- 1MSB Medical School Berlin, Berlin, Germany
- 2Institute for Psychosocial Prevention, Heidelberg University, Heidelberg, Germany
Background: Since the outbreak of COVID-19 pandemic, psychological distress is increased. Transdiagnostic mechanisms, including trauma, personality functioning, mentalizing and emotion regulation are considered relevant to the development and maintenance of mental health problems and therefore may play a role in individuals’ reactions to the pandemic.
Aim: To identify moderating and mediating factors associated with pandemic-related distress and mental health problems in adults and families, we aim to investigate the interactions of interpersonal trauma (childhood trauma and domestic violence), psychological capacities (personality functioning, mentalizing and emotion regulation) and pandemic-related adversity on psychological distress during the COVID-19 pandemic. Furthermore, we aim to investigate behavioral and cognitive consequences of the pandemic (e.g., media consumption, vaccination status, conspiracy beliefs).
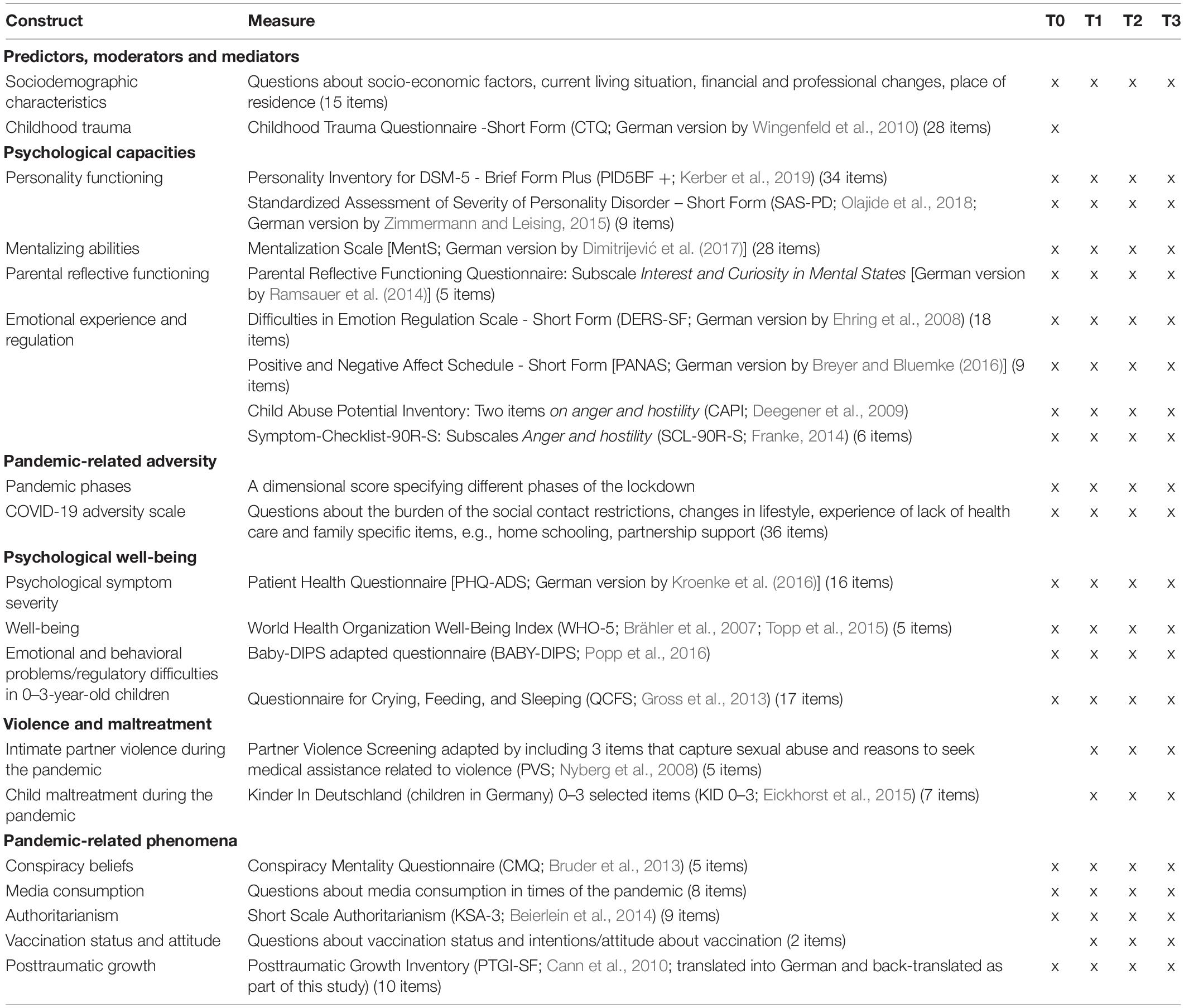
Methods: Using an online-based cross-sectional and longitudinal design, we will investigate a sample of adult participants recruited via online platforms in German-speaking countries over the course of 1 year with four measurements points via self-report instruments (personality functioning: PID5BF +; mentalizing: MentS, PRFQ; emotion regulation: DERS-SF; mental health problems: PHQ-9, GAD-7; a composite pandemic-related stress score). Structural equation and multi-level modeling will be performed for data analyses.
Implications: This study will provide data on the moderating and mediating effects of trauma, personality functioning and mentalizing during the pandemic in a large community sample, particularly on vulnerable groups like families. Identifying transdiagnostic mechanisms of psychopathology in the course of a pandemic crisis may provide valuable insight for the development of pre- and intervention measures for potential psychological distress during and post the pandemic.
Introduction
The current COVID-19 pandemic has a massive impact on all people’s life’s including individual, family related, societal, economic and financial hardship, social and cultural deprivation, and educational disadvantages (e.g., Kujawa et al., 2020).
A number of studies examined the psychological impact of the COVID-19 pandemic showing that psychological distress is generally increased across populations worldwide (e.g., Salari et al., 2020; Wu et al., 2020). In Europe, several studies have shown an increase in psychological distress related to the pandemic (Pierce et al., 2020; Rodríguez-Rey et al., 2020; Rossi et al., 2020). Studies from Germany, in particular, are also in line with international findings, showing for example significantly higher levels of depression, anxiety and increased psychological distress in the general population during the pandemic and specifically during lockdown phases (Bäuerle et al., 2020; Benke et al., 2020; Petzold et al., 2020). Studies have found a number of factors associated with psychological distress during the pandemic, namely being in quarantine, loneliness, worries about infections or death of important others, unemployment and housework, as well as social and financial consequences of the pandemic (Benke et al., 2020; Chandola et al., 2020; Rodríguez-Rey et al., 2020; Rossi et al., 2020).
Vulnerable populations, like families with young children are particularly affected during the pandemic (Pierce et al., 2020). Factors that have been identified to be associated with families’ psychological distress are their life circumstances (for example work- and learning spaces at home) (Pierce et al., 2020), financial anxiety and lack of social support. While the burden is higher in those families with younger children and those with two or more children (Mazza et al., 2020; Li et al., 2020), the impact on the mental health of young children, i.e., infants and toddlers, has been less investigated. Furthermore, several studies found an increase in intimate partner violence and child maltreatment since the COVID-19 pandemic (e.g., Brown et al., 2020; Jetelina et al., 2021). Decreased service utilization, other COVID-19 related stressful events, and increased parental psychological symptoms were also related to higher child abuse potential (Brown et al., 2020; Lawson et al., 2020). However, so far little is known about psychological risk and protective factors of families, which may amplify or buffer the potential effect from COVID-19 related adversities and parental distress on risk of child abuse.
Drawing on existing transdiagnostic models of childhood trauma and psychopathology (McLaughlin et al., 2020), and mentalizing (Luyten et al., 2020), we aim to expand this to the understanding of the psychosocial impact of the pandemic. Thereby, we aim to investigate the relationship of childhood trauma, psychological capacities including personality functioning, emotional awareness and regulation, and mentalizing abilities on the psychosocial impact of the pandemic. Social risk factors like younger age, female gender or unemployment, in addition to families with young children, have been shown to play an important role in experiencing increased psychological distress during the pandemic (Horesh and Brown, 2020; Xiong et al., 2020). Fewer studies have focused on factors such as a history of traumatic experiences or personality factors (e.g., Fernández et al., 2020). In the following, we briefly outline the evidence based on these hypothesized risk and protective factors with regard to mental health problems and summarize current findings on the pandemic impact:
A history of interpersonal childhood trauma (for example physical, sexual, and emotional abuse or neglect) is associated with a higher risk for a psychopathological development later in life (Felitti et al., 1998; Mandelli et al., 2015). With regard to pandemic-related impacts on mental health, Guo et al. (2020) found that adolescents with pre-pandemic traumatic experiences were associated with increased anxiety during the pandemic, and Kim et al. (2020) found a moderating effect of early childhood trauma on the association between the perceived risk from COVID-19 and depression. Hence, experiences of childhood trauma may be understood as a vulnerability factor for psychopathology during the pandemic.
Personality functioning, conceptualized as basic psychological capacities of a person have an understanding and regulation abilities of the self of relationships with others, is considered a key factor to develop and maintain mental health (Kernberg and Caligor, 2005; Bender et al., 2011). With regard to the pandemic, a disposition toward internalizing personality traits (including negative affectivity, detachment, closed-mindedness and psychoticism), were associated with increased levels of depression, anxiety and stress during the pandemic (Mazza et al., 2020; Biondi et al., 2021) and elevated levels of negative affectivity were found to contribute to lower resilience and reduced subjective well-being (Kocjan et al., 2021).
Mentalizing - the basic human capacity to conceive oneself and others as intentional beings whose actions are guided by feelings, thoughts, desires, attitudes, and goals (Fonagy et al., 2002) - is implicated in a number of mental health problems and disorders (Luyten et al., 2020) and can be understood as an adaptive psychological mechanism for coping with pandemic-related stressors. In a similar vein, parents’ ability to mentalize their child may be a protective factor against the adverse effects of pandemic-related stress on the child because parents are able to co-regulate their child more effectively according to its needs (Zeegers et al., 2017). So far, very few empirical studies have investigated pandemic-related effects on mentalizing abilities (Lassri and Desatnik, 2020; Ventura Wurman et al., 2020) and none of the studies focused on mentalizing as a risk or protective factor in the general population or families.
Furthermore, an individual’s ability to experience and regulate emotions is also considered highly relevant to develop and maintain mental health (e.g., Aldao et al., 2010; Hu et al., 2014). According to Gratz and Roemer (2004) the concept of emotional (dys-)regulation comprises (a) the ability to identify and understand emotions, (b) the acceptance of emotions, (c) the potential to exhibit goal-directed behavior and control impulsive behavior even while exposed to negative emotions or stress, and (d) the ability to flexibly use situationally appropriate emotion regulation strategies to achieve individual goals (Kaufman et al., 2016). A recent study examining emotional dysregulation during the pandemic found that having survived a Covid-19 infection was associated with a greater likelihood of psychological distress, and this in turn was associated with greater emotional dysregulation as well as elevated levels of depressive mood (Janiri et al., 2020). Moreover, the concept may be of particular relevance to family’s mental health during the pandemic, as parents’ emotional dysregulation problems have been shown to be related to children’s stress reactions (Shorer and Leibovich, 2020). Young children of parents with deficits in emotion regulation may be at a heightened risk during the pandemic to experience less adaptive co-regulation and thus may show more mental health problems (e.g., regulatory symptoms).
According to transdiagnostic models of the development of mental health problems, interactions between interpersonal trauma, psychological capacities and other factors exist and are to some extend supported by empirical data. For example, Abdi and Pak (2019) found that the effect of maladaptive personality traits and low personality functioning on mental health problems was mediated by emotion dysregulation. Moreover, emotion dysregulation (Cloitre et al., 2019) as well as mentalizing (Huang et al., 2020) are found to serve as mediating factors in the relationship between childhood trauma and psychopathology. These findings indicate the extent to which psychological capacities can have a mediating influence on a psychopathological development against the background of traumatic experiences in early childhood.
Furthermore, the behavioral and cognitive consequences of the pandemic such as increasing media consumption, authoritarianism, conspiracy beliefs, vaccination status and attitude, and posttraumatic growth need to be considered, if we want to advance our understanding about maintaining and losing mental health in a global crisis. Recent studies have shown a new rise in people’s vulnerability to conspiracy beliefs during the pandemic (Šrol et al., 2020; Leibovitz et al., 2021; Oleksy et al., 2021). Dyrendal et al. (2021) identified right-wing authoritarianism within their analysis as one predictor of conspiracy theories. Hartman et al. (2020) also showed a correlation between COVID-19-specific conspiracy beliefs (i.e., that the virus originated on a Chinese laboratory) and a political attitude toward right-wing authoritarianism. These results are also supported by Prichard and Christman (2020), who found that authoritarianism was not only a predictor of less concern about the COVID-19 virus and low compliance, but also associated with the belief that the virus had been produced in China. Moreover, this COVID-19 pandemic may also be regarded an infodemic, in which the overabundance of information, individuals’ increased media consumption and deliberate attempts to disseminate wrong information effects people’s psychological capacities and mental health (Cellini et al., 2020; Valdez et al., 2020; World Health Organization [WHO], 2020, September 23). At the same time, people may also be able to cope with the crisis in a positive way and develop posttraumatic growth as a result of the pandemic (e.g., Vazquez et al., 2021).
Rationale and Aim of This Study
Based on the research outlined above, we aim to investigate a multi-factorial and transdiagnostic model of risk and protective factors associated with pandemic-related distress and psychological impairments in adults and families in the general German-speaking population during the COVID-19 pandemic in a cross-sectional and 1-year longitudinal study. In particular, the effects and complex interactions of interpersonal trauma- namely childhood trauma and domestic violence- psychological capacities- namely personality functioning, mentalizing and emotion regulation- and pandemic-related adversity on psychological distress in adults and families will be investigated. Furthermore, we aim to exploratorily investigate behavioral and cognitive consequences of the pandemic including vaccination status and attitude, media consumption, authoritarianism and conspiracy beliefs, as well as violence, maltreatment and posttraumatic growth during the pandemic.
Research Questions
Main Research Questions Cross-Sectional Data
(1) Is there a relationship between pandemic-related adversity and psychological distress?
(1.1) Is pandemic-related adversity a predictor of psychological distress?
(2) Is there a relationship between childhood trauma, psychological capacities and pandemic-related adversity and psychological distress in adults and families?
(2.1) Is the relationship between pandemic-related adversity and psychological distress moderated by childhood trauma?
(2.2) Is the relationship between pandemic-related adversity and psychological distress mediated by psychological capacities (personality functioning, mentalizing, emotional experience and regulation)?
(2.3) Is the relationship between pandemic-related adversity and psychological distress as well as infant/toddler regulatory problems mediated by parental psychological capacities (parental mentalizing, emotional experience and regulation)?
(2.4) Is the relationship between pandemic-related adversity and psychological distress moderated by childhood trauma and mediated by psychological capacities (personality functioning, mentalizing, emotional experience and regulation)?
Main Research Questions Longitudinal Data
(3) Is there a relationship between changes in pandemic-related adversity and psychological distress in course of the 1-year longitudinal study?
(4) Is there a relationship between childhood trauma, changes in psychological capacities and pandemic-related adversity and changes in psychological distress over time?
(4.1) Is the relationship between changes in pandemic-related adversity and psychological distress predicted by childhood trauma?
(4.2) Is the relationship between changes in pandemic-related adversity and psychological distress mediated by changes in psychological capacities (personality functioning, mentalizing, emotional experience and regulation)?
(4.3) Is the relationship between changes in pandemic-related adversity and psychological distress as well as infant/toddler regulatory problem problems mediated by changes in parental psychological capacities (parental mentalizing, emotional experience and regulation)?
(4.4) Is the relationship between changes in pandemic-related adversity and psychological distress predicted by childhood trauma and mediated by changes in psychological capacities (personality functioning, mentalizing, emotional experience and regulation)?
(5) Is there a relationship between changes in parental psychological capacities, pandemic-related adversity and violence and maltreatment during the pandemic?
(5.1) Is the relationship between changes in pandemic-related adversity, violence and maltreatment during the pandemic mediated by changes in psychological capacities (parental reflective functioning, emotional experience and regulation)?
Additionally, further exploratory analyses with regard to the relationship between psychological capacities, pandemic-related adversity, psychological well-being and pandemic-related phenomena including conspiracy beliefs, media consumption, authoritarianism and vaccination status and attitudes will be conducted.
Method
A cross-sectional and longitudinal study of the relationship between childhood trauma, personality functioning, mentalizing ability, pandemic-related stressors, and psychological distress will be conducted. The survey will be conducted online using the SoSci Survey platform. Ethic approval has been obtained from the local ethics board (Heidelberg University; AZ Tau 2020 3/1). The first measurement period (t0) began in August 2020 and continued through February 2021. After the first survey period t0, three additional follow-up surveys will be conducted at 3-months intervals. The first follow-up survey (t1) started in November 2020 and ended in May 2021. The second follow-up survey (t2) started in February 2021 and will end in August 2021. The third follow-up survey (t3) started in May 2021 and will end in November 2021. Figure 1 illustrates the study design with time measurement points.
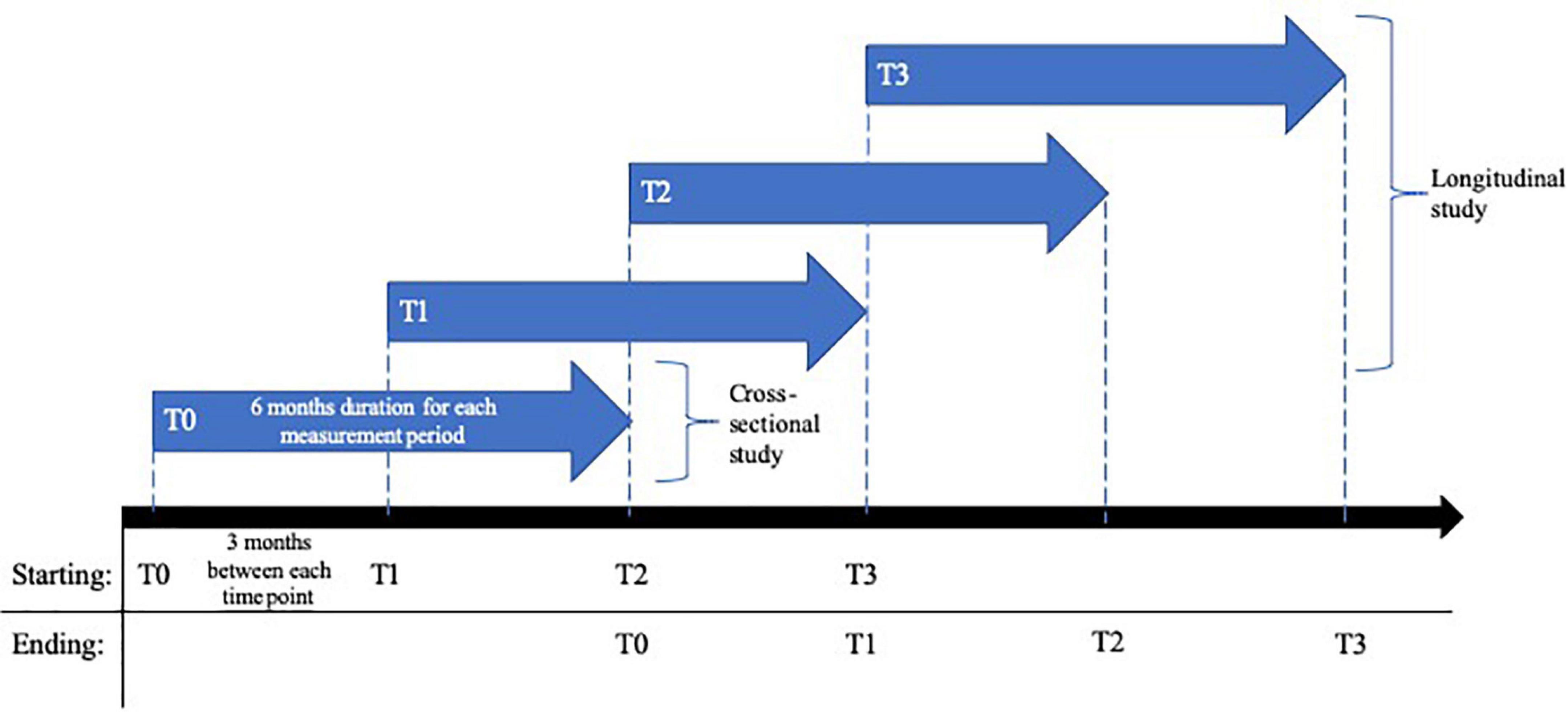
Figure 1. Design of the cross-sectional and 1-year longitudinal study on risk and protective factors of the psychosocial impact during the COVID-19 pandemic in Germany.
Sample
Adults over 18 years of age will be included. Aiming at a sample size of N = 800 at the last time point after 9 months and considering a drop-out rate of approx. 35% per time point (cf., Kujawa et al., 2020), appr. N = 3,000 adults (cross-sectional study) need to be included.
Participants will be recruited via the Institute for Psychosocial Prevention at Heidelberg University Hospital, via online and social media platforms (including Facebook, Instagram, Twitter, and Reddit), e-mails, and print flyers. Recruitment strategies are designed to reach a diverse population of German-speaking adults, with a focus on populations that may be particularly affected by the pandemic (including participants working in system-relevant occupations and families). Therefore, we particularly target respective groups on social media platforms (e.g., parent groups and forums) while we also recruit in more general groups/forums (e.g., COVID-19 related groups, sport clubs, and universities nationwide). Although our strategy aims at including a diverse population, participants’ characteristics will be analyzed for oversampling younger and better educated participants.
Measures
Table 1 includes an overview of all measures used in the study and their respective assessment time point.
Predictors, Moderators and Mediators
Sociodemographic Characteristics
At baseline general sociodemographic data using a standardized questionnaire including information about age, gender, educational and occupational background, and socio-economic situation will be collected and data about changes in sociodemographic background is collected at all follow-up timepoints.
Childhood Trauma
The childhood trauma questionnaire (CTQ; German version: Wingenfeld et al., 2010) is a 28-item retrospective self-report measure that is divided into five subscales to assess different aspects of maltreatment experiences in childhood: emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect. Each subscale consists of five statements, which can be rated with a five- point Likert Scale (1 = not at all; 5 = very often). Three additional items measure the individual’s tendency to minimize and deny. The subscale-scores range from 5 to 25 and the total score ranges from 25 to 125, with higher points indicating a greater extent of maltreatment. For each subscale specific cutoffs indicate the frequency of exposure. Strong psychometric properties have been demonstrated for the CTQ in clinical as well as community samples (Scher et al., 2001). The German version showed similar properties to the original version and demonstrated to be reliable and valid (Wingenfeld et al., 2010).
Psychological Capacities
Personality functioning
The PID-5 Brief Form + (PID5BF +; Kerber et al., 2019) is a brief self-report measure for assessing the six pathological trait domains described in AMPD criterion B and the ICD-11: negative affectivity, detachment, antagonism/dissociality, disinhibition, anankastia and psychoticism. Items are rated on a four-point scale ranging from 0 (“very false or often false”) to 3 (“very true or often true”). The internal consistency of the domain scores in three large samples was high (mean McDonald’s ω = 0.81), and domain scores were substantially positively correlated with each other.
The Standardized Assessment of Severity of Personality Disorder (SASPD; Olajide et al., 2018; German version: Zimmermann and Leising, 2015) is a brief measure to assess the severity of a potential personality disorder (PD) according to ICD-11 (Olajide et al., 2018). It consists of a total of nine items relating to different life domains and skills such as friendships, self-control, or compassion. Respondents can choose between four statements, which can then be recoded into a four-point scale according to the severity of a potential personality disorder (0 = Non-existent, 1 = Mild, 2 = Moderate and 3 = Severe). However, studies that addressed the validation of the SASPD found that the SASPD total score may be more useful as an indicator of a complex and heterogeneous mix of PD characteristics rather than actually representing severity (Rek et al., 2020). The SASPD nonetheless shows acceptable internal consistency in both clinical (ω = 0.78) and non-clinical (ω = 0.70) samples (Rek et al., 2020).
Mentalizing Abilities
The Mentalization Ability Assessment Questionnaire (MentS; Dimitrijević et al., 2018; German version: D-MentS by Dimitrijević et al., 2017) is a self-report questionnaire with 28 items to assess mentalization in clinical and healthy populations. Items are rated on a five-point scale (1 = “strongly disagree” to 5 “strongly agree”). The questionnaire consists of three subscales: MentS-A (10 items) captures mentalizing in relation to the other; MentS-S (8 items) captures mentalizing in relation to the self; and MentS-M (10 items) captures motivation to mentalize. A sum score maps the total mentalizing abilities score. Internal consistencies are acceptable in clinical and healthy populations and validity is adequately ensured (Dimitrijević et al., 2017).
Parental Reflective Functioning
We used the interest and curiosity in mental states scale of the German version of the Parental Reflective Functioning Questionnaire [PRFQ by Ramsauer et al. (2014); Luyten et al. (2017)] to assess parental reflective functioning. The scale consists of six items and assesses a parents’ proclivity to be interested in the child’s mental states. Items are rated on a seven-point Likert scale ranging from strongly disagree to strongly agree. The PRFQ reliably and validly assessed parental reflective functioning (Luyten et al., 2017; Anis et al., 2020).
Emotional Experience and Regulation
The Difficulties in Emotion Regulation Scale- Short Form (DERS-SF; German version: Ehring et al., 2008) is a 18-item self-report measure to assess emotional dysregulation across six domains: non-acceptance of emotional responses, lack of emotional awareness, limited access to ER strategies, lack of emotional clarity, difficulties engaging in goal-directed behavior, and impulse control difficulties when experiencing negative emotions. Participants rate the frequency with which the 18 statements apply to themselves by choosing from a five-point Likert-type scale. The items were recoded, with higher scores for each item and a higher overall score indicating more deficits in emotional dysregulation. The original version of the DERS showed high internal consistency (α = 0.93), good test-retest reliability, and adequate constructive and predictive validity (Gratz and Roemer, 2004). The German version of the DERS also demonstrated adequate to good internal consistencies within the original sample (0.76 < α < 0.87; Ehring et al., 2008).
The Positive and Negative Affect Schedule (PANAS; Janke and Glöckner-Rist, 2014) captures various feelings and emotions consisting of 20 items. With ten items each, the dimensions of positive and negative affect are captured on a 5-point Likert scale with response options “not at all” to “extremely.” Reliability assessment good Cronbach’s α values of 0.86 for the two dimensions of positive and negative affect (Janke and Glöckner-Rist, 2014).
Symptomatic anger was assessed using the anger/hostility subscale of the Symptom-Checklist-90 (SCL-90R-S; Franke, 2014). Six items are rated on a five-point Likert scale from 0 (not at all) to 4 (extremely) with higher scores indicating higher distress. The subscale has demonstrated sufficient internal consistency (α = 0.79; Franke, 2014).
In addition, two items from the German of the Child Abuse Potential Inventory (CAPI; Deegener et al., 2009) were utilized to assess general anger/hostility (English translation of the German version: “I am often angry inside”; “Many things in my life make me angry”). Items are rated on a four-point Likert scale. The CAPI is a valid and reliable inventory to determine the degree of stress of parents or other primary caregivers to assess the risk of child endangerment and abuse (Milner, 1994). Internal consistency (α = 0.91) is high (Deegener et al., 2009).
Pandemic-Related Adversity
Pandemic Phases
A dimensional score specifying different phases of the lockdown will be calculated. The score will be calculated based on the specific lockdown phase present at the assessment timepoint of each individual participant.
COVID-19 Adversity Scale
This summative score, developed as part of the project, is composed of items that are classified as stressful in the context of the COVID-19 pandemic. These include e.g., pandemic-related adversity experienced due to social contact restrictions, changes in life style (incl. activities, nutrition, exercise) and experience of lack of access to health care due to the pandemic. The COVID-19 adversity scale for families additionally covers experiences relevant to families and partnership support (incl. homeschooling, co-parenting). The conceptually derived scales (e.g., Benke et al., 2020; Kujawa et al., 2020; Rossi et al., 2020) will be empirically validated using confirmatory factor analyses.
Outcomes
Psychological Distress
Psychological Symptom Severity
The Patient Health Questionnaire (PHQ-D; German version: Löwe et al., 2008) represents a widely used, valid screening instrument based on the DSM-IV for the diagnosis of mental disorders. In order to assess psychological distress, the depression module (PHQ-9) with nine items and the module on generalized anxiety (GAD-7; English original version: Spitzer et al., 2006; German translation and validation: Löwe et al., 2008) with seven items are used in this study. Both modules are answered on a four-point scale (0 = “not at all” to 3 = “almost every day”) and are characterized by high validity, good internal consistencies (PHQ-9: α = 0.88; GAD-7: α = 0.89) and, especially for the depression module, by a high sensitivity to change (Gräfe et al., 2004; Löwe et al., 2008).
Regulatory Problems in Infants/Toddlers
Regulatory problems, which include excessive crying, sleep-onset, and night waking problems were assessed by parental report utilizing four screening items based on the structured diagnostic interview for regulatory problems in infancy (BABY-DIPS; Popp et al., 2016) and frequency and duration criteria of the Diagnostic Classification System DC:0-3R (Zero to Three, 2005). In addition, regulatory problems and related parental burden were assessed dimensionally utilizing 13 items from the Questionnaire for Crying, Feeding, and Sleeping (QCFS), which has been shown to be a valid measure for clinically significant regulatory disorders (Gross et al., 2013). Items are rated on a four-point Likert scale from never/rarely to always/every day. Higher scores signify more regulatory problems across all areas. Both instruments validly and reliably assess regulatory problems in infancy.
Further Secondary Outcomes
Psychological Well-being
Well-being
The German short version of the World Health Organization Well-Being Index (WHO-5; Brähler et al., 2007; Topp et al., 2015) consists of five items that refer to the well-being within the past 2 weeks. The response options are positively worded and refer to participants’ mood, calmness and relaxation, as well as perceived vitality, activity, restfulness of sleep and interest in things of daily living (Simon, 2017). The evaluation of the answers is recorded via a six-point Likert scale (0 = at no time; 5 = all the time). For scoring, the response scores of the five items are added together. The raw scores vary from 0 to 25 points, with a score of 0 being interpreted as the lowest psychological well-being and lowest quality of life, and a score of 25 being interpreted as the highest psychological well-being and highest quality of life. A score of <13 points is recommended as a cut-off criterion for poor psychological well-being. The internal consistencies of the test can be assessed as good with α = 0.88 (cf. α ≥ 0.89; Brähler et al., 2007; Döring and Bortz, 2016).
Violence and Maltreatment
Intimate Partner Violence During the Pandemic
The modified Partner Violence Screen (PVS, Nyberg et al., 2008) was used to assess exposure to partner violence during the last 12 months and particularly, since the beginning of the pandemic. The original PVS (Feldhaus et al., 1997) consists of three items that capture physical abuse and perceptions of safety. It has been translated to German and adapted by Nyberg et al. (2008) by including two items that capture sexual abuse and reasons to seek medical assistance related to violence. The measure has shown a sensitivity of 0.80 and a specificity of 0.78 (Nyberg et al., 2008). In this study, the PVS was modified in order to screen for violence against a partner of either gender and the item on medical assistance has been deleted due to the context of our study which does not provide crisis intervention.
Child Maltreatment During the Pandemic
We assessed child maltreatment and violence among parents with 7 items stemming from a nationwide survey on young families in Germany (KID 0-3; Eickhorst et al., 2015). The items cover instances of child abuse and neglect (e.g., “Has your child been shaken or pushed against a wall by an adult?”) and instances of partner violence (e.g., “Has one parent threatened the other parent seriously?”). All items are assessed dichotomously (yes/no). We asked participants to answer whether instance occurred before or since the beginning of the pandemic or both. The measure has been successfully used to assess child maltreatment in German young families.
Pandemic-Related Phenomena
Conspiracy Beliefs
The Conspiracy Mentality Questionnaire (CMQ) by Bruder et al. (2013) is an instrument that captures the conspiratorial mentality as a one-dimensional construct. On an eleven-point scale with a range from: 0% “certainly not” to 100% “certain” with a total of five-items, a generic conspiracy conviction is shown. The internal consistency of the questionnaire has been calculated and showed “good” results of Cronbach‘s Alpha for the German language version (α = 0.84). In addition, the model indices showed a very good fit (CFI > 0.95, RMSEA < 0.06), as well as factor loadings of >0.50. Furthermore, the test-retest-reliability in a 2-week interval was also satisfactory.
Media Consumption
Participants are asked about their media usage (e.g., type of newspapers, social media platforms, YouTube channels or podcasts) and indicate, which media they have used to obtain information about the Covid-19 pandemic.
Authoritarianism
The short scale authoritarianism (KSA-3) by Beierlein et al. (2014) is an economic instrument for assessing authoritarianism with its three sub-dimensions (aggression, submission and conventionalism). The scale comprises a total of nine items, with three items per sub-dimension. Those are rated on a five-point rating scale with a range from: (1) completely disagree to (5) completely agree. The factorial validity shows model indices of CFI = 0.962, RMSEA = 0.067, and SRMR = 0.043, which can be classified as satisfactory. Furthermore, factor loadings of all items on the scale (>0.50) and the three sub-dimensions on the general factor authoritarianism were shown. Using the McDonald ω coefficient, the reliability of the scales was determined, showing sufficient reliabilities of the three sub-dimensions of ω = 0.86 for authoritarian aggression, ω = 0.74 for authoritarian subservience, ω = 0.78 for conventionalism.
Posttraumatic Growth Inventory
Posttraumatic Growth Inventory (PTGI-SF; Cann et al., 2010) is the short form of the Posttraumatic Growth Inventory from Tedeschi and Calhoun (1996) and comprises 10 items about the positive outcomes of traumatic experiences. The five domains include New Possibilities, Relating to Others, Appreciation of Life, Spiritual Change and Personal Strength are measured with two items for each subscale. The calculation of the reliability has shown sufficient results (α = 0.90). Also, the Fit indices indicate a good fit (CFI = 0.965; RMSEA = 0.072). We adapted the instructions in order to assess posttraumatic growth related to the pandemic.
Vaccination Status and Attitude
We have included two questions about COVID-19 vaccination status of the participant and their close relatives as well as their motivation their general attitude toward COVID-19 vaccination.
Statistical Analysis
Data within individual timepoints will be assessed for missing data and patterns of missingness. For missing at random data, we will conduct multiple imputation by chained equations (MICE) using the R package mice (Groothuis-Oudshoorn and Van Buuren, 2011). We will use predictive mean matching (Little, 1988) as imputation algorithm, since it is moderately robust when the empirical data deviate from distributional assumptions (Kleinke, 2017). Cross-sectional analysis: To answer research questions 1 to 2.4 on the association between childhood trauma, psychological capacities, pandemic-related adversity and psychological distress structural equation modeling will be applied for the cross-sectional data analyses. Longitudinal analysis: To answer the research questions 3 to 6.1 on the moderating and mediating effect of the named risk and protective factors regarding the relationship of pandemic-related adversity and psychological distress as well as potential associated pandemic-related phenomena, the data analyses of the longitudinal correlations are performed using multilevel modeling with measurement time points (level 1) nested in subjects (level 2). Here, changes in psychological distress at Level 1 is predicted by pandemic-related distress factors and linear time, as well as potential covariates (including age, gender). Psychological capacities are introduced as a mediator at Level 1. Analyses will be conducted using the Lavaan and semPlot-packages of the statistical software R.
Discussion
This paper describes the study protocol of a cross-sectional and longitudinal study on risk and protective factors of mental health during the COVID-19 pandemic. To the best of the authors’ knowledge, this is the first study of its kind that investigates the moderating and mediating role of traumatic experiences and psychological capacities during the pandemic in a large community sample with a particular focus on families using a longitudinal design.
By expanding and testing the existing transdiagnostic models of childhood trauma and psychopathology (McLaughlin et al., 2020), and mentalizing (Luyten et al., 2020), this study will make an important contribution to a better understanding of risk and protective factors of mental health in the course of a worldwide pandemic crisis and the experience of related adverse events. Furthermore, the longitudinal examination of psychological capacities like personality functioning, mentalizing skills and emotion regulation in the relationship between pandemic-related stressors and psychological stress experience may provide valuable information for the development of pre- and intervention measures for potential psychological stress experience during and post the pandemic.
The strengths of this study include the broad and comprehensive recruitment approach, the investigation of theoretically grounded risk and protective factors of mental health during the COVID-19 crisis, in particular investigating a vulnerable population of families with young children.
Limitations of this study include a strategy that is primarily limited to online recruitment, which may potentially exclude individuals, who do not access these online platforms. Moreover, this sample is self-selected and will not be representative for the larger general population of Germany or Europe.
In addition, the survey is long and may attract only highly motivated individuals. Thus, our results will contribute to identifying risk and protective factors which, however, we cannot claim to be representative for the general population. In case of a large drop-out in the follow-up assessments, the sample will further suffer from self-selection processes. However, we will assess demographic characteristics in the follow-up surveys in order to accurately describe the sample in these aspects and will take on control measures for oversampling younger and better educated participants. Another limitation is the use of only self-report assessments, which may result in response biases and are limited to contents that are consciously processable. Finally, although we aim to assess pandemic-related adversity operationalized by including pandemic phases as well as a COVID-19 adversity scale retrospectively, the lack of pre-pandemic data limits our data validity regarding immediate effects caused by the pandemic-related restrictions and measures on mental health.
In light of the massive global psychological impact of the pandemic, this study with a strong focus on intra- and interpersonal psychological risk and protective factors will be of direct relevance to the evaluation of how pandemic measures affect vulnerable populations but also to the development of mental health and preventive services during and after the pandemic.
Author Contributions
JV drafted the current manuscript. AB, LK, HW, JH, AG, and ST revised, corrected, and finally approved. All authors provided a substantial contribution to the conception and design of the work by developing the research question, study design, methodology, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work were appropriately investigated and resolved.
Funding
This study was funded by the German Association of Psychoanalysis (Deutsche Gesellschaft für Psychoanalyse; DPG).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abdi, R., and Pak, R. (2019). The mediating role of emotion dysregulation as a transdiagnostic factor in the relationship between pathological personality dimensions and emotional disorders symptoms severity. Person. Individ. Differ. 142, 282–287. doi: 10.1016/j.paid.2018.09.026
Aldao, A., Nolen-Hoeksema, S., and Schweizer, S. (2010). Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin. Psychol. Rev. 30, 217–237. doi: 10.1016/j.cpr.2009.11.004
Anis, L., Perez, G., Benzies, K. M., Ewashen, C., Hart, M., and Letourneau, N. (2020). Convergent validity of three measures of reflective function: parent development interview, parental reflective function questionnaire, and reflective function questionnaire. Front. Psychol. 11:3385. doi: 10.3389/fpsyg.2020.574719
Bäuerle, A., Teufel, M., Musche, V., Weismüller, B., Kohler, H., Hetkamp, M., et al. (2020). Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J. Public Health 42, 672–678. doi: 10.1093/pubmed/fdaa106
Beierlein, C., Asbrock, F., Kauff, M., and Schmidt, P. (2014). Die Kurzskala Autoritarismus (KSA-3): Ein ökonomisches Messinstrument zur Erfassung Dreier Subdimensionen Autoritärer Einstellungen. Mannheim: GESIS – Leibniz Institut für Sozialwissenschaften.
Bender, D. S., Morey, L. C., and Skodol, A. E. (2011). Toward a model for assessing level of personality functioning in DSM–5, part I: a review of theory and methods. J. Person. Assessment 93, 332–346. doi: 10.1080/00223891.2011.583808
Benke, C., Autenrieth, L. K., Asselmann, E., and Pané-Farré, C. A. (2020). Lockdown, quarantine measures, and social distancing: associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatry Res. 293:113462. doi: 10.1016/j.psychres.2020.113462
Biondi, S., Casale, S., Burrai, J., Mazza, C., Cavaggioni, G., Ferracuti, S., et al. (2021). Personality and lockdown: a study on italian undergraduates during the COVID-19 pandemic. Front. Psychiatry 12:622366. doi: 10.3389/fpsyt.2021.622366
Brähler, E., Mühlan, H., Albani, C., and Schmidt, S. (2007). Teststatistische Prüfung und normierung der deutschen Versionen des EUROHIS-QOL lebensqualität-index und des WHO-5 wohlbefindens-index. Diagnostica 53, 83–96. doi: 10.1026/0012-1924.53.2.83
Breyer, B., and Bluemke, M. (2016). Deutsche version der positive and negative affect schedule PANAS (GESIS panel) [German version of the positive and negative affect schedule PANAS]. Zusammenstellung Sozialwissenschaftlicher Items und Skalen (ZIS). doi: 10.6102/zis242
Brown, S. M., Doom, J. R., Lechuga-Peña, S., Watamura, S. E., and Koppels, T. (2020). Stress and parenting during the Global COVID-19 Pandemic. Child Abuse Negl. 110:104699. doi: 10.1016/j.chiabu.2020.104699
Bruder, M., Haffke, P., Neave, N., Nouripanah, N., and Imhoff, R. (2013). Measuring individual differences in generic beliefs in conspiracy theories across cultures: conspiracy mentality questionnaire. Front. Psychol. 4:225. doi: 10.3389/fpsyg.2013.00225
Cann, A., Calhoun, L. G., Tedeschi, R. G., Taku, K., Vishnevsky, T., Triplett, K. N., et al. (2010). A short form of the posttraumatic growth inventory. Anxiety Stress Coping 23, 127–137. doi: 10.1080/10615800903094273
Cellini, N., Canale, N., Mioni, G., and Costa, S. (2020). Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 29:e13074.
Chandola, T., Kumari, M., Booker, C. L., and Benzeval, M. (2020). The mental health impact of COVID-19 and lockdown-related stressors among adults in the UK. Psychol. Med. [Online ahead of print] 1–10. doi: 10.1017/S0033291720005048
Cloitre, M., Khan, C., Mackintosh, M. A., Garvert, D. W., Henn-Haase, C. M., Falvey, E. C., et al. (2019). Emotion regulation mediates the relationship between ACES and physical and mental health. Psychol. Trauma: Theory Res. Pract. Pol. 11:82. doi: 10.1037/tra0000374
Deegener, G., Spangler, G., Körner, W., and Becker, N. (2009). Eltern-Belastungs-Screening zur Kindeswohlgefährdung. Deutsche Form des Child Abuse Potential Inventory (CAPI) von Joel S. Milner. Göttingen: Hogrefe.
Dimitrijević, A., Hanak, N., Altaras Dimitrijević, A., and Jolić Marjanović, Z. (2018). The Mentalization Scale (MentS): a self-report measure for the assessment of mentalizing capacity. J. Person. Assessment 100, 268–280. doi: 10.1080/00223891.2017.1310730
Dimitrijević, A., Ristein, L., Licata, M., Hamburger, A., Altaras Dimitrijević, A., and Jolić Marjanović, Z. (2017). Validation of the German Version of the Mentalization Scale (D- MentS). Manuscript in Preparation.
Dyrendal, A., Kennair, L. E. O., and Bendixen, M. (2021). Predictors of belief in conspiracy theory: the role of individual differences in schizotypal traits, paranormal beliefs, social dominance orientation, right wing authoritarianism and conspiracy mentality. Person. Individ. Differ. 173:110645. doi: 10.1016/j.paid.2021.110645
Ehring, T., Fischer, S., Schnülle, J., Bösterling, A., and Tuschen-Caffier, B. (2008). Characteristics of emotion regulation in recovered depressed versus never depressed individuals. Person. Individ. Differ. 44, 1574–1584. doi: 10.1016/j.paid.2008.01.013
Eickhorst, A., Brand, C., Lang, K., Liel, C., Neumann, A., Schreier, A., et al. (2015). Die Prävalenzstudie, Kinder in Deutschland–KiD 0-3“zur erfassung von psychosozialen belastungen und frühen hilfen in familien mit 0-3-jährigen kindern: studiendesign und analysepotential. Soziale Passagen 7, 381–387. doi: 10.1007/s12592-015-0212-z
Feldhaus, K. M., Koziol-McLain, J., Amsbury, H. L., Lowenstein, S. R., and Abbott, J. T. (1997). Accuracy of 3 brief screening questions for detecting partner violence in the emergency department. JAMA 277, 1357–1361. doi: 10.1001/jama.1997.03540410035027
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study. Am. J. Prevent. Med. 14, 245–258. doi: 10.1016/S0749-3797(98)00017-8
Fernández, R. S., Crivelli, L., Guimet, N. M., Allegri, R. F., and Pedreira, M. E. (2020). Psychological distress associated with COVID-19 quarantine: latent profile analysis, outcome prediction and mediation analysis. J. Affect. Disord. 277, 75–84. doi: 10.1016/j.jad.2020.07.133
Fonagy, P., Gergely, G., Jurist, E. L., and Target, M. (2002). Affect Regulation, Mentalization, and the Development of the Self. London: Karnac Books.
Gräfe, K., Zipfel, S., Herzog, W., and Löwe, B. (2004). Screening psychischer Störungen mit dem “Gesundheitsfragebogen für Patienten (PHQ-D)”. Diagnostica 50, 171–181. doi: 10.1026/0012-1924.50.4.171
Gratz, K. L., and Roemer, L. (2004). Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J. Psychopathol. Behav. Assessment 26, 41–54. doi: 10.1023/B:JOBA.0000007455.08539.94
Groothuis-Oudshoorn, K., and Van Buuren, S. (2011). Mice: multivariate imputation by chained equations in R. J. Stat, Softw. 45, 1–67.
Gross, S., Reck, C., Thiel-Bonney, C., and Cierpka, M. (2013). Empirical basis of the questionnaire for crying, feeding and sleeping. Praxis Kinderpsychologie Kinderpsychiatrie 62, 327–347. doi: 10.13109/prkk.2013.62.5.327
Guo, J., Fu, M., Liu, D., Zhang, B., Wang, X., and van IJzendoorn, M. H. (2020). Is the psychological impact of exposure to COVID-19 stronger in adolescents with pre-pandemic maltreatment experiences? A survey of rural chinese adolescents. Child Abuse Negl. 110:104667. doi: 10.1016/j.chiabu.2020.104667
Hartman, T. K., Marshall, M., Stocks, T. V., McKay, R., Bennett, K. M., Butter, S., et al. (2020). Different conspiracy theories have different psychological and social determinants: comparison of three theories about the origins of the COVID-19 virus in a representative sample of the UK population. PsyArXiv [Preprints] doi: 10.31234/osf.io/mz5sw
Horesh, D., and Brown, A. D. (2020). Traumatic stress in the age of COVID-19: a call to close critical gaps and adapt to new realities. Psychol. Trauma: Theory Res. Pract. Pol. 12:331. doi: 10.1037/tra0000592
Hu, T., Zhang, D., Wang, J., Mistry, R., Ran, G., and Wang, X. (2014). Relation between emotion regulation and mental health: a meta-analysis review. Psychol. Rep. 114, 341–362. doi: 10.2466/03.20.PR0.114k22w4
Huang, Y. L., Fonagy, P., Feigenbaum, J., Montague, P. R., and Nolte, T. London Personality and Mood Disorder Research Consortium (2020). Multidirectional pathways between attachment, mentalizing, and posttraumatic stress symptomatology in the context of childhood trauma. Psychopathology 53, 48–58. doi: 10.1159/000506406
Janiri, D., Kotzalidis, G. D., Giuseppin, G., Molinaro, M., Modica, M., Montanari, S., et al. (2020). Psychological distress After Covid-19 recovery: reciprocal effects with temperament and emotional dysregulation. an exploratory study of patients over 60 years of age assessed in a post-acute care service. Front. Psychiatry 11:590135. doi: 10.3389/fpsyt.2020.590135
Janke, S., and Glöckner-Rist, A. (2014). “Deutsche Version der positive and negative affect schedule (PANAS),” in Zusammenstellung Sozialwissenschaftlicher Items und Skalen, eds S. Janke and A. Glöckner-Rist (Mannheim: GESIS), 6102.
Jetelina, K. K., Knell, G., and Molsberry, R. J. (2021). Changes in intimate partner violence during the early stages of the COVID-19 pandemic in the USA. Injury Prevent 27, 93–97. doi: 10.1136/injuryprev-2020-043831
Kaufman, E. A., Xia, M., Fosco, G., Yaptangco, M., Skidmore, C. R., and Crowell, S. E. (2016). The Difficulties in Emotion Regulation Scale Short Form (DERS-SF): validation and replication in adolescent and adult samples. J. Psychopathol. Behav. Assessment 38, 443–455. doi: 10.1007/s10862-015-9529-3
Kerber, A., Schultze, M., Müller, S., Rühling, R. M., Wright, A. G., Spitzer, C., et al. (2019). Development of a short and ICD-11 compatible measure for DSM-5 maladaptive personality traits using ant colony optimization algorithms. Assessment doi: 10.1177/1073191120971848
Kernberg, O. F., and Caligor, E. (2005). “A psychoanalytic theory of personality disorders,” in Major Theories of Personality Disorder, eds M. F. Lenzenweger and J. F. Clarkin (New York, NY: Guilford Press), 114–156.
Kim, A. W., Nyengerai, T., and Mendenhall, E. (2020). Evaluating the mental health impacts of the COVID-19 pandemic: perceived risk of COVID-19 infection and childhood trauma predict adult depressive symptoms in urban South Africa. Psychol. Med. [Online ahead of print] 1–13. doi: 10.1017/S0033291720003414
Kleinke, K. (2017). Multiple imputation under violated distributional assumptions: a systematic evaluation of the assumed robustness of predictive mean matching. J. Educ. Behav. Stat. 42, 371–404. doi: 10.3102/1076998616687084
Kocjan, G. Z., Kavčič, T., and Avsec, A. (2021). Resilience matters: explaining the association between personality and psychological functioning during the COVID-19 pandemic. Int. J. Clin. Health Psychol. 21:100198. doi: 10.1016/j.ijchp.2020.08.002
Kroenke, K., Wu, J., Yu, Z., Bair, M. J., Kean, J., Stump, T., et al. (2016). Patient health questionnaire anxiety and depression scale: initial validation in three clinical trials. Psychosom Med. 78, 716–727. doi: 10.1097/PSY.0000000000000322
Kujawa, A., Green, H., Compas, B. E., Dickey, L., and Pegg, S. (2020). Exposure to COVID-19 pandemic stress: associations with depression and anxiety in emerging adults in the United States. Depression Anxiety 37, 1280–1288.
Lassri, D., and Desatnik, A. (2020). Losing and regaining reflective functioning in the times of COVID-19. Clinical risks and opportunities from a mentalizing approach. Psychol. Trauma: Theory Res. Pract. Pol. 12, 38–40. doi: 10.1037/tra0000760
Lawson, M., Piel, M. H., and Simon, M. (2020). Child maltreatment during the COVID-19 pandemic: consequences of parental job loss on psychological and physical abuse towards children. Child Abuse Negl. 110:104709. doi: 10.1016/j.chiabu.2020.104709
Leibovitz, T., Shamblaw, A. L., Rumas, R., and Best, M. W. (2021). COVID-19 conspiracy beliefs: relations with anxiety, quality of life, and schemas. Person. Individ. Differ. 175:110704.
Li, L. Q., Huang, T., Wang, Y. Q., Wang, Z. P., Liang, Y., Huang, T. B., et al. (2020). COVID-19 Patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J. Med. Virol. 92, 577–583. doi: 10.1002/jmv.25757
Little, R. J. A. (1988). Missing-Data adjustments in large surveys. J. Bus. Econ. Stat. 6, 287–301. doi: 10.2307/1391878
Löwe, B., Decker, O., Müller, S., Brähler, E., Schellberg, D., Herzog, W., et al. (2008). Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med. Care 46, 266–274.
Luyten, P., Campbell, C., Allison, E., and Fonagy, P. (2020). The mentalizing approach to psychopathology: state of the art and future directions. Annu. Rev. Clin. Psychol. 16, 297–325. doi: 10.1146/annurev-clinpsy-071919-015355
Luyten, P., Nijssens, L., Fonagy, P., and Mayes, L. C. (2017). Parental reflective functioning: theory, research, and clinical applications. Psychoanalytic Study Child 70, 174–199. doi: 10.1080/00797308.2016.1277901
Mandelli, L., Petrelli, C., and Serretti, A. (2015). The role of specific early trauma in adult depression: a meta-analysis of published literature. Childhood trauma and adult depression. Eur. Psychiatry 30, 665–680. doi: 10.1016/j.eurpsy.2015.04.007
Mazza, C., Ricci, E., Biondi, S., Colasanti, M., Ferracuti, S., Napoli, C., et al. (2020). A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health 17:3165. doi: 10.3390/ijerph17093165
McLaughlin, K. A., Colich, N. L., Rodman, A. M., and Weissman, D. G. (2020). Mechanisms linking childhood trauma exposure and psychopathology: a transdiagnostic model of risk and resilience. BMC Med. 18:96. doi: 10.1186/s12916-020-01561-6
Milner, J. S. (1994). Assessing physical child abuse risk: the child abuse potential inventory. Clin. Psychol. Rev. 14, 547–583. doi: 10.1016/0272-7358(94)90017-5
Nyberg, E., Hartman, P., Stieglitz, R., and Riecher-Rössler, A. (2008). Screening partnergewalt: ein deutschsprachiges screeninginstrument für häusliche gewalt gegen frauen. Fortschritte Neurol.-Psychiatrie (FDN) 76, 28–36.
Olajide, K., Munjiza, J., Moran, P., O’Connell, L., Newton-Howes, G., Bassett, P., et al. (2018). Development and psychometric properties of the standardized assessment of severity of personality disorder (SASPD). J. Person. Disord. 32, 44–56. doi: 10.1521/pedi_2017_31_285
Oleksy, T., Wnuk, A., Maison, D., and Łyś, A. (2021). Content matters. Different predictors and social consequences of general and government-related conspiracy theories on COVID-19. Person. Individ. Differ. 168:110289.
Petzold, M. B., Bendau, A., Plag, J., Pyrkosch, L., Mascarell Maricic, L., Betzler, F., et al. (2020). Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain Behav. 10:e01745. doi: 10.1002/brb3.1745
Pierce, M., Hope, H., Ford, T., Hatch, S., Hotopf, M., John, A., et al. (2020). Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry 7, 883–892. doi: 10.1016/S2215-0366(20)30308-4
Popp, L., Fuths, S., Seehagen, S., Bolten, M., Gross-Hemmi, M., Wolke, D., et al. (2016). Inter-rater reliability and acceptance of the structured diagnostic interview for regulatory problems in infancy. Child Adolescent Psychiatry Ment. Health 10, 1–10. doi: 10.1186/s13034-016-0107-6
Prichard, E. C., and Christman, S. D. (2020). Authoritarianism, conspiracy beliefs, gender and COVID-19: links between individual differences and concern about COVID-19, mask wearing behaviors, and the tendency to blame China for the virus. Front. Psychol. 11:597671. doi: 10.3389/fpsyg.2020.597671
Ramsauer, B., Lotzin, A., Mühlhan, C., Romer, G., Nolte, T., Fonagy, P., et al. (2014). A randomized controlled trial comparing circle of security intervention and treatment as usual as interventions to increase attachment security in infants of mentally ill mothers: study protocol. BMC Psychiatry 14:24. doi: 10.1186/1471-244X-14-24
Rek, K., Thielmann, I., Henkel, M., Crawford, M., Piccirilli, L., Graff, A., et al. (2020). A psychometric evaluation of the standardized assessment of severity of personality disorder (SASPD) in nonclinical and clinical German samples. Psychol. Assessment 32:984. doi: 10.1037/pas0000926
Rodríguez-Rey, R., Garrido-Hernansaiz, H., and Collado, S. (2020). Psychological Impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Front. Psychol. 11:1540. doi: 10.3389/fpsyg.2020.01540
Rossi, R., Socci, V., Talevi, D., Mensi, S., Niolu, C., Pacitti, F., et al. (2020). COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front. Psychiatry 11:790. doi: 10.3389/fpsyt.2020.00790
Salari, N., Hosseinian-Far, A., Jalali, R., Vaisi-Raygani, A., Rasoulpoor, S., Mohammadi, M., et al. (2020). Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob. Health 16, 1–11.
Scher, C. D., Stein, M. B., Asmundson, G. J., McCreary, D. R., and Forde, D. R. (2001). The childhood trauma questionnaire in a community sample: psychometric properties and normative data. J. Traumatic Stress 14, 843–857. doi: 10.1023/A:1013058625719
Shorer, M., and Leibovich, L. (2020). Young Children’s emotional stress reactions during the COVID-19 outbreak and their associations with parental emotion regulation and parental playfulness. Early Child Dev. Care 1–11. doi: 10.1080/03004430.2020.1806830
Spitzer, R. L., Kroenke, K., Williams, J. B., and Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Internal Med. 166, 1092–1097. doi: 10.1001/archinte.166.10.1092
Šrol, J., Mikušková, E. B., and Cavojova, V. (2020). When we are worried, what are we thinking? Anxiety, lack of control, and conspiracy beliefs amidst the COVID-19 pandemic. Appl. Cogn. Psychol. 35, 720–729.
Tedeschi, R. G., and Calhoun, L. G. (1996). The posttraumatic growth inventory: measuring the positive legacy of trauma. J. Traumatic Stress 9, 455–471. doi: 10.1007/BF02103658
Topp, C. W., Østergaard, S. D., Søndergaard, S., and Bech, P. (2015). The WHO-5 well-being index: a systematic review of the literature. Psychother. Psychosomatics 84, 167–176. doi: 10.1159/000376585
Valdez, D., Ten Thij, M., Bathina, K., Rutter, L. A., and Bollen, J. (2020). Social media insights into US mental health during the COVID-19 pandemic: longitudinal analysis of twitter data. J. Med. Internet Res. 22:e21418.
Vazquez, C., Valiente, C., García, F. E., Contreras, A., Peinado, V., Trucharte, A., et al. (2021). Post-traumatic growth and stress-related responses during the COVID-19 pandemic in a national representative sample: the role of positive core beliefs about the world and others. J. Happiness Stud. [Online ahead of print] 1–21. doi: 10.1007/s10902-020-00352-3
Ventura Wurman, T., Lee, T., Bateman, A., Fonagy, P., and Nolte, T. (2020). Clinical management of common presentations of patients diagnosed with BPD during the COVID-19 pandemic. The contribution of the MBT framework. Counsell. Psychol. Q. 292, 1–27. doi: 10.1080/09515070.2020.1814694
Wingenfeld, K., Spitzer, C., Mensebach, C., Grabe, H. J., Hill, A., Gast, U., et al. (2010). Die deutsche Version des Childhood Trauma Questionnaire (CTQ): erste befunde zu den psychometrischen Kennwerten. PPmP-Psychotherapie⋅Psychosomatik⋅ Medizinische Psychol. 60, 442–450. doi: 10.1055/s-0030-1247564
World Health Organization [WHO] (2020). Managing the COVID-19 Infodemic: Promoting Healthy Behaviours and Mitigating the Harm from Misinformation and Disinformation. Geneva: World Health Organiztion.
Wu, T., Jia, X., Shi, H., Niu, J., Yin, X., Xie, J., et al. (2020). Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J. Affect. Disord. 281, 91–98. doi: 10.1016/j.jad.2020.11.117
Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M., Gill, H., Phan, L., et al. (2020). Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 277, 55–64. doi: 10.1016/j.jad.2020.08.001
Zeegers, M. A., Colonnesi, C., Stams, G. J. J., and Meins, E. (2017). Mind matters: a meta-analysis on parental mentalization and sensitivity as predictors of infant–parent attachment. Psychol. Bull. 143:1245. doi: 10.1037/bul0000114
Zero to Three (2005). Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood: Revised Edition (DC: 0-3R). Washington, DC: Zero to Three.
Keywords: pandemic (COVID-19), crisis, trauma, reflective functioning, mentalizing, personality functioning, emotion regulation, family
Citation: Volkert J, Taubner S, Berning A, Kling L, Wießner H, Georg AK and Holl J (2021) Transdiagnostic Mechanisms of Mental Health During the COVID-19 Pandemic on Adults and Families in Germany: Study Protocol of a Cross-Sectional and 1-Year Longitudinal Study. Front. Psychol. 12:720104. doi: 10.3389/fpsyg.2021.720104
Received: 03 June 2021; Accepted: 22 November 2021;
Published: 22 December 2021.
Edited by:
Anders Hakansson, Lund University, SwedenReviewed by:
Carmen Moret-Tatay, Catholic University of Valencia San Vicente Mártir, SpainAlexander Michael Ponizovsky, Ministry of Health (Israel), Israel
Copyright © 2021 Volkert, Taubner, Berning, Kling, Wießner, Georg and Holl. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jana Volkert, jana.volkert@medicalschool-berlin.de
†These authors have contributed equally to this work and share last authorship
 Jana Volkert
Jana Volkert Svenja Taubner
Svenja Taubner Anna Berning2
Anna Berning2 Anna K. Georg
Anna K. Georg Julia Holl
Julia Holl