Self-Reported Health in Adolescents With Exercise-Induced Laryngeal Obstruction; A Cross-Sectional Study
- 1The Faculty of Health and Social Sciences, Western Norway University of Applied Sciences, Bergen, Norway
- 2Department of Pediatrics, Haukeland University Hospital, Bergen, Norway
- 3Department of Global Public Health and Primary Care, University of Bergen, Bergen, Norway
- 4Department of Clinical Science, Faculty of Medicine, University of Bergen, Bergen, Norway
- 5Department of Otolaryngology/Head and Neck Surgery, Haukeland University Hospital, Bergen, Norway
- 6Norwegian School of Sport Sciences, Oslo, Norway
- 7Department of Psychosocial Science, Faculty of Psychology, University of Bergen, Bergen, Norway
Background: Exercise-induced laryngeal obstruction (EILO) is common in young people with exertional breathing difficulties. Psychological characteristics have been proposed as underlying contributors; however, the evidence for this is limited.
Objectives: Describe self-reported health, self-efficacy, and anxiety symptoms in adolescents with EILO, and address possible associations with EILO subtypes and severity.
Methods: Cross-sectional study of 71/180 (39%) adolescents tested for EILO at Haukeland University Hospital during 2014–2016, age range 14–18 years. Validated questionnaires were used to assess general self-rated health, subjective health complaints (Health Behavior in School-aged Children-Symptom Check List; HBSC-SCL), general self-efficacy (GSE), and anxiety symptoms (SCARED). The outcomes were compared with normative data from comparable unselected populations.
Results: The HBSC-SCL items for somatic complaints revealed weekly or more often occurrence of headache in 42%, abdominal pain in 30%, backache in 31%, and dizziness in 32%. For psychological complaints, corresponding figures were 26% for feeling low, 43% for irritability or bad mood, 33% for feeling nervous, and 38% for sleep problems. Mean (range) GSE score was 3.13 (2.2–4.0), and reports suggesting anxiety symptoms were rare. The outcomes were in line with normative data from comparable unselected populations. Self-rated health, and scores obtained for HBSC-SCL, GSE, and SCARED were similarly distributed across EILO subtypes and severity.
Conclusion: Self-reported health, self-efficacy, and level of anxiety symptoms in adolescents with laryngoscopically confirmed EILO were similar to data obtained in comparable unselected populations, irrespective of EILO subtype and severity. The findings challenge the notion that pediatric EILO is causally related to psychological problems.
Introduction
Exercise-related breathing problems caused by laryngeal airflow obstruction (EILO) are relatively common in otherwise healthy young individuals. Studies of unselected childhood and adolescent populations report prevalence rates of 5 and 7%, respectively (1, 2). Moreover, a recent large study of recreational runners revealed inspiratory wheeze in nearly 10%, suggesting that EILO still might be an under-recognized condition in the general population (3). This clinical scenario was previously seen as a form of vocal fold (cord) dysfunction (VCD), and therefore often labeled exercise induced paradoxical vocal fold (cord) motion (PVFM or PVCM). Better diagnostic tools have improved the understanding that vocal fold adduction per se might not represent an “inciting incident” in many patients (4, 5). Therefore, a task force appointed by the European Respiratory Society (ERS), the European Laryngological Society (ELS), and the American College of Chest Physician (ACCP) has proposed a taxonomy that rests on findings made by laryngoscopy (6, 7). The umbrella term “inducible laryngeal obstruction” (ILO) should be linked to a description of the predominant anatomical location of the obstruction; e.g., glottic or supraglottic or both. The inducer should be listed first, hence the acronym EILO for obstruction induced by exercise.
Historically, VCD carried strong psychological and even psychiatric connotations (8–10). Recent literature have questioned this notion, and suggested that the causality might be reverse; i.e., that potential psychological associations might in fact be secondary to the dyspnea and the sense of failure to control breathing while under pressure (11). Studies of asthma have suggested links between respiratory symptoms and psychological and/or emotional factors and/or coping mechanisms (12–16). However, the direction of these associations is not self-evident, and may vary between patients. Although certainly important, these issues have not been properly addressed in young people with EILO. Traditionally, treatment of EILO has focused on breathing advice, speech therapy and psychological support. In recent years, there has been a development toward more “mechanistic interventions,” such as inspiratory muscle training and even irreversible surgery (17–22). The role of psychological problems in this group of patients is therefore important to establish.
We hypothesized that a higher rate of psychological symptoms would be most prominent in patients with the most severe findings, or in patients with glottic EILO, as this subtype might resemble what used to be labeled VCD. Our aim was to study self-reported health, self-efficacy, and anxiety across EILO subtypes and severity, diagnosed and classified as proposed by the ERS/ELS/ACCP nomenclature. A control group was not included, but the outcome data were compared to normative data obtained from large groups of comparable individuals.
Methods
Ethical Considerations
The Regional Committee for Medical Research Ethics for Western Norway had approved the study before it was commenced, Protocol no. 2017/299. Informed written consent was obtained from all participants.
Subjects Descriptions
In this cross-sectional study, all adolescents (age range 14–18 years) enrolled in the EILO registry at Haukeland University Hospital in Bergen, Norway, during 2014–2016 were invited to participate. A letter of invitation, a paper-based consent form, the questionnaires listed below, and a prepaid return envelope, were sent by post to the participants' home address.
The EILO registry enrolls patients referred for investigation of unexplained exercise related breathing problems and tested for EILO by completing a continuous laryngoscopy exercise (CLE) test, performed as described in detail previously (23). Asthma and/or exercise induced bronchial obstruction (EIB) do not preclude enrollment in this registry; however, if present adequate treatment should be instituted and the presenting symptoms should not resemble those of EIB. Great care is taken to exclude (to the extent possible) that asthma plays a significant role in the enrolled patients' exercise related respiratory problems. Untreated or under-treated asthma is considered contraindication for performing a CLE-test, but well-treated stable asthma is not, as the two conditions may co-exist. Any use of asthma medication is reported in the questionnaire filled in at enrollment.
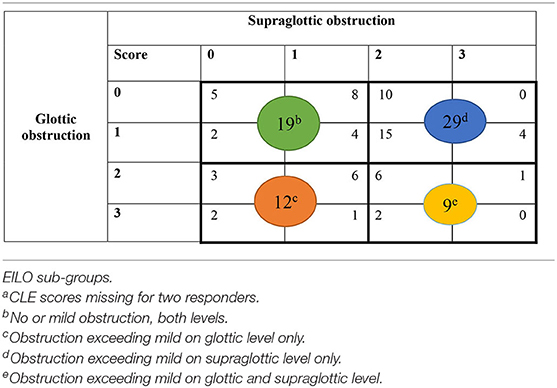
EILO was diagnosed according to obstruction in the larynx on two levels; glottic and supraglottic. EILO severity and subtype were scored according to published criteria (24). Only two highly experienced raters performed all scoring procedures. Both raters reviewed the videos retrospectively and individually, and all ratings were performed in one session, solving disagreements subsequently by consensus. No obstruction was classified as 0, mild as 1, moderate as 2 and severe as 3 (Figure 1) (24). For the purpose of this article, the patients were split into four subgroups based on their CLE scores obtained at maximum intensity exercise at the glottic and supraglottic laryngeal levels: 1 = no or mild obstruction at both levels; 2 = obstruction exceeding mild on glottic level only; 3 = obstruction exceeding mild on supraglottic level only; 4 = obstruction exceeding mild on both glottic and supraglottic level. For the purpose of this study, subgroup 1 was seen as normal; subgroup 2 as predominantly glottic EILO; subgroup 3 as predominantly supraglottic EILO; and subgroup 4 as severe EILO.
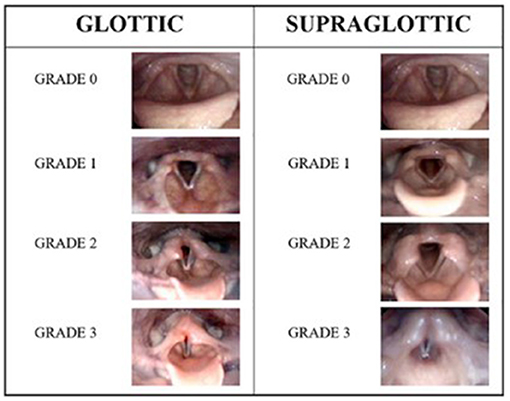
Figure 1. The human grading system according to Maat et al. (24) illustrated by endoscopic photographic images during exercise from the larynx showing the different grades of laryngeal obstruction at the glottic and supraglottic levels.
Questionnaires
A general questionnaire was applied to obtain information on age, gender, health, medication use, and the level of parental education. Specific questions were asked about the participants' physical activities and sports, and how they performed their training, such as “are you active in sport,” “what type of sport are you involved in,” and “how many times per month do you practice your sport?.”
General Self-Rated Health
General self-rated health was assessed by the question “would you say your health is.” and then rated on a 4-point scale ranging from “poor” to “excellent,” and thereafter responses were assigned values from 1 to 4, respectively. The question has demonstrated good validity and reliability in adolescent populations (25, 26).
Subjective Health Complaints
The Health Behavior in School-aged Children – Symptom Check List (HBSC-SCL) assesses the occurrence of eight somatic and psychological symptoms. The participants were asked to rate the frequency experienced in the past 6 months with items divided into the psychological sub-score (feeling low/depressed, irritable/bad tempered, nervous, and sleeping difficulties) and the somatic sub-score (headache, abdominal pain, backache, and feeling dizzy). Each item was assessed on a 5-point response scale ranging from daily (4) to rarely/never (0). Two sub scores (0–16) and a total sum score (0–32) were calculated (27). Other studies have reported high reliability and validity for adolescents between 11 and 15 years (27, 28). We applied the translated and validated Norwegian version (28).
General Self-Efficacy (GSE)
GSE was measured using the 10-item scale based on Bandura's concept of self-efficacy. The scale is designed for subjects from 12 years of age and older (29). The GSE scale has demonstrated good psychometric properties (30, 31). A validated Norwegian version was used (31). The scale is measured on a 4-point Likert scale ranging from 1 (not true at all) to 4 (exactly true).
Anxiety
Anxiety symptoms were measured with the short version of the Screen for Child Anxiety Related Disorder (SCARED) developed for adolescents between 8 and 18 years (32). The scale measured five statements on a 3-point Likert scale ranging from not true (0) to often true (2). The items are summarized to calculate a total score ranging from 0 to 10. The short version has similar well-established psychometric properties as the original scale (32). No validation studies have been conducted on the Norwegian translation, but it has been used in different studies (33, 34).
Statistical Analysis
Descriptive analyses were used to assess means and standard deviations (SD) of general health, anxiety, subjective health complaints and GSE, whereas demographic and clinical characteristics were reported as numbers and proportions. One-Way ANOVA was used to investigate if there were any differences between the four EILO sub-groups regarding general health, anxiety, subjective health complaint, and GSE. The criterion for statistical significance was p-value ≤ 0.05. All analyses were conducted using Statistical Package for the Social Sciences (SPSS) Version 24 for Windows.
Results
Participant Characteristics
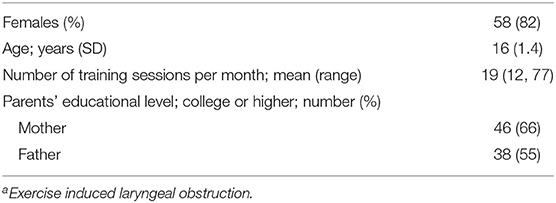
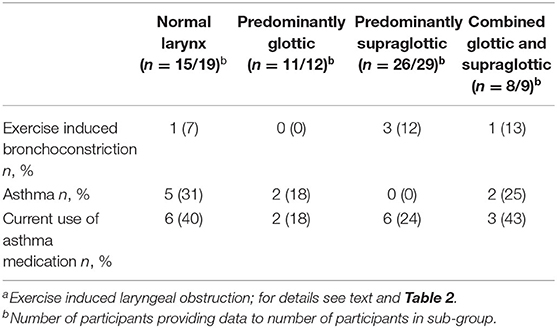
There were 71/180 (39%) adolescents who returned the questionnaires, of whom 58 (82%) were females, and the mean (SD) age was 16 (1.4) years (Table 1). Background variables and EILO subgroups for the participants are displayed in Table 2. A larger fraction of non-responders than responders had been classified as normal (subgroup 1). In two of the responders, the quality of the CLE test did not allow sub-grouping, thus EILO could be classified in 69/71 participants. Few participants reported asthma or EIB, and there were no differences between the EILO subgroups (Table 3).
General Self-Rated Health
Most participants 61/70 (87%) rated their health as “good” or “very good,” and only one responded “poor.” There were no significant differences between the EILO subgroups (Tables 4, 5).
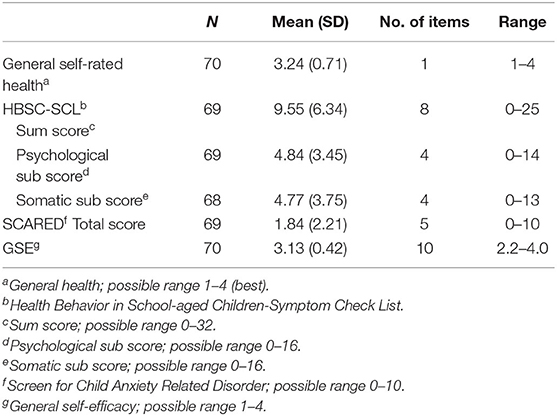
Table 4. Scores on patient reported outcome measures among participating adolescents with exercise induced laryngeal obstruction (EILO).
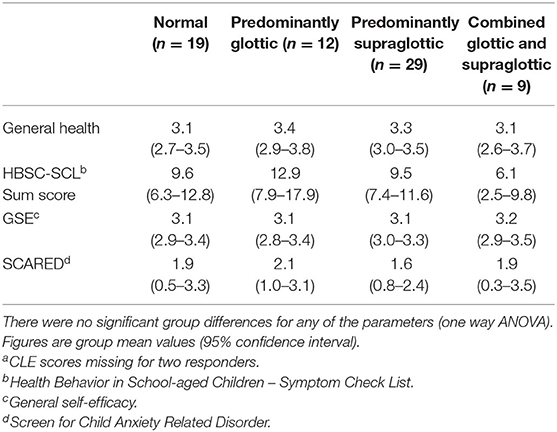
Table 5. Scores on patient reported outcome measures of 69 participantsa, split by the four types of exercise induced laryngeal obstruction (EILO); for details see text and Table 2.
Subjective Health Complaints (HBSC-SCL)
Headache and abdominal pain were the most common subjective somatic health complaints, with 28 (42%) and 20 (30%) reporting headache and abdominal pain weekly or more often, respectively. The most common subjective psychological health complaint was being irritable or in a bad mood, with 30 (43%) responding that this occurred weekly or more often. Mean HBSC-SCL score was 9.55, with responses ranging from 0 to 25 of the possible range 0–32. There were no significant differences between the four EILO subgroups (Tables 4, 5).
Self-Efficacy
The overall mean score for GSE were 3.13, which is considered well within normal range. The scores did not differ between the four EILO subgroups (Tables 4, 5).
Anxiety
The majority of the participants (n = 69) reported no symptoms of anxiety. The responses did not differ between the four EILO subgroups (Tables 4, 5).
Discussion
The major finding from this study was that adolescents with EILO rated their health as good, with data for general health, subjective health complaints (psychological and somatic), self-efficacy, and anxiety symptoms similar to data obtained from comparable unselected populations. Moreover, these outcome variables were unrelated to EILO subtype and severity.
Strengths and Weaknesses of the Study
A major strength of this study was that it approached all adolescents included in the EILO-registry between 2014 and 2016 at Haukeland University Hospital, which is a nationwide center for EILO and therefore receives referrals from a broad and representative selection of young people suffering from EILO. The idea was that this set-up should ensure a correspondingly broad and representative recruitment of EILO patients, producing outcome data with a high degree of generalizability. However, the rather disappointing rate of participation of 39% challenged this concept, and this is the obvious and major weakness of the study. Nonetheless, the finding that general health, subjective health complaints, self-efficacy, and anxiety were similarly distributed over EILO subtypes and severity certainly challenges the notion that these characteristics should be causally implicated in EILO. There were 82% female participants, which is approximately representative for the gender distribution of the EILO registry with 75% being females, and with previous studies reporting similarly high rates of EILO among females (1, 2). There was a high level of exercise frequency among the participants, which is also consistent with previous studies, reporting that EILO is more common in physically active adolescent and in athletes (1, 35). One may speculate if physically highly active adolescents who experience respiratory symptoms are more likely to seek medical advice than average adolescents with a more sedentary lifestyle. It was a limitation of the study that the participants received the questionnaires after they were diagnosed with EILO, and thus we do not know their status prior to this point in their life. It was also a limitation that we had no healthy controls matched to our participants, but instead had to compare our findings to normative data obtained in comparable large population studies. A co-existing asthma or use of asthma medication was relatively rare and also similarly distributed across the EILO sub-groups, and thus not likely to have influenced the major findings in significant ways.
General Health and Health Behavior in School-Aged Children
The rate of subjective health complaints might seem high, but the findings were similar to data reported from a population based study of Norwegian adolescents (36). Moreover, a large international survey of pain in adolescents reported similarly high rates of health complaints, with more than 50 % reporting headache, and 49.8 % reporting abdominal pain weekly or more often (37). Thus, adolescents with EILO did not differ from otherwise comparable peers in terms of self-perceived health (25).
General Self-Efficacy
The mean GSE score of 3.1 was comparable to data reported from a study of Norwegian otherwise comparable adolescents (38, 39). Self-efficacy determines how people feel, think, motivate themselves and behave in new and challenging situations and is considered an important feature in behavioral change and coping (40, 41). A Norwegian study of adolescents reported positive associations between GSE and health-related quality of life (39). Thus, the good (normal) GSE score observed in our EILO patients may help them cope with their condition.
Anxiety
Anxiety symptoms measured the SCARED questionnaire were in line with data obtained in comparable reference populations (33). Moreover, as for the other parameters tested in this study, we found no gradients over EILO subtypes or severity. Particularly it was of interest, and somewhat surprising, that the level of anxiety for the glottic subtype of EILO was in line with the other EILO subgroups and with the data reported from a from a population based study (33). Two individuals had the highest possible score on the SCARED questionnaire (11); one of them had a normal laryngeal response to exercise (i.e., no EILO) and the other a predominantly glottic EILO.
The CLE scoring system has been questioned by some authors, and studies have reached somewhat variable conclusions regarding repeatability and precision (23, 42, 43). In order to avoid pitfalls in this area, only two highly experienced raters performed all scoring procedures, both having assessed CLE recordings from more than 2,000 individuals. Both raters reviewed the videos retrospectively and individually, but all in one session, solving disagreements subsequently by consensus. The CLE scoring system opened for studying if the outcomes that we addressed varied across EILO subtypes and EILO severity. We were particularly interested in the glottic subtype, as we have hypothesized that this EILO variant may resemble what was previously labeled exercise induced VCD. Moreover, it had seemed reasonable to hypothesis that if personality traits or psychological mechanisms were involved in the causal chain leading to EILO, this would be most evident in patients with the most severe subtype; i.e., in participants in whom both glottic and supraglottic scores were at least moderate or severe. However, we found no such tendencies; the confidence intervals for all the addressed parameters showed nearly full overlap in all subgroups. One way of interpreting this finding is that the addressed outcomes are not involved in the causal chain leading to EILO. However, due to our low rate of participation, this interpretation must obviously be tested in future studies. Moreover, we advise future studies to rate patients before they are tested and assigned the EILO diagnosis. We know that worldwide, too many of these patients are misdiagnosed as malingerers or as suffering from poorly controlled asthma, and therefore exposed to asthma medication with no effect (44, 45). To live for years in such situations conceivably challenges self-esteem and psychological well-being. Thus, a correct diagnosis relieves stress, and represents a “new beginning” for many patients.
Conclusion
Our findings indicate good self-rated health and self-efficacy in adolescents with EILO, and no more anxiety symptoms than usually found in this age group. None of these outcome variables were associated with EILO subtype or severity. The findings question the notion that psychological problems are causally involved in EILO.
Data Availability Statement
In accordance with the approvals granted for this study by The Regional Committee on Medical Research Ethics and The Norwegian Data Inspectorate, the data files are stored securely and in accordance with the Norwegian Law of Privacy Protection. The data file cannot be made publicly available as this might compromise the respondents' privacy. A subset of the data file with anonymized data can be made available to interested researchers upon reasonable request to Hege Clemm (hsyh@helse-bergen.no), providing Norwegian privacy legislation and GDPR are respected, and that permission is granted from The Norwegian Data Inspectorate and the data protection officer at Haukeland University Hospital.
Ethics Statement
The studies involving human participants were reviewed and approved by The Regional Committee for Medical Research Ethics for Western Norway, Protocol no. 2017/299. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
MB collected the data, analyzed the data, drafted the initial manuscript, reviewed, and edited the manuscript. BV, MH, HC, OR, MV, and TH designed the data collection instruments. BV, TH, HC, and JD reviewed and edited the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Christensen PM, Thomsen SF, Rasmussen N, Backer V. Exercise-induced laryngeal obstructions: prevalence and symptoms in the general public. Eur Arch Oto-rhino-laryngol. (2011) 268:1313–9. doi: 10.1007/s00405-011-1612-0
2. Johansson H, Norlander K, Berglund L, Janson C, Malinovschi A, Nordvall L, et al. Prevalence of exercise-induced bronchoconstriction and exercise-induced laryngeal obstruction in a general adolescent population. Thorax. (2015) 70:57–63. doi: 10.1136/thoraxjnl-2014-205738
3. Sails J, Hull JH, Allen H, Darville L, Walsted ES, Price OJ. High prevalence of exercise-induced stridor during Parkrun: a cross-sectional field-based evaluation. BMJ Open Resp Res. (2020) 7:e000618. doi: 10.1136/bmjresp-2020-000618
4. Roksund OD, Maat RC, Heimdal JH, Olofsson J, Skadberg BT, Halvorsen T. Exercise induced dyspnea in the young. Larynx as the bottleneck of the airways. Respir Med. (2009) 103:1911–8. doi: 10.1016/j.rmed.2009.05.024
5. Clemm HSH, Sandnes A, Vollsaeter M, Hilland M, Heimdal JH, Roksund OD, et al. The heterogeneity of exercise induced laryngeal obstruction. Am J Respir Crit Care Med. (2018) 197:1068–9. doi: 10.1164/rccm.201708-1646IM
6. Christensen PM, Heimdal JH, Christopher KL, Bucca C, Cantarella G, Friedrich G, et al. ERS/ELS/ACCP 2013 international consensus conference nomenclature on inducible laryngeal obstructions. Eur Respir Rev. (2015) 24:445–50. doi: 10.1183/16000617.00006513
7. Halvorsen T, Walsted ES, Bucca C, Bush A, Cantarella G, Friedrich G, et al. Inducible laryngeal obstruction: an official joint European Respiratory Society and European Laryngological Society statement. Eur Respir J. (2017) 50:1602221. doi: 10.1183/13993003.02221-2016
8. Leo RJ, Konakanchi R. Psychogenic respiratory distress: a case of paradoxical vocal cord dysfunction and literature review. Prim Care Companion J Clin Psychiatry. (1999) 1:39–46. doi: 10.4088/PCC.v01n0203
9. Husein OF Husein TN Gardner R Chiang T Larson DG Obert K. Formal psychological testing in patients with paradoxical vocal fold dysfunction. Laryngoscope. (2008) 118:740–7. doi: 10.1097/MLG.0b013e31815ed13a
10. Freedman MR, Rosenberg SJ, Schmaling KB. Childhood sexual abuse in patients with paradoxical vocal cord dysfunction. J Nerv Ment Dis. (1991) 179:295–8. doi: 10.1097/00005053-199105000-00009
11. Roksund OD, Heimdal JH, Clemm H, Vollsaeter M, Halvorsen T. Exercise inducible laryngeal obstruction: diagnostics and management. Paediatr Respir Rev. (2017) 21:86–94. doi: 10.1016/j.prrv.2016.07.003
12. Mancuso CA, Rincon M, McCulloch CE, Charlson ME. Self-efficacy, depressive symptoms, and patients' expectations predict outcomes in asthma. Med Care. (2001) 39:1326–38. doi: 10.1097/00005650-200112000-00008
13. Cevik Guner U, Celebioglu A. Impact of symptom management training among asthmatic children and adolescents on self-efficacy and disease course. J Asthma. (2015) 52:858–65. doi: 10.3109/02770903.2015.1010732
14. Cui W, Zack MM, Zahran HS. Health-related quality of life and asthma among United States adolescents. J Pediatr. (2015) 166:358–64. doi: 10.1016/j.jpeds.2014.10.005
15. Carpentier MY, Mullins LL, Van Pelt JC. Psychological, academic, and work functioning in college students with childhood-onset asthma. J Asthma. (2007) 44:119–24. doi: 10.1080/02770900601182418
16. Bruzzese J-M, Reigada LC, Lamm A, Wang J, Li M, Zandieh SO, et al. Association of youth and caregiver anxiety and asthma care among urban young adolescents. Acad Pediatr. (2016) 16:792–8. doi: 10.1016/j.acap.2016.03.009
17. Sandnes A, Andersen T, Hilland M, Ellingsen TA, Halvorsen T, Heimdal JH, et al. Laryngeal movements during inspiratory muscle training in healthy subjects. J Voice. (2013) 27:448–53. doi: 10.1016/j.jvoice.2013.02.010
18. Sandnes A, Andersen T, Clemm HH, Hilland M, Vollsaeter M, Heimdal JH, et al. Exercise-induced laryngeal obstruction in athletes treated with inspiratory muscle training. BMJ Open Sport Exerc Med. (2019) 5:e000436. doi: 10.1136/bmjsem-2018-000436
19. Sandnes A, Hilland M, Vollsaeter M, Andersen T, Engesaeter IO, Sandvik L, et al. Severe Exercise-induced laryngeal obstruction treated with supraglottoplasty. Front Surg. (2019) 6:44. doi: 10.3389/fsurg.2019.00044
20. Mehlum CS, Walsted ES, Godballe C, Backer V. Supraglottoplasty as treatment of exercise induced laryngeal obstruction (EILO). Eur Arch Otorhinolaryngol. (2016) 273:945–51. doi: 10.1007/s00405-015-3823-2
21. Maat RC, Roksund OD, Olofsson J, Halvorsen T, Skadberg BT, Heimdal JH. Surgical treatment of exercise-induced laryngeal dysfunction. Eur Arch Otorhinolaryngol. (2007) 264:401–7. doi: 10.1007/s00405-006-0216-6
22. Famokunwa B, Sandhu G, Hull JH. Surgical intervention for exercise-induced laryngeal obstruction: a UK perspective. Laryngoscope. (2020) 130:E667–73. doi: 10.1002/lary.28497
23. Heimdal JH, Roksund OD, Halvorsen T, Skadberg BT, Olofsson J. Continuous laryngoscopy exercise test: a method for visualizing laryngeal dysfunction during exercise. Laryngoscope. (2006) 116:52–7. doi: 10.1097/01.mlg.0000184528.16229.ba
24. Maat RC, Roksund OD, Halvorsen T, Skadberg BT, Olofsson J, Ellingsen TA, et al. Audiovisual assessment of exercise-induced laryngeal obstruction: reliability and validity of observations. Eur Arch Otorhinolaryngol. (2009) 266:1929–36. doi: 10.1007/s00405-009-1030-8
25. Fosse NE, Haas SA. Validity and stability of self-reported health among adolescents in a longitudinal, nationally representative survey. Pediatrics. (2009) 123:496–501. doi: 10.1542/peds.2008-1552
26. Lundberg O, Manderbacka K. Assessing reliability of a measure of self-rated health. Scand J Public Health. (1996) 24:218–24. doi: 10.1177/140349489602400314
27. Gariepy G, McKinnon B, Sentenac M, Elgar FJ. Validity and reliability of a brief symptom checklist to measure psychological health in school-aged children. Child Indic Res. (2016) 9:471–84. doi: 10.1007/s12187-015-9326-2
28. Haugland S, Wold B. Subjective health complaints in adolescence—reliability and validity of survey methods. J Adolesc. (2001) 24:611–24. doi: 10.1006/jado.2000.0393
29. Schwarzer R, Bäßler J, Kwiatek P, Schröder K, Zhang JX. The assessment of optimistic self-beliefs: comparison of the German, Spanish, and Chinese versions of the general self-efficacy scale. Appl Psychol. (1997) 46:69–88. doi: 10.1111/j.1464-0597.1997.tb01096.x
30. Leganger A, Kraft P, Røysamb E. Perceived self-efficacy in health behaviour research: conceptualisation, measurement and correlates. Psychol Health. (2000) 15:51–69. doi: 10.1080/08870440008400288
31. Røysamb E, Schwarzer R, Jerusalem M. Norwegian version of the general perceived self-efficacy scale (1998). Available online at: https://userpage.fu-berlin.de/~health/norway.htm (accessed June 09, 2021).
32. Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry. (1999) 38:1230–6. doi: 10.1097/00004583-199910000-00011
33. Sivertsen B, Petrie KJ, Wilhelmsen-Langeland A, Hysing M. Mental health in adolescents with Type 1 diabetes: results from a large population-based study. BMC Endocr Disord. (2014) 14:83. doi: 10.1186/1472-6823-14-83
34. Sivertsen B, Harvey AG, Pallesen S, Hysing M. Mental health problems in adolescents with delayed sleep phase: results from a large population-based study in Norway. J Sleep Res. (2015) 24:11–8. doi: 10.1111/jsr.12254
35. Nielsen EW, Hull JH, Backer V. High prevalence of exercise-induced laryngeal obstruction in athletes. Med Sci Sports Exerc. (2013) 45:2030–5. doi: 10.1249/MSS.0b013e318298b19a
36. Myrtveit Sæther SM, Sivertsen B, Haugland S, Bøe T, Hysing M. Health complaints in late adolescence; Frequency, factor structure and the association with socio-economic status. Scand J Public Health. (2017) 46:141–9. doi: 10.1177/1403494817711359
37. Swain MS, Henschke N, Kamper SJ, Gobina I, Ottová-Jordan V, Maher CG. An international survey of pain in adolescents. BMC Pub Health. (2014) 14:447. doi: 10.1186/1471-2458-14-447
38. Natvig GK, Albrektsen G, Anderssen N, Qvarnstrøm U. School-related stress and psychosomatic symptoms among school adolescents. J School Health. (1999) 69:362–8. doi: 10.1111/j.1746-1561.1999.tb06430.x
39. Kvarme LG, Haraldstad K, Helseth S, Sørum R, Natvig GK. Associations between general self-efficacy and health-related quality of life among 12-13-year-old school children: a cross-sectional survey. Health Qual Life Outcomes. (2009) 7:85. doi: 10.1186/1477-7525-7-85
40. Bandura A. Self-efficacy. In: Ramachaudran VS, editor. Encyclopedia of Human Behavior, Vol. 4. New York, NY: Academic Press (1994). p. 71–81.
41. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. (1977) 84:191. doi: 10.1037/0033-295X.84.2.191
42. Norlander K, Christensen PM, Maat RC, Halvorsen T, Heimdal JH, Moren S, et al. Comparison between two assessment methods for exercise-induced laryngeal obstructions. Eur Arch Otorhinolaryngol. (2015) 273:425–30. doi: 10.1007/s00405-015-3758-7
43. Walsted ES, Hull JH, Hvedstrup J, Maat RC, Backer V. Validity and reliability of grade scoring in the diagnosis of exercise-induced laryngeal obstruction. ERJ Open Res. (2017) 3:00070-2017. doi: 10.1183/23120541.00070-2017
44. Hull JH. Not all wheeze is asthma: time for patients to exercise their rights. Thorax. (2015) 70:7–8. doi: 10.1136/thoraxjnl-2014-206096
Keywords: exercise-induced laryngeal obstruction, self-reported health, adolescents, breathing difficulties, self-efficacy
Citation: Benestad MR, Drageset J, Clemm H, Røksund OD, Vollsæter M, Halvorsen T, Hysing M and Vederhus BJ (2021) Self-Reported Health in Adolescents With Exercise-Induced Laryngeal Obstruction; A Cross-Sectional Study. Front. Pediatr. 9:617759. doi: 10.3389/fped.2021.617759
Received: 15 October 2020; Accepted: 09 June 2021;
Published: 08 July 2021.
Edited by:
Emil Schwarz Walsted, Bispebjerg Hospital, DenmarkReviewed by:
Anand Marya, University of Puthisastra, CambodiaOliver J. Price, University of Leeds, United Kingdom
Copyright © 2021 Benestad, Drageset, Clemm, Røksund, Vollsæter, Halvorsen, Hysing and Vederhus. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Merete R. Benestad, merete.roineland.benestad@helse-bergen.no
 Merete R. Benestad
Merete R. Benestad Jorunn Drageset1,3
Jorunn Drageset1,3  Hege Clemm
Hege Clemm Ola D. Røksund
Ola D. Røksund Thomas Halvorsen
Thomas Halvorsen Mari Hysing
Mari Hysing