- 1Department of Family Medicine, International School of Medicine, Bishkek, Kyrgyzstan
- 2Department of Public Health, International School of Medicine, Bishkek, Kyrgyzstan
- 3Department of Public Health and Clinical Medicine, Umeå University, Umeå, Sweden
- 4Institute of Family Medicine and Public Health, University of Tartu, Tartu, Estonia
- 5Department of Psychology, Umeå University, Umeå, Sweden
- 6Institute of Social Studies, University of Tartu, Tartu, Estonia
The purpose of this study was to characterize different ethnic groups in Kyrgyzstan regarding cardiovascular disease (CVD) and mental distress, and to investigate the association between CVD and mental distress. The mental distress was measured in terms of sleep disturbance, burnout, and stress.
Materials and Methods: A cross-sectional study was carried out among six ethnic groups in Kyrgyzstan, aged 18 years and above. The sample was stratified for age, education, family status, and income. We used the Karolinska Sleep Questionnaire to assess sleep disturbance, the physical and emotional subscale of the Shirom Melamed Burnout Questionnaire to assess burnout, and the 10-item Perceived Stress Scale to assess perceived stress.
Results: The distribution of CVD differed significantly between the six ethnic groups, with higher prevalence among East Europeans, and Western Asians and lower among Other minorities and Central Asians. In all ethnic groups in Kyrgyzstan, individuals with CVD had increased odds of sleep disturbance and burnout. There was a significant difference in burnout and stress between persons with and without CVD in Kyrgyz and East European ethnic groups.
Conclusion: There was a significant difference in burnout and stress between persons with and without CVD in Kyrgyz and East European ethnic groups. In addition to CVD prevention, mitigating sleep disturbance and preventing burnout in the general population should be aimed at in public health measures.
Introduction
Cardiovascular diseases (CVDs) are the worldwide leading cause of mortality (1, 2). Globally, the highest CVD mortality rates are found in Ukraine, Russia, and Central-Asia (63, 55, 63–42% in 2016, respectively) (3). Those post-Soviet countries like Kyrgyzstan [with a population of 6.3 million in 2018 (4)] have experienced volatile economic and political transitions that make up challenging socioeconomic conditions for health and well-being in the multi-ethnic population.
The main risk factors for CVD include physical inactivity, obesity, unhealthy diet, smoking, drug abuse, hypertension, and lipid abnormalities (5–11). Prior studies have shown lower CVD mortality attributable to dietary risk in Kyrgyzstan and among Central Asians (Kazakhs, Tajiks, and Kyrgyzs) compared to East Europeans (Russians, Ukranians, and Belorussians) and Western Asians (Georgians, Azerbaijani) (12). There are also gender differences as women have lower incidence levels and develop the disease later than men (13, 14). Their protective mechanisms against CVD are mainly associated with sex hormone (e.g., estrogen) levels as the incidence and severity of CVD increase in women during post-menopause period (15). At the same time, gender behavioral differences may play an important role. As women visit physicians more often, their diseases are registered more frequently, whereas men may not visit a physician until it may be too late (16).
Apart from those, various social factors may contribute to differences in CVD incidence. Individuals with low socioeconomic status experience higher rates of CVD burden and mortality (17–21). Low level of educational attainment is associated with high prevalence of cardiovascular risk factors, high CVD incidence, and CVD mortality (19, 22). In Kyrgyzstan, in 2017, the Gini coefficient, that is a measure of inequality among levels of income, was 26.8 (23). This reflects relatively good equality in income distribution since the country residents have a similar relatively low standard of living.
It has been indicated that socioeconomic inequalities are more prevalent among minority ethnic populations who have high prevalence of CVD and related risk factors (24), and this inequality is growing globally (25–28). Ethnic minorities also experience more barriers to access a CVD diagnosis (29), poorer recording of clinical data (30), receive lower quality of health care, and have poorer health outcomes (31). Carson and colleagues showed that ethnicity is an important predictor of hypertension (32). Kontsevaya et al. found that among Kyrgyz women, arterial hypertension prevalence was significantly lower than in their Russian peers (36.8 vs. 46.2%, respectively) (33). At the same time, among Kazakh and Kyrgyz men, systolic blood pressure was significantly higher than in Russians (33).
It is well-documented that social factors may moderate stress level (34). Chronic psychological stress is associated with a greater risk of depression, autoimmune diseases, respiratory infections as well as coronary heart disease (35, 36). Stress as a complaint is related to anxiety (37) and depression (38). Psychosocial factors such as depression and low social support are in turn established risk factors for heart disease (36, 39) and have been associated with high risk of adverse cardiovascular outcomes (35, 40–44), and mortality among patients with CVD (45, 46). Mental distress is associated to social factors (poverty and unemployment), ethnicity, gender, age, and disability (47, 48).
Stress may perpetuate sleep disturbance, as complaints in burnout (49) and symptoms of insomnia (50), may lead to poor sleep, worry, and increase of blood pressure (51, 52). Whereas, stress fluctuates strongly since it is a necessity in daily life in coping with everyday hassles, chronic stress that results in burnout may be a particular risk factor for chronic diseases (53, 54). Sleep disturbance is both an initiator and a consequence of burnout and depression (51, 55–57). As the result of long-term inflammatory processes due to mental distress, plaque formation on the vascular walls in atherosclerosis may eventually lead to a CVD event (58–60). The fact that stress also underlies burnout and sleep disturbance, highlights the importance of these conditions on persons with CVD.
The current study aimed at characterizing different ethnic groups in Kyrgyzstan with respect to CVD and the mental distress conditions including sleep disturbance, burnout, and stress, and to investigate the association between CVD and mental distress. Based on earlier evidence, we infer that some ethnic groups are more likely than other to contract CVD. The present study tested the hypotheses of the minorities, compared to dominant Kyrgyz ethnic group, being more likely to suffer from CVD and/or having higher levels of mental distress. Following Mezick et al. (61), Grandner et al. (62), Slopen et al. (63), and Johnson et al. (64), we expected ethnic-group differences also in sleep disturbance.
Materials and Methods
Data Collection
A sample of 694 individuals aged 18 years and older visiting polyclinics (Centers of Family Medicine) and health care centers were invited to participate in a study entitled “Health status of ethnic minorities in Kyrgyzstan.” We chose five polyclinics in the suburban areas, where representatives of minorities mainly reside in Bishkek. Kyrgyzs as a control group were recruited from the same facilities. We used a questionnaire with 47 questions to explore the health status, behavioral and psychological determinants and prevalence of CVD, body mass index (BMI), age, gender, education level, ethnicity, and income. Informed consent was obtained from participants after explaining the study aims, voluntariness of participation, and anonymised data processing. The respondents answered the questionnaire and could ask for assistance or explanations from the study leader.
The initial sample included 1,200 participants. With a response rate of 57.8%, this resulted in 694 respondents. We used random sampling stratified for ethnicity, age, education, and gender. Ethnicity was asked as open question: “Please, indicate your ethnicity:…” [see also Phinney and Ong (65)]. In Kyrgyzstan, the Kyrgyz comprise 73.3% of the population. Other major ethnic groups include Russians (5.6%) concentrated in the north, and Uzbeks (14.7%) living in the south. Small, but noticeable minorities include Dungans (1.1%), Uyghurs (0.9%), Tajiks (0.9%), Kazakhs (0.6%), and Koreans (0.3%). Other small ethnic minorities make up 2.6% of the population (4). Following this, the participants were divided into six groups based on their ethnicity. Kyrgyz people, (1) “Kyrgyz,” functioned as a control group for comparison with the other ethnic groups. Due to their similarity in religious background and geographical origins we grouped five additional ethnic groups as follows: (2) “East Europeans”: Russian, Byelorussian, and Ukrainian; (3) “Central Asians”: Uzbek, Kazakh, Tatar; (4) “East Asians”: Korean; (5) “Western Asians”: Georgian, Armenian, Turk, and Azerbaijan; and (6) “Other minorities”: Dungan and Uyghur. In the initial sample of 1,200 participants, we aimed at ethnic group proportions of 40% Kyrgyz, 20% East Europeans, 20% Central Asians, 5% East Asians, 5% Western Asians, and 10% Other minorities. The final sample of respondents consisted of 31.3% Kyrgyz, 34.4% East Europeans, 16.4% Central Asians, 5.5% East Asians, 3.3% Western Asians, and 9.1% Other minorities. Regarding age groups, we aimed at equal proportions of age groups, resulting in 24.9% aged 18-29, 24.4% aged 30-39, 17.3% aged 40-49, 17.3% aged 50-59, and 16.1% aged ≥ 60 years. Regarding education, we aimed at the proportions 26% with higher education, 68% with high school education, and 5% with elementary or secondary school. In the final sample, higher education was overrepresented, 41%, and the proportions were 57.2% with high school education, and 1.6% with elementary education. In the final sample male sex are slightly under-represented (43.5%).
The 694 respondents were distributed across the ethnic groups: Kyrgyzs (control, 217 individuals, mean age = 39.2 ± 14.8), East Europeans (239 individuals, mean age = 48.5 ± 15.7), East Asians (38 individuals, mean age = 43.4 ± 20.6), Central Asians (114 individuals, mean age = 38.1 ± 14.7), Western Asians (23 individuals, mean age = 43.2 ± 13.3), and Other Minorities (63 individuals, mean age = 34.3 ± 14.3).
Questionnaire Instruments
The questionnaire used was in the Russian language. Socio-demographic variables were assessed following the Guidelines for Handling the Harmonized Questionnaire (66), and anthropometric data (e.g., height and weight) were assessed according to the WHO recommendations (67). We used the question “Do you have any CVD diagnosed by a doctor” to determine any diagnosed CVD, coded as “Any CVD.” We grouped individuals according to their educational background (1 = Primary; 2 = Secondary High school, incomplete higher education, or vocational school; and 3 = University degree). Individuals were grouped according to their BMI (weight in kilograms divided by the square of height in meters) as follows: BMI <25 kg/m2 as (1) reference; BMI ≥ 25 kg/m2 as (2) individuals with higher risk (68).
The Karolinska Sleep Questionnaire (KSQ) was used to assess sleep disturbance (69). The questions were: “Have you been bothered by the following complaints during the past three months”: “… difficulties falling asleep,” “… repeated awakenings with difficulties falling asleep again,” “… premature awakenings involuntary,” and “… disturbed/restless sleep.” The response options throughout the KSQ are (0) never, (1) seldom (occasionally), (2) sometimes (several times per month), (3) often, (4) most of the times, or (5) always. The score can range from 0 to 20 (high score representing high level of sleep disturbance). The KSQ has good reliability, construct validity, and criterion validity (69). The internal consistency in the current study was good (Cronbach's Alfa 0.868). For further analysis, the participants were divided into groups that as far as possible constituted the first to third and the fourth quartile: 82.7% individuals with score 0-8 (“less sleep problems”); and the rest with score 9 or higher (“much sleep problems”).
The physical and emotional subscale of the Shirom Melamed Burnout Questionnaire was used to measure burnout (70, 71). The subscale consists of eight items (“I feel tired,” “I feel refreshed,” “I feel physically exhausted,” “I feel fed-up,” “My batteries" are “dead", “I feel burned out,” “I feel mentally fatigued,” “I feel no energy for going to work in the morning”). The response scale ranges from 1—“almost never” to 7—“Almost always.” The score can thus range between 7 and 56 (high score representing high level of burnout). The SMBQ has good construct validity and reliability (72). The internal consistency in the current study was good (Cronbach's Alfa 0.848). For further analysis, we divided individuals into two groups according to quartiles: 76.5% individuals with score 8-25 as “low burnout”; and the remaining with score 26 or higher as “high burnout.”
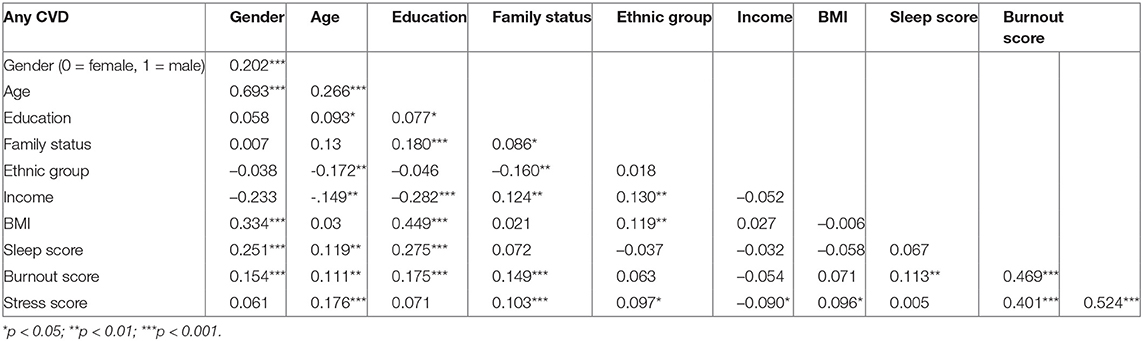
The 10-item Perceived Stress Scale (PSS-10) was used to measure degree to which situations are appraised as stressful (73). The items assess how unpredictable, uncontrollable, and overloaded the respondents find their lives (“… been upset because of something that happened unexpectedly?” “…felt that you were unable to control the important things in your life?”, “…felt nervous and stressed?”, “…felt confident about your ability to handle your personal problems?”, “…felt that things were going your way?”, “…felt that you could not cope with all the things that you had to do?”, “…felt you been able to control irritations in your life?”, “…felt that you were on top of things?”, “.how often have you been angered because of things that happened that were outside of your control?”, “how often have you felt difficulties were piling up so high that you could not overcome them?”). The score can range from 0 to 40 (high score representing high stress level). The PSS-10 has good construct validity (74). The internal consistency in the current study was good (Cronbach's Alfa 0.901). For further analysis, we divided individuals into two groups according to quartiles: 75.6% individuals with score 0-21 (“low stress”); and the rest with score 22 or higher (“high stress”). Mean scores for all “mental distress factors” (sleep disturbance, burnout, perceived stress) were calculated (see Table 1).
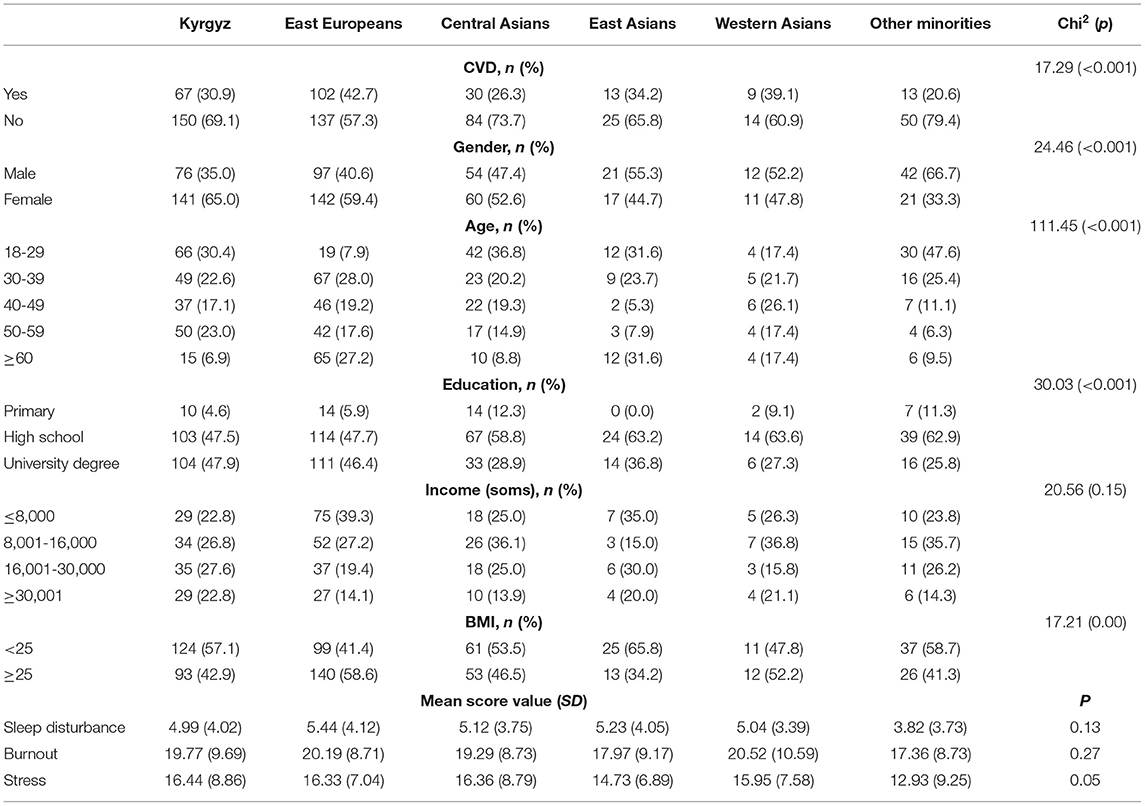
Table 1. Prevalence of cardiovascular disease (CVD), socio-demographic outcomes, and mental distress factor in various ethnic groups.
Statistical Analysis
The statistical analysis was performed using the IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp. Differences between ethnic groups in prevalence of CVD, socio-demographic outcomes and mental distress factor were tested with Chi-Square Test, T-Test, and post-hoc Bonferroni Test. Analyses of covariance (ANCOVAs) were conducted to study the associations between prevalence of CVD and levels of sleep disturbance, burnout, and stress. The odds for having CVD in relation to level of sleep disturbance, burnout, and stress in the various ethnic groups, with the Kyrgyz as referents, were assessed with logistic regression analysis, where also gender and BMI were considered. Confounding variables were only included in the analyses if they correlated with the analyzed variables according to Spearman correlation analysis. Since age was highly correlated with CVD (0.693, see Appendix 1), we removed age from further calculations. Due to multicollinearity, the independent variables with a high bivariate correlation should not be included in multiple regression analysis (75). The α-level was set at 0.05.
Ethical Concerns
Ethical approval was received from the Research Ethics Committee of the International School of Medicine, Kyrgyzstan (Ref #10, 28.06. 2017). All study participants gave written informed consent in accordance with the Declaration of Helsinki.
Results
There were significant differences in the distribution of CVD (χ2 = 17.29 at DF = 1, p < 0.001) and socio-demographic outcomes between the ethnic groups (Table 1). According to post-hoc tests, compared to Kyrgyz people (30.9%), the prevalence was significantly higher (p < 0.05) among East Europeans (42.7%), Western Asians (39.1%), and lower among Central Asians (26.3%) and other minorities (20.6%), in this study. Having high BMI (≥25) was more common among East Europeans and Western Asians. Among the mental distress factors, stress level showed a clear tendency to differ significantly (p = 0.05) between ethnic groups, whereas levels of sleep disturbance and burnout did not (Table 1). Post-hoc Bonferroni tests showed that East Asians and Other minorities had significantly lower prevalence of high stress than the Kyrgyz (p < 0.05). The results from the Spearman correlation analyses are given in Appendix 1, showing ethnic group, gender and BMI as confounding variables.
We explored the association between CVD and mental distress in all studied individuals. Income was excluded from the analyses since too many respondents had not answered that question. The ANCOVA on the associations between severity of mental distress and prevalence of CVD, showed a statistically significant difference in level of sleep disturbance between individuals with CVD (M = 6.50, SD = 3.96) and those without CVD (M = 4.36, SD = 3.81) [F (47.43), DF = 1, p < 0.001]. The difference remained after controlling for ethnic group, gender and BMI (F for in between group = 23.25, p < 0.001). There was also statistically significant difference in burnout score between the CVD group (M = 21.48, SD = 9.43) and the reference group (M = 18.57, SD = 8.83) [F (16.06), DF = 1, p < 0.001]. The difference remained after controlling for ethnic group, gender and BMI (F for in between group = 14.81, p < 0.001). The difference in stress score between the CVD group (M = 16.79, SD = 7.63) and the reference group (M = 15.55, SD = 8.46) did not show a trend [F (3.54), DF = 1, p = 0.060]. The difference remained insignificant after controlling for ethnic group, gender, and BMI. Thus, in this study, sleep disturbance and burnout seem to be associated with CVD, but not stress.
The logistic regression analyses (Table 2) indicated that compared to individuals with low levels of sleep problems, individuals with high levels of sleep problems have 2.16 (95% CI 1.4–3.34) times higher odds of having a CVD. Compared to individuals with low levels of burnout, individuals with high levels of burnout have higher (1.58 95% CI 1.07–2.33) odds of having a CVD. There was no difference in chances of having a CVD among individuals with high level of perceived stress compared to low level of perceived stress group. As for the differences in ethnic groups, in analysis of burnout and stress, compared to the majority ethnic group Kyrgyz, East Europeans had 1.55 (95% CI 1.02–2.35—for burnout) and 1.52 (1.01–2.31 for stress) times higher odds of having a CVD. Furthermore, compared to Kyrgyz, Central Asians and Other minorities had a tendency for lower odds and Western Asians and East Asians had a tendency for higher odds of having a CVD in case of all mental distress factors. However, these associations need to be considered carefully considering the small number of representatives in some minority groups.
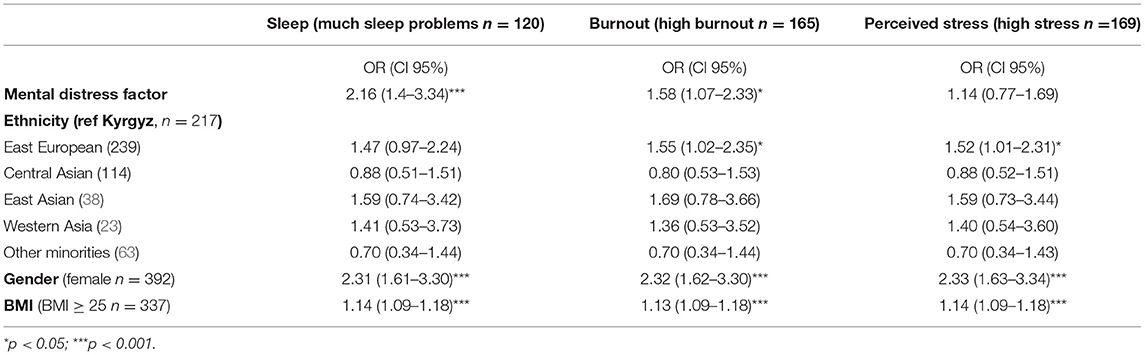
Table 2. Association between mental distress factors and cardiovascular disease in regression analysis, odds ratios (95% CI); models adjusted for ethnicity and gender, and BMI (n = 694; with CVD n = 234).
Discussion
This study addressed the differences in cardiovascular health as well as social and psychological determinants in Kyrgyzstan. As for the prevalence of CVD, the results confirm findings of earlier studies showing different CVD pattern among various ethnic groups (32, 37). Particularly, East-Europeans like Russians have been shown to have a higher prevalence of CVD compared to Central Asians (Kyrgyzs and Kazakhs) (33). This study indicated significantly higher prevalence of CVD among East Europeans (42.7%) and Western Asians (39.1%) compared to Kyrgyz people (30.9%). Furthermore, compared to these groups, the prevalence of CVD was significantly lower among Central Asians (26.3%) and Other minorities (Dungans and Uyghurs, 20.6%). This may be explained by the tendency of East Europeans and Western Asians, compared to Kyrgyzs and Central Asians (Kazakhs, Tajiks) and other minorities, showing lower CVD mortality attributable to dietary risk, including less alcohol consumption (12, 76, 77).
We also clarified the levels of mental distress factors among the ethnic groups in Kyrgyzstan. Based on studies of Salyers and Bond (78), Mezick et al. (61), Grandner et al. (62), and Slopen et al. (63), we expected ethnic differences in burnout and sleep disturbances. However, in the current study the levels of burnout or sleep disturbance did not differ among ethnic groups whereas such differences by ethnic groups have been shown in other contexts (79). Vice versa, in this study, the mean score value of stress was lower among East Asians (M = 14.7) and Other minorities (Dungans and Uygurs, M = 12.9) than among the Kyrgyzs, East Europeans, and Central Asians (m > 16.3). This suggests that the majority population, Kyrgyz, does not stand out as having particularly better mental health than the other ethnic groups. The conclusions on the ethnic differences in burnout and sleep disturbance differ from those from studies in the US (61, 79). Thus, the present finding that in Kyrgyzstan, compared to other ethnic groups, the majority of the population, Kyrgyzs do not stand out having better mental stress outcomes can be explained by the lower economic status of this group (80–82). Furthermore, the higher rate of mental stress in Kyrgyzs, East Europeans and Central Asians may be attributed to the fact that unlike these ethnic groups, East Asians (Koreans), Dungans and Uyghurs (Other minorities) have kept their religious practices (e.g., pray five times a day) throughout Soviet time till currently (83–85), and religious practices have been associated with positive mental health outcomes (86).
The ANCOVAs showed significantly higher levels of sleep disturbance and burnout in the CVD group compared to the referent group. This difference remained significant after controlling for ethnic group, gender and BMI. Our regression analysis confirmed that compared to the individuals with lower levels of sleep problems and burnout, individuals with high levels of either of these mental distress factors were more likely to have CVD. Earlier studies have shown that poor sleep can lead to disease (51, 52) and cause exhaustion disorder and stress (49). Thus, our findings of associations of CVD with sleep disturbance and burnout, but not with stress, are not surprising. Stress fluctuates strongly over time to cope with everyday hassles, which compromises the sensitivity of this variable. Despite of previous reports of declining of sleep disturbance with age (79, 87), our results did not find this negative correlation.
In our logistic regression analysis for burnout and stress we could see significantly higher odds of having a CVD among East Europeans compared to Kyrgyz; and a tendency for lower odds compared to Central Asians and Other minorities compared to Kyrgyz. Thus, next to the level of mental distress, gender and BMI, specificities in ethnic groups may be associated with the higher prevalence of CVD. The mechanisms behind the effect of ethnic group for mental distress factors and CVD needs further exploration. The cross-sectional design of this study does not enable to test of such cause and effect. Whereas, ethnic group can be expected to be a cause rather than effect in this context, the associations can well be bidirectional.
We believe that some of our results may be explained by insufficient number of minority participants. Despite stratified random sampling, ethnic groups differed significantly in age, gender, and education. The invitations for participation directed at patients visiting polyclinics and health care centers cannot be expected to have resulted in a fully representative sample of participants, which compromises the representativeness of the findings, in particular regarding the prevalence rates. Since results on prospective self-reported assessment of mental distress, such as sleep disturbance and burnout, lack in consistency (88), there is a need for further assessment as well as psychophysiological evaluation. We also asked the participants about having any CVD diagnosed by a doctor rather than using hospital records. This might have caused diagnosis bias, even if we specified CVD diagnosed by a doctor.
Nevertheless, the current study is one of the very few studies of health inequality among ethnic minorities in Central Asia. The current findings add value to the existing bulk of knowledge of mechanisms mediating the relationship between cultural, mental stress factors, and CVD. The present use of self-reported CVD and mental distress may in future research be complemented by hospital records of CVD diagnosis and psychophysiological measures related to distress.
Conclusion
This study suggests that Kyrgyz people have lower prevalence of CVD, compared to East Europeans and Western Asians in Kyrgyzstan, and higher compared to Central Asians and Other minorities. In studied sample in Kyrgyzstan, individuals with relatively high level of sleep disturbance and burnout, more likely reported suffering from CVD. Next to the mental distress factors, gender and BMI, the characteristics of ethnic groups may be associated with the higher prevalence of CVD, as there were higher odds for CVD among East Europeans compared to Kyrgyz.
The high prevalence rates indicate the need of better diagnosis and treatment of CVD and burnout as well as improving sleep quality with public health measures, including stress management, restful environment, increased physical activity, and better nutrition. Based on the present and previous study outcomes, it can be concluded that there is a need for the development of a relevant approach in mitigating sleep disturbance and preventing burnout in the general population, not only in specific ethnic groups.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
Ethical approval was received from the Research Ethics Committee of the International School of Medicine, Kyrgyzstan (Ref #10, 28.06. 2017). All study participants gave written informed consent in accordance with the Declaration of Helsinki.
Author Contributions
HA and KD contributed conception of the study and organized the data collection and analysis. KO and HO contributed design, methods of the study, and interpretation of the data. MN and SN contributed interpretation of the study findings. KO and HA performed the statistical analysis and wrote the first draft of the manuscript. HO and KD wrote sections of the manuscript. All authors contributed to the manuscript revision, read and approved the submitted version.
Funding
This study was supported by the International School of Medicine, Bishkek, Kyrgyzstan (Order #21 18.02.2016). HO's work was supported by the Estonian Ministry of Education and Research, grant IUT34-17, and MN's and SN's work by AFA Insurance, Sweden (190082). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to express the gratitude to the staff of the Polyclinics number 7, 10, 13 of Bishkek city, the Family Medicine center of the Issyk-Ata district, and the Family Medicine center of the Toktogul district who have enabled the data collection of this study.
References
1. Lazzini A, Lazzini S. Cardiovascular disease: an economical perspective. Curr Pharm Des. (2009) 15:1142–56. doi: 10.2174/138161209787846883
2. WHO. The World Health Report 2002 - Reducing Risks, Promoting Healthy Life. Geneva: World Health Organization (2002).
3. [Dataset] WHO. Noncommunicable Diseases Country Profiles 2018. (2018). Available online at: https://www.who.int/nmh/countries/en/ (accessed March 31, 2021).
4. [Dataset] National Statistical Committee of the Kyrgyz Republic. Total Population by Nationality. (2018). Available online at: http://www.stat.kg/en/ (accessed March 31, 2021).
5. Akesson A, Larsson SC, Discacciati A, Wolk A. Low-risk diet and lifestyle habits in the primary prevention of myocardial infarction in men: a population-based prospective cohort study. J Am Coll Cardiol. (2014) 64:1299–306. doi: 10.1016/j.jacc.2014.06.1190
6. Chomistek AK, Chiuve SE, Eliassen AH, Mukamal KJ, Willett WC, Rimm EB. Healthy lifestyle in the primordial prevention of cardiovascular disease among young women. J Am Coll Cardiol. (2015) 65:43–51. doi: 10.1016/j.jacc.2014.10.024
7. Hulsegge G, Looman M, Smit HA, Daviglus ML, van der Schouw YT, Verschuren WM. Lifestyle changes in young adulthood and middle age and risk of cardiovascular disease and all-cause mortality: the Doetinchem cohort study. J Am Heart Assoc. (2016) 5:e002432. doi: 10.1161/JAHA.115.002432
8. Maruthur NM, Wang NY, Appel LJ. Lifestyle interventions reduce coronary heart disease risk: results from the PREMIER trial. Circulation. (2009) 119:2026–31. doi: 10.1161/CIRCULATIONAHA.108.809491
9. Meng XJ, Dong GH, Wang D, Liu MM, Lin Q, Tian S, et al. Prevalence, awareness, treatment, control, and risk factors associated with hypertension in urban adults from 33 communities of China: the CHPSNE study. J Hypertens. (2011) 29:1303–10. doi: 10.1097/HJH.0b013e328347f79e
10. Stevens VJ, Obarzanek E, Cook NR, Lee IM, Appel LJ, Smith West D, et al. Long-term weight loss and changes in blood pressure: results of the trials of hypertension prevention, phase II. Ann Intern Med. (2001) 134:1–11. doi: 10.7326/0003-4819-134-1-200101020-00007
11. West DS, Elaine Prewitt T, Bursac Z, Felix HC. Weight loss of black, white, and Hispanic men and women in the Diabetes Prevention Program. Obesity. (2008) 16:1413–20. doi: 10.1038/oby.2008.224
12. Meier T, Gräfe K, Senn F, Sur P, Stangl GI, Dawczynski C, et al. Cardiovascular mortality attributable to dietary risk factors in 51 countries in the WHO European region from 1990 to 2016: a systematic analysis of the Global Burden of Disease Study. Eur J Epidemiol. (2019) 34:37–55. doi: 10.1007/s10654-018-0473-x
13. Canto JG, Rogers WJ, Goldberg RJ, Peterson ED, Wenger NK, Vaccarino V, et al. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. JAMA. (2012) 307:813–22. doi: 10.1001/jama.2012.199
14. Iorga A, Cunningham CM, Moazeni S, Ruffenach G, Umar S, Eghbali M. The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biol Sex Differ. (2017) 8:33. doi: 10.1186/s13293-017-0152-8
15. Hayward CS, Kelly RP, Collins P. The roles of gender, the menopause and hormone replacement on cardiovascular function. Cardiovasc Res. (2000) 46:28–49. doi: 10.1016/S0008-6363(00)00005-5
17. Clark AM, DesMeules M, Luo W, Duncan AS, Wielgosz A. Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol. (2009) 6:712–22. doi: 10.1038/nrcardio.2009.163
18. Ramsay SE, Morris RW, Whincup PH, Papacosta O, Rumley A, Lennon L, et al. Socioeconomic inequalities in coronary heart disease risk in older age: contribution of established and novel coronary risk factors. J Thromb Haemost. (2009) 7:1779–86. doi: 10.1111/j.1538-7836.2009.03602.x
19. Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. (1992) 82:816–20. doi: 10.2105/AJPH.82.6.816
20. Franks P, Winters PC, Tancredi DJ, Fiscella KA. Do changes in traditional coronary heart disease risk factors over time explain the association between socio-economic status and coronary heart disease? BMC Cardiovasc Disord. (2011) 11:28. doi: 10.1186/1471-2261-11-28
21. Stringhini S, Carmeli C, Jokela M, Avendaño M, Muennig P, Guida F, et al. Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1·7 million men and women. Lancet. (2017) 389:1229–37. doi: 10.1016/S0140-6736(16)32380-7
22. Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. (2005) 111:1233–41. doi: 10.1161/01.CIR.0000158136.76824.04
23. [Dataset] Bank TW. GINI Index. Kyrgyzstan (2018). Available online at: https://data.worldbank.org/indicator/SI.POV.GINI?locations=KG&view=map (accessed March 31, 2021).
24. Holmes L, Hossain J, Ward D, Opara F. Racial/ethnic variability in hypertension prevalence and risk factors in National health interview survey. ISRN Hypertension. (2013) 2013:257842. doi: 10.5402/2013/257842
25. Freund KM, Jacobs AK, Pechacek JA, White HF, Ash AS. Disparities by race, ethnicity, and sex in treating acute coronary syndromes. J Women's Health. (2012) 21:126–32. doi: 10.1089/jwh.2010.2580
26. Kurian AK, Cardarelli KM. Racial and ethnic differences in cardiovascular disease risk factors: a systematic review. Ethn Dis. (2007) 17:143–52. doi: 10.13016/rsqw-ztls
27. Liu R, So L, Mohan S, Khan N, King K, Quan H. Cardiovascular risk factors in ethnic populations within Canada: results from national cross-sectional surveys. Open Med. (2010) 4:e143–53.
28. Perini W, Kunst AE, Snijder MB, Peters RJG, van Valkengoed IGM. Ethnic differences in metabolic cardiovascular risk among normal weight individuals: implications for cardiovascular risk screening. The HELIUS study. Nutr Metab Cardiovasc Dis. (2019) 29:15–22. doi: 10.1016/j.numecd.2018.09.004
29. Khan NA, Grubisic M, Hemmelgarn B, Humphries K, King KM, Quan H. Outcomes after acute myocardial infarction in South Asian, Chinese, and white patients. Circulation. (2010) 122:1570–7. doi: 10.1161/CIRCULATIONAHA.109.850297
30. Lewey J, Shrank WH, Bowry AD, Kilabuk E, Brennan TA, Choudhry NK. Gender and racial disparities in adherence to statin therapy: a meta-analysis. Am Heart J. (2013) 165:665–78, 78.e1. doi: 10.1016/j.ahj.2013.02.011
31. Gupta M, Tabas JA, Kohn MA. Presenting complaint among patients with myocardial infarction who present to an urban, public hospital emergency department. Ann Emerg Med. (2002) 40:180–6. doi: 10.1067/mem.2002.126396
32. Carson AP, Howard G, Burke GL, Shea S, Levitan EB, Muntner P. Ethnic differences in hypertension incidence among middle-aged and older adults: the multi-ethnic study of atherosclerosis. Hypertension. (2011) 57:1101–7. doi: 10.1161/HYPERTENSIONAHA.110.168005
33. Kontsevaya A, Myrzamatova A A, Polupanov A, Alikhanova K, Kashirin A, Khalmatov A, et al. Ethnic specifics of the main cardiovascular risk factors prevalence among rural inhabitants of a Russian region and regions of Kyrgyzstan and Kazakhstan. Russ J Cardiol. (2017) 146:113–21. doi: 10.15829/1560-4071-2017-6-113-121
34. Algren MH, Ekholm O, Nielsen L, Ersbøll AK, Bak CK, Andersen PT. Associations between perceived stress, socioeconomic status, and health-risk behaviour in deprived neighbourhoods in Denmark: a cross-sectional study. BMC Public Health. (2018) 18:250. doi: 10.1186/s12889-018-5170-x
35. Cohen S, Janicki-Deverts D, Doyle WJ, Miller GE, Frank E, Rabin BS, et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc Natl Acad Sci USA. (2012) 109:5995–9. doi: 10.1073/pnas.1118355109
36. Khandaker GM, Zuber V, Rees JMB, Carvalho L, Mason AM, Foley CN, et al. Shared mechanisms between coronary heart disease and depression: findings from a large UK general population-based cohort. Mol Psychiatry. (2020) 25:1477–86. doi: 10.1038/s41380-019-0395-3
37. Liu RT, Alloy LB. Stress generation in depression: a systematic review of the empirical literature and recommendations for future study. Clin Psychol Rev. (2010) 30:582–93. doi: 10.1016/j.cpr.2010.04.010
38. Kivimäki M, Nyberg ST, Batty GD, Fransson EI, Heikkilä K, Alfredsson L, et al. Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet. (2012) 380:1491–7. doi: 10.1016/S0140-6736(12)60994-5
39. Compare A, Zarbo C, Manzoni GM, Castelnuovo G, Baldassari E, Bonardi A, et al. Social support, depression, and heart disease: a ten year literature review. Front Psychol. (2013) 4:384. doi: 10.3389/fpsyg.2013.00384
40. Glassman AH, Bigger JT Jr, Gaffney M. Psychiatric characteristics associated with long-term mortality among 361 patients having an acute coronary syndrome and major depression: seven-year follow-up of SADHART participants. Arch Gen Psychiatry. (2009) 66:1022–9. doi: 10.1001/archgenpsychiatry.2009.121
41. Rugulies R. Depression as a predictor for coronary heart disease. A review and meta-analysis. Am J Prev Med. (2002) 23:51–61. doi: 10.1016/S0749-3797(02)00439-7
42. Nicholson A, Kuper H, Hemingway H. Depression as an aetiologic and prognostic factor in coronary heart disease: a meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur Heart J. (2006) 27:2763–74. doi: 10.1093/eurheartj/ehl338
43. Richardson S, Shaffer JA, Falzon L, Krupka D, Davidson KW, Edmondson D. Meta-analysis of perceived stress and its association with incident coronary heart disease. Am J Cardiol. (2012) 110:1711–6. doi: 10.1016/j.amjcard.2012.08.004
44. Balch CM, Freischlag JA, Shanafelt TD. Stress and burnout among surgeons: understanding and managing the syndrome and avoiding the adverse consequences. Arch Surg. (2009) 144:371–6. doi: 10.1001/archsurg.2008.575
45. Marmot M, Friel S, Bell R, Houweling TAJ, Taylor S. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. (2008) 372:1661–9. doi: 10.1016/S0140-6736(08)61690-6
46. Sørensenf C, Friis-Hasché E, Haghfelt T, Bech P. Postmyocardial infarction mortality in relation to depression: a systematic critical review. Psychother Psychosom. (2005) 74:69–80. doi: 10.1159/000083165
47. Coppock V, Dunn B. Understanding Social Work Practice in Mental Health. London (2010). Available online at: https://sk.sagepub.com/books/understanding-social-work-practice-in-mental-health (accessed March 31, 2021).
48. Gunther PW, Sanches M F. SCC, Krishnadath ISK. Prevalence of psychological distress in Suriname in urban and rural areas: the Suriname Health Study. J Human Psychol. (2017) 1:8–17. doi: 10.14302/issn.2644-1101.jhp-17-1665
49. Söderström M, Jeding K, Ekstedt M, Perski A, Akerstedt T. Insufficient sleep predicts clinical burnout. J Occup Health Psychol. (2012) 17:175–83. doi: 10.1037/a0027518
50. Welfare SNBoHa. Utmattnings syndrom. Stressrelaterad Psykisk Ohälsa. Stockholm: Bjurner& Bruno AB (2003).
51. Roth T, Roehrs T. Insomnia: epidemiology, characteristics, and consequences. Clin Cornerstone. (2003) 5:5–15. doi: 10.1016/S1098-3597(03)90031-7
52. Ekstedt M, Akerstedt T, Söderström M. Microarousals during sleep are associated with increased levels of lipids, cortisol, and blood pressure. Psychosom Med. (2004) 66:925–31. doi: 10.1097/01.psy.0000145821.25453.f7
53. Mariotti A. The effects of chronic stress on health: new insights into the molecular mechanisms of brain-body communication. Future Sci OA. (2015) 1:FSO23. doi: 10.4155/fso.15.21
54. Rohleder N. Chapter 9 - Chronic stress and disease. In: Berczi I, editor. Insights to Neuroimmune Biology, 2nd ed. Amsterdam: Elsevier (2016). p. 201–14.
55. Bell CC. DSM-IV: diagnostic and statistical manual of mental disorders. JAMA. (1994) 272:828–9. doi: 10.1001/jama.1994.03520100096046
56. McEwen BS, Eiland L, Hunter RG, Miller MM. Stress and anxiety: structural plasticity and epigenetic regulation as a consequence of stress. Neuropharmacology. (2012) 62:3–12. doi: 10.1016/j.neuropharm.2011.07.014
57. Sagaspe P, Taillard J, Bayon V, Lagarde E, Moore N, Boussuge J, et al. Sleepiness, near-misses and driving accidents among a representative population of French drivers. J Sleep Res. (2010) 19:578–84. doi: 10.1111/j.1365-2869.2009.00818.x
58. Serban C, Drăgan S. The relationship between inflammatory and oxidative stress biomarkers, atherosclerosis and rheumatic diseases. Curr Pharm Des. (2014) 20:585–600. doi: 10.2174/138161282004140213145806
59. Kattoor AJ, Pothineni NVK, Palagiri D, Mehta JL. Oxidative stress in atherosclerosis. Curr Atheroscler Rep. (2017) 19:42. doi: 10.1007/s11883-017-0678-6
60. Wirtz PH, von Känel R. Psychological stress, inflammation, and coronary heart disease. Curr Cardiol Rep. (2017) 19:111. doi: 10.1007/s11886-017-0919-x
61. Mezick EJ, Matthews KA, Hall M, Strollo PJ Jr, Buysse DJ, Kamarck TW, et al. Influence of race and socioeconomic status on sleep: Pittsburgh SleepSCORE project. Psychosom Med. (2008) 70:410–6. doi: 10.1097/PSY.0b013e31816fdf21
62. Grandner MA, Petrov MER, Rattanaumpawan P, Jackson N, Platt A, Patel NP. Sleep symptoms, race/ethnicity, and socioeconomic position. J Clin Sleep Med. (2013) 9:897–905. doi: 10.5664/jcsm.2990
63. Slopen N, Williams DR. Discrimination, other psychosocial stressors, and self-reported sleep duration and difficulties. Sleep. (2014) 37:147–56. doi: 10.5665/sleep.3326
64. Johnson DA, Jackson CL, Williams NJ, Alcántara C. Are sleep patterns influenced by race/ethnicity - a marker of relative advantage or disadvantage? Evidence to date. Nat Sci Sleep. (2019) 11:79–95. doi: 10.2147/NSS.S169312
65. Phinney JS, Ong AD. Conceptualization and measurement of ethnic identity: current status and future directions. J Couns Psychol. (2007) 54:271–81. doi: 10.1037/0022-0167.54.3.271
66. Hoffmeyer-Zlotnik J, Warner U. Sociodemographic Questionnaire Modules for Comparative Social Surveys. Cham: Springer (2018).
67. WHO. Physical Status: The Use and Interpretation of Anthropometry. Report of a WHO Expert Committee. WHO Technical Report Series 854. Geneva: World Health Organization (1995).
68. Consultation WE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. (2004) 363:157–63. doi: 10.1016/S0140-6736(03)15268-3
69. Nordin M, Åkerstedt T, Nordin S. Psychometric evaluation and normative data for the Karolinska Sleep Questionnaire. Sleep Biol Rhythms. (2013) 11:216–26. doi: 10.1111/sbr.12024
70. Melamed S, Kushnir T, Shirom A. Burnout and risk factors for cardiovascular diseases. Behav Med. (1992) 18:53–60. doi: 10.1080/08964289.1992.9935172
71. Melamed S, Ugarten U, Shirom A, Kahana L, Lerman Y, Froom P. Chronic burnout, somatic arousal and elevated salivary cortisol levels. J Psychosom Res. (1999) 46:591–8. doi: 10.1016/S0022-3999(99)00007-0
72. Grossi G, Perski A, Evengård B, Blomkvist V, Orth-Gomér K. Physiological correlates of burnout among women. J Psychosom Res. (2003) 55:309–16. doi: 10.1016/S0022-3999(02)00633-5
73. Taylor JM. Psychometric analysis of the Ten-Item Perceived Stress Scale. Psychol Assess. (2015) 27:90–101. doi: 10.1037/a0038100
74. Cohen S. Perceived stress in a probability sample of the United States. The social psychology of health. In: The Claremont Symposium on Applied Social Psychology. Thousand Oaks, CA: Sage Publications, Inc., (1988). p. 31–67.
76. Guillot M, Gavrilova N, Pudrovska T. Understanding the “Russian mortality paradox” in Central Asia: evidence from Kyrgyzstan. Demography. (2011) 48:1081–104. doi: 10.1007/s13524-011-0036-1
77. Sharygin EJ, Guillot M. Ethnicity, russification, and excess mortality in Kazakhstan. Vienna Yearb Popul Res. (2013) 11:219–46. doi: 10.1553/populationyearbook2013s219
78. Salyers MP, Bond GR. An exploratory analysis of racial factors in staff burnout among assertive community treatment workers. Community Ment Health J. (2001) 37:393–404. doi: 10.1023/A:1017575912288
79. Grandner MA, Patel NP, Gehrman PR, Xie D, Sha D, Weaver T, et al. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med. (2010) 11:470–8. doi: 10.1016/j.sleep.2009.10.006
80. Schmidt M, Sagynbekova L. Migration past and present: changing patterns in Kyrgyzstan. Cent Asian Surv. (2008) 27:111–27. doi: 10.1080/02634930802355030
81. Agadjanian V, Gorina E. Economic swings, political instability and migration in Kyrgyzstan. Eur J Popul. (2018) 35:285–304. doi: 10.1007/s10680-018-9482-4
82. Hatcher C, Thieme S. Institutional transition: internal migration, the propiska, and post-socialist urban change in Bishkek, Kyrgyzstan. Urban Stud. (2015) 53:2175–91. doi: 10.1177/0042098015587252
83. Kokaisl P. Koreans in Central Asia – a different Korean nation. Asian Ethn. (2018) 19:428–52. doi: 10.1080/14631369.2018.1439725
84. Hann C, Pelkmans M. Realigning religion and power in Central Asia: Islam, Nation-State and (Post)Socialism. Europe-Asia Stud. (2009) 61:1517–41. doi: 10.1080/09668130903209111
85. Ashymov D. The religious faith of the Kyrgyz. Relig State Soc. (2003) 31:133–8. doi: 10.1080/09637490308277
86. Fabricatore AN, Handal PJ, Rubio DM, Gilner FH. RESEARCH: stress, religion, and mental health: religious coping in mediating and moderating roles. Int J Psychol Relig. (2004) 14:91–108. doi: 10.1207/s15327582ijpr1402_2
87. Grandner MA, Martin JL, Patel NP, Jackson NJ, Gehrman PR, Pien G, et al. Age and sleep disturbances among American men and women: data from the U.S. behavioral risk factor surveillance system. Sleep. (2012) 35:395–406. doi: 10.5665/sleep.1704
88. Grandner MA. Sleep, health, and society. Sleep Med Clin. (2017) 12:1–22. doi: 10.1016/j.jsmc.2016.10.012
Appendix
Keywords: mental distress, cardiovascular disease, ethnicity, Central Asia, minority
Citation: Azfar HS, Dzhusupov KO, Orru H, Nordin S, Nordin M and Orru K (2021) Cardiovascular Disease and Mental Distress Among Ethnic Groups in Kyrgyzstan. Front. Public Health 9:489092. doi: 10.3389/fpubh.2021.489092
Received: 01 August 2019; Accepted: 17 March 2021;
Published: 04 May 2021.
Edited by:
Wulf Rössler, Charité – Universitätsmedizin Berlin, GermanyReviewed by:
Serge Brand, University Psychiatric Clinic Basel, SwitzerlandSouheil Hallit, Holy Spirit University of Kaslik, Lebanon
Rene Schilling, University of Basel, Switzerland
Copyright © 2021 Azfar, Dzhusupov, Orru, Nordin, Nordin and Orru. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hans Orru, hans.orru@umu.se
 Hossain Syed Azfar
Hossain Syed Azfar Kenesh O. Dzhusupov2
Kenesh O. Dzhusupov2 Hans Orru
Hans Orru