- 1Department of Obstetrics and Gynecology, Faculty of Medicine Vajira Hospital, Navamindradhiraj University, Bangkok, Thailand
- 2Department of Pediatrics, Faculty of Medicine, Prince of Songkla University, Hat Yai, Thailand
Objective: Over the last 10 years, online interventions to improve mental health have increased significantly. This study's primary objective was to determine the effectiveness of online interventions in improving the mental health of pediatric, adolescent, and young adult (PAYA) cancer survivors. The secondary objective was to identify the independent variables associated with online intervention efficacy for mental health improvement.
Methods: On June 25–30, 2021, we searched the Medline, PsycINFO, EMBASE, and Cochrane databases for eligible English language publications that reported randomized controlled trials of online interventions aimed at improving mental health among PAYA cancer survivors. The results were analyzed using a systematic review and a three-level meta-analysis.
Results: Thirteen studies met the inclusion criteria. In six (42%) studies, the intervention focused on physical activity enhancement, while ten (77%) studies used self-directed interventions. Online interventions were more efficacious, compared to control conditions, in improving sleep g = 0.35 (95% CI 0.04–0.66) and psychological well-being g = 0.32 (95% CI 0.09–0.56), but not for reducing the symptoms of depression g = 0.17 (95% CI −0.13 to 0.47), anxiety g = 0.05 (95% CI −0.15 to 0.25), and pain g = 0.13 (95% CI −0.13 to 0.39).
Conclusion: Online interventions were generally effective in improving mental health in PAYA cancer survivors, although negative results were found in some critical outcomes. More high-quality evidence is needed for definite conclusions to be drawn. The study protocol was registered in PROSPERO (CRD42021266276).
Background
Advanced treatment modalities have increased the survival rate of children, adolescents, and young adults with cancer to above 80% (1, 2). The United States has over 400,000 cases, and this population is growing, with 10,000 new cases diagnosed each year (3). Centers for Disease Control and Prevention have defined that cancer survivor is anyone who has been diagnosed with cancer, from the time of diagnosis through the balance of his or her life (4). A cancer diagnosis during children (defined as ages 0–15) and adolescence or young adulthood (AYA; defined as ages 15–39) generates unique medical and psychological needs as developmental milestones are simultaneously impacted (5). For instance, a critical element of the adolescent population (i.e., those aged 15–20) is the confluence of the cancer experience with a period of rapid biological and psychological changes. Specifically, this group may face difficulties with autonomy and independence, sexual and romantic maturity, reproduction, and economics (6). Additionally, adverse effect of cancer therapy can have a physical impact on survivors, as well as affect their self-image and well-being in the short and long term (5, 6). Consequently, pediatric, adolescent, and young adult (PAYA) cancer survivors face a variety of problems, including disruptions in education, careers, and social milestones, as well as the long-term side effects of their treatments (7–9).
Cancer treatment complications and unique psychological development combine to associated with mental health problems (10), including post-traumatic stress disorder (11), anxiety (12), and depression (13), which are frequently observed in PAYA cancer survivors. More than half of PAYA cancer survivors reported at least one significant chronic mental health problem that requires ongoing care (14). However, they are often lost to follow-up (15, 16) and have an inadequate understanding of their cancer care (17). Therefore, more research on PAYA cancer survivors' mental health interventions to solve unmet psychological needs is critically needed.
Cancer knowledge, self-efficacy, coping style, and physical activity play a significant role in the onset and persistence of mental health problems in PAYA cancer survivors (18).
Having a limited or inaccurate cancer knowledge may impair survivors' ability to communicate effectively with healthcare providers, which may have an effect on the quality of care they receive. Inadequate cancer knowledge also prevents survivors from taking critical efforts to avoid health risks in their daily lives (e.g., smoking cessation, physical activity, diet) (19, 20). Cancer-related self-efficacy refers to the belief that a survivor can successfully carry out the behaviors necessary to achieve the desired outcome in connection to the effects of cancer and its treatment (21). Self-efficacy is connected with greater self-care behaviors and lower physical and psychological symptoms in cancer patients (22). For the coping style, while some cancer survivors employ adaptive coping methods to alleviate suffering, others rely on less adaptive coping mechanisms (23). Poor adaptive coping may provide a momentary reprieve from anxiety-provoking thoughts, these ideas may grow more obsessive and intrusive with time (24). Physical activity has been shown to be beneficial in reducing the cluster of symptoms associated with cancer treatment (25). Regular physical activity or exercise has been shown to promote positive psychological functioning (26) and can be used to cope with the side effects of cancer and its treatment, including increased feelings of depression, anxiety, sleep difficulties, and cancer-related fatigue (27), as well as the cognitive confusion or impairment that frequently persists following cancer treatment (28, 29). A bidirectional relationship between these factors and mental health outcomes has been proven (30). From this perspective, intervention programs seek to improve PAYAs' mental health by increasing their cancer knowledge, self-efficacy, coping style, and physical activity (30).
Despite the well-established interventions for PAYAs' mental health, few PAYA cancer survivors receive such interventions (31). Several challenges faced by PAYA cancer survivors when using mental health services include the cost of services, inconvenient timing or location, and a shortage of competent staff (32–34). Technology based interventions, using the webpages, email, mobile applications, and social media can help them to overcome these constraints (35). Technology-based interventions are those that use a technological platform to give information, support, and therapy for physical or mental health problems (36). Early technology-based interventions in the field of mental health were typically static with minimal interactivity and were delivered offline (e.g., via a PC or laptop equipped with a CD-ROM or installed software), requiring patients to be in a certain location to receive the intervention. Recent advancements in digital technology have enabled the potential of online intervention, which is typically defined as the delivery of a computerized program via the Internet (37). Online interventions utilize telecommunications systems (e.g., text messaging, emailing, and videoconferencing) to provide the distant delivery of synchronous and asynchronous interventions (36–38). PAYA cancer survivors may participate in interventions from the convenience of their own residents and at a lower cost than that for face-to-face interventions, depending on the quality of technology-based interventions (39, 40). The most common manner to offer technology-based interventions is through online platforms (38, 41). The benefits of these interventions include immediate access, the ability to update content easily, the patients' ability to ask questions and receive help, and the ability to track their progress (42, 43). Because internet penetration is constantly expanding, online interventions for improving mental health of PAYA cancer survivors are increasingly promising (44).
Both single studies (45, 46)and two meta-analyses studying on the effect of distance-delivered physical activity interventions and technology-assisted psychosocial interventions support the efficacy of online interventions on improving PAYA's mental health (47, 48). However, a recent meta-analysis studying on the effect of digital self-management interventions revealed an inconsistent finding (49). Mizrahi et al. (47) demonstrated the moderate effectiveness of distance-delivered physical activity interventions in improving psychosocial outcomes in childhood cancer survivors. Zhang et al. (48) discovered that technology-assisted interventions are effective for a variety of children's outcomes (distraction from intrusive treatment—medium effect size, mental health—small effect size, physical health—small effect size, and cancer knowledge—small effect size). However, Hong et al. (49) found that digital self-management interventions do not influence the quality of life and physical activity.
Apart from drawing inconclusive findings, these meta-analyses have several noteworthy limitations. Overall, previous meta-analyses examined the effect of technology-based interventions without examining the effectiveness of online interventions separately. For example, Zhang et al. (48) conducted a meta-analysis on the effectiveness of technology-assisted psychosocial interventions for childhood, adolescent, and young adult cancer survivors and found that eight out of twenty-eight randomized controlled trials (RCTs) examined online interventions; however, their independent effectiveness was not examined. The effect sizes for mental and physical health outcomes were pooled by merging research with a variety of objectives. Mizrahi et al. (47) conducted a meta-analysis, which included four trials that focused exclusively on distance-delivered physical activity interventions for childhood cancer survivors. Hong et al. (49) focused exclusively on physical health outcomes and quality of life. No study analyzed mental and physical health outcomes separately.
The primary objective of this study was to determine the effectiveness of online interventions in improving the mental health of PAYA cancer survivors. The secondary objective was to identify the independent variables associated with online intervention efficacy for mental health improvement. This study included difference instruments and outcomes. Furthermore, several groups explored the use and effects of online intervention and reported meaningful results. To date, evidence regarding the effects of online intervention on mental health of PAYA cancer survivors has not been synthesized for clinical practice.
Methods
Protocol
This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (50). The study protocol was registered in PROSPERO (CRD42021266276).
Selection Procedure
English language reports published in peer-reviewed sources were included. We assessed study eligibility using the PICO approach (population, intervention, comparison, and outcome) (51).
Population
Children, adolescents, or young adult patients with or survivors of cancer (0–39 years of age with cancer diagnoses) (48). Studies of adult patients with cancer (>40 years of age with cancer diagnoses), patients without current cancer or a cancer history, or caregivers of patients with cancer were excluded.
Intervention
Any psychological intervention that were delivered online, using a computer or a mobile application (both therapists delivered and self-directed). Interventions that involved physical approaches—for example, physical activity intervention—could be included in the intervention but only if they were delivered online. Interventions were not required to directly target mental health.
Comparison
Eligible studies were required to use a control group—for example, waitlist, treatment as usual, or alternative control. Case studies, studies that included only two active psychological interventions and no control group (e.g., non-inferiority trials) were excluded from the meta-analysis.
Outcome
Pre- and postintervention data, or pre–post change score data on one or more quantitative mental health outcome. Mental health outcome could be both primary and secondary outcome. Studies that used qualitative assessments, quantitative measures at one-time point only, or only measures of quality of life were excluded. Studies needed to report results as either pre–post means and standard deviation/SE in all groups with sufficient detail to allow the calculation of an effect size, or the data could be requested from the authors. Studies that lacked sufficient data to calculate the effect size or had a sample size of less than N = 10 were also omitted, as were pilot studies that did not adequately explore the effectiveness of interventions in improving PAYAs' mental health.
Searching Strategies
The literature was searched extensively for RCTs examining online interventions that were aimed at improving mental health for PAYA cancer survivors. We searched for studies on June 25–30, 2021, in the Medline, PsycINFO, Web of Science, and Cochrane Library databases. The following keywords were used in the titles and abstracts: participants (e.g., child* OR pediatric OR adolescents* OR young adult OR AYA), cancer (e.g., cancer OR cancer survivor* OR oncology*), intervention (e.g., interv* OR program* OR educat* OR Psychosocial*), online (e.g., online* OR Internet* OR web*), and RCTs (e.g., controlled trial OR trial* OR RCT). We also reviewed the bibliographies of relevant review articles to identify additional publications. Please refer to Supplementary Appendix 1 for all the search strategies and approaches used to locate relevant articles in all the databases.
Study Selection
RefWorks was used to eliminate duplicate data. Both authors independently reviewed the studies' titles and abstracts for compliance with the inclusion criteria. Thereafter, the same authors reviewed the papers that were considered for full-text screening individually, and any disagreements were handled through a discussion. The inter-reviewer reliability (Kappa) was 0.93 (p < 0.001), indicating good inter-reviewer agreement.
Data Extraction
We extracted the studies' identifying data (i.e., authors, publication year, and country) and the data necessary for the effect size calculation (i.e., sample sizes, means, and standard deviations). Similarly, data on study procedures, interventions, and sample characteristics were retrieved. All extracted data were imported into R version 4.1.0, which was used to conduct the analyses.
Analyses and Coding of Independent Variables Associated With Intervention Efficacy
Consistent with our research question, the primary outcome was the mental health of PAYA cancer survivors, which was measured using tools with established psychometric properties. The secondary outcomes were independent variables that were associated with online intervention efficacy for mental health improvement. In the sensitivity analyses, the participants' ages were classified as follows: children and adolescents (<20 years) and adults (≥20 years) (30). Mental health outcomes were classified into five categories: depression, anxiety, pain, sleep, and psychological well-being. Psychological content was classified as follows: cognitive behavioral therapy (CBT), psychoeducation, physical activity, and legacy intervention (30, 47, 48). We also coded online interventions as individual and group deliveries. The comparison group comprised two conditions: a waiting list and an alternative treatment (face-to-face counseling or offline self-guided interventions). If patients underwent the intervention independently, they were classified as self-directed; they were classified as therapist-involved if the intervention program was administered directly by a therapist (e.g., videoconference) (30, 47, 48). Additionally, the online platforms for each intervention module were coded using the data contained in the articles. We coded platforms as websites alone, websites with text messages, wearable respiratory monitoring and applications, wearable physical activity monitoring and social media applications, chatbots, and VDO conferences (47–49). The continuous factors considered were the participants' mean age, length of the intervention, dropout rate, and bias risk.
Meta-Analytical Procedure
Because the studies were conducted in different countries and with participants from diverse socioeconomic backgrounds, the effect size was determined using a random-effects model (52). At each time point, the effect size on PAYAs' mental health was calculated independently (posttest and follow-up). The effect sizes of the online interventions were assessed in comparison to the control condition. Sensitivity analyses were employed to account for clinical and methodological heterogeneity in the secondary objective (53). The continuous variables were analyzed using meta-regression (54).
Effect Size Calculation
Compared to the control condition, the standard mean difference (SMD) as well as 95% confidence interval (CI), as the measure of online intervention effect, were calculated and then converted into the adjusted Hedges' g (55). The effect size is small between 0.20 and 0.50; medium between 0.50 and 0.80; and large >0.80 (56). SMD is the difference in means between the online intervention and comparison groups divided by the pooled SD of both groups. A positive effect size means that the intervention group outperformed the control group in improving mental health.
A three-level meta-analysis was used since the mental health outcomes were measured using several instruments (in the same study) (57). For each effect size, Level 1 reflects the sampling variance. The variance between the effect sizes within a study was assumed to be at Level 2. Level 3 illustrates the variation in effect sizes among the studies. By fitting meta-analysis models without an intercept, we quantified the extent of the intervention effect. Statistical analysis was performed to examine the variables, both within and between studies (58).
The I2 statistic was used to quantify heterogeneity. This statistic indicates the percentage of observed variance (I2 = 0 indicates no heterogeneity; I2 = 25 indicates low heterogeneity; I2 = 50 indicates a medium heterogeneity; I2 = 75 indicates a high heterogeneity) (59). Because a basic assumption of publication bias test (e.g., funnel plots, Egger's test) is the independence of effect sizes, we were unable to assess publication bias for this meta-analysis. The conventional test of publication bias was not applicable since we included all relevant effect estimates from each study (60).
Quality Assessment
The quality of the studies was determined by using the Cochrane Collaboration's risk of bias RoB 2.0 tool to calculate the risk of bias (ROB) in randomized trials. ROB was assessed across five domains (52). Each of the five domains was assigned a low or high risk of bias as well as some concern risks. Both authors individually examined the probability of ROB, with any disagreements being discussed. The kappa coefficient was used to determine the inter-rater agreement between the authors (50).
Results
Included Studies
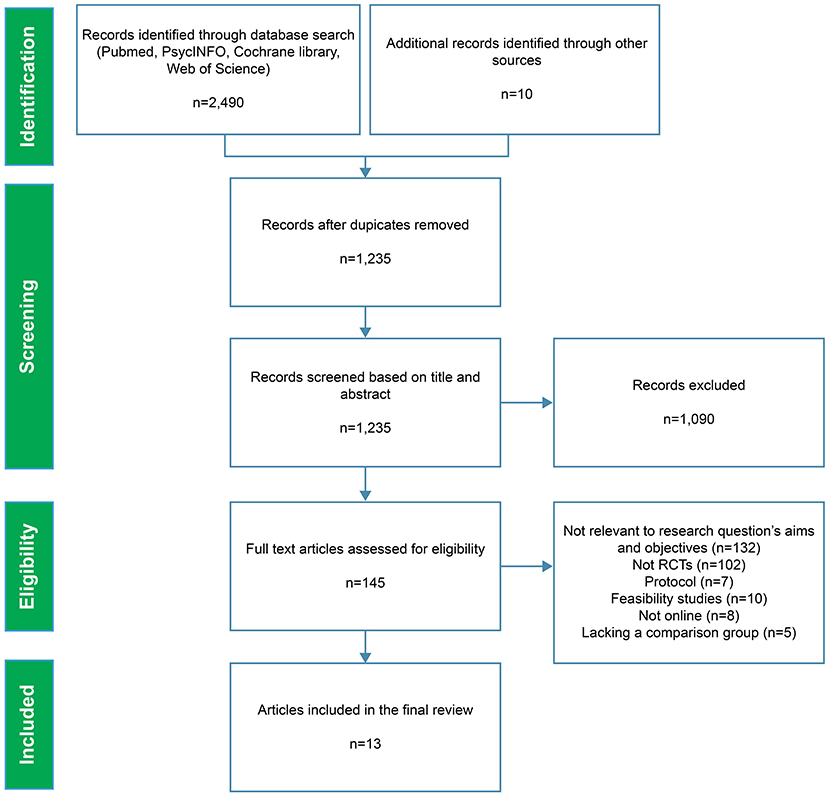
The PRISMA flow diagram is shown in Figure 1. The search yielded 2,490 papers, with ten additional records discovered by reviewing the references of the systematic reviews that were included, and 1,265 duplicates were excluded. The remaining studies (n = 1,235) were screened using the keywords in titles and abstracts, which eliminated 1,090 more studies. The full text of the remaining 145 studies was then evaluated, with 132 studies being eliminated for the following reasons: 102 studies were not RCTs; 17 studies dealt with protocols, usability, or feasibility; eight studies did not deliver online; five studies did not have a control group or a comparison intervention. Finally, 13 studies were included in this systematic review.
Systematic Review
Sample Description
All online interventions for PAYA cancer survivors that were included focused on multiple cancer types. The sample sizes ranged from 38 to 150 subjects (M = 71.85, SD = 37.73). Participants' mean age ranged from 10.6 to 44.1 (M = 23.73, SD = 9.30). Most studies (n = 11) were developed in the US, and the rest in China and Australia. We found that 46.2% of the studies aimed at PAYA cancer survivors' general mental health prevention (n = 6) (61–66). In contrast, 53.8% of the studies focused on the participants' physical health (n = 7) (67–73), including physical activity enhancement (n = 5; 38.5%) (68, 69, 71–73), sleep (n = 1; 7.7%) (70), and chronic pain (n = 1; 7.7%) (67). Finally, we found a dropout rate of 1.5–40%, with a mean of 15.65% (SD = 13.21).
Study Characteristics
Table 1 lists the characteristics (e.g., age, format, outcomes) of the included studies. Online intervention for childhood, adolescent, and young adult cancer survivors was compared to an alternative treatment (n = 7; 53.8%), a treatment as usual (n = 3; 23.1%), and a waiting list (n = 3; 23.1%). Almost all interventions were primarily self-directed, with or without minimal therapist support. Therapist-led interventions (n = 1) were compared to an alternative treatment in one study (66). The majority of the studies (n = 10) were two-arm randomized trials, with three being three-arm randomized trials. The first three-arm randomized trial compares the two online interventions to an alternative treatment. The second compares online intervention to a waiting list as well as an alternative treatment. The final one compares online intervention with two alternative treatments. Among the included studies, 76.9% (n = 10) show two measurement time points of the outcomes (baseline and post-test), whereas 23.1% (n = 3) have at least one additional follow-up assessment.
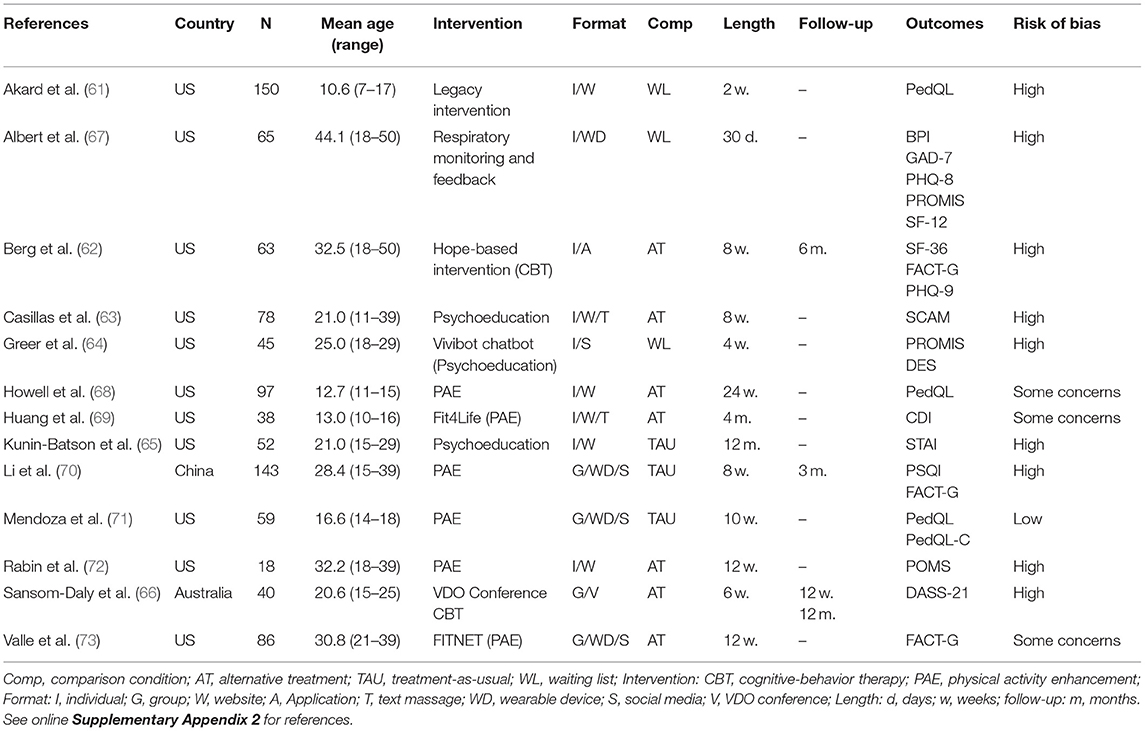
Table 1. Characteristics of online interventions for pediatric, adolescent, and young adult cancer survivors.
Intervention Characteristics
In total, 46.2% (n = 6) of the studies used psychological interventions (e.g., psycho-education, CBT, and legacy intervention) to improve mental health. Another six studies (n = 6) provided a physical activity enhancement program, while another study provided respiratory monitoring and feedback (n = 1). The median treatment duration was 8 weeks. Psychoeducation took an average of 8 weeks (SD = 3.3), CBT took 7 weeks (SD = 1), and physical activity enhancement programs took 13 weeks (SD = 5.2).
In total, 69.2% (n = 9) of the included studies used an individual online delivery format. Most of the interventions (n = 6) used a web-based intervention, two studies (n = 2) used web-based intervention with additional text messages, and four studies (n = 4) used web-based intervention without interactive contact. One study (n = 1) used a mobile application, one (n = 1) used a wearable respiratory monitoring device, and one (n = 1) used a social media chatbot. The other studies (n = 4) had a group online format that used wearable devices with social media (n = 3) and videoconferences (n = 1). In total, 76.9% (n = 10) of the trials were self-administered, whereas 23.1% (n = 3) included therapist support via videoconference (n = 1) and phone calls (n = 2).
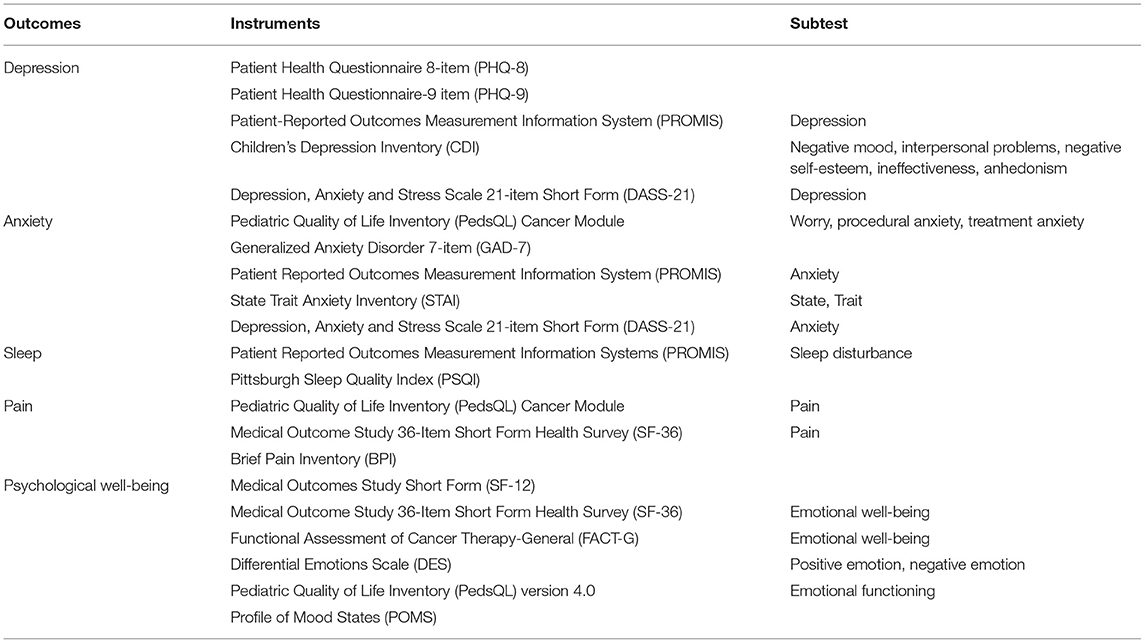
Outcome Measured
We found some diversity in the measures used to assess online interventions for mental health effects. Depression, anxiety, sleep, pain, and psychological well-being were all considered as mental health outcomes. For additional information, see Table 2. All 13 studies used self-reports to assess the effects of the intervention, using a variety of tools. One study considered both self-reported and parent-reported outcomes.
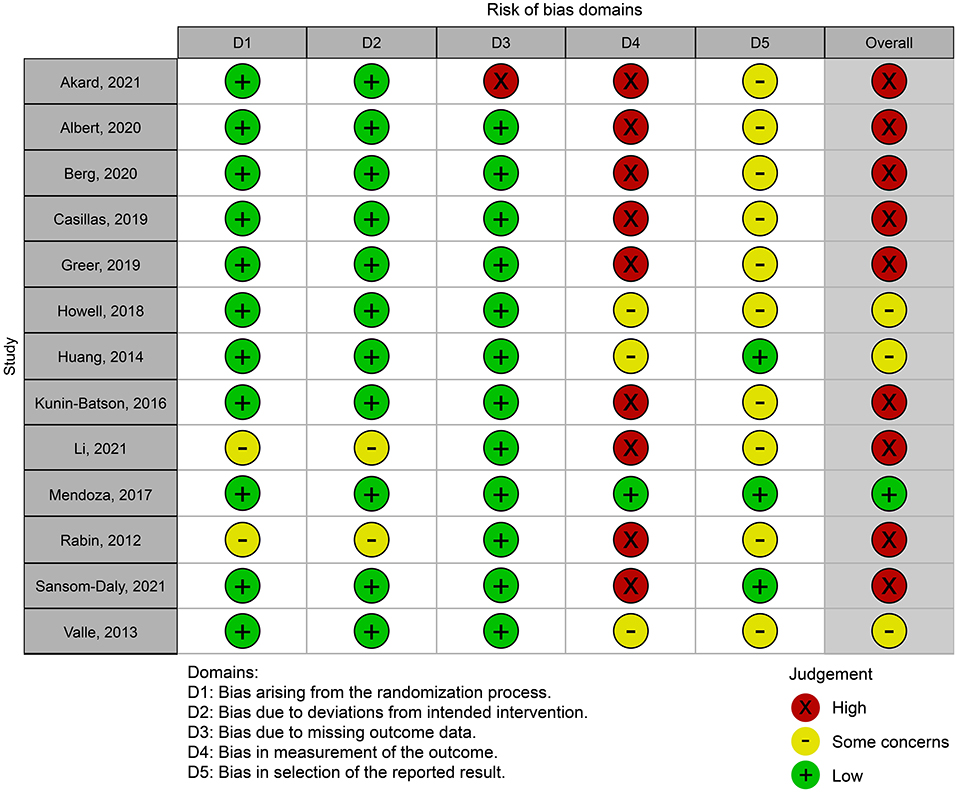
Risk of Bias
Figure 2 shows a summary of the authors' ROB judgments for each ROB domain. All included studies were found to have ROB. Kappa was 0.92 (p < 0.001), indicating good inter-evaluator agreement. Eleven studies were classified as having low ROB in the randomization procedure domain, while two were rated as having some concern. In the second domain, that is, deviations from intended interventions, 11 studies were rated as having a low ROB rating, while two were rated as having some concern. In the third domain, one study was classified as having a high ROB and missing outcome data, while the others were rated as having a low risk of bias. Only one study was judged as having a low risk of bias in the fourth area—assessment of the outcome—owing to the assessors' lack of blinding. Nine studies were rated as having high ROB, and three were rated as having some concerns. As only three studies had a pre-registered protocol, the fifth domain, selection of the reported results, was graded as having some bias concerns for the other ten studies.
Meta-Analyses
Primary Analysis
A primary analysis compared post-test means of PAYA's mental health outcomes for online intervention and control groups (n = 13, k = 37; see Figure 3). Only two comparators, g = 1.31 and g = 0.86, have a statistically significant positive effect size. The 95% CIs for the 35 comparators, including zero, indicated that no statistically significant difference was found between the intervention and control groups. Overall, the pooled effect size was small (g = 0.24, 95% CI 0.09–0.40) with low heterogeneity (I2 = 24%, Q = 47.34, p = 0.009). A statistically significant difference in favor of the intervention group was found (Z = 3.10, p = 0.002) (Figure 3).
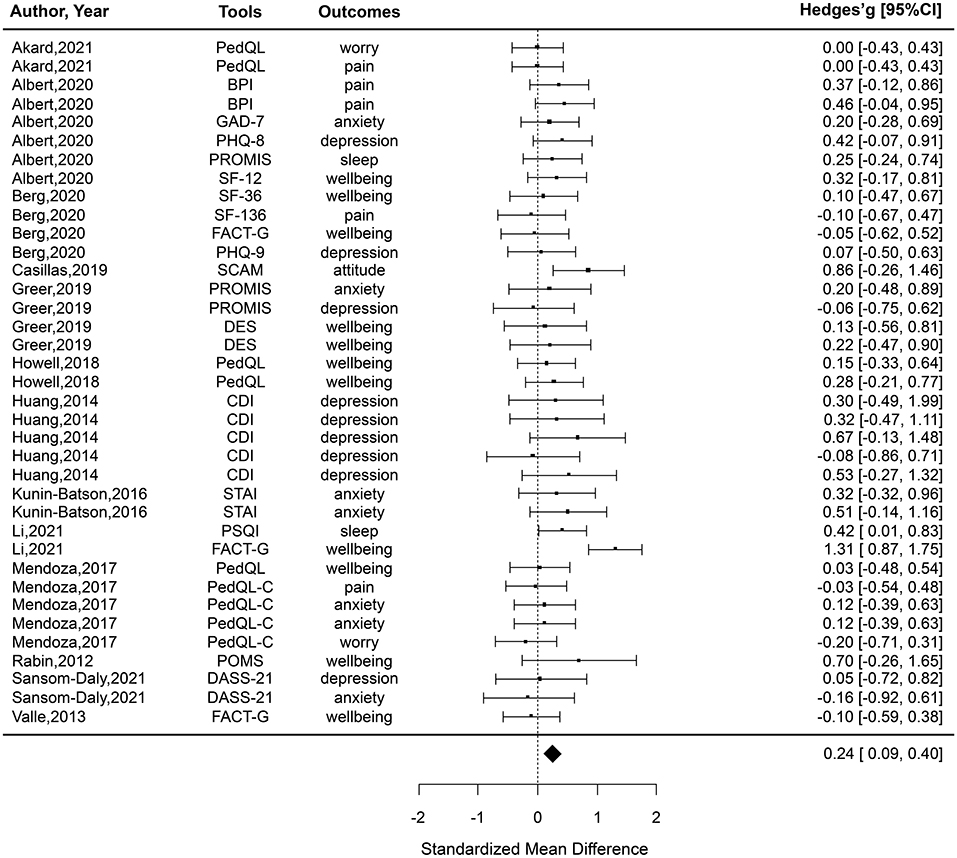
Figure 3. All effect sizes included in the meta-analysis from the studies comparing online interventions to a control group.
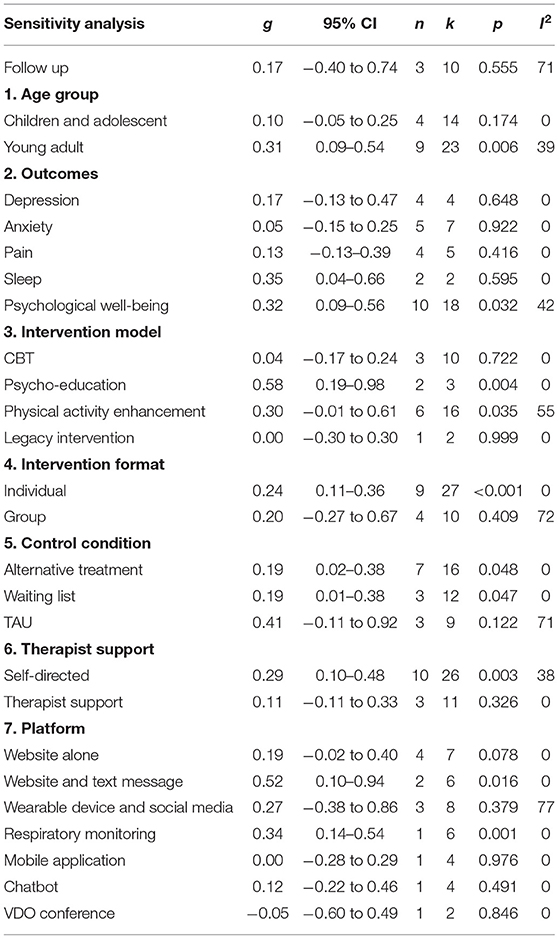
Analysis of Follow-Up Effectiveness
At the follow-up time points (n = 3, k = 10; Table 3), we examined the efficacy of the online interventions. The mean scores from the studies' follow-ups were used in this analysis. Two comparators from one study indicated that the intervention groups had statistically significant positive effect sizes ranging from 0.44 to 1.22. However, no statistically significant differences were found between the groups using the eight comparators. The pooled effect size was small (g = 0.17, 95% CI −0.40 to 0.74), with moderate heterogeneity (I2 = 71%) and a non-statistically significant difference (Z = 0.59, p = 0.555).
Sensitivity Analysis
Age Group
Young adult studies (mean age > 20 years) revealed a larger effect size (g = 0.31; 95% CI 0.09–0.54) compared to childhood and adolescence studies (g = 0.10; 95% CI −0.05 to 0.25).
Outcome
A sensitivity analysis was performed to test for variations in effect size between the intervention and control groups' post-treatment scores for depression (n = 4), anxiety (n = 5), pain (n = 4), sleep (n = 2), and psychological well-being (n = 10). When compared to studies that measured psychological well-being (g = 0.32; 95% CI 0.09–0.56), those that used sleep measures had a larger positive effect size (g = 0.35; 95% CI 0.04–0.66). Conversely, depression (g = 0.17; 95% CI −0.13 to 0.47), anxiety (g = 0.05; 95% CI −0.15 to 0.25), and pain (g = 0.13; 95 % CI −0.13 to 0.39) had no effect.
Intervention Model
A sensitivity analysis was carried out to test for differences in effect size among the intervention and control groups' post-treatment scores, according to the intervention model. Studies using psychoeducational interventions (n = 2, k = 3) reported a medium effect size (g = 0.58; 95% CI 0.19–0.98) with no heterogeneity (I2 = 0). However, CBT (n = 3), physical activity enhancement (n = 6), and legacy intervention (n = 1) demonstrated a non-significant overall effect with low to medium heterogeneity (I2 = 0–55).
Intervention Format
A sensitivity analysis was conducted to determine whether the effect size of post-treatment effects varied between studies with individual (n = 9) and group interventions (n = 4). Individual intervention studies had a small effect size (g = 0.24, 95% CI 0.11–0.36). There was no statistically significant difference in the overall effect size of group intervention between the intervention and control groups (g = 0.20; 95% CI: −0.27 to 0.67) with medium heterogeneity (I2 = 72).
Control Condition
A sensitivity analysis was conducted to determine whether the effect size of post-treatment effects varied between studies with alternative treatment (n = 7), waiting list (n = 3), and treatment as usual (n = 3). Although the biggest effect size is reported for studies comparing treatment-as-usual (g = 0.41; 95% CI −0.11–0.92) to alternative treatment (g = 0.19; 95% CI 0.02–0.38) and waiting list (g = 0.19; 95% CI 0.01–0.38), this subgroup demonstrates no effect.
Therapist Support
A sensitivity analysis was conducted to test whether the effect sizes between the intervention and control group's post-treatment scores varied when the intervention group received therapist support. The positive effect size in the self-directed intervention studies was small (g = 0.29; 95% CI 0.10–0.48). Nonetheless, no effect was shown when therapist support was used (g = 0.11; 95% CI −0.11 to 0.33).
Platform
A sensitivity analysis was performed to determine the effect size differences between the intervention and control group post-treatment ratings when using an online platform. A medium effect size (g = 0.52; 95% CI 0.10–0.54) with no heterogeneity (I2 = 0) was found in the studies using websites with text messages (n = 2), while no effects were found for studies that only used websites (g = 0.19; 95% CI −0.02 to 0.40). A small effect size (g = 0.34; 95% CI 0.14–0.54) was found in the studies using respiratory monitoring (n = 1). No effects were found for studies that used wearable devices and social media (g = 0.27; 95% CI −0.38 to 0.86), mobile application (g = 0.00; 95% CI −0.28 to 0.29), chatbots (g = 0.12; 95% CI −0.22 to 0.46), and VDO conferences (g = −0.05; 95% CI −0.60 to 0.49).
Continuous Moderators (Meta-Regression)
The participants' mean age (slope = 0.007, p = 0.417), duration of intervention (slope = 0.01, p = 0.483), dropout rate (slope = −0.01, p = 0.18), and ROB (slope = −0.03, p = 0.20) had no effect on the mental health outcomes.
Discussion
While psychosocial interventions have been recommended to improve the mental health of PAYA cancer survivors (18), few patients obtain them (31). Online interventions are a viable way to broaden access to psychosocial interventions, and trials that support their effectiveness have been published (47–49). The present study conducts a meta-analysis to investigate how online interventions improve the mental health of PAYA cancer survivors. Thirteen studies with a total sample size of 934 participants were included in the total search results. The findings indicate small effect sizes for online intervention groups, with statistically significant differences from control groups, implying that online interventions can improve the mental health of PAYA cancer survivors.
The current findings match and extend the findings of an earlier meta-analysis on a technology-assisted intervention by Zhang et al. (48). However, the effect sizes of this previous meta-analysis were pooled across heterogeneous studies, with varied types of intervention (both online and offline technologies) and objectives (e.g., mental health, cancer knowledge, and distraction of intrusive treatment). In addition to Zhang et al.'s (48) inquiries, we examined the effectiveness of interventions for certain outcomes and intervention delivery methods. These findings have practical implications. Practitioners interacting with families of PAYA cancer survivors may be particularly interested in the efficacy of online therapies tailored specifically to minimize PAYAs' mental health problems.
We evaluated online interventions for PAYA cancer survivors across multiple outcome domains. Online interventions show a significantly small effect size for sleep and psychological well-being. However, the overall intervention effects for depression, anxiety, and pain were non-significant. This is concerning because these outcomes are critical for mental health care services for PAYA cancer survivors, which highlights the importance of developing different interventions to target these mental health symptoms for PAYA. Our findings on psychological well-being outcomes are consistent with previous meta-analyses, which found that a technology-assisted intervention improves psychological well-being (48) but not physical health (47, 48).
Nearly half of the online interventions provided physical activity enhancement as a core intervention model. However, physical activity enhancement demonstrated a non-significant effect on the improvement of PAYA's mental health. A previous meta-analysis showed that a distance-delivered physical activity intervention can improve only physical health-related quality of life but did not increase the physical activity (e.g., Moderate to vigorous physical activity; MVPA) of childhood cancer survivors (47). It can be assumed that enhancing physical and functional health using online interventions did not have a transfer effect on improving mental health.
Psychoeducation showed the greatest treatment effect sizes, while CBT-based interventions showed statistically non-significant effects. Assuming that an online CBT-based intervention cannot be didactic, PAYA cancer survivors may show poor engagement with these formats of interventions, resulting in suboptimal treatment outcomes (62). This demonstrates that it is critical for future research to focus on designing psychological interventions to improve engagement of PAYA cancer survivors.
This study found that the effects of treatment on mental health outcomes vary by age, within the PAYA age range. The effect sizes on mental health were lower in children and adolescent cancer survivors than in young adult cancer survivors. Despite the innovative approach, online intervention contents for adolescents remain insufficient, necessitating the ongoing clinical and research efforts to improve care and mental health outcomes for PAYA cancer survivors specifically. One possible explanation is that most interventions did not provide adolescent-specific materials (61, 63, 64, 68). As a result, online interventions do not adequately meet age-specific needs.
Self-directed or individual online interventions were no less effective than those with therapist support or group-delivered were; however, the small number of interventions may have hampered the detection of existing differences (53). These findings are consistent with those of another meta-analysis (30), which found that in-person and telehealth-involved therapies are equally beneficial for various mental health issues. However, in our findings, when the effect sizes for therapist-led online interventions were pooled across the three studies, and those for group-based online interventions were pooled across the four studies, these findings were inconclusive.
Combining websites with text messages in online interventions can lead to the highest effect on improving mental health outcomes (63, 69), while websites alone showed non-significant effects (61, 65, 68, 72). Despite the effect sizes for websites with text messages pooled across the two studies, a multiple platform (one study using websites with text messages and one using websites with text messages and phone calls) may increase the effect of online interventions; therefore, future studies are needed to confirm the benefit of multimodality online interventions. A novel technology such as wearable respiratory monitoring also showed a significant effect. However, further studies are needed to identify an effective delivery platform. As many interventions in this review used multiple delivery platforms, there is considerable scope to examine the impact of a different platform.
The effects of online interventions on mental health outcomes marginally diminished from posttest to follow-up, according to the follow-up assessments. However, because the effect sizes were aggregated over four investigations, these findings should be interpreted with caution. Although our findings show that the effects wane over time, more research is needed to provide a more detailed explanation.
Clinical Implications
Although the overall effect of online interventions for improving the mental health of PAYA cancer survivors was promising, health care providers should consider that they are not effective for all outcomes, especially critical outcomes for the improvement of depression, anxiety, and pain. Recommendation for online interventions need to consider for the age group of patients as significant effect was found among interventions for young adults.
Study Limitations
The first limitation is the study's small sample size. Although Fu et al. (53) recommended a minimum number of studies (at least six for a meta-analysis and four for subgroup analyses of each group), more studies would provide the opportunity for subgroup analyses. As a result, sensitivity analyses were preferred for groups with fewer than four studies. However, if possible, subgroup analyses would have allowed for more specific identification of the intervention characteristics associated with intervention effects. Second, as only three RCTs had a pre-registered protocol, determining whether the data were reviewed according to a pre-defined method was difficult. Thus, practically every study was found to exhibit some amount of bias in the fifth area of RoB 2.0 selection of reported outcomes. Third, all but one study (parent reports) used self-reports to assess mental health outcomes. Therefore, the PAYA cancer survivors were aware of the examination, which may have influenced their mental health scores. Fourth, treatment effects for PAYA survivorship outcomes may differ by age/developmental stages within the PAYA age range. There was a lack of online interventions for children under the age of ten. Online intervention delivered by some delivery methods may be effective for young adults, but not feasible for younger children. The effectiveness of online interventions for children will be determined in future meta-analyses once sufficient papers have been published. Fifth, few studies compare online interventions to traditional interventions (e.g., group-based psychoeducation and in-person CBT). We were unable to determine the efficacy of online vs. traditional therapies on mental health outcomes.
Future Directions
Self-reports may overstate the effectiveness of interventions (74, 75); thus, future research should utilize more objective tools or parental reports. As mobile phones become the most frequent devices for connecting to the Internet (76), specially designed RCTs should investigate the efficacy of m-health interventions that include the functions of sending reminders, providing feedback, and monitoring (77). The most frequently cited advantage of online interventions is their accessibility (78). Although we discovered that online interventions improve PAYAs' mental health, the pooled effect size was small. Therefore, future studies should find innovative strategies to improve their effectiveness. More studies should compare self-directed online interventions with those provided face-to-face or by videoconference to gain a better understanding of which online interventions are more beneficial. Finally, while this study's objective was not to investigate the mechanisms of change, our findings are consistent with the fundamental assumptions of cancer psychological interventions, which state that increasing cancer knowledge, physical health, and self-efficacy can improve mental health outcomes (79). Future meta-analytic approaches may use a novel methodology, such as meta-analytic structural equation modeling, to provide definitive answers on this subject (80, 81). Thus, it is feasible to evaluate whether gains in physical health, cancer knowledge, psychological skills (CBT or relaxation), or self-efficacy influence the effect of therapies on mental health outcomes.
Conclusions
Online interventions are effective in improving the mental health outcomes of PAYA cancer survivors. The present study contributes to the body of knowledge offered by prior meta-analyses. Online interventions were found to be effective for sleep and psychological well-being but not for depression, anxiety, or pain. The small number of studies found to be eligible for this meta-analysis, the paucity of RCTs using pre-registered protocols, and outcome measurement dependent on self-reports are all key limitations. Future studies should design more effective interventions targeted at areas related to depression, anxiety, or pain.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
NC and TT contributed to the design and implementation of the research, to the analysis of the results, and to the writing of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We acknowledge all authors that provided an RCTs included in this study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.784615/full#supplementary-material
References
1. Suh E, Stratton KL, Leisenring WM, Nathan PC, Ford JS, Freyer DR, et al. Late mortality and chronic health conditions in long-term survivors of early-adolescent and young adult cancers: a retrospective cohort analysis from the childhood cancer survivor study. Lancet Oncol. (2020) 21:421–35. doi: 10.1016/S1470-2045(19)30800-9
2. Robison LL, Hudson MM. Survivors of childhood and adolescent cancer: life-long risks and responsibilities. Nat Rev Cancer. (2014) 14:61–70. doi: 10.1038/nrc3634
3. Miller KD, Fidler-Benaoudia M, Keegan TH, Hipp HS, Jemal A, Siegel RL. Cancer statistics for adolescents and young adults, 2020. CA Cancer J Clin. (2020) 70:443–59. doi: 10.3322/caac.21637
4. Centers for Disease Control and Prevention, Department of Health and Human Services & Lance Armstrong Foundation. A National Action Plan for Cancer Survivorship: Advancing Public Health Strategies. (2004). p. 3–4.
5. Barnett M, McDonnell G, DeRosa A, Schuler T, Philip E, Peterson L, et al. Psychosocial outcomes and interventions among cancer survivors diagnosed during adolescence and young adulthood (AYA): a systematic review. J Cancer Surviv. (2016) 10:814–31. doi: 10.1007/s11764-016-0527-6
6. Bleyer WA. Cancer in older adolescents and young adults: epidemiology, diagnosis, treatment, survival, and importance of clinical trials. Med Pediatr Oncol. (2002) 38:1–10. doi: 10.1002/mpo.1257
7. Thongseiratch T, Chandeying N. Chronic illnesses and student academic performance. J Health Sci Med Res. (2020) 38:245–53. doi: 10.31584/jhsmr.2020738
8. Jin Z, Griffith MA, Rosenthal AC. Identifying and meeting the needs of adolescents and young adults with cancer. Curr Oncol Rep. (2021) 23:17. doi: 10.1007/s11912-020-01011-9
9. D'Souza AM, Devine KA, Reiter-Purtill J, Gerhardt CA, Vannatta K, Noll RB. Internalizing symptoms in AYA survivors of childhood cancer and matched comparisons. Psychooncology. (2019) 28:2009–16. doi: 10.1002/pon.5183
10. Geue K, Brähler E, Faller H, Härter M, Schulz H, Weis J, et al. Prevalence of mental disorders and psychosocial distress in German adolescent and young adult cancer patients (AYA). Psychooncology. (2018) 27:1802–9. doi: 10.1002/pon.4730
11. Ljungman L, Hovén E, Ljungman G, Cernvall M, von Essen L. Does time heal all wounds? A longitudinal study of the development of posttraumatic stress symptoms in parents of survivors of childhood cancer and bereaved parents. Psychooncology. (2015) 24:1792–8. doi: 10.1002/pon.3856
12. Liu W, Cheung YT, Brinkman TM, Banerjee P, Srivastava D, Nolan VG, et al. Behavioral symptoms and psychiatric disorders in child and adolescent long-term survivors of childhood acute lymphoblastic leukemia treated with chemotherapy only. Psychooncology. (2018) 27:1597–607. doi: 10.1002/pon.4699
13. Bitsko MJ, Cohen D, Dillon R, Harvey J, Krull K, Klosky JL. Psychosocial late effects in pediatric cancer survivors: a report from the children's oncology group. Pediatr Blood Cancer. (2016) 63:337–43. doi: 10.1002/pbc.25773
14. Friend AJ, Feltbower RG, Hughes EJ, Dye KP, Glaser AW. Mental health of long-term survivors of childhood and young adult cancer: a systematic review. Int J Cancer. (2018) 143:1279–86. doi: 10.1002/ijc.31337
15. Szalda D, Pierce L, Hobbie W, Ginsberg JP, Brumley L, Wasik M, et al. Engagement and experience with cancer-related follow-up care among young adult survivors of childhood cancer after transfer to adult care. J Cancer Surviv. (2016) 10:342–50. doi: 10.1007/s11764-015-0480-9
16. Otth M, Denzler S, Koenig C, Koehler H, Scheinemann K. Transition from pediatric to adult follow-up care in childhood cancer survivors-a systematic review. J Cancer Surviv. (2021) 15:151–62. doi: 10.1007/s11764-020-00920-9
17. Hart RI, Cowie FJ, Jesudason AB, Lawton J. Adolescents and young adults' (AYA) views on their cancer knowledge prior to diagnosis: findings from a qualitative study involving AYA receiving cancer care. Health Expect. (2021) 24:307–16. doi: 10.1111/hex.13170
18. Richter D, Koehler M, Friedrich M, Hilgendorf I, Mehnert A, Weißflog G. Psychosocial interventions for adolescents and young adult cancer patients: a systematic review and meta-analysis. Crit Rev Oncol Hematol. (2015) 95:370–86. doi: 10.1016/j.critrevonc.2015.04.003
19. Bradford NK, Chan RJ. Health promotion and psychological interventions for adolescent and young adult cancer survivors: a systematic literature review. Cancer Treat Rev. (2017) 55:57–70. doi: 10.1016/j.ctrv.2017.02.011
20. Henderson TO, Friedman DL, Meadows AT. Childhood cancer survivors: transition to adult-focused risk-based care. Pediatrics. (2010) 126:129–36. doi: 10.1542/peds.2009-2802
21. Foster C, Breckons M, Cotterell P, Barbosa D, Calman L, Corner J, et al. Cancer survivors' self-efficacy to self-manage in the year following primary treatment. J Cancer Surviv. (2015) 9:11–9. doi: 10.1007/s11764-014-0384-0
22. Lorig K, Sobel D, Ritter P, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Eff Clin Pract. (2001) 4:256–62.
23. Waldrop DP, O'Connor TL, Trabold N. “Waiting for the other shoe to drop:” distress and coping during and after treatment for breast cancer. J Psychosoc Oncol. (2011) 29:450–73.
24. Mehnert A, Hartung TJ, Friedrich M, Vehling S, Brähler E, Härter M, et al. One in two cancer patients is significantly distressed: Prevalence and indicators of distress. Psychooncology. (2018) 27:75–82. doi: 10.1002/pon.4464
25. Segal R, Zwaal C, Green E, Tomasone JR, Loblaw A, Petrella T. The exercise for people with cancer guideline development group exercise for people with cancer: a systematic review. Curr Oncol. (2017) 24:e290. doi: 10.3747/co.24.3519
26. Gilliam MB, Schwebel DC. Physical activity in child and adolescent cancer survivors: a review. Health Psychol Rev. (2013) 7:92–110. doi: 10.1080/17437199.2011.603641
27. Mustian KM, Cole CL, Lin PJ, Asare M, Fung C, Janelsins MC, et al. Exercise recommendations for the management of symptoms clusters resulting from cancer and cancer treatments. Semin Oncol Nurs. (2016) 32:383–93. doi: 10.1016/j.soncn.2016.09.002
28. Brown JC, Huedo-Medina TB, Pescatello LS, Ryan SM, Pescatello SM, Moker E, et al. The efficacy of exercise in reducing depressive symptoms among cancer survivors: a meta-analysis. PLoS ONE. (2012) 7:1. doi: 10.1371/journal.pone.0030955
29. Mustian KM, Alfano CM, Heckler C, Kleckner AS, Kleckner IR, Leach CR, et al. Comparison of pharmaceutical, psychological, and exercise treatments for cancer-related fatigue: a meta-analysis. JAMA Oncol. (2017) 3:961–8. doi: 10.1001/jamaoncol.2016.6914
30. Zhang A, Wang K, Zebrack B, Tan CY, Walling E, Chugh R. Psychosocial, behavioral, and supportive interventions for pediatric, adolescent, and young adult cancer survivors: a systematic review and meta-analysis. Crit Rev Oncol Hematol. (2021) 160:103291. doi: 10.1016/j.critrevonc.2021.103291
31. Sender L, Zabokrtsky KB. Adolescent and young adult patients with cancer: a milieu of unique features. Nat Rev Clin Oncol. (2015) 12:465–80. doi: 10.1038/nrclinonc.2015.92
32. Berg CJ, Stratton E, Esiashvili N, Mertens A. Young adult cancer survivors' experience with cancer treatment and follow-up care and perceptions of barriers to engaging in recommended care. J Cancer Educ. (2016) 31:430–42. doi: 10.1007/s13187-015-0853-9
33. Arroyave WD, Clipp EC, Miller PE, Jones LW, Ward DS, Bonner MJ, et al. Childhood cancer survivors' perceived barriers to improving exercise and dietary behaviors. Oncol Nurs Forum. (2008) 35:121–30. doi: 10.1188/08.ONF.121-130
34. Sim JA, Yun YH, Yoo SH. Barriers to improving awareness of the importance on exercise and dietary intervention, impact of it on lung cancer survivors' behavior. Ann Oncol. (2017) 28:556. doi: 10.1093/annonc/mdx388.036
35. Ramsey WA, Heidelberg RE, Gilbert AM, Heneghan MB, Badawy SM, Alberts NM. eHealth and mHealth interventions in pediatric cancer: a systematic review of interventions across the cancer continuum. Psychooncology. (2020) 29:17–37. doi: 10.1002/pon.5280
36. Devine KA, Viola AS, Coups EJ, Wu YP. Digital health interventions for adolescent and young adult cancer survivors. JCO Clin Cancer Inform. (2018) 2:1–15. doi: 10.1200/CCI.17.00138
37. Viola A, Panigrahi G, Devine KA. Digital interventions for adolescent and young adult cancer survivors. Curr Opin Support Palliat Care. (2020) 14:51–9. doi: 10.1097/SPC.0000000000000480
38. Bradbury K, Steele M, Corbett T, Geraghty AWA, Krusche A, Heber E, et al. Developing a digital intervention for cancer survivors: an evidence-, theory- and person-based approach. NPJ Digit Med. (2019) 2:85. doi: 10.1038/s41746-019-0163-4
39. Tonorezos ES, Barnea D, Cohn RJ, Cypriano MS, Fresneau BC, Haupt R, et al. Models of care for survivors of childhood cancer from across the globe: advancing survivorship care in the next decade. J Clin Oncol. (2018) 36:2223–30. doi: 10.1200/JCO.2017.76.5180
40. Heirs M, Suekarran S, Slack R, Light K, Gibson F, Glaser A, et al. A systematic review of models of care for the follow-up of childhood cancer survivors. PediatrBlood Cancer. (2013) 60:351–6. doi: 10.1002/pbc.24253
41. Harrer M, Adam SH, Baumeister H, Cuijpers P, Karyotaki E, Auerbach RP, et al. Internet interventions for mental health in university students: a systematic review and meta-analysis. Int J Methods Psychiatr Res. (2019) 28:e1759. doi: 10.1002/mpr.1759
42. Harrer M, Adam SH, Fleischmann RJ, Baumeister H, Auerbach R, Bruffaerts R, et al. Effectiveness of an Internet- and app-based intervention for college students with elevated stress: randomized controlled trial. J Med Internet Res. (2018) 20:e136. doi: 10.2196/jmir.9293
43. Bolinski F, Kleiboer A, Karyotaki E, Bosmans JE, Zarski AC, Weisel KK, et al. Effectiveness of a transdiagnostic individually tailored Internet-based and mobile-supported intervention for the indicated prevention of depression and anxiety (ICare prevent) in Dutch college students: study protocol for a randomised controlled trial. Trials. (2018) 19:118. doi: 10.1186/s13063-018-2477-y
44. Weisel KK, Zarski AC, Berger T, Krieger T, Moser CT, Schaub MP, et al. User experience and effects of an individually tailored transdiagnostic Internet-based and mobile-supported intervention for anxiety disorders: mixed-methods study. J Med Internet Res. (2020) 22:e16450. doi: 10.2196/16450
45. Zhou ES, Recklitis CJ. Internet-delivered insomnia intervention improves sleep and quality of life for adolescent and young adult cancer survivors. Pediatr Blood Cancer. (2020) 67:e28506. doi: 10.1002/pbc.28506
46. Sansom-Daly UM, Wakefield CE, Bryant RA, Patterson P, Anazodo A, Butow P, et al. Recapture Life Working Party. Feasibility, acceptability, and safety of the Recapture Life videoconferencing intervention for adolescent and young adult cancer survivors. Psychooncology. (2019) 28:284–92. doi: 10.1002/pon.4938
47. Mizrahi D, Wakefield CE, Fardell JE, Quinn VF, Lim Q, Clifford BK, et al. Distance-delivered physical activity interventions for childhood cancer survivors: a systematic review and meta-analysis. Crit Rev Oncol Hematol. (2017) 118:27–41. doi: 10.1016/j.critrevonc.2017.08.008
48. Zhang A, Zebrack B, Acquati C, Roth M, Levin NJ, Wang K, et al. Technology-assisted psychosocial interventions for childhood, adolescent, and young adult cancer survivors: a systematic review and meta-analysis. J Adolesc Young Adult Oncol. (2021). doi: 10.1089/jayao.2021.0012
49. Hong HC, Min A, Kim YM. The effectiveness of digital self-management interventions on health outcomes among childhood cancer survivors: a systematic review and meta-analysis. J Adv Nurs. (2021) 77. doi: 10.1111/jan.14925
50. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 72:n71. doi: 10.1136/bmj.n71
51. Sackett DL, Rosenberg WMC, Gray JAM, et al. Evidence based medicine: What it is and what it isn't. BMJ. (1996) 312:71–2. doi: 10.1136/bmj.312.7023.71
52. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Method. (2010) 1:97–111. doi: 10.1002/jrsm.12
53. Fu R, Gartlehner G, Grant M, Shamliyan T, Sedrakyan A, Wilt TJ, et al. Conducting quantitative synthesis when comparing medical interventions: AHRQ and the effective health care program. J Clin Epidemiol. (2011) 64:1187–97. doi: 10.1016/j.jclinepi.2010.08.010
54. Baker WL, Michael White C, Cappelleri JC, Kluger J, Coleman CI. Health Outcomes, Policy, and Economics (HOPE) Collaborative Group. Understanding heterogeneity in meta-analysis: the role of meta-regression. Int J Clin Pract. (2009) 63:1426–34. doi: 10.1111/j.1742-1241.2009.02168.x
55. Hedges LV. What are effect sizes and why do we need them? Child Dev Perspect. (2008) 2:167–71. doi: 10.1111/j.1750-8606.2008.00060.x
56. Lachenbruch PA. Cohen J. Statistical power analysis for the behavioral sciences (2nd ed). J Am Stat Assoc. (1989) 84:1096. doi: 10.2307/2290095
57. Van den Noortgate W, López-López JA, Marín-Martínez F, Sánchez-Meca J. Three-level meta-analysis of dependent effect sizes. Behav Res Methods. (2013) 45:576–94. doi: 10.3758/s13428-012-0261-6
58. Cheung MW. A guide to conducting a meta-analysis with non-independent effect sizes. Neuropsychol Rev. (2019) 29:387–96. doi: 10.1007/s11065-019-09415-6
59. Borenstein M, Higgins JPT, Hedges LV, Rothstein HR. Basics of meta-analysis: I2 is not an absolute measure of heterogeneity. Res Synth Methods. (2017) 8:5–18. doi: 10.1002/jrsm.1230
60. van Enst WA, Ochodo E, Scholten RJPM, Hooft L, Leeflang MM. Investigation of publication bias in meta-analyses of diagnostic test accuracy: a meta-epidemiological study. BMC Med Res Methodol. (2014) 14:70. doi: 10.1186/1471-2288-14-70
61. Akard TF, Dietrich MS, Friedman DL, Wray S, Gerhardt CA, Hendricks-Ferguson V, et al. Randomized clinical trial of a legacy intervention for quality of life in children with advanced cancer. J Palliat Med. (2021) 24:680–8. doi: 10.1089/jpm.2020.0139
62. Berg CJ, Vanderpool RC, Getachew B, Payne JB, Johnson MF, Sandridge Y, et al. A hope-based intervention to address disrupted goal pursuits and quality of life among young adult cancer survivors. J Cancer Educ. (2020) 35:1158–69. doi: 10.1007/s13187-019-01574-7
63. Casillas JN, Schwartz LF, Crespi CM, Ganz PA, Kahn KL, Stuber ML, et al. The use of mobile technology and peer navigation to promote adolescent and young adult (AYA) cancer survivorship care: results of a randomized controlled trial. J Cancer Surviv. (2019) 13:580–92. doi: 10.1007/s11764-019-00777-7
64. Greer S, Ramo D, Chang YJ, Fu M, Moskowitz J, Haritatos J. Use of the chatbot “Vivibot” to deliver positive psychology skills and promote well-being among young people after cancer treatment: randomized controlled feasibility trial. JMIR Mhealth Uhealth. (2019) 7:e15018. doi: 10.2196/15018
65. Kunin-Batson A, Steele J, Mertens A, Neglia JP. A randomized controlled pilot trial of a Web-based resource to improve cancer knowledge in adolescent and young adult survivors of childhood cancer. Psychooncology. (2016) 25:1308–16. doi: 10.1002/pon.3956
66. Sansom-Daly UM, Wakefield CE, Ellis SJ, McGill BC, Donoghoe MW, Butow P, et al. Online, group-based psychological support for adolescent and young adult cancer survivors: results from the recapture life randomized trial. Cancers. (2021) 13:2460. doi: 10.3390/cancers13102460
67. Alberts NM, Leisenring WM, Flynn JS, Whitton J, Gibson TM, Jibb L, et al. Wearable respiratory monitoring and feedback for chronic pain in adult survivors of childhood cancer: a feasibility randomized controlled trial from the childhood cancer survivor study. Clin Cancer Inform. (2020) 4:1014–26. doi: 10.1200/CCI.20.00070
68. Howell CR, Krull KR, Partin RE, Kadan-Lottick NS, Robison LL, Hudson MM, et al. Randomized web-based physical activity intervention in adolescent survivors of childhood cancer. Pediatr Blood Cancer. (2018) 65:e27216. doi: 10.1002/pbc.27216
69. Huang JS, Dillon L, Terrones L, Schubert L, Roberts W, Finklestein J, et al. Fit4Life: a weight loss intervention for children who have survived childhood leukemia. Pediatr Blood Cancer. (2014) 61:894–900. doi: 10.1002/pbc.24937
70. Li L, Wang L, Sun Q, Xiao P, Duan Y, Liu X, et al. Effect of two interventions on sleep quality for adolescent and young adult cancer survivors: a pilot randomized controlled trial. Cancer Nurs. (2021). doi: 10.1097/NCC.0000000000000932
71. Mendoza JA, Baker KS, Moreno MA, Whitlock K, Abbey-Lambertz M, Waite A, et al. A Fitbit and Facebook mHealth intervention for promoting physical activity among adolescent and young adult childhood cancer survivors: a pilot study. Pediatr Blood Cancer. (2017) 64. doi: 10.1002/pbc.26660
72. Rabin C, Dunsiger S, Ness KK, Marcus BH. Internet-based physical activity intervention targeting young adult cancer survivors. J Adolesc Young Adult Oncol. (2011) 1:188–94. doi: 10.1089/jayao.2011.0040
73. Valle CG, Tate DF, Mayer DK, Allicock M, Cai J. A randomized trial of a Facebook-based physical activity intervention for young adult cancer survivors. J Cancer Surviv. (2013) 7:355–68. doi: 10.1007/s11764-013-0279-5
74. Zlotnik S, Toglia J. Measuring adolescent self-awareness and accuracy using a performance-based assessment and parental report. Front Public Health. (2018) 6:15. doi: 10.3389/fpubh.2018.00015
75. Stedal K, Dahlgren CL. Neuropsychological assessment in adolescents with anorexia nervosa - exploring the relationship between self-report and performance-based testing. J Eat Disord. (2015) 3:27. doi: 10.1186/s40337-015-0062-2
76. Vilkomir S. Multi-device coverage testing of mobile applications. Software Qual J. (2018) 26:197–215. doi: 10.1007/s11219-017-9357-7
77. Thongseiratch T, Leijten P, Melendez-Torres G. Online parent programs for children's behavioral problems: a meta-analytic review. Eur Child Adolesc Psychiatry. (2020) 29:1555–68. doi: 10.1007/s00787-020-01472-0
78. Davies F, Shepherd HL, Beatty L, Clark B, Butow P, Shaw J. Implementing web-based therapy in routine mental health care: systematic review of health professionals' perspectives. J Med Internet Res. (2020) 22:e17362. doi: 10.2196/17362
79. Austin JD, Allicock M, Atem F, Lee SC, Fernandez ME, Balasubramanian BA, et al. structural equation modeling approach to understanding pathways linking survivorship care plans to survivor-level outcomes. J Cancer Surviv. (2020) 14:834–46. doi: 10.1007/s11764-020-00896-6
80. Cheung MW, Chan W. Meta-analytic structural equation modeling: a two-stage approach. Psychol Methods. (2005) 10:40–64. doi: 10.1037/1082-989X.10.1.40
Keywords: cancer survivors, online, internet, AYA, pediatric, children, mental health
Citation: Chandeying N and Thongseiratch T (2021) Online Interventions to Improve Mental Health of Pediatric, Adolescent, and Young Adult Cancer Survivors: A Systematic Review and Meta-Analysis. Front. Psychiatry 12:784615. doi: 10.3389/fpsyt.2021.784615
Received: 28 September 2021; Accepted: 03 December 2021;
Published: 23 December 2021.
Edited by:
Pedro Gamito, Universidade Lusófona, PortugalReviewed by:
Ka Yan Ho, Hong Kong Polytechnic University, Hong Kong SAR, ChinaLauren McGillivray, University of New South Wales, Australia
Copyright © 2021 Chandeying and Thongseiratch. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Therdpong Thongseiratch, ttherd@gmail.com
 Nutthaporn Chandeying1
Nutthaporn Chandeying1 Therdpong Thongseiratch
Therdpong Thongseiratch