Screening for early warning of psychological crisis and intervention in children aged 8–18 years with cancer: a historical controlled trial
- 1Department of Outpatient, Children’s Hospital of Chongqing Medical University, Chongqing, China
- 2Chongqing Key Laboratory of Pediatrics, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, China International Science and Technology Cooperation Base of Child Development and Critical Disorders, Chongqing, China
- 3Department of Pediatrics, Children's Hospital of Chongqing Medical University, Chongqing, China
- 4Department of Oncology, Children's Hospital of Chongqing Medical University, Chongqing, China
Background: Childhood cancer is becoming an emerging healthcare issue in mainland China. Extensive evidence in the literature has demonstrated that cancer and its treatment experience can cause psychological distress that can lead to developmental problems in children with cancer. This study aims to screen for early warning of psychological crisis in children aged 8–18 years with cancer, establish a model of early warning intervention for children with cancer, and explore its application effects.
Methods: We recruited 345 children with cancer and aged 8–18 years as the study participants, of whom 173 children were selected as historical controls during the period between December 2019 and March 2020 and 172 children were selected as the intervention group during the period between July 2020 and October 2020. The routine nursing model was adopted for the control group, and the early warning and intervention model was applied for the intervention group. The early warning and intervention model consisted of four stages: (1) establishing a management team to assess the risk of psychological crisis, (2) developing a three-level early warning response mechanism, (3) developing specific response plans, and (4) creating an evaluation summary and optimization mode. The DASS-21 was used to evaluate the psychological status of children with cancer before and 3 months after the intervention.
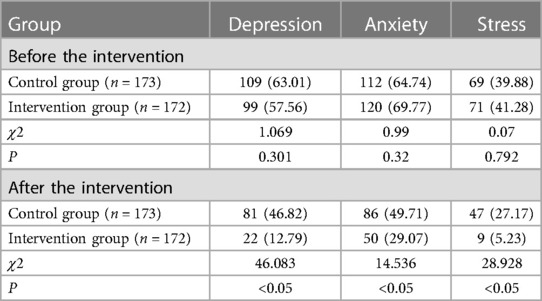
Results: The average age of the control group was 11.43 ± 2.39 years, with 58.96% boys and 61.27% diagnosed with leukemia. The average age of the intervention group was 11.62 ± 2.31 years, with 58.72% boys and 61.63% diagnosed with leukemia. There was a significant reduction in depressive symptoms (4.91 ± 3.98, t = 12.144, P < 0.05), anxiety symptoms (5.79 ± 4.34, t = 8.098, P < 0.05), and stress symptoms (6.98 ± 4.67, t = 11.22, P < 0.05) in the intervention group. The incidence rates of depression, anxiety, and stress were significantly lower in the intervention group (12.79%, 29.07%, and 5.23%, respectively) than in the control group (46.82%, 49.71%, and 27.17%, respectively) (all P's < 0.05).
Conclusions: Our study suggests that the early detection and timely management of psychological symptoms through a nursing intervention model can effectively reduce depressive, anxiety, and stress symptoms in Chinese children with cancer. Future work should include conducting qualitative interviews to understand the psychological experiences of children with cancer throughout their entire life cycle.
Introduction
Cancer is a major disease that seriously threatens the physical and mental health of adolescents. Its incidence and survival rates are increasing year by year (1). In 2017, the number of new cancer cases among children and adolescents in the world was approximately 416,500 (2). Between 2018 and 2020, the number of new cancer cases among children and adolescents in China was approximately 121,145, with an average incidence rate of 126.48 million (3). With the development of, and advances in, medical technology, the 5-year survival rate for children with cancer has been increasing gradually, which is as high as 85% (4). This means that there is a growing number of children and their families facing a range of problems such as late complications (5), secondary tumors, poor behavior (6), and even death.
Adolescence is an important period for physical growth and mental development. When adolescents are diagnosed with serious conditions during this critical period, they may be more sensitive to physiological and emotional changes than adults, making them a high-risk group for psychological and mental health crises. Some studies have shown that the diagnosis and treatment of cancer make adolescents bear more psychological pressure than what is required, which leads to different psychological reactions during different stages of cancer (7–10). Excessive and persistent negative pressure increases the degree of negative emotions in children, and children tend to have negative cognition. The result is a weakening of their self-confidence to overcome the disease and lower treatment compliance, both of which reduce the effect of treatment and disease rehabilitation.
However, research has shown that children with cancer show both negative and positive psychological responses in their fight against cancer. According to the relevant literature, children possess a definite cultural knowledge base after the age of 8 years to have an initial understanding of society and their personal thoughts (11). As their age of education advances and their level of education increases, the autonomy, cognitive level, and judgment ability of younger minors improve significantly. An 8-year-old child can clearly discern which training class they want to attend and which teacher is more strict than others. They also show the ability to self-report the occurrence of events (12). Moreover, children are at a specific stage of transition to adulthood during this time and are prone to stress while fulfilling their mandatory bodily needs of growing up.
The psychological problems of children with cancer and the relevant intervention strategies to be adopted have attracted the attention of researchers. Many research groups have evaluated different types of psychological interventions for adolescents with cancer. A study of psychological crisis intervention models in foreign countries has been recorded as early as 1964 when American psychologist Gerald Caplan first proposed the theory of psychological crisis. He divided the formation and evolution process of psychological crisis into four stages. Later researchers proposed the development of ecological models, situational ecological models, psychological first aid, and seven-stage psychological crisis intervention models. Chinese researchers proposed a real-time reservation model, an online-to-offline model, and a cognitive regulatory model. These models were mainly applied to healthy children and therefore lacked research on early identification, warning, and intervention of psychological problems in adolescents with cancer. Therefore, this study will construct an early warning and intervention model for psychological crisis in children with cancer and explore its application effect.
Materials and methods
Study participants
Adolescents with cancer were recruited from the Children's Hospital of Chongqing Medical University. The inclusion criteria were as follows: (1) children aged 8–18 years (this age group has self-reporting capabilities); (2) children diagnosed with cancer by the standard guidelines for the diagnosis and treatment of childhood malignancies (13); and (3) children who provided informed consent. The exclusion criteria were as follows: (1) children suffering from severe organic or cognitive impairment and (2) children who were unable to understand the questionnaire. Exit criteria included the following: treatment was terminated during the study, and children or guardians were asked to withdraw midway during the study. The Institutional Review Board of Children's Hospital of Chongqing Medical University approved this study, File No.: (2018) Lun Li (Research) No. (1).
Sample size calculation
Refer to the formula of sample size for controlled trials, , where α = 0.05 and β = 0.1. According to the bilateral test table, Z0.05 = 1.96 and Z0.1 = 1.282; after literature review (14), σ = 4.37 and δ = 1.64, and the sample size for each group was calculated as 150 cases. Considering a 20% loss rate in the samples, the final sample size was determined as 180 cases. During the study, eight cases in the control group terminated intervention due to changes in the condition, six cases in the intervention group terminated intervention, and one case withdrew midway. Finally, 173 patients recruited from December 2019 to March 2020 were selected as the control group, and 172 patients recruited from July 2020 to October 2020 were selected as the intervention group.
Measurement tools
The Depression Anxiety Stress Scale (DASS-21) is a self-assessment scale and was translated into Chinese by Xu et al. (15); it contains three dimensions: depression, anxiety, and stress. Each dimension has seven entries, and each item is scored from 0 (never) to 3 (always). The DASS-21 has good test reliability in the adolescent group and can be used as both a norm-referenced test and a standard reference test when evaluating the negative emotions of adolescents (16). The author's previous research showed that the total Cronbach's alpha of the DASS-21 is 0.916, the subscale's alpha coefficient is 0.793–0.819, the Kaiser–Meyer–Olkin (KMO) value is 0.919 (>0.8), the Bartlett spherical test statistic is χ2 = 1,938.6993 (P < 0.001), and the scale has good reliability and validity. Based on the total score, there were five levels: (1) normal, depression (≤9), anxiety (≤7), and stress (≤14); (2) mildly abnormal, depression (10–13), anxiety (8–9), and stress (15–18); (3) moderately abnormal, depression (14–20), anxiety (10–14), and stress (19–25); (4) severe abnormal, depression (21–27), anxiety (15–19), and stress (26–33); and (5) extremely severe abnormal, depression (≥28), anxiety (≥20), and stress (≥34).
Interventions
Patients in the control group received routine nursing care. Nurses received patients warmly when they were admitted, introduced them to the environment of the hospital, implemented the doctor's advice, communicated with them before the operation, listened to them, and took care of them.
The intervention group was based on routine nursing care and also implemented the early warning and intervention model of psychological crisis (hereafter called the early model). The early model includes four steps.
Establishing a management team
Two doctors formulated treatment plans and discussed patients' conditions with their family members. Of four nurses, one was responsible for coordination and quality control, and the others were responsible for implementing nursing interventions. Two psychological counselors developed the intervention plans, trained in psychological knowledge, and provided one-on-one counseling if necessary. One community worker mobilized the support resources of the community or school, and another organized volunteer activities. In addition, the team should receive training in terms of the characteristics of children's psychological and behavioral development and crisis intervention, skills of psychological counseling and program implementation, clinical application of cognitive behavioral therapy, training of comfortable nursing ability of pediatric nurse, and procedures and considerations of the intervention.
Developing a response plan with the three-level early warning
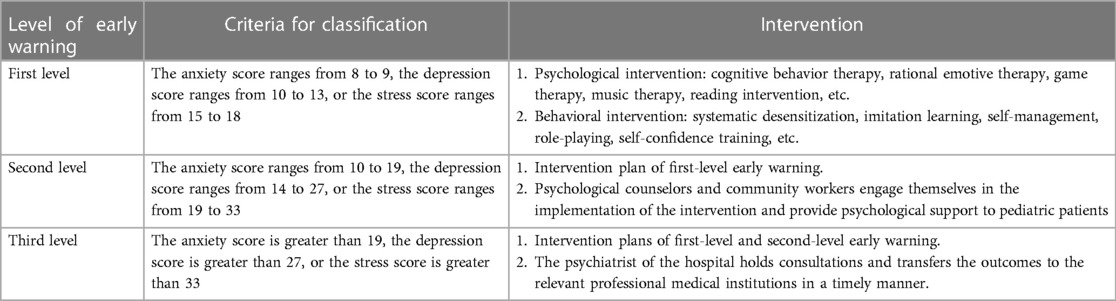
According to the scoring standard of the Depression Anxiety Stress Scale (DASS-21), the early warning of a psychological crisis in adolescents with cancer was divided into three levels (Table 1).
Implementing intervention
Establish archives (the first week): general information, family education, medical insurance, and psychological status.
Physiological support (every week): doctors, nurses, and patients formulated plans and promoted orderly activities, providing patients with timely care, reducing physical injury in operation and side effects of drugs, and helping patients establish a regular and healthy lifestyle, for example, providing children with healthy food and ensuring that they get enough sleep.
Psychological support (every week): providing cognitive therapy through semistructured interviews, understanding patients' adverse cognition, and correcting through semantic analysis, imitation, or decentralization.
Behavioral therapy (every week): analyzing the frequency and severity of adverse behaviors of patients, and correcting through systematic desensitization, imitation learning, self-management, role-playing, and self-confidence training.
Social support (every week): holding a series of lectures on “caring for children with cancer”; holding theme activities on a weekly basis, such as music activities, painting activities, sharing stories, film appreciation, and knowledge contests; and establishing a network group, for example, online communication, release of disease-related knowledge, psychological counseling, and regular children education. For example, Xiao Ming (assumed name) told us that he would eventually die from cancer. Then, we corrected his misconception, gave him confidence in overcoming the disease, and asked the recovered children to share their stories.
(1) Evaluation and summary: after 3 months of early warning intervention, we assessed the current psychological status of the children with cancer by the DASS-21.
Statistical analysis
SPSS Statistics 22.0 was used for statistical analysis. The measurement data are described as the mean [±standard deviation (SD)]. The count data are described as the frequency and percentage (%). The chi-square test was applied to compare the qualitative data. The Bonferroni method was used to correct the P value in pairwise comparison. t-test, paired t-test, and analysis of variance method were used for quantitative data conforming to normal distribution. All tests were two-sided, and statistical significance was defined as P < 0.05.
Results
Baseline characteristics
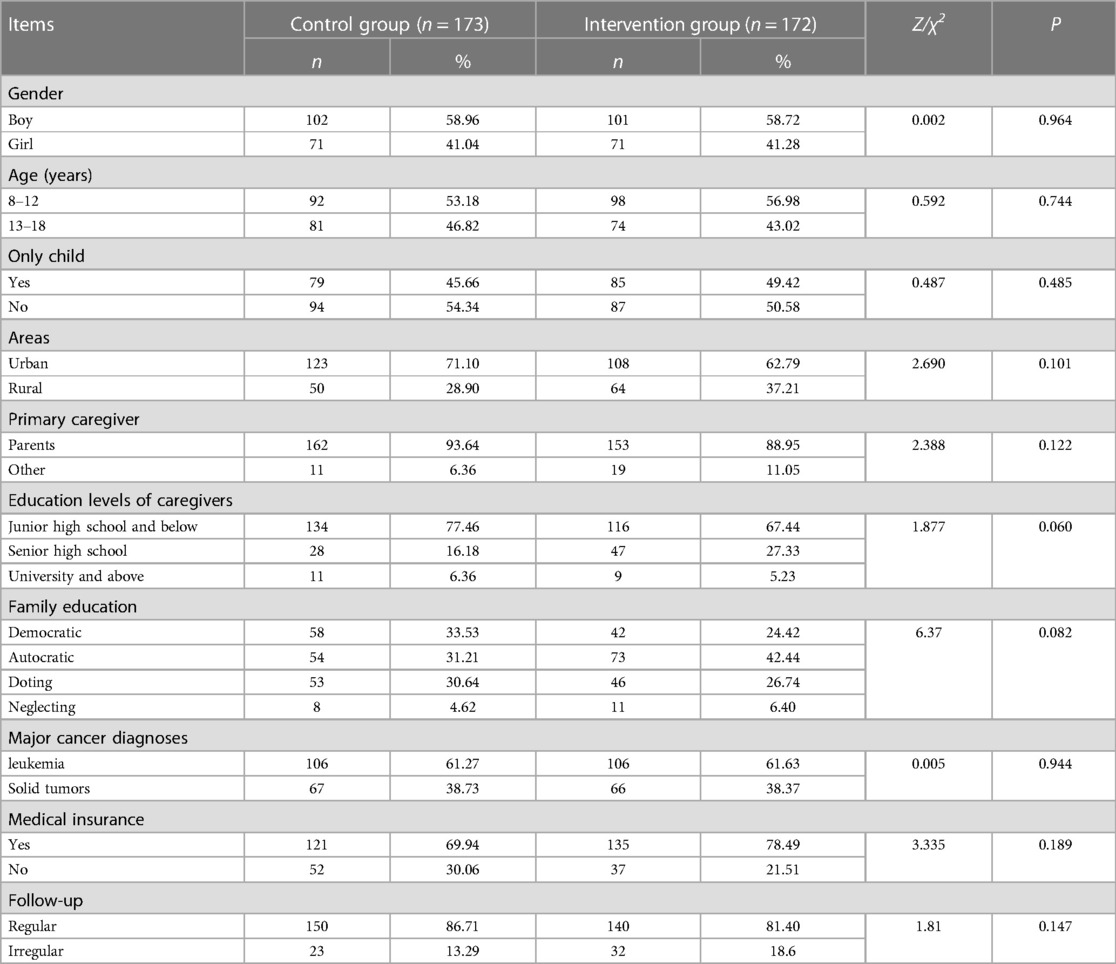
There were no significant differences in the baseline characteristics of the intervention and control groups. The study participants were young in age (55.07% were 8–12 years old) and comprised a higher percentage of males (58.84%), mainly lived in cities (66.96%), mostly taken care of by their parents (90%), and mostly diagnosed with leukemia (61.63%) and had medical insurance (74.2%). The caregiver's cultural level was relatively low (72.46% received secondary school education) (Table 2).
The levels of anxiety, depression, and stress
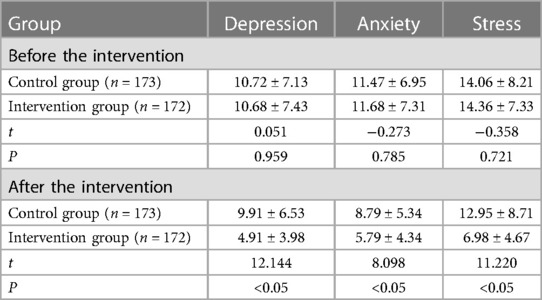
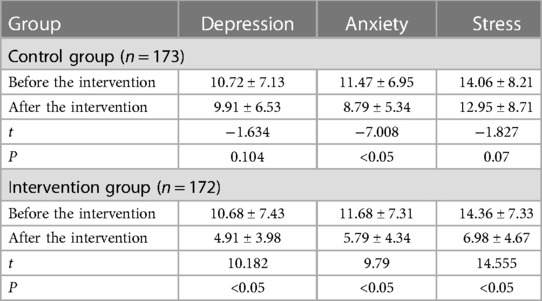
There was no significant difference in levels of depression, anxiety, and stress between the control group and the intervention group before the intervention. After the intervention, the levels of depression, anxiety, and stress in the intervention group (4.91 ± 3.98, 5.79 ± 4.34, 6.98 ± 4.67) were lower than those in the control group (9.91 ± 6.53, 8.79 ± 5.34, 12.95 ± 8.71), and the difference between the two groups was statistically significant (P < 0.05) (Table 3). In addition, the levels of depression, anxiety, and stress in the intervention group (4.91 ± 3.98, 5.79 ± 4.34, 6.98 ± 4.67) were greatly lower than those before the intervention (10.72 ± 7.13, 11.47 ± 6.95, 14.06 ± 8.21). Only anxiety levels (8.79 ± 5.34) in the control group were significantly lower than those before the intervention (11.68 ± 7.31) (Table 4).
The detection rate of depression, anxiety, and stress
As shown in Table 5, there were no significant differences in the detection rate of depression, anxiety, and stress between the control group and the intervention group before the intervention. After the intervention, the detection rates of depression, anxiety, and stress in the intervention group (12.79%, 29.07%, and 5.23%) were lower than those in the control group (46.82%, 49.71%, and 27.17%), and the difference between the two groups was statistically significant (P < 0.05).
Discussion
Children aged 8–18 years with cancer have obvious psychological problems
Children aged 8–18 years with cancer have obvious psychological problems. In this study, it was found that the detection rates of depression, anxiety, and stress in the intervention group before the intervention were 57.56%, 69.77%, and 41.28%, respectively, which were higher than those of middle school students (29.0%, 51.0%, and 23.9%, respectively) (17). Our previous investigation involving 217 adolescents with cancer found that 91.7% of them had various degrees of psychological problems (18). The immaturity of children's own physical and psychological development is the subjective factor of their psychological problems. On the one hand, children aged 8–18 years are about to have or already have entered adolescence. Individual physiology develops rapidly before reaching maturity, and therefore, there are significant changes in their physiological, psychological, and social development. On the other hand, children with cancer also suffer from the physiological or psychological effects of cancer symptoms, treatment, and long-term complications (19–22). In addition, the negative influences of family, school, and society are important objective stimuli for psychological problems. The interaction between physiological, psychological, and social factors serves to heighten some contradictions that could be solved in the development process of physiology and psychology. If the characteristics of diversity, overlapping, and timeliness are present, the psychological problems of adolescents usually cannot be solved by an intervention.
The early warning and intervention model effectively improves the psychological state of children with cancer
The research results showed that the score and the detection rate of depression, anxiety, and stress in the intervention group were all markedly lower than those in the control group after the intervention. This means the early model effectively improves the psychological state of children with cancer. Furthermore, in the intervention group, the scores for depression, anxiety, and stress were greatly different from those after the intervention. In contrast, the scores for depression and stress in the control group were not observably different from those after the intervention; only the difference in the score of anxiety was statistically significant. All these indicated that traditional nursing intervention could appropriately alleviate the anxiety of children with cancer, but had no obvious effect on depression and stress. The early model could provide timely preventive interventions by comprehensively assessing the psychological and social conditions of children, thereby effectively improving their psychological problems, consistent with reports by researchers such as Chen Jin (23–25). Research has confirmed that early warning intervention can effectively improve patients' psychological state (26) and enhance intervention effectiveness (27).
This study constructed an early warning and intervention model for psychological crisis in children with cancer. First, qualification setting and responsibility clarifying and a multidisciplinary team including doctors, nurses, psychological counselors, community workers, and volunteers were established. Teamwork can effectively improve the members' ability to solve problems. Second, we developed the response of early warning and included the appropriate psychological scale to scientifically formulate grading standards. We arranged the response personnel, formulated intervention programs, and implemented preventive intervention rigorously and in a systematic way. Preventive intervention was carried out to correct patients’ unreasonable beliefs or cognition; to help them establish peer, social, and information support system; and to prevent the occurrence of psychological crisis. In addition, the specific implementation details of the program were formulated. The intervention program was set up after considering the physical, psychological, social, and spiritual aspects and combined with various interventions. Online and offline interventions were carried out simultaneously, which compensated for the deficiencies of routine psychological intervention. After the intervention, evaluation, feedback analysis, and file improvement were conducted. On this account, personalized and precise warning interventions could be achieved, effectively preventing and reducing the occurrence of psychological crisis in children with cancer.
Conclusions
Children with cancer have obvious mental health problems. The early warning and intervention model of psychological crisis contained three aspects, which were regular assessment of psychological crisis, screening for psychological crisis, and intervention of psychological crisis, which was conducive to early detection and intervention of psychological problems in children with cancer, thereby preventing the occurrence or reducing the severity of the psychological problems.
Clinical implications
Clinicians and nurses should pay more attention to early diagnosis and intervention of children with cancer to improve the disease outcome. Future work should include conducting qualitative interviews to understand the psychological experiences of children with cancer throughout their entire life cycle.
Study limitations
This study did not classify the patients' disease diagnosis. It is necessary to collect information on the diagnosis of children with cancer to research whether there are differences in different cancer types. In addition, this is a historical controlled trial and not a randomized clinical trial, and therefore, the presence of some confounding variables cannot be ruled out.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions. The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions. Requests to access these datasets should be directed to molin999@126.com.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of the Children's Hospital of Chongqing Medical University. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
All authors conceptualized and designed the study. LY, XH, and YL conducted the study. LY and YL performed data analysis. LY and LM either wrote or contributed to the writing of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The study was supported by a research grant from the Chongqing Municipal Health Bureau (grant no. cstc2018jscx-msybX0110).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. National Cancer Center. Annual report of cancer registration in China in 2017. Beijing: People’s Medical Publishing House (2018). 50–60.
2. GBD 2017 Childhood Cancer Collaborators. The global burden of childhood and adolescent cancer in 2017: an analysis of the global burden of disease study 2017. Lancet Oncol. (2019) 20(9):1211–25. doi: 10.1016/S1470-2045(19)30339-0
3. Ni X, Li Z, Li X, Zhang X, Bai G, Liu Y, et al. Socioeconomic inequalities in cancer incidence and access to health services among children and adolescents in China: a cross-sectional study. Lancet. (2022) 400(10357):1020–32. doi: 10.1016/S0140-6736(22)01541-0
4. Rivera LR, Shalkow KJ, Velasco HL, Cárdenas CR, Zapata TM, Olaya VA, et al. Descriptive epidemiology in Mexican children with cancer under an open national public health insurance program. BMC Cancer. (2014) 14:790. doi: 10.1186/1471-2407-14-790
5. Firkins J, Hansen L, Driessnack M, Dieckmann N. Quality of life in “chronic” cancer survivors: a meta-analysis. J Cancer Surviv. (2020) 14(4):504–17. doi: 10.1007/s11764-020-00869-9
6. Tao S, Wu S, Zheng J, Liu K. Healthy-related quality of life among long-term survivors of childhood cancer. J Nurs Sci. (2021) 36(2):77–80. doi: 10.3870/j.issn.1001-4152.2021.02.077
7. Leuteritz K, Friedrich M, Nowe E, Sender A, Stöbel-Richter Y, Geue K. Life situation and psychosocial care of adolescent and young adult (AYA) cancer patients study protocol of a 12 month prospective longitudinal study. BMC Cancer. (2017) 1(17):82–9. doi: 10.1186/s12885-017-3077-z
8. Zhang P, Mo L, Li X, Wang Q, Shi L, Wang Z. Effect of different psychological interventions on negative emotion in children with malignant tumor: a network meta-analysis. J China Med Univ. (2017) 42(9):1208–13. doi: 10.13406/j.cnki.cyxb.001362
9. Sint Nicolaas SM, Hoogerbrugge PM, van den Bergh EM, Custers JA, Gameiro S, Gemke RJ, et al. Predicting trajectories of behavioral adjustment in children diagnosed with acute lymphoblastic leukemia. Support Care Cancer. (2016) 24(11):4503–13. doi: 10.1007/s00520-016-3289-9
10. James C, George R, Jean K, Phillip M. Mindfulness, spirituality and health-related symptoms. J Psychosom Res. (2008) 64(4):393–403. doi: 10.1016/j.jpsychores.2007.06.015
11. Chen X. The general principles of the civil law to amend the minimum age limit of civil capacity of minors to explore the reasonableness. Legality Vision. (2019) 7:235.
12. Mack JW, McFatrich M, Withycombe JS, Maurer SH, Jacobs SS, Lin L, et al. Agreement between child self-report and caregiver-proxy report for symptoms and functioning of children undergoing cancer treatment. JAMA Pediatric. (2020) 174:e202861. doi: 10.1001/jamapediatrics.2020.2861
13. Children’s National Medical Center. Treatment specifications for 12 diseases related to hematological diseases and malignant tumors in children (2021 version). Available at: http://www.nhc.gov.cn/yzygj/s7659/202105/3c18fec8a37d452b82fe93e2bcf3ec1e.shtml (Accessed May 13, 2021).
14. Zhang P, Mo L, Li X, Huang X. The effect of cognitive behavioral therapy on the resilience and negative emotions of children with cancer undergoing chemotherapy. J Nurs. (2018) 33(13):60–4. doi: 10.3870/j.issn.1001-4152.2018.13.060
15. Gong X, Xie X, Xu R, Luo Y. Psychometric properties of the Chinese versions of DASS-21 in Chinese college students. Chin J Clin Psychol. (2010) 18(4):443–6. doi: 10.16128/j.cnki.1005-3611.2010.04.020
16. Qiu T, Zhang L, Yao C, Luo J. Multiple generalizability analysis of the simplified depression anxiety stress scale. Chin J Behav Med Brain Sci. (2023) 32(1):75–9. doi: 10.3760/cma.j.cn371468-20220517-00271
17. Sha L, Yanrui J, Qingmin L, Min M, Yunting Z, Wenjie S, et al. Association between negative emotions and insomnia symptoms in middle school students in Shanghai. Chin J Child Health Care. (2019) 27(09):936–40.
18. Lu Y, Lin M, Xia L, Ping Z, Yang L. Research progress of psychological crisis early warning intervention in adolescent cancer children. Today Nurse. (2020) 27(04):10–3. doi: 10.19791/j.cnki.1006-6411.2020.10.004
19. Xingli L, Jing L, Chengyu Z. A qualitative study on psychological status of adolescent cancer patients undergoing chemotherapy. Med Inf. (2010) 23(16):2615–7.
20. Dyson GJ, Thompson K, Palmer S, Thomas DM, Schofield P. The relationship between unmet needs and distress amongst young people with cancer. Support Care Cancer. (2012) 20:1. doi: 10.1007/s00520-010-1059-7
21. Shin KJ, Lee YJ, Yang YR, Park S, Suh PG, Follo MY, et al. Molecular mechanisms underlying psychological stress and cancer. Curr Pharm Des. (2016) 22(16):2389–402. doi: 10.2174/1381612822666160226144025
22. Davis LZ, Slavich GM, Thaker PH, Goodheart MJ, Bender DP, Dahmoush L, et al. Eudaimonic well-being and tumor norepinephrine in patients with epithelial ovarian cancer. Cancer. (2015) 121(19):3543–50. doi: 10.1002/cncr.29516
23. Jin C. The therapeutic effect of mental nursing intervention on alleviating psychological anxiety in adolescent cancer patients. Guangdong Med. (2018) 39(5):797–9. doi: 10.13820/j.cnki.gdyx.2018.05.021
24. Lopes-Júnior LC, Bomfim EO, Nascimento LC, Nunes MD, Pereira-da-Silva G, Lima RA. Non-pharmacological interventions to manage fatigue and psychological stress in children and adolescents with cancer: an integrative review. Eur J Cancer Care. (2016) 25(6):921–35. doi: 10.1111/ecc.12381
25. Lili X, Jingjing W, Mei W, Mengxia X, Chong W. The impact of the cooperative nursing mode of medical care and family members on the psychological status and complications of children with brain tumor. Chin J Cancer Clin Rehabil. (2022) 29(03):355–8. doi: 10.13455/j.cnki.cjcor.2022.03.25
26. Yuying L, Xiangni W, Xiaomei Z. Classic cases point out the impact of early warning nursing intervention on the psychological status of postpartum women and the incidence of postpartum complications. Guizhou Med. (2022) 46(12):2000–1.
Keywords: children with cancer, psychological crisis, early warning, intervention, 8–18 years
Citation: Yu L, Mo L, Liu Y and Huang X (2023) Screening for early warning of psychological crisis and intervention in children aged 8–18 years with cancer: a historical controlled trial. Front. Pediatr. 11:1156185. doi: 10.3389/fped.2023.1156185
Received: 1 February 2023; Accepted: 5 June 2023;
Published: 22 June 2023.
Edited by:
Chi-kong Li, Chinese University of Hong Kong, ChinaReviewed by:
Yin Ting Cheung, The Chinese University of Hong Kong, Hong Kong SAR, ChinaYasuhiro Okamoto, Kagoshima University, Japan
© 2023 Yu, Mo, Liu and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lin Mo molin999126.com
 Lu Yu
Lu Yu Lin Mo
Lin Mo Yixuan Liu2,3
Yixuan Liu2,3