- 1West China School of Medicine, Sichuan University, Chengdu, China
- 2Department of Nephrology, The Affiliated Hospital of Southwest Medical University, Luzhou, China
- 3Sichuan Clinical Research Center for Nephropathy, Luzhou, China
- 4Division of Nephrology, Department of Medicine, Affiliated Hospital of Zunyi Medical University, Zunyi, China
- 5Department of Nephrology, People's Hospital of Jianyang, Chengdu, China
- 6Division of Nephrology, Zigong Third People's Hospital, Zigong, China
- 7Division of Nephrology, Department of Medicine, West China Hospital of Sichuan University, Chengdu, China
Background: The outbreak of coronavirus disease 2019 (COVID-19) has attracted global attention. During the lockdown period of COVID-19, follow-up of many patients with chronic disease had been interrupted, which brought severe challenges to better management of their disease. This study aimed at exploring the change of illness, daily life, and psychological responses during the COVID-19 pandemic among chronic kidney disease (CKD) patients.
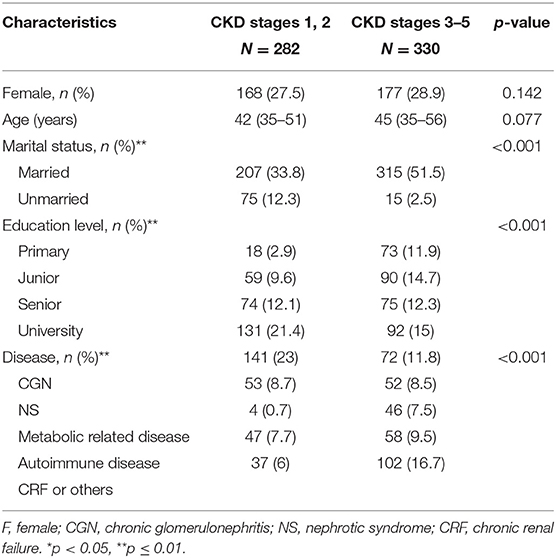
Methods: A total of 612 patients were enrolled in this study; 282 patients were categorized into the CKD stage 1–2 group and 330 patients were categorized into the CKD stage 3–5 group. Among two groups, 168 (27.5%) and 177 (28.9%) patients were female with a median age of 42 and 45, respectively. The study was conducted by collecting the questionnaires in five nephrology centers. The questionnaire consisted of assessment of anxiety by using the Self-Rating Anxiety Scale and the influences of COVID-19, which included basic demographic data, the influences of COVID-19 on illness and daily life, as well as the patients' psychological responses during the epidemic.
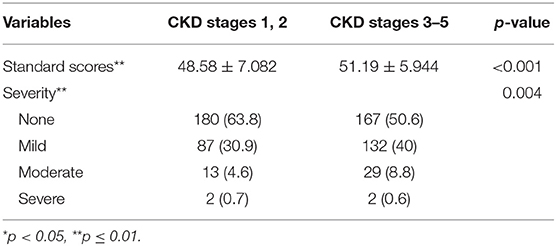
Results: A total of 612 patients were included and divided into two groups according to eGFR. Ninety-six patients (34%) in the CKD stage 1–2 group and 141 patients (42.7%) in the CKD stage 3–5 group had reduced their follow-up frequency (p = 0.031). More patients with CKD stages 1–2 consulted online (25.9%), p = 0.005. Besides, patients in the CKD stage 3–5 group tended to be more anxious about follow-up (p = 0.002), fearful of being infected with COVID-19 (p = 0.009), and more likely to feel symptoms getting worse (p = 0.006). The standard scores of SAS were 48.58 ± 7.082 and 51.19 ± 5.944 in the CKD stage 1–2 group and the CKD stage 3–5 group, respectively (p < 0.001). There were significant differences in the severity of anxiety (p = 0.004).
Conclusion: COVID-19 had a greater impact on patients with CKD stages 3–5 than those with stages 1–2 in terms of illness, daily life, and psychological disorder. Patients with CKD stages 3–5 were more anxious during the COVID-19 pandemic.
Introduction
Since December 2019, the outbreak of coronavirus disease 2019 (COVID-19) has attracted global attention (1, 2). In China and many other countries, governments have implemented several compulsory measures, such as quarantine, restriction of mass gatherings and events, business and school closures, and reduced frequency of transport, to mitigate the spread of COVID-19 (3, 4).
It is reported that chronic kidney disease (CKD) patients are more vulnerable to COVID-19 than the general population (5). COVID-19 infection could lead to high frequency of renal abnormalities, which not only included massive proteinuria and hematuria, but also elevated serum creatinine and blood urea nitrogen (6). What is more, CKD is associated with an increased risk of pneumonia, and the pneumonia-related mortality rate in CKD patients seems to be 14–16 times higher than in the general population (7). During the lockdown period, owing to the lack of personal protective equipment and limited transport, COVID-19 seems to pose a threat to the health of CKD patients in terms of follow-up and acquiring drugs. They are more anxious about their illness and whether they could use vaccines against COVID-19. Due to these factors, CKD patients are more likely to gain negative emotions. A latest study demonstrated that hemodialysis patients had more severe trauma-related stress symptoms than peritoneal dialysis patients (8).
However, there were few studies focused on CKD patients who did not enter the maintenance dialysis stage. The impact of COVID-19 on different stages of CKD patients and the potential problems remained unknown. This study aimed at analyzing the change of illness, daily life, and psychological responses during the COVID-19 pandemic among CKD patients.
Materials and Methods
Study Design and Data Collection
This study was performed in five nephrology centers (West China Hospital, Affiliated Hospital of Southwest Medical University, Affiliated Hospital of Zunyi Medical University, People's Hospital of Jianyang city, and Zigong Third People's Hospital) from June to August 2020. The inclusion criteria were as follows: (1) CKD patients without dialysis over 14 years of age; (2) the patients could communicate smoothly and use smartphones independently or with the help of their families to perform the questionnaires. Those who could not use smartphones, did not finish all questions, or were unwilling to answer the questionnaire were excluded. Informed consent was obtained before the data collection. By scanning a Quick Response code on WeChat, the patients could enter the Wenjuanxing platform to complete the questionnaire in the outpatient department of five study centers and our WeChat follow-up group of CKD patients. The study was in compliance with the Declaration of Helsinki and was approved by the ethical committee of West China Hospital of Sichuan University.
Composition of Questionnaire
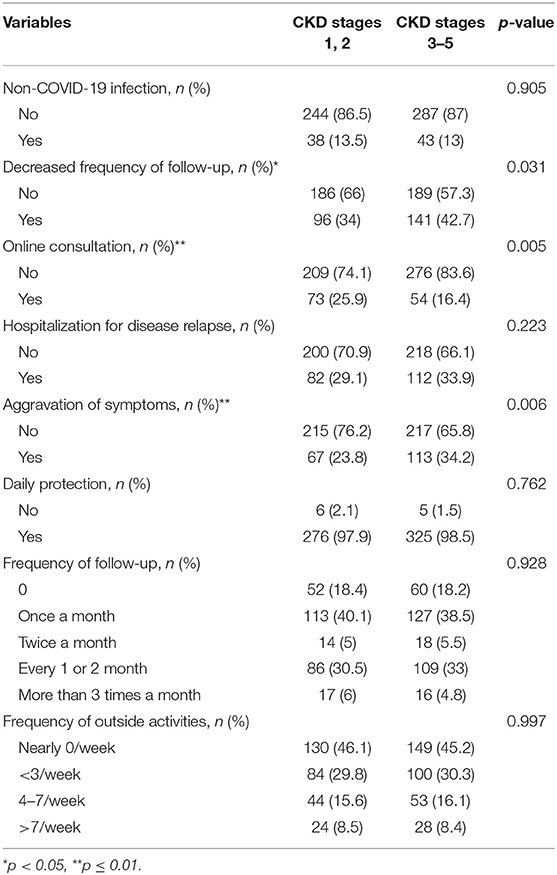
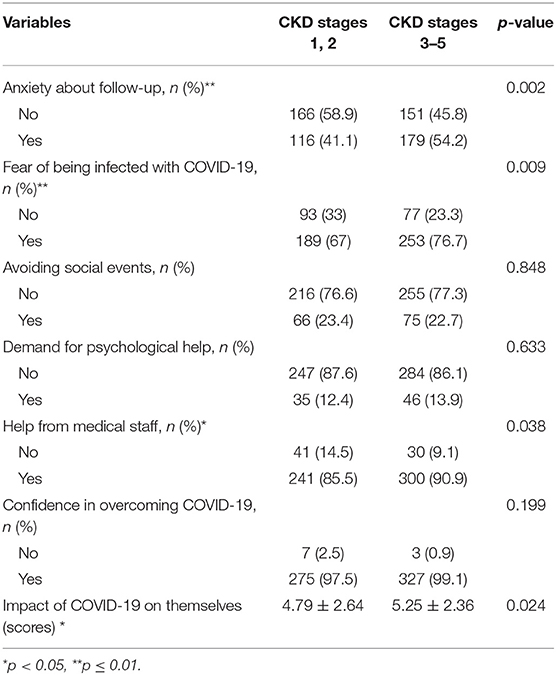
The questionnaire consisted of two main parts: the influences of COVID-19 and assessment of anxiety. The first part included (1) basic demographic data; (2) the influences of COVID-19 on the illness and daily life; (3) and their psychological responses during the epidemic. The impact of COVID-19 on patients was measured by scores according to different degrees, ranging from 0 to 10. (1) Basic demographic data included age, sex, marital status, education level, and primary disease (Table 1). (2) Influences of COVID-19 on the illness and daily life included the severity of clinical symptoms and signs (edema, fatigue, poor appetite, dizziness, joint pain, rash, foam urine, hematuria, and blood pressure), non-COVID-19 infection, hospitalization for disease relapse, the frequency of follow-up, online consultation (including telephone hotline or smartphone application), the frequency of outside activities, and awareness of daily protection (Table 2). (3) Psychological responses during the epidemic included the attitudes toward follow-up and COVID-19 and the demand for psychological help (Table 3).
Self-Rating Anxiety Scale
The second part of the questionnaire was the Self-Rating Anxiety Scale (SAS), a self-report scale developed by Zung (9), which was used to specifically measure anxiety symptoms. The questionnaire had 20 self-report questions and scored on a four-point Likert scale, which was according to the frequency of symptoms, ranging from 1 to 4. The standard cutoff scores were used to define the following: ≤50 as no anxiety; 50–59 as minimal to mild anxiety; 60–69 as moderate anxiety; and ≥70 scores as severe anxiety. The SAS (Chinese version) had been widely used and demonstrated adequate reliability and validity (10).
Statistical Analyses
Continuous variables were expressed as means ± SDs or medians (interquartile ranges). Categorical variables were expressed as number and percentages (%). Student's t-test or Mann–Whitney U test was used for continuous variables and χ2 test was used for categorical variables. The linear regression was used to examine the relationship between SAS scores and other variables. Then, the significant factors were further analyzed for SAS scores using multiple linear stepwise regression analysis. A two-tailed p < 0.05 was considered statistically significant. All statistical analysis was performed by using IBM SPSS statistics 26.0 software.
Results
Demographic Characteristics
In this study, 632 patients responded to the survey, and after removing 20 questionnaires for repeated or incomplete information, 612 patients were included. No patients were infected with COVID-19. Among them, 282 patients were categorized into the CKD stage 1–2 group and 330 patients were in the CKD stage 3–5 group.
There were no significant differences in sex and age between the two groups (Table 1). More patients with CKD stages 3–5 were married [207 patients (33.8%) in the CKD stage 1–2 group vs. 315 patients (51.5%) in the CKD stage 3–5 group, p < 0.001]. Patients with CKD stages 1–2 had a higher proportion of university degree (21.3%) and higher proportion of junior degree (14.7%) than in the group with CKD stages 3–5 (p < 0.001). The disease types of most patients with CKD stages 1–2 and stages 3–5 were chronic glomerulonephritis and chronic renal failure, respectively (p < 0.001, Table 1).
Comparisons of Illness and Daily Life Toward COVID-19
In this study, the frequency of follow-up during the pandemic did not show differences between two groups. However, it was notable that the difference in decreased frequency of follow-up was significant. Ninety-six patients (34%) in the CKD stage 1–2 group and 141 patients (42.7%) in the CKD stage 3–5 group had reduced their follow-up frequency (p = 0.031). It could be noticed that more patients with CKD stages 1–2 consulted online (25.9%, p = 0.005). Besides, more patients in the CKD stage 3–5 group tended to feel their symptoms getting worse (p = 0.006). There were also no significant differences in non-COVID-19 infection, awareness of daily protection, hospitalization for disease relapse, and the frequency of outside activities (Table 2).
Comparisons of Psychological Influences Toward COVID-19
Patients in the CKD stage 3–5 group felt more anxious about follow-up (p = 0.002) and more afraid of being infected with COVID-19 (p = 0.009). A total of 241 patients (85.5%) in the CKD stage 1–2 group and 300 patients (90.9%) in the CKD stage 3–5 group thought they had gained help from medical staff during the pandemic period (p = 0.038). The results of avoiding social events, demand for psychological help, confidence in overcoming COVID-19, and the impact of COVID-19 on themselves did not show differences between two groups (Table 3).
Comparisons of SAS Scores and the Severity of Anxiety
The standard scores of SAS were 48.58 ± 7.082 and 51.19 ± 5.944 in the CKD stage 1–2 group and the CKD stage 3–5 group, respectively (p < 0.001). There were significant differences in the severity of anxiety; about 36.2% of patients in the CKD stage 1–2 group and 49.4% of patients in the CKD stage 3–5 group had symptoms of anxiety, most of which were mild (p = 0.004) (Table 4).
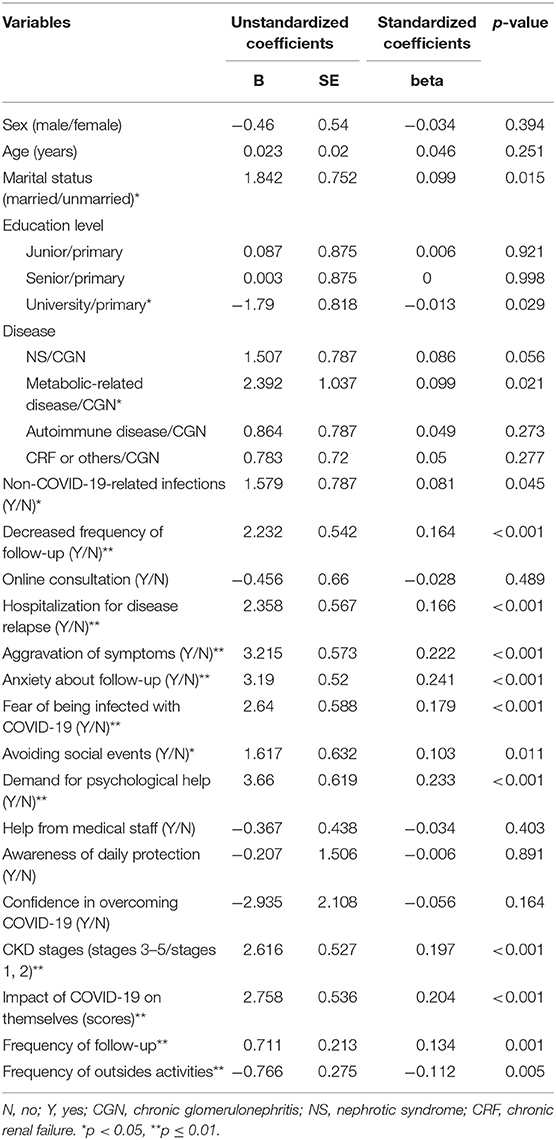
Univariate Analysis and Multivariate Analysis: Risk of SAS Scores
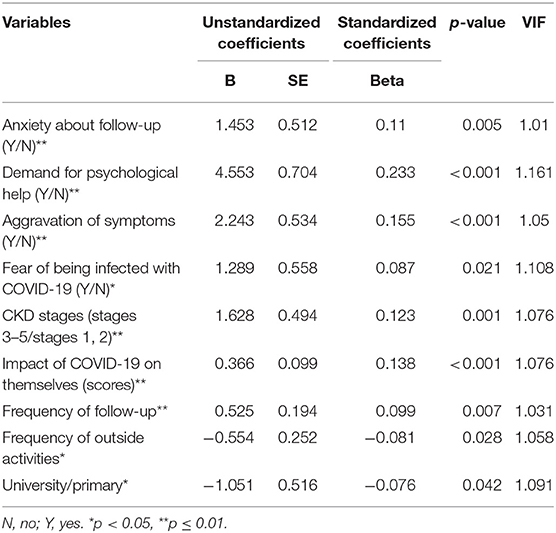
In the results of univariate analysis (Table 5), marital status (p = 0.015), university (p = 0.029), non-COVID-19 infection (p = 0.045), metabolic-related disease (p = 0.021), decreased frequency of follow-up (p < 0.001), hospitalization for disease relapse (p < 0.001), aggravation of symptoms (p < 0.001), anxiety about follow-up (p < 0.001), fear of being infected with COVID-19 (p < 0.001), avoiding social events (p = 0.011), demand for psychological help (p < 0.001), CKD stages (p < 0.001), the impact of COVID-19 on themselves (p < 0.001), the frequency of follow-up (p = 0.001), and the frequency of outside activities (p = 0.005) were chosen for the multiple linear stepwise regression model (Table 5). However, the multivariate analysis indicated that anxiety about follow-up (p = 0.005), demand for psychological help (p < 0.001), aggravation of symptoms (p < 0.001), fear of being infected with COVID-19 (p = 0.021), CKD stages (p = 0.001), the impact of COVID-19 on themselves (p < 0.001), university degree (p = 0.042), the frequency of follow-up (p = 0.007), and frequency of outside activities (p = 0.028) were associated with the severity of SAS independently (Table 6).
Discussion
In this study, we found that COVID-19 had a greater impact on patients with CKD stages 3–5 than on those with CKD stages 1–2 in terms of illness, daily life, and psychological disorder. In addition, patients with CKD stages 3–5 seemed more anxious. The COVID-19 pandemic has a strong impact on the lives and work of people all over the world. The whole society is under great pressure for unemployment, infection, being separated from family, death, and so on (11–13). For CKD patients, they often need regular follow-up in the hospital. However, during the lockdown period, they cannot visit the hospital on time, which brings difficulties in better controlling their disease and the adjustment of treatment. The epidemic poses a huge challenge to patients with CKD because they require frequent care and support, and these needs are still required during the pandemic (5). Some researchers had realized the unique challenges that kidney disease patients experienced during the COVID-19 pandemic. These patients may be at increased risk of infection or worse outcomes and were already facing obstacles in their routine medical care (14, 15).
In this study, we investigated the daily life, illness, and psychological responses of CKD patients during the COVID-19 pandemic. We found that there were significant differences in online consultation, aggravation of symptoms, fear of being infected with COVID-19, decreased frequency of follow-up, anxiety about follow-up, the impact of COVID-19 on themselves by self-scoring, and the help from medical staff between patients with CKD stages 1–2 and stages 3–5. We were surprised to observe that the median scores of SAS were not high in the whole included patients. The median scores of patients with CKD stages 1–2 and CKD stages 3–5 were 48.58 and 51.19, which represented normal and mild anxiety, respectively. Overall, most CKD patients could calmly handle the situation. Patients with CKD stages 3–5 seemed to be more anxious during this period.
Several reasons might lead to these differences between the two groups. The condition of patients with CKD stages 1–2 was relatively stable with simpler drug treatments, fewer complications, and slower progression of disease. However, the condition of patients with CKD stages 3–5 was more serious, with complications in most cases, and that was why they needed to visit the hospital more often. Owing to the usual higher frequency of follow-up of the CKD stage 3–5 patients, their decreased frequency of follow-up would be more apparent during the lockdown period.
During the epidemic, hospitals opened a special COVID-19 telephone hotline and smartphone application for online consultations, through which medical staff offered suggestions and interventions out of the hospital (16). It could reduce crowd gathering in offline hospitals (17). Especially for those who had mild symptoms, online doctors could give professional advice on self-management and treatment (18). Many hospitals began to offer internet-based drug prescription and delivery service for patients with common and chronic diseases (16). However, the illness of patients with CKD stages 3–5 tended to be more severe and some drugs could not be obtained online; for example, erythropoietin and insulin must be transported in low temperature, which was difficult to carry out. CKD patients with anemia or diabetes may not have good access to the needed drugs, which proved harmful to their condition. Furthermore, some special examination items could only be performed in the central hospitals, which could not be solved by online consultation. Consequently, it could not take the place of offline treatment completely. Also, patients with CKD stages 1–2 had a higher education level, which may make them more accustomed to using telephones for the new type of treatment. These were reasons why patients with CKD stages 3–5 had a lower proportion of online consultation. Better drug delivery system for some special drugs and improvements in more convenient ways to online access could contribute to the popularity of online consultation. A future area community lab center would be beneficial to patients with chronic disease for blood or other examination during an epidemic.
Besides, because of the lack of enough protective equipment, transportation inconvenience, and fear of being infected in the hospital, which was a high-risk area full of sick patients (19), patients with CKD stages 3–5 could be more anxious about follow-up in the hospital. Additionally, due to the more severe illness of these patients, they could easily feel their symptoms getting worse.
SAS was a norm-referenced screener with adequate reliability and validity, which had been shown to discriminate anxiety from mood disorders (20). All the reasons mentioned above may contribute to the higher scores of SAS in patients with CKD stages 3–5. The results of multivariate analysis indicated that CKD stage was one of the independent risk factors of SAS. Despite the fact that the impact of COVID-19 on patients themselves and the demand for psychological help had no statistical difference between the two groups, these factors were all positively associated with SAS. Education level and frequency of outside activities were negatively associated with SAS, which showed that patients with a university degree or higher frequency of outside activities were less likely to be anxious. Patients with a higher education level may know more proper ways of self-protection, which is helpful in facing the epidemic more calmly and rationally. In addition, patients had a higher frequency of outside activities mainly because they need better work, which often made them more adaptable in the society coexisting with the epidemic.
Actually, in some previous studies, researchers had realized that psychiatric disorders were common among the public during the 2003 SARS and 2014 Ebola virus outbreaks or other epidemics (21, 22). In 2016, it was reported that during the Middle East Respiratory Syndrome (MERS) pandemic, about 47.2% MERS patients had symptoms of anxiety and 52.8% had feelings of anger (23). Additionally, many studies concentrated on infected patients, the general population (24), frontline health and social care professionals (25), and students (26), and only few studies focused on patients with chronic disease. This study was the first to report on how CKD patients without dialysis reacted during the pandemic. To date, there are still many confirmed cases of COVID-19 worldwide. Our study might contribute to improving the management and treatment of CKD patients during the pandemic. Careful psychological assessment and sufficient mental support should be provided to more CKD patients, especially those with lower eGFR.
However, there were some limitations in our study. First, our data were collected in Sichuan province, which was not a high prevalence area. Second, there were no data about how CKD patients obtained drugs during the lockdown period. Third, some parts of the questionnaire were answered according to the patients' subjective perception, which may lack objectivity.
Conclusion
In conclusion, compared with patients with CKD stages 1–2, patients with CKD stages 3–5 were more affected in terms of illness, daily life, and psychological disorder during the COVID-19 pandemic. They seemed more anxious when confronted with such infectious diseases. More careful management of illness and mental support should be provided to CKD patients, especially those with lower eGFR.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethical Committee of West China Hospital of Sichuan University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
ZJ designed the study, collected data, performed statistical analyses, and wrote the manuscript. JL, LG, ZZ, DW, and LZ collected the data. JT collected the data and performed statistical analyses. WQ and YT designed the study and critically revised the work. All authors read and approved the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors thank all of the participants and attending physicians for their contributions.
References
1. Weiss P, Murdoch DR. Clinical course and mortality risk of severe COVID-19. Lancet. (2020) 395:1014–5. doi: 10.1016/S0140-6736(20)30633-4
2. Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. (2020) 324:782–93. doi: 10.1001/jama.2020.12839
3. Ebrahim SH, Ahmed QA, Gozzer E, Schlagenhauf P, Memish ZA. Covid-19 and community mitigation strategies in a pandemic. BMJ. (2020) 368:m1066. doi: 10.1136/bmj.m1066
4. Deng SQ, Peng HJ. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. J Clin Med. (2020) 9:575. doi: 10.3390/jcm9020575
5. Okoro RN. COVID-19 pandemic: The role of community pharmacists in chronic kidney disease management supportive care. Res Social Adm Pharm. (2021) 17:1925–8. doi: 10.1016/j.sapharm.2020.07.008
6. Naicker S, Yang CW, Hwang SJ, Liu BC, Chen JH, Jha V. The novel coronavirus 2019 epidemic and kidneys. Kidney Int. (2020) 97:824–8. doi: 10.1016/j.kint.2020.03.001
7. Henry BM, Lippi G. Chronic kidney disease is associated with severe coronavirus disease 2019 (COVID-19) infection. Int Urol Nephrol. (2020) 52:1193–4. doi: 10.1007/s11255-020-02451-9
8. Xia X, Wu X, Zhou X, Zang Z, Pu L, Li Z. Comparison of psychological distress and demand induced by covid-19 during the lockdown period in patients undergoing peritoneal dialysis and hemodialysis: a cross-section study in a tertiary hospital. Blood Purif . (2020) 1–9. doi: 10.1101/2020.04.13.20063099
9. Zung WW. A rating instrument for anxiety disorders. Psychosomatics. (1971) 12:371–9. doi: 10.1016/S0033-3182(71)71479-0
10. Ran MS, Gao R, Lin JX, Zhang TM, Chan SKW, Deng XP, et al. The impacts of COVID-19 outbreak on mental health in general population in different areas in China. Psychol Med. (2020) 1–10. doi: 10.1017/S0033291720004717
11. Lu Dong, Bouey J. Public mental health crisis during covid-19 pandemic, China. Emerg Infect Dis. (2020) 26:1616–8. doi: 10.3201/eid2607.202407
12. Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. (2020) 89:531–42. doi: 10.1016/j.bbi.2020.05.048
13. Rubin GJ, Wessely S. The psychological effects of quarantining a city. BMJ. (2020) 368:m313. doi: 10.1136/bmj.m313
14. Rabb H. Kidney diseases in the time of COVID-19: major challenges to patient care. J Clin Invest. (2020) 130:2749–51. doi: 10.1172/JCI138871
15. Riccio E, Rizzo M, Rossano R, Pisani A. Impact of COVID-19 pandemic on CKD outpatient management. Clin Nephrol. (2021) 95:112–4. doi: 10.5414/CN110343
16. Hong Z, Li N, Li D, Li J, Li B, Xiong W, et al. Telemedicine during the covid-19 pandemic: experiences from western China. J Med Internet Res. (2020) 22:e19577. doi: 10.2196/19577
17. Xie X, Zhou W, Lin L, Fan S, Lin F, Wang L, et al. Internet hospitals in China: cross-sectional survey. J Med Internet Res. (2017) 19:e239. doi: 10.2196/jmir.7854
18. Gong K, Xu Z, Cai Z, Chen Y, Wang Z. Internet hospitals help prevent and control the epidemic of COVID-19 in China: multicenter user profiling study. J Med Internet Res. (2020) 22:e18908. doi: 10.2196/18908
19. Zhang Z, Liu S, Xiang M, Li S, Zhao D, Huang C, et al. Protecting healthcare personnel from 2019-nCoV infection risks: lessons and suggestions. Front Med. (2020) 14:229–31. doi: 10.1007/s11684-020-0765-x
20. Dunstan DA, Scott N. Norms for zung's self-rating anxiety scale. BMC Psychiatry. (2020) 20:90. doi: 10.1186/s12888-019-2427-6
21. Mak IW, Chu CM, Pan PC, Yiu MG, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. (2009) 31:318–26. doi: 10.1016/j.genhosppsych.2009.03.001
22. Shultz JM, Cooper JL, Baingana F, Oquendo MA, Espinel Z, Althouse BM, et al. The role of fear-related behaviors in the 2013-2016 West Africa ebola virus disease outbreak. Curr Psychiatry Rep. (2016) 18:104. doi: 10.1007/s11920-016-0741-y
23. Jeong H, Yim HW, Song YJ, Ki M, Min JA, Cho J, et al. Mental health status of people isolated due to middle east respiratory syndrome. Epidemiol Health. (2016) 38:e2016048. doi: 10.4178/epih.e2016048
24. Wang Y, Kala MP, Jafar TH. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: a systematic review and meta-analysis. PLoS ONE. (2020) 15:e0244630. doi: 10.1371/journal.pone.0244630
25. Pollock A, Campbell P, Cheyne J, Cowie J, Davis B, McCallum J, et al. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed methods systematic review. Cochrane Database Syst Rev. (2020) 11:CD013779. doi: 10.1002/14651858.CD013779
Keywords: COVID-19, chronic kidney disease, self-rating anxiety scale (SAS), psychological response, online consultation
Citation: Jiang Z, Liu J, Geng L, Zhong Z, Tan J, Wen D, Zhou L, Tang Y and Qin W (2021) The Influences of COVID-19 on Patients With Chronic Kidney Disease: A Multicenter Cross-Sectional Study. Front. Psychiatry 12:754310. doi: 10.3389/fpsyt.2021.754310
Received: 06 August 2021; Accepted: 25 October 2021;
Published: 25 November 2021.
Edited by:
Elham Ahmadian, Tabriz University of Medical Sciences, IranReviewed by:
Si-Tong Chen, Victoria University, AustraliaRicha Tripathi, All India Institute of Medical Sciences, India
Copyright © 2021 Jiang, Liu, Geng, Zhong, Tan, Wen, Zhou, Tang and Qin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yi Tang, tmka1986@163.com; Wei Qin, qinweihx@scu.edu.cn
 Zheng Jiang
Zheng Jiang Jiang Liu2,3
Jiang Liu2,3 Zhengxia Zhong
Zhengxia Zhong Ling Zhou
Ling Zhou Yi Tang
Yi Tang Wei Qin
Wei Qin