication; (2) time period and location of the study; (3) study design; (4) sample type; (5) time of sample collection; (6) sample size; (7) diagnostic criteria for GDM; (8) concentration of cadmium; (9) covariates adjusted; and (10) OR/RR and 95% CI. The OR/RR and 95% CI were extracted from the adjusted models. When divergence occurred, the two investigators asked the mentor. Among the eligible studies, a study by Tomoko Oguri and his colleagues included nulliparous and parous women. As a result, we included them as two studies in our meta-analysis. Jia et al. used the prevalence ratios (PRs) to describe the risk. Based on the previous study (11), we also used the PRs. The quality of each study was assessed according to the Newcastle–Ottawa quality assessment scale (NOS) and divided into different grades based on their scores as follows: (1) a score ≤ 3 was regarded as low quality; (2) a score of 4–6 was regarded as intermediate quality; and (3) a score ≥ 7 was regarded as high quality.
Statistical Analysis
Heterogeneity among the eligible studies was measured by Cochran's Q-test and inconsistency index (I2). Pooled OR and 95% CI were calculated using the fixed-effects model if the heterogeneity test was not significant (P ≥ 0.05). Otherwise, the random-effects model was adopted. Sensitivity analyses were performed by excluding studies one after the other to estimate the stability of the pooled findings. Begg's and Egger's tests were performed to evaluate potential publication bias. Multivariate meta-regression analysis was applied to assess the possible sources of heterogeneity. Subgroup analysis was performed by publication year, geographic region, study design, diagnosis criteria, sample type, sample size, NOS score, and time of collection. All statistical analyses were two-sided and carried out by StataSE 12.0 (Stata Corp LP, College Station, Texas, USA). P < 0.05 indicated statistical significance.
Results
Search Results and Study Characteristics
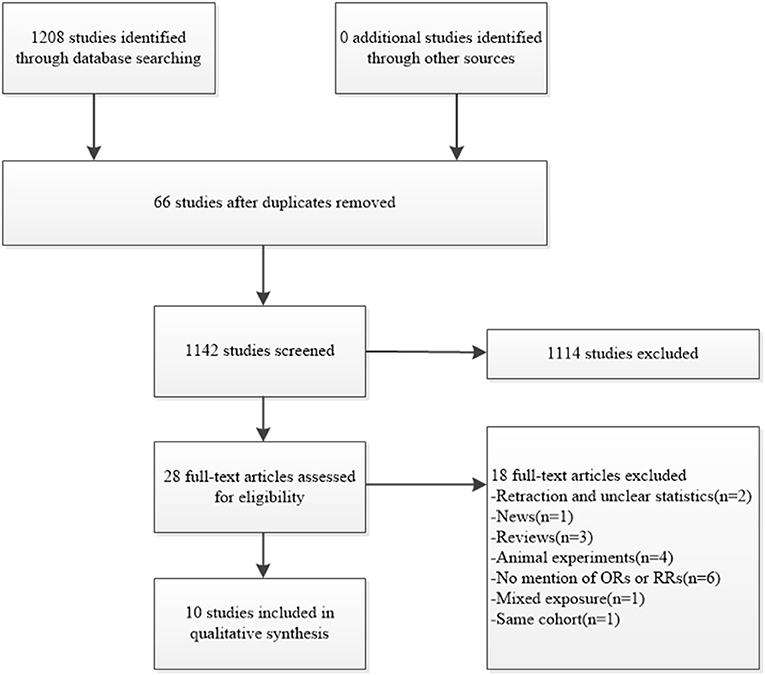
After searching the mentioned databases, 1,208 articles were identified as eligible in total, and 66 were excluded after finding duplicates. A total of 1,142 articles were then further screened, and 1,114 were excluded for different reasons, such as unrelated context, meeting abstract, or animal studies. The full texts of the remaining 28 articles were screened further. Among them, 1 news article, 1 retraction, 3 reviews, and 4 animal experiments were excluded. A total of 6 studies did not mention the ORs or RRs, and 1 study focused on mixed exposure. One study was then excluded for unclear statistics (12). We also attempted to send an e-mail to the author for data clarification but received no reply. Another two studies were from the same cohort, and we therefore chose the most recent one (13). Finally, we included the remaining 10 studies in the meta-analysis on the connection between cadmium exposure and the risk of GDM (Figure 1). Some studies focusing on this issue have found significant evidence to prove the relationship between cadmium and the risk of GDM (14–17), while others have found negative results (13, 18–22).
Among the 10 studies, six were cohort studies, while four were case-control studies. Seven studies were conducted in China, one in the USA, one in Japan, and one in Canada. Five of them measured the concentrations of cadmium in urine samples, three in blood samples, one in meconium samples, and one in hair samples. The quality scores of all the included studies ranged from 7 to 9 and were regarded as high quality. The eligible studies were published from 2015 to 2021, and 32,000 pregnant women were enrolled in total. The characteristics and NOS scores of the 10 studies are described in Table 1.
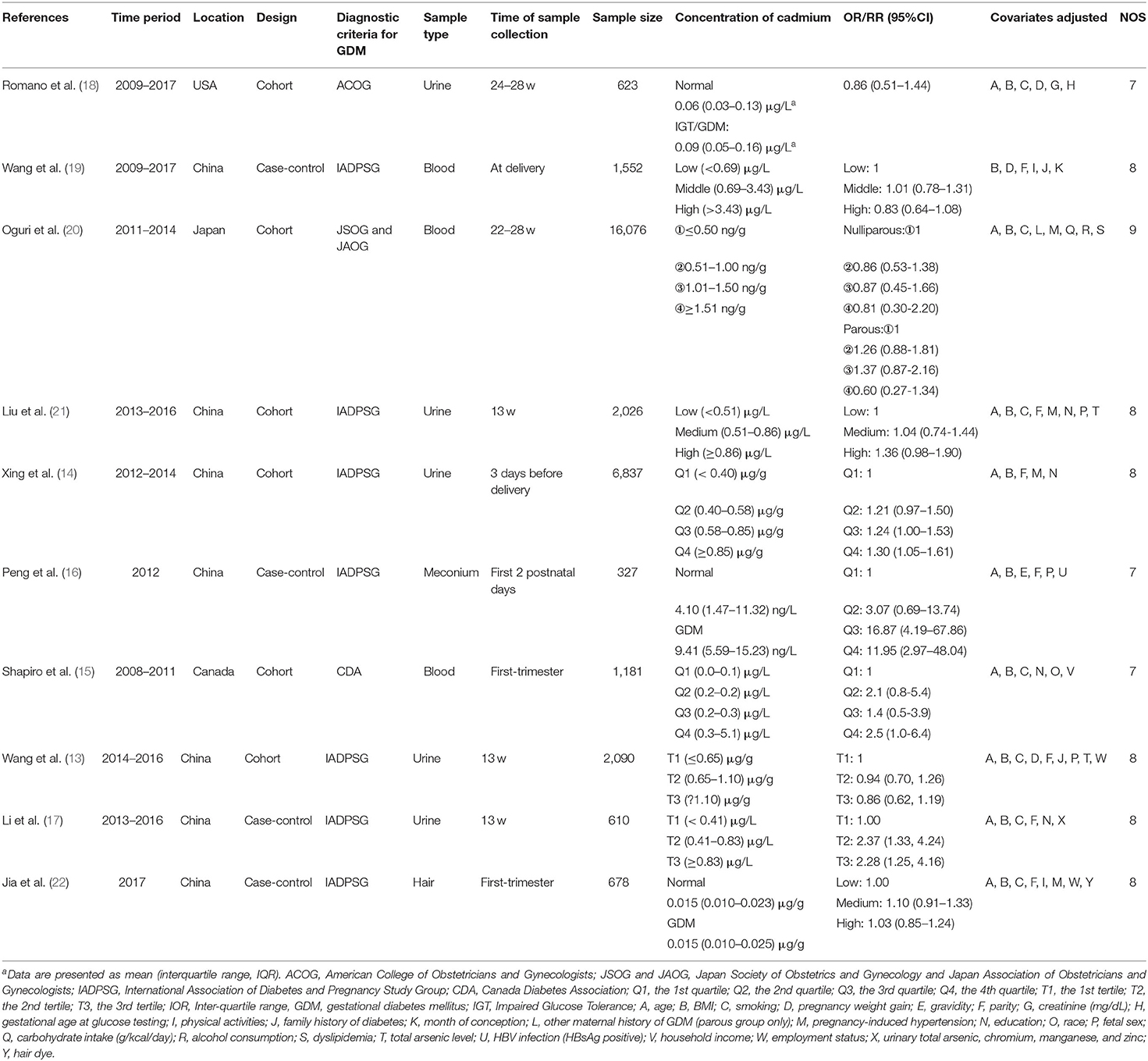
Table 1. Characteristics of eligible studies investigating the association between cadmium exposure and gestational diabetes mellitus.
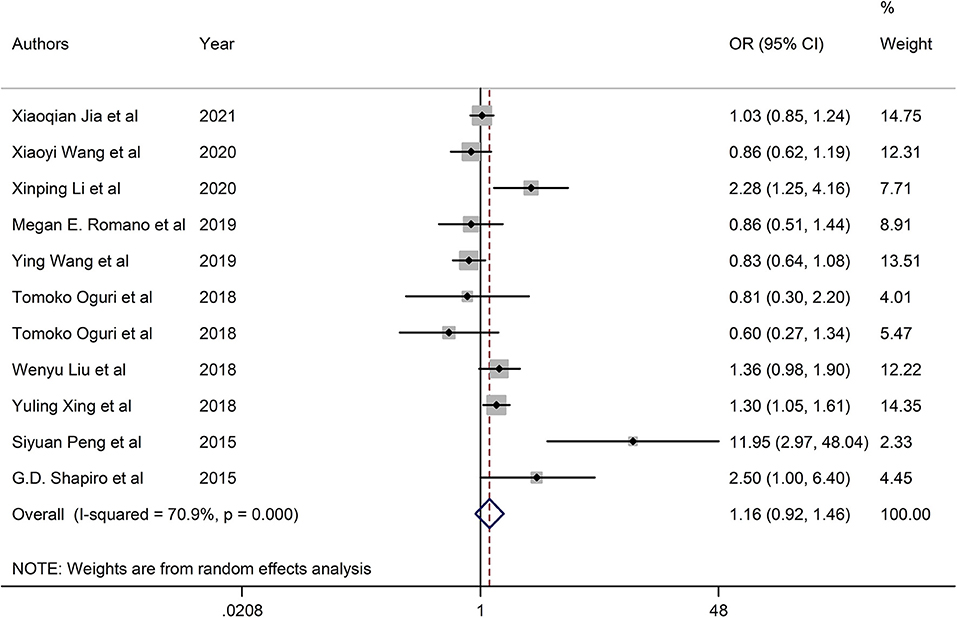
Combined Effect Evaluation
The pooled OR of cadmium exposure was 1.16 (95% CI = 0.92, 1.46) in the random-effects model due to the high heterogeneity, revealing that cadmium exposure had no significant association with the increased risk of GDM (Figure 2).
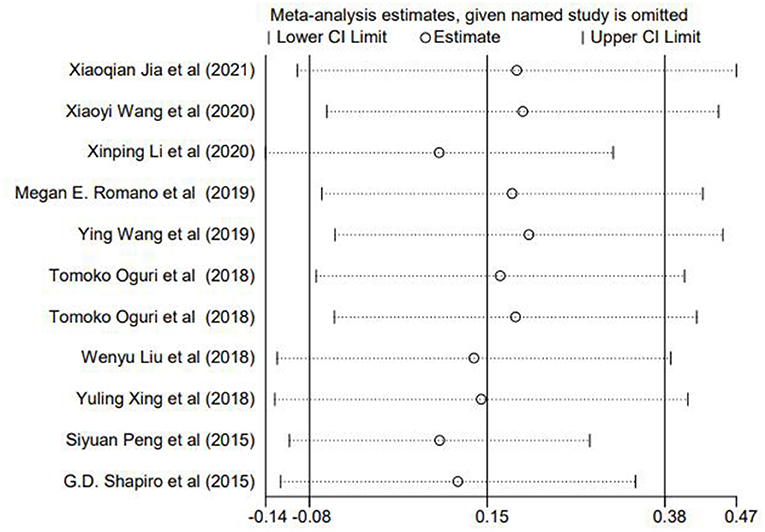
Sensitivity Analyses and Publication Bias
To evaluate whether the findings was changed by excluding each study, a sensitivity analysis was performed. As shown in Figure 3, no single study had a significant effect on the summary ORs, thereby supporting the stableness of our results.
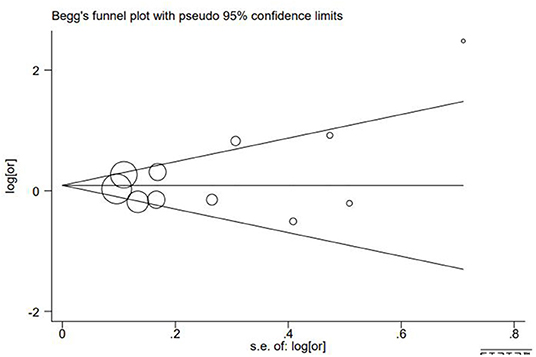
Egger's test and Begg's test were used to calculate the publication bias of these studies. We found no publication bias according to the results (PEgger = 0.316, PBegg = 0.213, Figure 4).
Meta-Regression Analysis and Subgroup Analysis
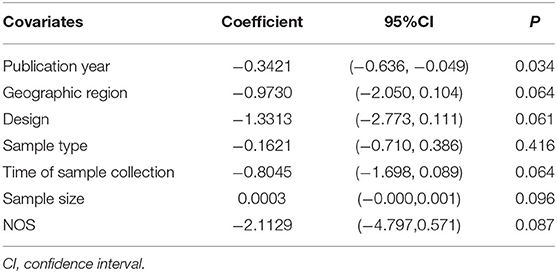
We performed meta-regression analysis to assess the sources of heterogeneity, including publication year, geographic region, design, sample type, time of sample collection, sample size, and NOS score. As shown in Table 2, publication year contributed to the high heterogeneity (P = 0.034). However, the source of heterogeneity was not observed among other factors (all P > 0.05).
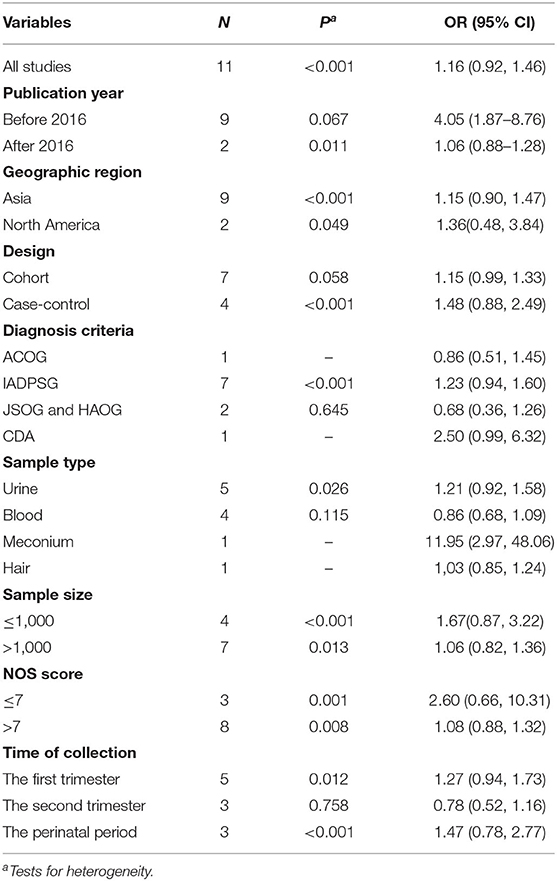
In subgroup analysis, when stratified by publication year, the summary OR of nine studies with publication year before 2016 was 4.05 (95% CI = 1.87–8.76, P < 0.001). When stratified by study design, we found a borderline increased risk of gestational diabetes due to cadmium exposure in cohort studies (OR = 1.15, 95% CI = 0.99–1.33, P = 0.061). Subgroup analyses by geographic region, diagnosis criteria, sample type, sample size, NOS score, and time of collection were not statistically significant (all P > 0.05, Table 3).
Discussion
Overall, our manuscript shows no statistically significant association between cadmium exposure and the risk of GDM. However, the negative results should be interpreted with caution for several reasons.
In subgroup analyses, we observed a borderline increased risk of disease in cohort studies. Cohort studies are conducted to determine the causal association between initial participant exposure characteristics and diseases, while case-control studies can only prove the potential relationship between exposure characteristics and diseases. Cohort studies have several strengths when compared with case-control studies, such as a large number of participants and relatively complete data. Moreover, studies enrolling <1,000 participants are more than 50% in our meta-analysis. Meta-analyses may be inaccurate because of the smaller size of the included studies and the low number of participants, which may result in more random errors (23). Several studies have studied the role of cadmium exposure in the development of GDM at present, which has led to an insufficient number of included studies in our meta-analysis. At last, the result of meta-regression showed that the time of publication contributed to the high heterogeneity. The methods of detecting cadmium are becoming more and more accurate and multiple, and the design may be more reasonable according to the previous studies. Notably, the measurements and samples for cadmium exposure were variable among these included studies. Debate still remains as to which type of sample reflects the cadmium burden. Different samples can be used to reflect the chemical exposure of a particular pregnancy time period. Additionally, it is crucial to consider all available analytes to determine the actual cadmium burden of the body during pregnancy (24). All studies selected in our meta-analysis adopted only one type of sample to measure the cadmium burden of pregnant women, which may not correctly reflect the total body burden of cadmium. As a result, the association between cadmium exposure and the risk of GDM may have been influenced by different or even improper measurements. We also conducted subgroup analyses according to the different processes of pregnancy due to the pathophysiology of GDM. It has been proven that there is decreased insulin sensitivity before conception in pregnant women with GDM, which further decreases during pregnancy (25, 26). This means that potential changes in the pathophysiology of GDM may appear earlier than the first trimester of pregnancy. Although the development of GDM results from changes in pathophysiology during the full process of pregnancy, changes in early life are still more important. However, all the included studies in our meta-analysis evaluated cadmium exposure after conception. Five studies measured the cadmium burden in the first trimester, three in the second trimester, and three in the perinatal period, and no statistically significant association was found.
In addition, some emerging factors are associated with GDM, such as fetal sex and toxic metals including arsenic and antimony (27, 28). As mentioned in the study done by Liu, women carrying male fetuses tend to develop insulin resistance when compared with those carrying female fetuses. Additionally, unknown or unmeasured co-exposures also exist in our environment, which could result in an increased risk of GDM. Although, the studies took the possible confounding factors related to GDM into consideration, these limitations possibly affected the results of our meta-analysis. Nevertheless, not all included studies evaluated the risk with models adjusted by exposure to other metals. Moreover, the adjusted confounding factors were variable among these studies. Multiple factors were verified to be connected with GDM, such as BMI, smoking, family history of diabetes, and alcohol consumption.
Although, we found no statistically significant association between cadmium exposure and GDM, it is still possible that cadmium plays an important role in the development of GDM. Cadmium exposure has been linked to inflammation and oxidative stress, and it up-regulates the expression of tumor necrosis factor (TNF) and different chemokines in various cell types (10). TNF activates a signaling pathway that increases the levels of sphingomyelinase and ceramides, which disrupt the insulin signaling pathway (29). The potential effect of cadmium on type 2 diabetes has been shown in several studies. Some experiments found that cadmium exposure can destroy the function of β-cells and cause insulin resistance (9). However, the role of cadmium exposure in GDM remains unclear. Moreover, we performed this analysis by using the highest vs. the lowest exposure group rather than the continuous exposure group. Therefore, the concentrations of cadmium were variable among these studies, and participants in studies with high concentrations of cadmium seemed to have a higher risk of GDM. As a result, other studies with relatively lower levels of cadmium could have obtained negative effects. Prospectively, more epidemiological proof and experimental efforts are urgently needed.
Our meta-analysis has several strengths. First, our meta-analysis is the first to explore the relationship between the risk of GDM and cadmium exposure. Second, the included studies were limited to English papers and Chinese papers, the latter of which could be more objective and representative for elaborating the potential effect of cadmium on GDM. Third, sub-analyses were conducted to further explore the associations and determine the source of heterogeneity, and the null results may have been due to the limited number of participants. Nevertheless, our study has several limitations. The small sample size may have resulted in random errors in our meta-analysis due to the relatively less attention given to GDM and cadmium exposure. Three studies had NOS scores ≤ 7, indicating potential defects in methods or study design, which may have affected the accuracy of our meta-analysis. Third, the accuracy of the analysis was affected by the high heterogeneity and inconsistent adjusted confounding factors.
Conclusion
In conclusion, we found no statistically significant association between cadmium exposure and the risk of GDM. More studies with larger sample sizes and detailed experiments should be conducted to further explore the associations and identify the role of cadmium exposure in the mechanism of GDM.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
YL and KX designed the study. YL and TL searched for and evaluate the included studies. ZS and KX contributed to the funding acquisition and manuscript editing. YL and JX wrote the manuscript. KX analyzed data. All authors contributed to the article and approved the submitted version.
Funding
This research was supported by the National Natural Science Foundation of China (81971410 and 81571458), Postdoctoral Research Funding Program of Jiangsu Province (2020Z146), and State Key Laboratory of Reproductive Medicine (SKLRM-UC201901 and SKLRM-UC201902).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.555539/full#supplementary-material
References
1. McIntyre HD, Catalano P, Zhang C, Desoye G, Mathiesen ER, Damm P. Gestational diabetes mellitus. Nat Rev Dis Primers. (2019) 5:47. doi: 10.1038/s41572-019-0098-8
2. Casey BM, Lucas MJ, McIntire DD, Leveno KJ. Pregnancy outcomes in women with gestational diabetes compared with the general obstetric population. Obstetr Gynecol. (1997) 90:869–73. doi: 10.1016/S0029-7844(97)00542-5
3. Chiefari E, Arcidiacono B, Foti D, Brunetti A. Gestational diabetes mellitus: an updated overview. J Endocrinol Invest. (2017) 40:899–909. doi: 10.1007/s40618-016-0607-5
4. Smarr MM, Grantz KL, Zhang C, Sundaram R, Maisog JM, Barr DB, et al. Persistent organic pollutants and pregnancy complications. Sci Total Environ. (2016) 551–2:285–91. doi: 10.1016/j.scitotenv.2016.02.030
5. Zhang C, Sundaram R, Maisog J, Calafat AM, Barr DB, Buck Louis GM. A prospective study of prepregnancy serum concentrations of perfluorochemicals and the risk of gestational diabetes. Fertil Steril. (2015) 103:184–9. doi: 10.1016/j.fertnstert.2014.10.001
6. Amzal B, Julin B, Vahter M, Wolk A, Johanson G, Akesson A. Population toxicokinetic modeling of cadmium for health risk assessment. Environ Health Perspect. (2009) 117:1293–301. doi: 10.1289/ehp.0800317
7. Lin X, Peng L, Xu X, Chen Y, Zhang Y, Huo X. Connecting gastrointestinal cancer risk to cadmium and lead exposure in the Chaoshan population of Southeast China. Environ Sci Pollut Res Int. (2018) 25:17611–9. doi: 10.1007/s11356-018-1914-5
8. Liu Q, Zhang R, Wang X, Shen X, Wang P, Sun N, et al. Effects of sub-chronic, low-dose cadmium exposure on kidney damage and potential mechanisms. Ann Transl Med. (2019) 7:177. doi: 10.21037/atm.2019.03.66
9. Dover EN, Patel NY, Stýblo M. Impact of in vitro heavy metal exposure on pancreatic β-cell function. Toxicol Lett. (2018) 299:137–44. doi: 10.1016/j.toxlet.2018.09.015
10. Tinkov AA, Filippini T, Ajsuvakova OP, Aaseth J, Gluhcheva YG, Ivanova JM, et al. The role of cadmium in obesity and diabetes. Sci Total Environ. (2017) 601–2:741–55. doi: 10.1016/j.scitotenv.2017.05.224
11. Li W, Xu B, Cao Y, Shao Y, Wu W, Zhou J, et al. Association of maternal folate intake during pregnancy with infant asthma risk. Sci Rep. (2019) 9:8347. doi: 10.1038/s41598-019-44794-z
12. Soomro MH, Baiz N, Huel G, Yazbeck C, Botton J, Heude B, et al. Exposure to heavy metals during pregnancy related to gestational diabetes mellitus in diabetes-free mothers. Sci Total Environ. (2019) 656:870–6. doi: 10.1016/j.scitotenv.2018.11.422
13. Wang X, Gao D, Zhang G, Zhang X, Li Q, Gao Q, et al. Exposure to multiple metals in early pregnancy and gestational diabetes mellitus: a prospective cohort study. Environ Int. (2020) 135:105370. doi: 10.1016/j.envint.2019.105370
14. Xing Y, Xia W, Zhang B, Zhou A, Huang Z, Zhang H, et al. Relation between cadmium exposure and gestational diabetes mellitus. Environ Int. (2018) 113:300–5. doi: 10.1016/j.envint.2018.01.001
15. Shapiro GD, Dodds L, Arbuckle TE, Ashley-Martin J, Fraser W, Fisher M, et al. Exposure to phthalates, bisphenol A and metals in pregnancy and the association with impaired glucose tolerance and gestational diabetes mellitus: the MIREC study. Environ Int. (2015) 83:63–71. doi: 10.1016/j.envint.2015.05.016
16. Peng S, Liu L, Zhang X, Heinrich J, Zhang J, Schramm KW, et al. A nested case-control study indicating heavy metal residues in meconium associate with maternal gestational diabetes mellitus risk. Environ Health. (2015) 14:19. doi: 10.1186/s12940-015-0004-0
17. Li X, Huang Y, Xing Y, Hu C, Zhang W, Tang Y, et al. Association of urinary cadmium, circulating fatty acids, and risk of gestational diabetes mellitus: a nested case-control study in China. Environ Int. (2020) 137:105527. doi: 10.1016/j.envint.2020.105527
18. Romano ME, Gallagher LG, Jackson BP, Baker E, Karagas MR. Maternal urinary cadmium, glucose intolerance and gestational diabetes in the New Hampshire Birth Cohort Study. Environ Res. (2019) 179(Pt A):108733. doi: 10.1016/j.envres.2019.108733
19. Wang Y, Zhang P, Chen X, Wu W, Feng Y, Yang H, et al. Multiple metal concentrations and gestational diabetes mellitus in Taiyuan, China. Chemosphere. (2019) 237:124412. doi: 10.1016/j.chemosphere.2019.124412
20. Oguri T, Ebara T, Nakayama SF, Sugiura-Ogasawara M, Kamijima M. Association between maternal blood cadmium and lead concentrations and gestational diabetes mellitus in the Japan Environment and Children's Study. Int Arch Occup Environ Health. (2019) 92:209–17. doi: 10.1007/s00420-018-1367-7
21. Liu W, Zhang B, Huang Z, Pan X, Chen X, Hu C, et al. Cadmium body burden and gestational diabetes mellitus: a prospective study. Environ Health Perspect. (2018) 126:027006. doi: 10.1289/EHP2716
22. Jia X, Zhang L, Zhao J, Ren M, Li Z, Wang J, et al. Associations between endocrine-disrupting heavy metals in maternal hair and gestational diabetes mellitus: a nested case-control study in China. Environ Int. (2021) 157:106770. doi: 10.1016/j.envint.2021.106770
23. Wetterslev J, Thorlund K, Brok J, Gluud C. Trial sequential analysis may establish when firm evidence is reached in cumulative meta-analysis. J Clin Epidemiol. (2008) 61:64–75. doi: 10.1016/j.jclinepi.2007.03.013
24. Barr DB, Wang RY, Needham LL. Biologic monitoring of exposure to environmental chemicals throughout the life stages: requirements and issues for consideration for the National Children's Study. Environ Health Perspect. (2005) 113:1083–91. doi: 10.1289/ehp.7617
25. Catalano PM, Huston L, Amini SB, Kalhan SC. Longitudinal changes in glucose metabolism during pregnancy in obese women with normal glucose tolerance and gestational diabetes mellitus. Am J Obstetr Gynecol. (1999) 180:903–16. doi: 10.1016/S0002-9378(99)70662-9
26. DeFronzo RA, Ferrannini E, Groop L, Henry RR, Herman WH, Holst JJ, et al. Type 2 diabetes mellitus. Nat Rev Dis Primers. (2015) 1:15019. doi: 10.1038/nrdp.2015.19
27. Ashley-Martin J, Dodds L, Arbuckle TE, Bouchard MF, Shapiro GD, Fisher M, et al. Association between maternal urinary speciated arsenic concentrations and gestational diabetes in a cohort of Canadian women. Environ Int. (2018) 121(Pt 1):714–20. doi: 10.1016/j.envint.2018.10.008
28. Zhang Q, Li X, Liu X, Dong M, Xiao J, Wang J, et al. Association between maternal antimony exposure and risk of gestational diabetes mellitus: a birth cohort study. Chemosphere. (2020) 246:125732. doi: 10.1016/j.chemosphere.2019.125732
Keywords: cadmium, gestational diabetes mellitus, meta-analysis, metal, systematic review
Citation: Lin Y, Li T, Xiao J, Xie K and Shi Z (2022) The Association Between Cadmium Exposure and Gestational Diabetes Mellitus: A Systematic Review and Meta-Analysis. Front. Public Health 9:555539. doi: 10.3389/fpubh.2021.555539
Received: 01 May 2020; Accepted: 28 December 2021;
Published: 10 February 2022.
Edited by:
Wei Bao, The University of Iowa, United StatesReviewed by:
Shohreh F. Farzan, University of Southern California, United StatesArman Arab, Isfahan University of Medical Sciences, Iran
Copyright © 2022 Lin, Li, Xiao, Xie and Shi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kaipeng Xie, kaipengxie@njmu.edu.cn; Zhonghua Shi, jesse_1982@163.com
 Yu Lin
Yu Lin Ting Li
Ting Li Jiangbo Xiao
Jiangbo Xiao Kaipeng Xie
Kaipeng Xie Zhonghua Shi
Zhonghua Shi