- Institute of Artificial Intelligence in Sports, Capital University of Physical Education and Sports, Beijing, China
Background: The COVID-19 pandemic has had a significant impact on physical and mental health, while physical activity and sleep are two important indicators of the impact that have been explored in recent studies. However, the results of studies with different measurement methods and populations with different levels of physical activity have been diverse in that physical activity and sleep are affected by the COVID-19 pandemic in some studies but not in others. Our study aimed to investigate the impact of the COVID-19 pandemic on physical activity and sleep and the role of measurement methods and populations on results.
Methods: PubMed, Web of Science, and CNKI databases were used to search for related studies systematically. Study characteristics and data on physical activity and sleep were collected and analyzed from each included study. Standardized mean differences (SMDs) with 95% confidence intervals (CIs) were used to estimate pooled effect sizes.
Results: A total of 13 articles were included in the systematic review, 11 of which were included in the meta-analysis. We found that moderate-to-vigorous physical activity (MVPA) time was 0.33 (95% CI 0.07 to 0.59) and sleep quality was 0.37 (95% CI 0.21 to 0.53) decreased, while sleep duration was −0.24 (95% CI −0.28 to −0.20) increased during the lockdown; overall physical activity time had no significant difference (p = 0.07) during the lockdown. The “wearables” subgroup had no heterogeneity (p = 0.89, I2 = 0) in sleep duration, while MVPA time measured by subjective scales was not significantly changed. The “elite athletes” subgroup had lower heterogeneity (p = 0.69, I2 = 0) in sleep duration than general adults, while the results of sleep quality for population subgroups were significant and there was no heterogeneity within either.
Conclusion: The COVID-19 pandemic had a significant impact on MVPA time, sleep duration, and sleep quality, instead of overall physical activity time among healthy adults. The results of MVPA time and sleep duration were greatly influenced by the measurement methods, and sleep behavior differed among populations with varying physical activity levels. Thus, when researching physical activity, especially MVPA time, should consider measurement methods, and more attention should be given to differences in populations when researching sleep behavior.
1. Introduction
The worldwide COVID-19 pandemic has brought immense distress to all human beings. In the period of early COVID-19, it was estimated that 2.6 billion people (Van Hoof, 2020) were in lockdown or quarantine for an average of 35.38 days in 49 countries (Atalan, 2020). Lockdown slowed down the spread of the coronavirus (Lau et al., 2020), but it influenced public health in both physical health (Werneck and Carvalho, 2020; Amerio et al., 2021; Jurecka et al., 2021; Knowles et al., 2021; Pensgaard et al., 2021; Jia et al., 2022) and mental health (McTiernan et al., 2019; Chandrasekaran and Ganesan, 2021; Khan et al., 2022). The most direct impact of COVID-19 on people was the changes in physical activity, which was reduced due to remote work or study (Bu et al., 2021) or the closure of outdoor activity areas (Ugolini et al., 2021). This had led to changes in life balance, creating difficulties for physical activity. In addition, mental health was affected in ways that cannot be ignored, negative moods (e.g., pressure, irritability, nervous, distress, and worry) were reported in many studies, and corresponding changes in sleep behavior were found in healthy adults (Ingram et al., 2020; Kocevska et al., 2020; Alfonsi et al., 2021; Amerio et al., 2021). Thus, synchronized investigations of physical activity and sleep behavior during the COVID-19 pandemic may provide further evidence for understanding its impact on public health.
The impact of the COVID-19 pandemic on physical activity and sleep behavior among healthy adults has been recently investigated in several studies with inconsistent results. While some studies have reported changes in physical activity (Janssen et al., 2020; Sañudo et al., 2020; Zinner et al., 2020; Buoite Stella et al., 2021; Chouchou et al., 2021; da Silva Santos et al., 2021; Massar et al., 2022) and sleep behavior (Mon-López et al., 2020; Sañudo et al., 2020; Zinner et al., 2020; Lorenzo Calvo et al., 2021; Martínez-de-Quel et al., 2021; Ong et al., 2021) during the lockdown, others have not found any significant changes (da Silva Santos et al., 2021; Vitale et al., 2021). One of the possible reasons could be that the results may be influenced by different measurement methods. Physical activity and sleep behavior can be assessed by subjective scales or wearables. The Pittsburgh sleep quality index (PSQI) (Smyth, 1999) is a traditional subjective way to measure sleep behavior, while the International Physical Activity Questionnaire (IPAQ) (IPAQ Group, 2020) is a common choice to assess physical activity subjectively. Meanwhile, both physical activity and sleep behavior can be measured by wearables (Rosenberger et al., 2016). Given the discrepancy between subjective estimates and objective measures, the results of physical activity and sleep behavior may not be accurately and consistently represented by different measurement methods. Another possible reason could be that different populations have different levels of physical activity in their normal life which is reported to play a moderating role in the impact of the pandemic on one's physical activity and sleep (Martínez-de-Quel et al., 2021). Most typically, elite athletes devote more time to training which results in a much higher level of physical activity than general adults. Furthermore, the inclusion of high-risk populations may confound the study of the relationship between the COVID-19 pandemic, physical activity, and sleep behavior (García-Lara et al., 2022). For instance, healthcare workers were acutely affected by the COVID-19 pandemic, and the disease could affect the physical and mental health of the patients.
In this regard, two existing systematic reviews on physical activity and sleep behavior among healthy adults during COVID-19 suffer from two main limitations: (1) the inclusion of a single population (Jurecka et al., 2021) or confusion of different populations for the study (Hamasaki, 2021) and (2) the inclusion of a single type of measurement method, without comparing both subjective and objective measurement methods (Hamasaki, 2021; Jurecka et al., 2021).
In our study, we conducted a systematic review and meta-analysis of studies examining physical activity and sleep behavior among healthy adults during the COVID-19 lockdown period. We investigated the impact of the COVID-19 pandemic on physical activity and sleep behavior among healthy adults, explored potential differences in these effects across different measurement methods and different populations through subgroup analyses, and, meanwhile, excluded high-risk populations.
2. Methods
2.1. Search strategy
This systematic review and meta-analysis were conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Moher et al., 2009). The search was performed independently by two authors (XZ and JG) using the databases Web of Science, PubMed, and CNKI. They chose articles that were published after 2020. The search strategy employed Medical Subject Headings (MeSH) terms and free words. The strategies are as follows: (quarantine OR COVID-19 OR lockdown OR coronavirus OR SARS-CoV-2) AND ((physical activity) OR training OR exercise) AND sleep NOT patients* NOT nurses* NOT doctors*. Titles and abstracts were screened, and full texts were assessed to ensure that they met the following eligibility criteria.
2.2. Eligibility criteria
Eligibility criteria were created based on the PICOs framework: (1) P, Participants: healthy adults who are not healthcare workers and without any risks of disease; (2) I, Intervention: experience the lockdown of the COVID-19 pandemic; (3) C, Comparison: physical activity and sleep behavior data during the lockdown and un-lockdown periods; (4) O, Outcome: the COVID-19 pandemic affects physical activity and sleep or not; and (5) S, Study design: cohort study or cross-sectional study. Any disagreements in the literature screening process were discussed and resolved by consensus between the two authors (XZ and JG).
2.3. Data abstraction
The two authors (XZ and JG) extracted the necessary data independently, and all disagreements were resolved through discussion until a consensus was reached. Since the variables that we are concerned with were physical activity and sleep behavior, the necessary data we extracted included overall physical activity time, different levels of physical activity time, sleep duration, and sleep quality, where different levels of physical activity time were not available due to insufficient data on sedentary behavior in the included studies, so we instead performed a detailed analysis of MVPA time. Finally, the necessary data extraction was performed using a Microsoft Excel spreadsheet, and the content of the sheet was author, year, study design, population characteristics, research tools used, date of data collection, main findings, and data regarding physical activity and sleep behavior.
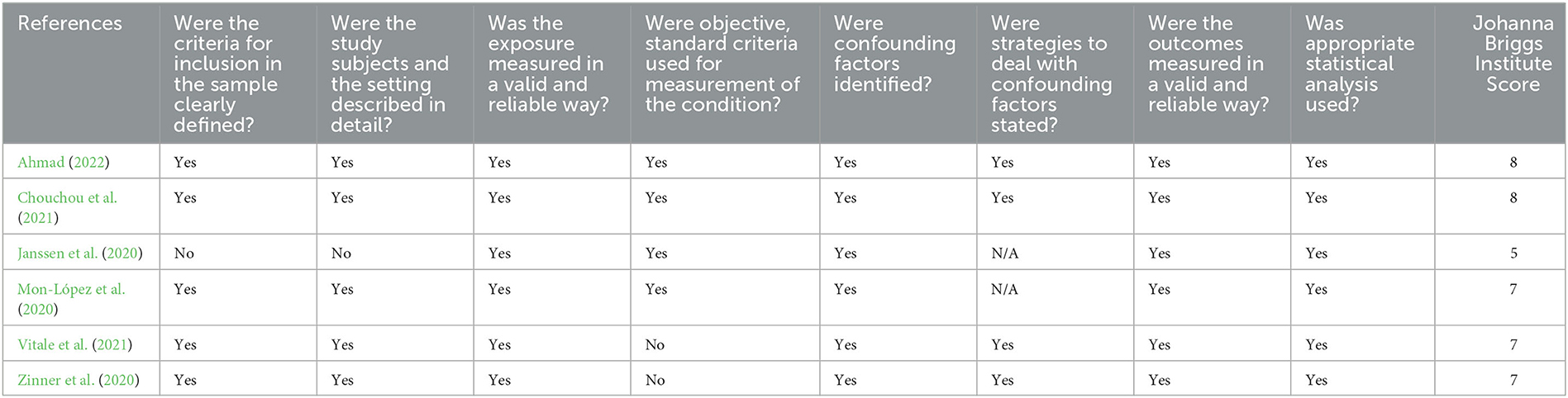
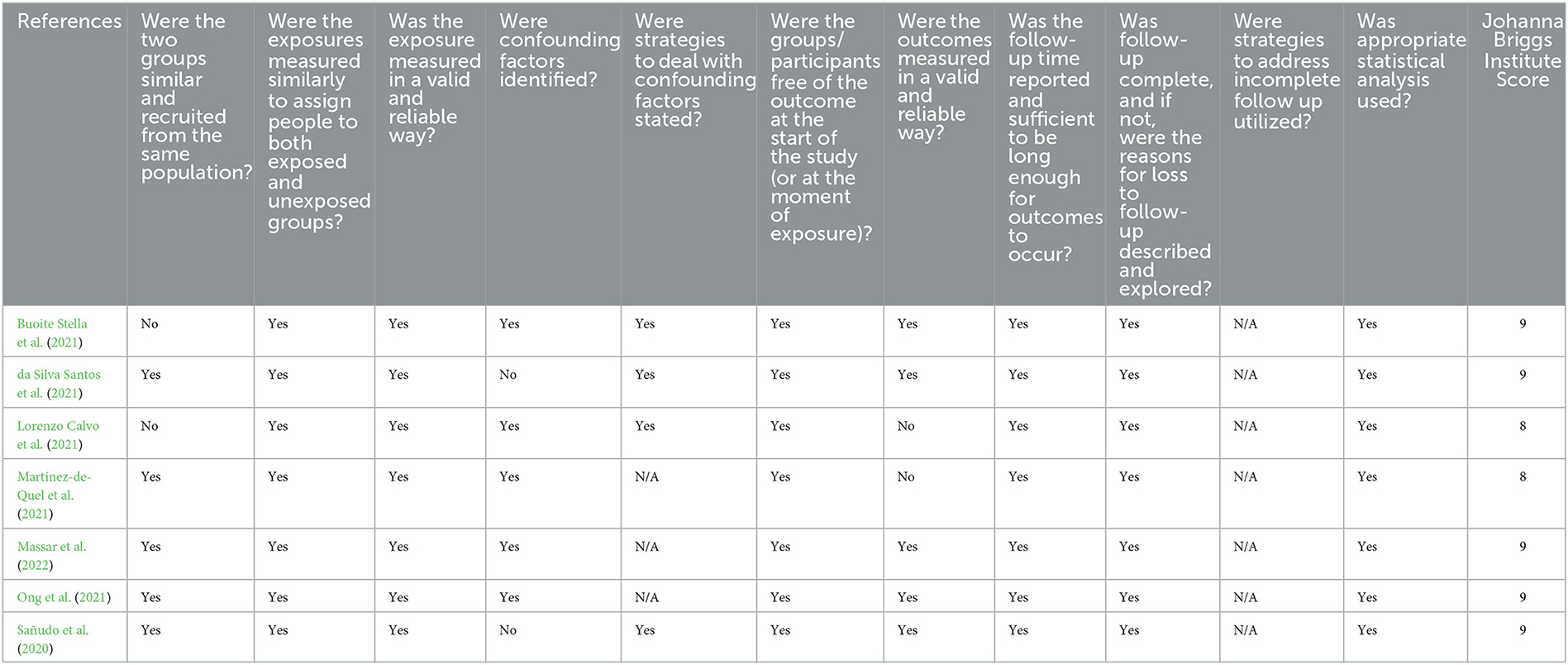
2.4. Risk-of-bias assessment
The quality of eligibility studies was assessed using the Joanna Briggs Institute (JBI) critical appraisal tools, including both cross-sectional and cohort (Aromataris and Munn, 2020). The grade standard of risk-of-bias assessment is based on the following criteria: 70% of the answers are “YES” for low risk, 50%−69% of the scores are “YES” for medium risk, and if the score of “YES” is <50%, then it is high risk (TIJ B, 2014). The two authors (XZ and JG) conducted and verified the assessment independently, and all disagreements in the assessment were resolved by an agreement through discussion.
2.5. Data analysis
A qualitative analysis was performed to summarize physical activity and sleep behavior among healthy adults during the lockdown period due to COVID-19 compared with a normal period without lockdown.
Quantitative analyses were conducted using Review Manager 5.4, and only SMDs related to statistical models that can be applied to continuous variables were considered. The primary measures were 95% CIs for all the meta-analyses, including overall physical activity time, MVPA time, sleep duration, and sleep quality, respectively. Therein, a fixed-effect model was used for sleep duration, and a random-effect model was used for all other variables.
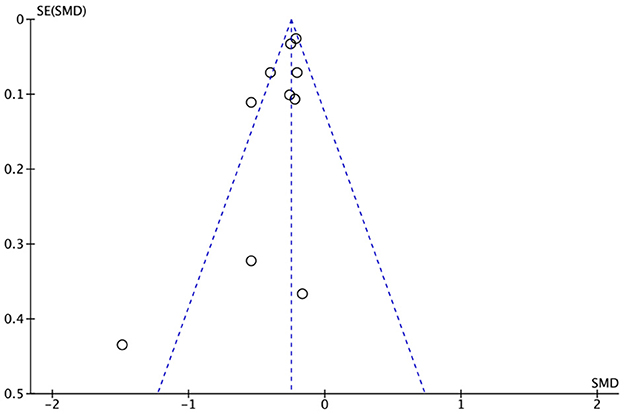
To assess the stability and reliability of pooled effect size results of the meta-analysis, sensitivity analyses were performed. A leave-one-out sensitivity analysis was used in our study, in which each study was removed from the model once to examine the results. A funnel plot was conducted to detect in meta-analysis where the effect estimates responded to the standard errors.
The difference between studies in a meta-analysis is heterogeneity. To assess heterogeneity in the quantitative analyses, we calculated the p-value, with a p-value of <0.05 indicating significant heterogeneity (Correll et al., 2018). Additionally, we considered I2 lower than 25%, between 25 and 75%, and higher than 75% as low, moderate, and high heterogeneity, respectively (Higgins et al., 2003). We pooled the results of the studies with low heterogeneity using fixed-effect models and of the studies with heterogeneity but not considerable heterogeneity using random-effect models. For events with considerable heterogeneity (p < 0.05 or I2 > 50%), subgroup analyses were conducted according to different populations and measurement methods which included a measurement by wearables or not, and whether the population was elite athletes or not for further research.
3. Results
3.1. Included studies
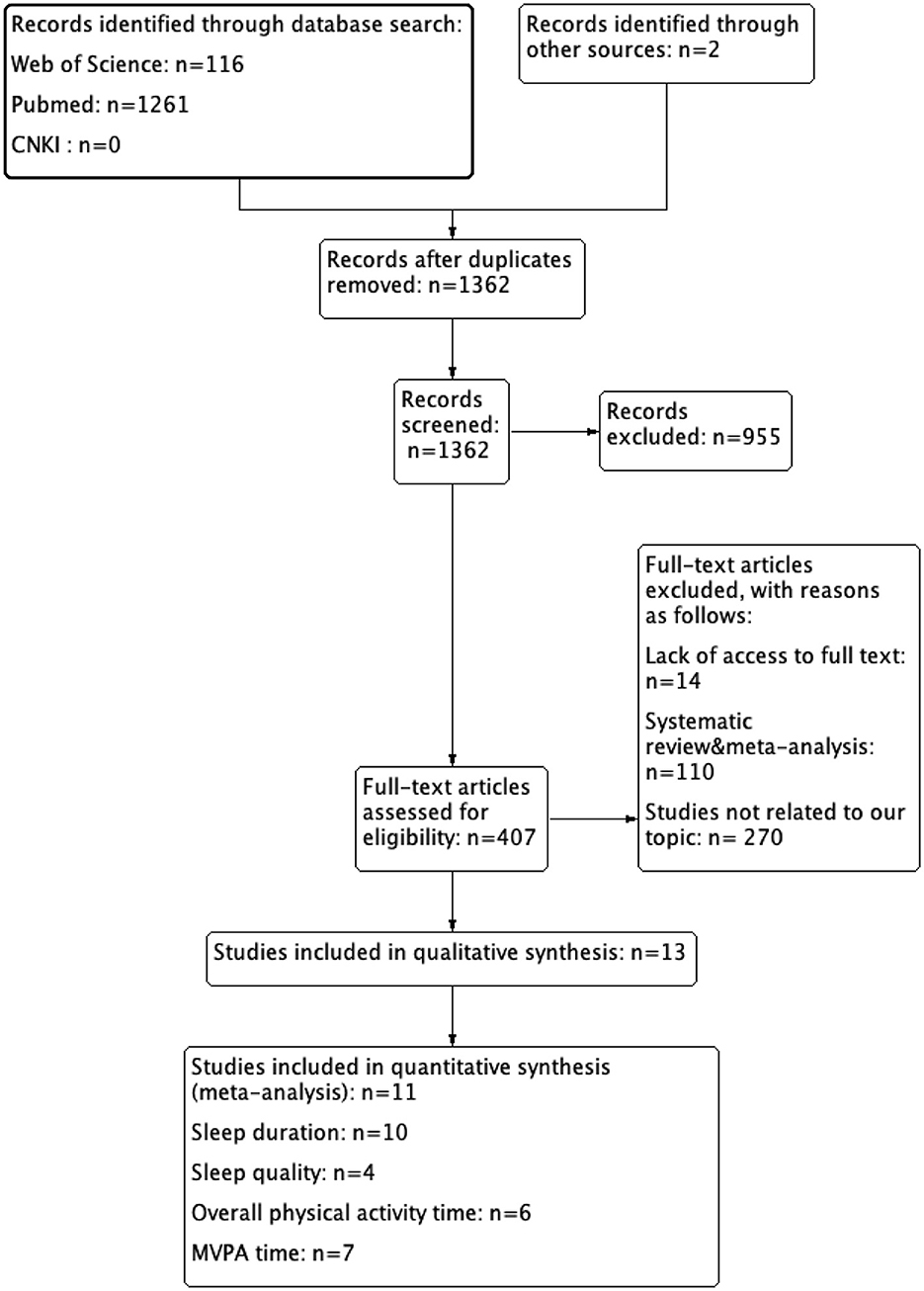
A total of 1,379 records were identified by searching PubMed, Web of Science, and CNKI databases, with two additional records from other sources. After the removal of duplicates (17 records) and studies not meeting the inclusion criteria (1,098 records), 407 studies remained. Ultimately, 13 studies were included in the systematic review according to the PICOs criteria, while 11 studies met the inclusion criteria of the meta-analysis. Details of the search results are shown in Figure 1.
3.2. Characteristics of included studies
A total of 7,096 participants were included in the studies, except one that did not mention the number of female participants, of which 38.06% were female participants. Of these participants, nine studies included general adults, while five studies included elite athletes in badminton, soccer, basketball, kayaking and canoeing, and track and field. The details are described in Table 1.
All the included studies conducted research in both lockdown and un-lockdown contexts, with one study focusing on the lockdown and post-lockdown and the others on the pre-lockdown and lockdown periods. The measurement methods used by the studies are summarized in Table 1. Of the measurement methods, six studies measured physical activity and sleep behavior through the use of wearables such as pedometers or accelerometers (see Table 1), while seven studies measured physical activity and sleep behavior through subjective scales. The results of all the studies were reported in the form of mean ± standard deviation (M ± SD).
3.3. Risk of bias within studies
We identified all 13 studies in our research, including seven cross-sectional studies and six cohort studies (Tables 2, 3). Five of the cross-sectional studies (Mon-López et al., 2020; Zinner et al., 2020; Chouchou et al., 2021; Vitale et al., 2021; Ahmad, 2022) were of low-risk, and one study (Janssen et al., 2020) was of medium risk. All six cohort studies (Sañudo et al., 2020; Buoite Stella et al., 2021; da Silva Santos et al., 2021; Lorenzo Calvo et al., 2021; Martínez-de-Quel et al., 2021; Ong et al., 2021; Massar et al., 2022) were of low risk.
3.4. Qualitative analysis
Changes in physical activity and sleep behavior between the lockdown and the un-lockdown periods in individuals are mixed. For overall physical activity time, six studies were included, and two studies presented a decrease during the lockdown period. Four of seven studies assessed MVPA time and showed decreases, while others showed no significant change. For sleep duration, 10 studies were included, and six studies presented an increase during the lockdown period while others were unchanged. Four studies assessed sleep quality, three of four showed a decrease, and one of four showed unchanged.
3.5. Quantitative analyses
For the quantitative analyses, we included 11 studies that assessed physical activity and sleep behavior, while studies (6, 7, 10, and 4) assessed overall physical activity time, MVPA time, sleep duration, and sleep quality, respectively. The exclusion reason for quantitative analyses is that the necessary data were not available in these two studies (Martínez-de-Quel et al., 2021; Vitale et al., 2021). After a leave-one-out sensitivity analysis, the pooled effect sizes of all the quantitative analyses remained stable.
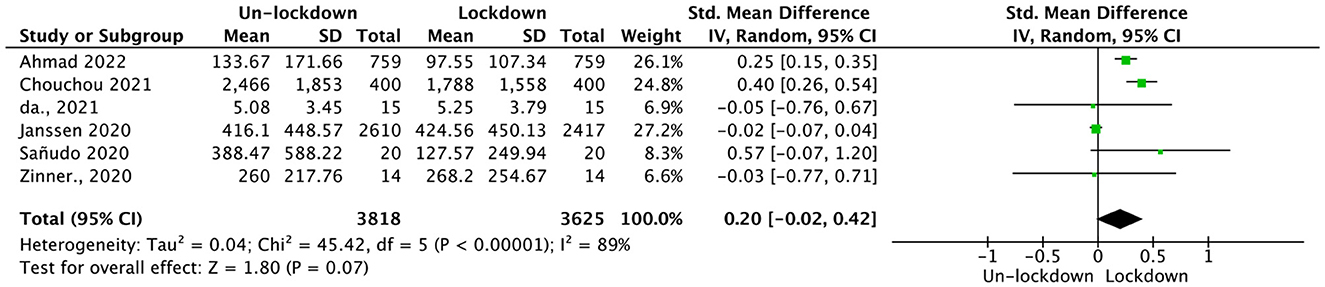
3.5.1. Overall physical activity
Data from six studies including 3,625 participants were analyzed for overall physical activity time. The random-effect pooled Hedges' g was 0.20 (95% CI = −0.02, 0.42; see Figure 2), which was not statistically significant (p = 0.07), and with high heterogeneity (p < 0.01, I2 = 89%). A subgroup analysis was conducted accordingly.
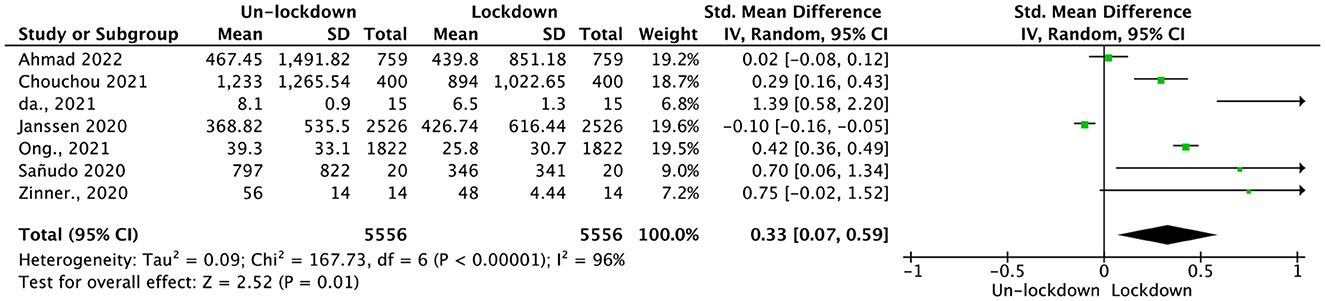
3.5.2. MVPA time
Data were acquired from seven studies which included 5,556 participants. An analysis of the data revealed a significant association between MVPA time and COVID-19 lockdown, as indicated by Hedges' g = 0.33; CI = (0.07, 0.59; see Figure 3). This association was statistically significant (p = 0.01), with high heterogeneity (p < 0.01, I2 = 96%). To further explore the source of heterogeneity, subgroup analyses were conducted.
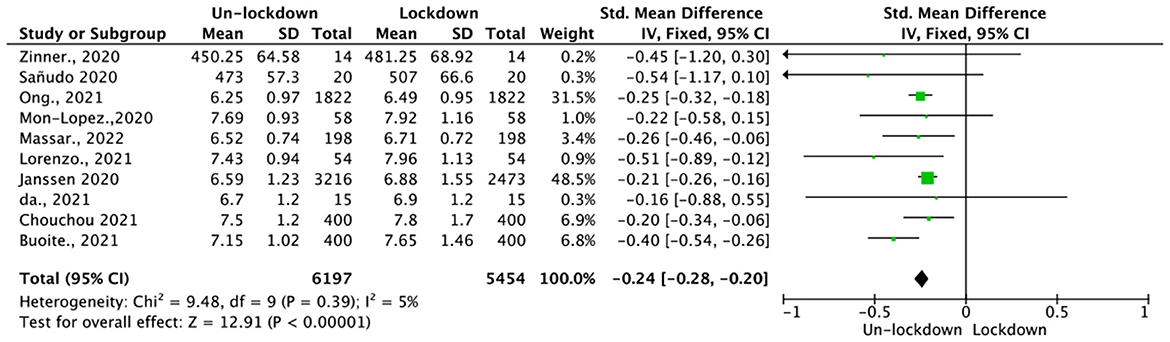
3.5.3. Sleep duration
Data were acquired from 10 studies, which included 5,454 participants. The measurements of sleep duration were based on wearables and subjective scales. Analysis of the sleep duration revealed a low heterogeneity (p = 0.39, I2 = 5%), and consequently, a fixed-effect model was employed. The resulting fixed-effect pooled SMD (Hedges' g) was −0.24 (95% CI = −0.28, −0.20), which was statistically significant (p < 0.01; see Figure 4).
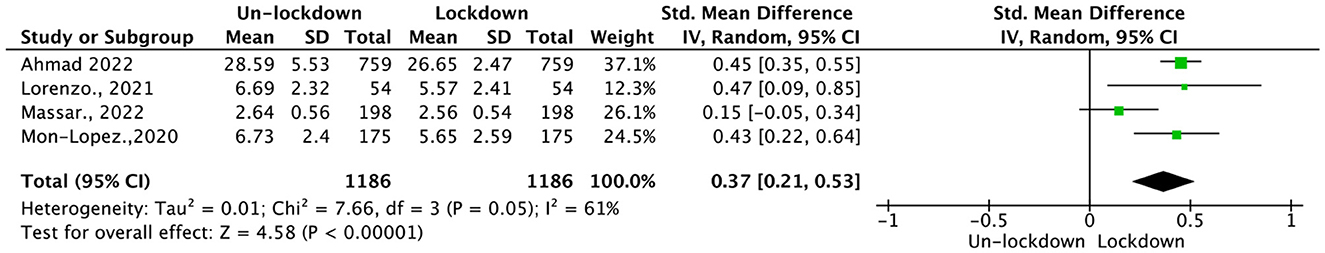
3.5.4. Sleep quality
Data from four studies including 1,186 participants were acquired, and a random-effect pooled SMD (Hedges' g) with a 95% CI was conducted. For sleep quality, the results showed a statistically significant Hedges' g of 0.37 (95% CI = 0.21, 0.53, p < 0.01; see Figure 5). However, moderate heterogeneity was observed (p = 0.05, I2 = 61%); thus, a subgroup analysis was performed.
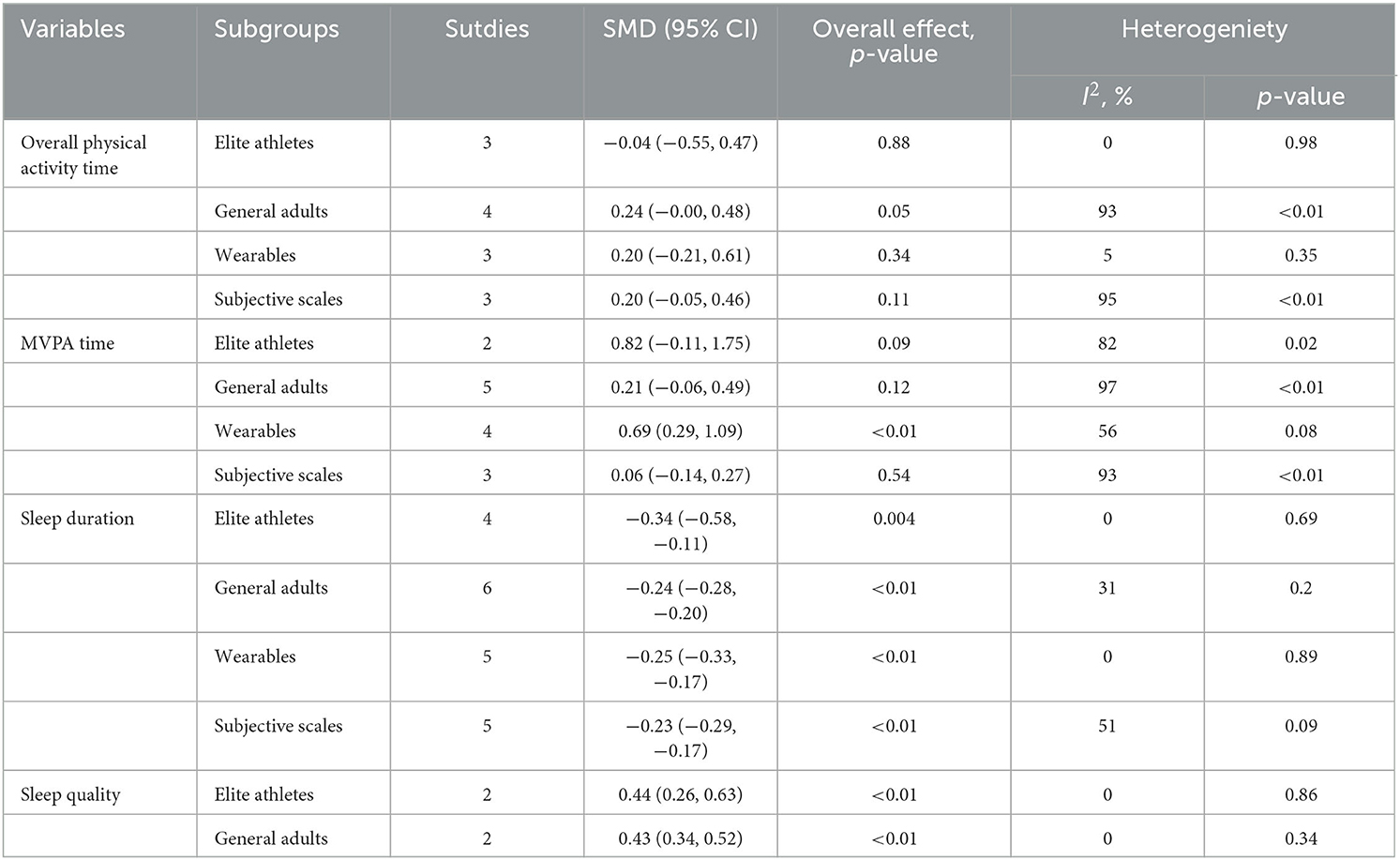
3.6. Subgroup analyses
Given that heterogeneity was observed in the results including overall physical activity time, MVPA time, and sleep quality, subgroup analyses were required. Moreover, we also intended to explore whether there was also an effect of different groupings on the results of sleep duration. Therefore, we conducted related subgroup analyses in measurement methods and populations. After a leave-one-out sensitivity analyses, the pooled effect sizes remained stable.
Six studies were included in the subgroup analysis of overall physical activity time. Neither the population nor the measurement methods showed statistically significant differences before and during the COVID-19 pandemic, with SMDs and 95% CIs for populations of −0.04 (−0.55 to 0.47) and 0.24 (−0.00 to 0.48), respectively, 0.20 (−0.21 to 0.61) and 0.20 (−0.05 to 0.46) for measurement methods, see Table 4.
In the subgroup analyses of measurement methods in MVPA time, the COVID-19 pandemic had a moderate heterogeneity (p = 0.08, I2 = 56%) effect on MVPA time measured by wearables (p < 0.01), while MVPA time measured using subjective scales was unaffected with high heterogeneity (p < 0.01, I2 = 93%). In the subgroups of elite athletes and general adults, there was no association between MVPA time and the COVID-19 pandemic, which is not consistent with the pooled effect result.
Ten studies were involved in sleep duration subgroup analyses. Table 4 shows that both subjective measurement and wearables were significantly associated with lockdown, with SMDs (95% CI) of −0.23 (−0.29 to −0.17) and −0.25 (−0.33 to −0.17), respectively, and no heterogeneity in the results for wearables. Furthermore, both elite athletes and general adults were significantly associated with lockdown state, with SMDs (95% CI) of −0.34 (−0.58 to −0.11) and −0.24 (−0.28 to −0.20), respectively. There was no heterogeneity in the results for elite athletes. Though the sample sizes varied significantly between elite athletes and general adults in the subgroup analysis of sleep duration, the results were robust after sensitivity analysis.
Four studies were involved in the subgroup analysis of sleep quality (see Table 4). The results showed that both elite athletes and general adults were significantly associated with the lockdown, with SMDs (95% CIs) of 0.44 (0.26 to 0.63) and 0.43 (0.34 to 0.52), respectively. There was no heterogeneity detected.
3.7. Publication bias
We conducted the publication bias assessment using a review manager which is summarized in Figure 6. We used analysis of sleep duration to generate the funnel plot since it included 10 of the 13 studies and covered more than any other analyses. With a visual inspection, there seems to be symmetry which means a low possibility of publication bias (see Figure 6).
4. Discussion
4.1. Meta-analysis
Our study summarizes the evidence for the prospective association between the COVID-19 pandemic and physical activity and sleep behavior in individuals. Overall, the association of the COVID-19 pandemic with both physical activity and sleep behavior was mixed.
4.1.1. Physical activity
Our results are not consistent with a number of previous studies that have emphasized that there was an increase in overall physical activity time for individuals during the COVID-19 pandemic (Sañudo et al., 2020; Buoite Stella et al., 2021; Chouchou et al., 2021; Massar et al., 2022), but we found no difference. First, the non-significant change may indicate the complexity of the impact of the COVID-19 pandemic on overall physical activity time, and there are different levels of physical activity, which include sedentary, light physical activity, and MVPA. Light physical activity with low exertion may increase during the COVID-19 pandemic, and Wilms et al. (2022) proposed that the lockdown restrictions could cause an increase in low MET activities, such as sedentary behavior (Janssen et al., 2020; Wilms et al., 2022), or increase in housework due to the long period of confinement (Wunsch et al., 2022). Meanwhile, some studies suggested a decrease in MVPA time for individuals during the COVID-19 pandemic (Janssen et al., 2020; Zinner et al., 2020; da Silva Santos et al., 2021), which is consistent with our final findings that MVPA time changed during the COVID-19 pandemic and people spent less time exercising, leading to a decrease in MVPA time, and Ugolini et al. (2021) also suggested that many outdoor leisure activity places were completely closed or restricted, which could reduce people's MVPA time (Karuc et al., 2020). The combination of increased low exertion physical activity and decreased MVPA time led to a non-significant result in overall physical activity time. Furthermore, the decrease in MVPA was more evident in athletes. The main component of physical activity in athletes is training, and some studies (Zinner et al., 2020; da Silva Santos et al., 2021) have shown a decreased training time in athletes during the COVID-19 pandemic which may account for the significant change in MVPA time.
However, there was high heterogeneity in the results for both overall physical activity time and MVPA time, so we further explored the results using subgroup analyses.
4.1.2. Sleep behavior
There is also a growing body of evidence suggesting that the COVID-19 pandemic may have an impact on sleep behavior, but equivocal findings were reported in the previous studies. For example, some studies suggest that sleep behavior (da Silva Santos et al., 2021) such as sleep duration (Vitale et al., 2021) was not affected negatively by the lockdown. However, our meta-analysis reveals that sleep duration increased and sleep quality decreased. Several possible mechanisms explain our results. First, the COVID-19 pandemic may have caused negative moods, many studies have shown that negative moods were related to poor sleep quality (e.g., pressure, irritability, nervous, distress, and worry) (Ingram et al., 2020; Kocevska et al., 2020; Alfonsi et al., 2021; Amerio et al., 2021), and increased negative moods during the COVID-19 pandemic may have worsened people's sleep quality indirectly. Second, less social time could lead to more free time for sleep in individuals. Changes in working or studying status could cause a reduction in socialization (Leone et al., 2020) as people did not need to go outside, and they could manage their own time freely which may be one of the reasons for the increase in sleep duration. Furthermore, the effects of the lockdown on sleep varied across different populations (Kocevska et al., 2020; Alfonsi et al., 2021).
4.2. Subgroup analysis
Our results indicated that there was no significant difference in the overall physical activity time in the two subgroups, suggesting that neither of them is the source of heterogeneity in overall physical activity time. Furthermore, we performed subgroup analyses of both measurement methods and populations for MVPA time, sleep duration, and sleep quality.
First, there are discrepancies regarding measurement methods on MVPA time and sleep duration, and the wearables subgroup showed a significant advantage in both the subgroup analysis of MVPA time and sleep duration. One of the possible reasons is that wearables are more accurate and reliable. Studies by Schmidt et al. (2008) and Hagstromer et al. (2010) have shown that objective and subjective measures are independent; in our study, MVPA time measured by wearables showed moderate heterogeneity (p = 0.08, I2 = 56%) and consistent with the results of the pooled effect size, while subjective scales were not. When comparing subjective and objective measurement methods of physical activity (Beagle et al., 2020) and sleep behavior (Grandner and Rosenberger, 2019), wearables were superior to subjective scales. Thus, this may suggest that wearables are more sensitive and may provide more valid results if more studies are conducted using them. Bias in subjective estimates is the other possible reason. In our results, high heterogeneity existed in the factors measured by the subjective scales, suggesting that there were other confounding factors. People may have inaccurate subjective results when they estimate time as they tend to perceive times later than objective measurement results (He et al., 2021), and this possibly confirmed the excessive subjective bias in people's estimates of time which led to the high heterogeneity.
Second, the difference of populations existed in sleep behavior, including sleep duration and sleep quality, of which sleep behavior among general adults was more affected by the pandemic. Physical activity may be the cause of the difference. Our study demonstrated small relative changes in physical activity for the population subgroups. Large differences in absolute values of physical activity between elite athletes and general adults existed, while the former still exhibited higher levels of physical activity than general adults during the lockdown period (Monterrosa Quintero et al., 2022; Shokri et al., 2022). Physical activity has been proven to improve sleep quality and mental health (Werneck and Carvalho, 2020), and some studies suggest that COVID-19 led to physical activity restriction, which may have led to changes in acute endocrine and metabolic profiles (Uchida et al., 2012), and thus inducing the decline in sleep quality. Elite athletes maintained a certain level of physical activity during the COVID-19 pandemic, and they lived a much more regular lifestyle compared to the more unstable lifestyle of the general adults which resulted in the latter being more vulnerable to the COVID-19 pandemic.
4.3. Limitations
In this study, we did not include enough studies on healthy adults with different levels of physical activity due to the limited availability of relevant studies, especially healthy adults with high physical activity levels, e.g., elite athletes. The results for both elite athletes and general adults in the MVPA time measure were not significant and inconsistent with the pooled effect size results, which may be due to the small sample size. Although the wearables results were more convincing than the subjective scale, it was not possible to further explore the subjective scale mechanisms and confounders, and it could be the motivation for our research on the improvement of measurement methods.
5. Conclusion
We conducted the first systematic review and meta-analysis of physical activity and sleep behavior among healthy adults to assess the impact of the COVID-19 pandemic on both of them during the lockdown period vs. the un-lockdown period. Subgroup analyses were conducted to identify grouping influencing factors. In summary, our results suggest that the COVID-19 pandemic had a significant effect on healthy adults' physical activity and sleep behavior, of which MVPA time and sleep quality decreased, and sleep duration increased. Additionally, measurement methods and populations were found to be valid grouping variables on measures of physical activity and sleep behavior. The results differed between subjective scales and wearables, with wearables being more significantly affected by MVPA time and sleep duration during the COVID-19 pandemic, suggesting that wearables are sensitive and that population subgroups have an impact on sleep duration and sleep quality.
These findings may provide a reference for the preparation of mental health and physical health-related countermeasures under a possible future pandemic. In future studies, the sleep behavior of different populations should be a concern, and we should pay more attention to the accuracy and stability of wearables and subjective scales in measurements for more efficient studies.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
XZ and JG conducted an assessment of included studies, data collection, analysis, and prepared the article for publication after editing and revisions. XZ wrote the initial draft. DC formulated the aims of this study, designed the methodology, made contributions to the revision, and acquired financial support for this study. All authors prepared the article to be published with critical reviews.
Funding
DC was supported by the National Natural Science Foundation of China (Grant No. 62106159), the National Key Research and Development Program of China (Grant No. 2020YFC2006200), and the China National Sprint and Relay Team preparing for the Tokyo Olympics in the scientific research and technical service project 2021 (2021TJ01001).
Acknowledgments
We are appreciative of the reviewers and editors who have made comments and suggestions on this article, and whose detailed feedback improved our research greatly.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ahmad, A. (2022). Changes in health-related lifestyles and food insecurity and its association with quality of life during the COVID-19 lockdown in Malaysia. BMC Public Health 9, 1270. doi: 10.1186/s12889-022-13640-9
Alfonsi, V., Gorgoni, M., Scarpelli, S., Zivi, P., Sdoia, S., Mari, E., et al. (2021). COVID-19 lockdown and poor sleep quality: not the whole story. J. Sleep Res. 30, e13368. doi: 10.1111/jsr.13368
Amerio, A., Lugo, A., Stival, C., Fanucchi, T., Gorini, G., Pacifici, R., et al. (2021). COVID-19 lockdown impact on mental health in a large representative sample of Italian adults. J. Affect. Disord. 292, 398–404. doi: 10.1016/j.jad.2021.05.117
Aromataris, E., and Munn, Z., (eds),. (2020). JBI Manual for Evidence Synthesis. JBI. Available online at: https://synthesismanual.jbi.global
Atalan, A. (2020). Is the lockdown important to prevent the COVID-19 pandemic? Effects on psychology, environment and economy-perspective. Ann. Med. Surg. 56, 38–42. doi: 10.1016/j.amsu.2020.06.010
Beagle, A. J., Tison, G. H., Aschbacher, K., Olgin, J. E., Marcus, G. M., and Pletcher, M. J. (2020). Comparison of the physical activity measured by a consumer wearable activity tracker and that measured by self-report: cross-sectional analysis of the Health eHeart Study. JMIR Mhealth Uhealth 8, e22090. doi: 10.2196/22090
Bu, F., Bone, J. K., Mitchell, J. J., Steptoe, A., and Fancourt, D. (2021). Longitudinal changes in physical activity during and after the first national lockdown due to the COVID-19 pandemic in England. Sci. Rep. 11, 17723. doi: 10.1038/s41598-021-97065-1
Buoite Stella, A., Ajčevi,ć, M., Furlanis, G., Cillotto, T., Menichelli, A., Accardo, A., et al. (2021). Smart technology for physical activity and health assessment during COVID-19 lockdown. J. Sports Med. Phys. Fitness 61, 452–460. doi: 10.23736/S0022-4707.20.11373-2
Chandrasekaran, B., and Ganesan, T. B. (2021). Sedentarism and chronic disease risk in COVID 19 lockdown – a scoping review. Scott. Med. J. 66, 3–10. doi: 10.1177/0036933020946336
Chouchou, F., Augustini, M., Caderby, T., Caron, N., Turpin, N., and Dalleau, G. (2021). The importance of sleep and physical activity on well-being during COVID-19 lockdown: reunion island as a case study. Sleep Med. 77, 297–301. doi: 10.1016/j.sleep.2020.09.014
Correll, C. U., Galling, B., Pawar, A., Krivko, A., Bonetto, C., Ruggeri, M., et al. (2018). Comparison of early intervention services vs treatment as usual for early-phase psychosis: a systematic review, meta-analysis, and meta-regression. JAMA Psychiatry 75, 555. doi: 10.1001/jamapsychiatry.2018.0623
da Silva Santos, A. M., Rossi, F. E., Dos Santos Nunes de Moura, H. P., de Sousa Junior, A. V. M., Machado, D. C. D., Neves, L. M., et al. (2021). COVID-19 pandemic impacts physical activity levels and sedentary time but not sleep quality in young badminton athletes. Sport Sci. Health 17, 969–977. doi: 10.1007/s11332-021-00763-6
García-Lara, R. A., Suleiman-Martos, N., Membrive-Jiménez, M. J., García-Morales, V., Quesada-Caballero, M., Guisado-Requena, I. M., et al. (2022). Prevalence of depression and related factors among patients with chronic disease during the COVID-19 pandemic: a systematic review and meta-analysis. Diagnostics 12, 3094. doi: 10.3390/diagnostics12123094
Grandner, M. A., and Rosenberger, M. E. (2019). “Actigraphic sleep tracking and wearables: Historical context, scientific applications and guidelines, limitations, and considerations for commercial sleep devices,” in Sleep and Health (Amsterdam: Elsevier), 147−157. doi: 10.1016/B978-0-12-815373-4.00012-5
Hagstromer, M., Ainsworth, B. E., Oja, P., and Sjostrom, M. (2010). Comparison of a subjective and an objective measure of physical activity in a population sample. J. Phys. Activity Health 7, 541–550. doi: 10.1123/jpah.7.4.541
Hamasaki, H. (2021). Daily physical activity and sleep measured by wearable activity trackers during the coronavirus disease 2019 pandemic: a lesson for preventing physical inactivity during future pandemics. Appl. Sci. 11, 9956. doi: 10.3390/app11219956
He, L., Zhao, W., Gao, Y., Gao, X., and Lei, X. (2021). The effect of COVID-19 lockdowns on sleep time perception: comparing actigraphy and sleep diary measures. Int. J. Psychophysiol. 167, 86–93. doi: 10.1016/j.ijpsycho.2021.07.001
Higgins, J. P. T., Thompson, S. G., Deeks, J., and Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ 327, 557–560. doi: 10.1136/bmj.327.7414.557
Ingram, J., Maciejewski, G., and Hand, C. (2020). Changes in diet, sleep, and physical activity are associated with differences in negative mood during COVID-19 lockdown. Front. Psychol. 11, 588604. doi: 10.3389/fpsyg.2020.588604
IPAQ Group (2020). International Physical Activity Questionnaire [EB/OL]. Available online at: http://www.ipaq.ki.se/downloads.html (accessed January 26, 2020).
Janssen, X., Fleming, L., Kirk, A., Rollins, L., Young, D., Grealy, M., et al. (2020). Changes in physical activity, sitting and sleep across the COVID-19 National Lockdown Period in Scotland. Int. J. Environ. Res. Public Health 17, 9362. doi: 10.3390/ijerph17249362
Jia, L., Carter, M. V., Cusano, A., Li, X., Kelly, J. D., Bartley, J. D., et al. (2022). The effect of the COVID-19 pandemic on the mental and emotional health of athletes: a systematic review. Am. J. Sports Med. doi: 10.1177/03635465221087473 [Epub ahead of print].
Jurecka, A., Skucińska, P., and Gadek, A. (2021). Impact of the SARS-CoV-2 coronavirus pandemic on physical activity, mental health and quality of life in professional athletes—a systematic review. Int. J. Environ. Res. Public Health 18, 9423. doi: 10.3390/ijerph18179423
Karuc, J., Sorić, M., Radman, I., and Mišigoj-Duraković, M. (2020). Moderators of change in physical activity levels during restrictions due to COVID-19 pandemic in young urban adults. Sustainability 12, 6392. doi: 10.3390/su12166392
Khan, M. B., Mustafa, A., Rehman, M., AbuAli, N. A., Yuan, C., Yang, X., et al. (2022). Non-contact smart sensing of physical activities during quarantine period using SDR technology. Sensors 22, 1348. doi: 10.3390/s22041348
Knowles, C., Shannon, S., Prentice, G., and Breslin, G. (2021). Comparing mental health of athletes and non-athletes as they emerge from a COVID-19 pandemic lockdown. Front. Sports Act. Living 3, 612532. doi: 10.3389/fspor.2021.612532
Kocevska, D., Blanken, T. F., Van Someren, E. J. W., and Rösler, L. (2020). Sleep quality during the COVID-19 pandemic: not one size fits all. Sleep Med. 76, 86–88. doi: 10.1016/j.sleep.2020.09.029
Lau, H., Khosrawipour, V., Kocbach, P., Mikolajczyk, A., Schubert, J., Bania, J., et al. (2020). The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J. Travel Med. 27, taaa037. doi: 10.1093/jtm/taaa037
Leone, M. J., Sigman, M., and Golombek, D. A. (2020). Effects of lockdown on human sleep and chronotype during the COVID-19 pandemic. Curr. Biol. 30, R930–R931. doi: 10.1016/j.cub.2020.07.015
Lorenzo Calvo, J., Granado-Peinado, M., de la Rubia, A., Muriarte, D., Lorenzo, A., and Mon-López, D. (2021). Psychological states and training habits during the COVID-19 pandemic lockdown in Spanish basketball athletes. Int. J. Environ. Res. Public Health 18, 9025. doi: 10.3390/ijerph18179025
Martínez-de-Quel, Ó., Suárez-Iglesias, D., López-Flores, M., and Pérez, C. A. (2021). Physical activity, dietary habits and sleep quality before and during COVID-19 lockdown: a longitudinal study. Appetite 158, 105019. doi: 10.1016/j.appet.2020.105019
Massar, S., Ng, A., Soon, C., Ong, J., Chua, X., Chee, N., et al. (2022). Reopening after lockdown: the influence of working-fromhome and digital device use on sleep, physical activity, and wellbeing following COVID-19 lockdown and reopening. Sleep 45, zsab250. doi: 10.1093/sleep/zsab250
McTiernan, A., Friedenreich, C. M., Katzmarzyk, P. T., Powell, K. E., Macko, R., Buchner, D., et al. (2019). Physical activity in cancer prevention and survival: a systematic review. Med. Sci. Sports Exerc. 51, 1252. doi: 10.1249/MSS.0000000000001937
Moher, D., Liberati, A., Tetzlaff, J., and Altman, D. G.. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS. Med. 6, 1000097. doi: 10.1371/journal.pmed.1000097
Mon-López, D., García-Aliaga, A., Ginés Bartolomé, A., and Muriarte Solana, D. (2020). How has COVID-19 modified training and mood in professional and non-professional football players? Physiol. Behav. 227, 113148. doi: 10.1016/j.physbeh.2020.113148
Monterrosa Quintero, A., Echeverri Rios, A. R., Fuentes-Garcia, J. P., and Gonzalez Sanchez, J. C. (2022). Levels of physical activity and psychological well-being in non-athletes and martial art athletes during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 19, 4004. doi: 10.3390/ijerph19074004
Ong, J. L., Lau, T., Massar, S. A. A., Chong, Z. T., Ng, B. K. L., Koek, D., et al. (2021). COVID-19-related mobility reduction: heterogenous effects on sleep and physical activity rhythms. Sleep 44, zsaa179. doi: 10.1093/sleep/zsaa179
Pensgaard, A. M., Oevreboe, T. H., and Ivarsson, A. (2021). Mental health among elite athletes in Norway during a selected period of the COVID-19 pandemic. BMJ Open Sport Exerc. Med. 7, 7, e001025. doi: 10.1136/bmjsem-2020-001025
Rosenberger, M. E., Buman, M. P., Haskell, W. L., Mcconnell, M. V., and Carstensen, L. L. (2016). Twenty-four hours of sleep, sedentary behavior, and physical activity with nine wearable devices. Med. Sci. Sports Exerc. 48, 457–465. doi: 10.1249/MSS.0000000000000778
Sañudo, B., Fennell, C., and Sánchez-Oliver, A. J. (2020). Objectively-assessed physical activity, sedentary behavior, smartphone use, and sleep patterns pre- and during-COVID-19 quarantine in young adults from Spain. Sustainability 12, 5890. doi: 10.3390/su12155890
Schmidt, M. D., Cleland, V. J., Thomson, R. J., Dwyer, T., and Venn, A. J. (2008). A comparison of subjective and objective measures of physical activity and fitness in identifying associations with cardiometabolic risk factors. Ann. Epidemiol. 18, 378–386. doi: 10.1016/j.annepidem.2008.01.005
Shokri, F., Taheri, M., Irandoust, K., and Mirmoezzi, M. (2022). Effects of the COVID−19 pandemic on physical activity, mood status, and eating patterns of Iranian Elite athletes and non-athletes. Zahedan J. Res. Med. Sci. 24, 120049. doi: 10.5812/zjrms-120049
Smyth, C. (1999). The Pittsburgh Sleep Quality Index (PSQI). J. Gerontol. Nurs. 25, 10. doi: 10.3928/0098-9134-19991201-10
TIJ B. (2014). Joanna Briggs Institute Reviewers' Manual, 2nd ed. Adelaide, SA: The Joanna Briggs Institute.
Uchida, S., Shioda, K., Morita, Y., Kubota, C., Ganeko, M., and Takeda, N. (2012). Exercise effects on sleep physiology. Front. Neur. 3, 48. doi: 10.3389/fneur.2012.00048
Ugolini, F., Massetti, L., Pearlmutter, D., and Sanesi, G. (2021). Usage of urban green space and related feelings of deprivation during the COVID-19 lockdown: lessons learned from an Italian case study. Land Use Policy 105, 105437. doi: 10.1016/j.landusepol.2021.105437
Van Hoof, E. (2020). “Lockdown is the world's biggest psychological experiment-and we will pay the price,” in World Economic Forum. Davos-Klosters: World Economic Forum, 9.
Vitale, J., Borghi, S., Codella, R., Lastella, M., Nedelec, M., Banfi, G., et al. (2021). Are elite track and field athletes on track? The impact of COVID-19 outbreak on sleep behavior and training characteristics. Biol. Sport 38, 741–751. doi: 10.5114/biolsport.2021.109950
Werneck, G. L., and Carvalho, M. S. (2020). A pandemia de COVID-19 no Brasil: crônica de uma crise sanitária anunciada. Cad. Saúde Pública 36, e00068820. doi: 10.1590/0102-311x00068820
Wilms, P., Schröder, J., Reer, R., and Scheit, L. (2022). The impact of “home office” work on physical activity and sedentary behavior during the COVID-19 pandemic: a systematic review. Int. J. Environ. Res. Public Health 19, 12344. doi: 10.3390/ijerph191912344
Wunsch, K., Kienberger, K., and Niessner, C. (2022). Changes in physical activity patterns due to the covid-19 pandemic: a systematic review and meta-analysis. Int. J. Environ. Res. Public Health 19, 2250. doi: 10.3390/ijerph19042250
Zinner, C., Matzka, M., Leppich, R., Kounev, S., Holmberg, H.-C., and Sperlich, B. (2020). The impact of the german strategy for containment of coronavirus SARS-CoV-2 on Training characteristics, physical activity and sleep of highly trained kayakers and canoeists: a retrospective observational study. Front. Sports Active Living 2, 579830. doi: 10.3389/fspor.2020.579830
Keywords: COVID-19, lockdown, physical activity, sleep, wearables, elite athletes, healthy adults
Citation: Cui D, Zhang X and Guo J (2023) The impact of the COVID-19 pandemic on physical activity and sleep among healthy adults: a systematic review and meta-analysis. Front. Psychol. 14:1149215. doi: 10.3389/fpsyg.2023.1149215
Received: 21 January 2023; Accepted: 02 June 2023;
Published: 29 June 2023.
Edited by:
Xiao Hou, Beijing Sport University, ChinaReviewed by:
Zihong He, China Institute of Sport Science, ChinaKuan Tao, Beijing Sport University, China
Sitong Chen, Victoria University, Australia
Copyright © 2023 Cui, Zhang and Guo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dandan Cui, ditto9@gmail.com
†These authors have contributed equally to this work
 Dandan Cui
Dandan Cui Xiangning Zhang
Xiangning Zhang Jianwei Guo
Jianwei Guo