Constipation and Lower Urinary Tract Dysfunction in Children and Adolescents: A Population-Based Study
- 1Centro de Distúrbios Miccionais na Infância (CEDIMI), Escola Bahiana de Medicina e Saúde Pública, Universidade Federal da Bahia, Salvador, Brazil
- 2Universidade Federal de Juiz de Fora, Juiz de Fora, Brazil
Objective: To evaluate the correlation between constipation and lower urinary tract dysfunction (LUTD) and nocturnal enuresis in a population-based study.
Material and methods: This is a cross-sectional study. The criteria for inclusion were children and adolescents of between 5 and 17 years and who agreed to sign the informed consent form. The study excluded students with neurological problems or who had documented abnormalities of the urinary tract. To identify the presence and severity of LUTD, we used the Voiding Dysfunction Symptom Score (DVSS). To evaluate the presence of constipation, Rome III questionnaire was used.
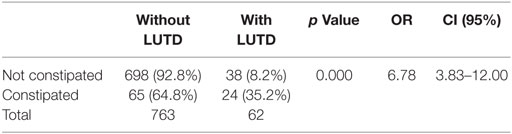
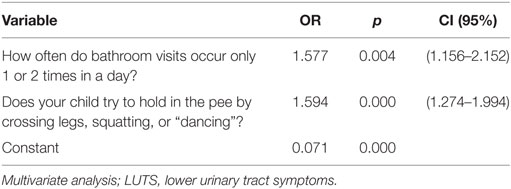
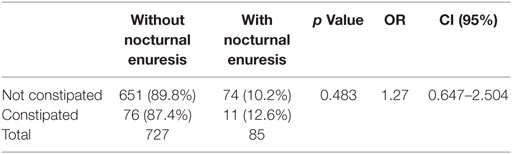
Results: We interviewed 829 children and adolescents, of which 416 (50.18%) were male. The mean (SD) age was 9.1 (±2.9) years. The overall prevalence of LUTD was 9.1%, predominantly in girls (15 versus 3.1%, p < 0.001). Constipation was found in 9.4% of boys and 12.4% of girls (p = 0.169). Constipated children were 6.8 times more likely to have LUTD than those not constipated (p < 0.001, coefficient and correlation of 0.411). Constipation was found in 8.2% of children without LUTD and in 35.2% of children with LUTD. We performed multivariate analysis to identify urinary symptoms that are independent predictors of the presence of constipation. The presence of infrequent urination (p = 0.004) and holding maneuvers (p < 0.001) were independent predictors. It was noted also noted that constipated children, according to the Rome III criteria, possess a worse DVSS (p < 0.001). Regarding the presence of nocturnal enuresis, 12.6% of children and adolescents had constipation in association with this symptom. However, this relationship was not statistically significant (p = 0.483).
Conclusion: Constipated children were 6.8 times more likely to have LUTD than those not constipated. Among the urinary symptoms, infrequent voiding and holding maneuvers are independent factors of urinary expressions in constipated children. Children with more severe constipation have more prominent urinary symptoms. The presence of enuresis was not associated with constipation.
Introduction
Constipation accounts for about 3–5% of consultations in pediatrics and up to 25% of consultations in pediatric gastroenterology (1). During childhood, one-third of children relate having had constipation at some time, most of whom had functional constipation (2). The presence of lower urinary tract dysfunction (LUTD) is a major cause of medical visits to pediatric urologists, accounting for up to 40% of cases (3). Its prevalence is around 2–25% of the population, varying with the intensity of symptoms measured (4).
The anatomical proximity between rectum and bladder and the innervation in common between the two structures may justify the association between constipation and LUTD (5), which is called bladder bowel dysfunction (BBD) (6). Children with BBD are more likely to develop emotional problems such as insecurity, anxiety, and low self-esteem, as well as behavioral problems (7).
Recently, Veiga et al. (8) demonstrated that constipation is associated not only with dysfunctional urination but also overactive bladder (OAB). In this study, 54.9% of children with OAB had constipation, in addition to being almost three times more likely to develop constipation than children without OAB. Some authors have demonstrated that children with dysfunctional voiding tend to have functional constipation, whereas children with OAB tend to have functional non-retentive fecal incontinence (9). Therefore, in approaching the child, it is essential that both disorders are investigated and treated.
The association between enuresis and constipation is also well established and known. In a study involving 30 enuretic children, Hogdes and Anthony (10) showed that 80% of them were also constipated and that these obtained significant resolution of their enuretic problem with laxative therapy. This association, however, needs further clarification preferably a population- or community-based study.
In spite of BBD being well described, to the best of our knowledge, there are no population-based studies to assess in detail the association between symptoms of constipation and lower urinary tract symptoms (LUTS). The term BBD is too generic: due to the large spectrum of LUTS presentation, the severity of urinary symptoms and constipation, different types of association between specific urinary and fecal symptoms could be found. In other words, constipation could be associated with more retentive symptoms such as low voiding frequency and children with a more severe constipation could present a more severe LUTS. Thus, this study aims to evaluate the correlation between constipation and LUTS and nocturnal enuresis in a population analysis.
Materials and Methods
This is a cross-sectional study conducted in two Brazilian cities with a combined population of about 4 million. Data collection was carried out in public places from May to July 2015. The criteria for inclusion were children and adolescents of between 5 and 17 years who agreed to sign the informed consent form. Individuals who happened to pass by the collection points were approached at random and invited to participate. The study excluded individuals with neurological problems or who had documented abnormalities of the urinary tract. The study was submitted to the ethics committee of our institution and obtained approval for its implementation.
To identify the presence and severity of LUTD, we used the Voiding Dysfunction Symptom Score (DVSS), modified, and validated for the language in use (11, 12). This questionnaire contains 10 questions, of which 9 are related to clinical symptoms and 1 is related to environmental factors (social and family problems). For questions 1–9, numerical answers were taken, according to the Likert scale with scores from 0 to 3 based on the presence and severity of symptoms. For question 10, a score of 0 was given if there were no events related to stress or 3 if these were present. Girls with six or more points and boys nine or more points were considered to have LUTD.
The presence of urinary symptoms more than 1–2 times per week (score 1) was considered positive for each distinct question of the DVSS. Children who had urgency at least 1–2 times per week were considered to have an OAB. In order to investigate the presence of nocturnal enuresis, the children were asked whether or not they had experienced bedwetting events. The bedwetting episodes were subdivided into two categories: children who had less than three bedwetting events in a week and children who had more than three bedwetting episodes per week.
To evaluate the presence of constipation, we applied the Rome III child questionnaire, for ages 4–18 years. Participants who responded positively to two out of the six questions were considered constipated (13).
Statistical Analysis
SPSS version 20.0 was used for statistical analysis. Numerical variables of age and score values were expressed as mean and SD or median and interquartile range (IQ). The variables included for analysis were age, gender, presence of enuresis, the DVSS, and Rome III scores. The age variable was divided into two groups: ≤9 and ≥10 years.
To perform the sample calculation, we estimated LUTD prevalence at 10% and accepted a difference of 3%, with 95% confidence level and requiring at least 385 participants in the survey.
Non-parametric variables of DVSS and Rome III scores were compared using the Spearman correlation, with p ≤ 0.05 considered significant. We performed a univariate analysis with chi-square test to compare proportions, with variables having p ≤ 0.05 considered significant, in order to test the association between constipation and the variables of nocturnal enuresis and LUTD. We adopted the manual procedure for the insertion and removal of variables.
Results
We interviewed 829 children and adolescents, of which 416 (50.18%) were male. The mean (SD) age was 9.1 (±2.9) years, with a median of 9 (7–11) years.
The median score of the DVSS was 2 with IQ from 0 to 4 (range 0–18). According to the DVSS, the overall prevalence of LUTD was 9.1%, predominantly in girls (15 versus 3.1%, p < 0.001). Constipation was found in 9.4% of boys and 12.4% of girls (p = 0.169).
A positive correlation was found between constipation and LUTD (Figure 1, p < 0.001, coefficient and correlation of 0.411). Constipated children were 6.8 times more likely to have LUTD than those not constipated (Table 1). Constipation was found in 8.2% of children without LUTD and in 35.2% of children with LUTD (p < 0.001, Table 1). However, 92.8% of non-constipated children did not have LUTD.
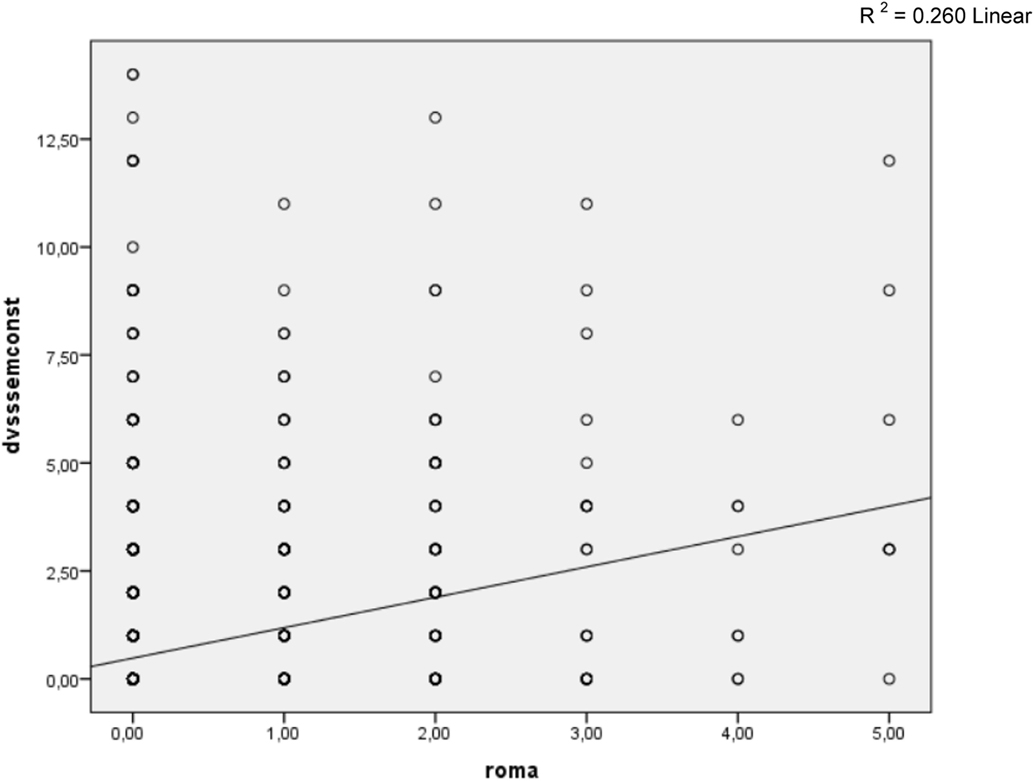
Figure 1. Spearman correlation between DVSS score (disregarding questions related to intestinal rhythm) and Rome III criteria. R2 = 0.260 linear.
Table 2 shows the relationship between constipated and non-constipated children according to responses on urinary issues in the DVSS. It may be noted that urinary incontinence, infrequent voiding, holding maneuvers, urinary urgency, dysuria, and stressful event, respectively, were associated with the presence of constipation. We performed multivariate analysis (Table 3) to identify urinary symptoms that are independent predictors of the presence of constipation. The presence of infrequent urination (p = 0.004) and holding maneuvers (p = 0.000) were the only independent predictors.
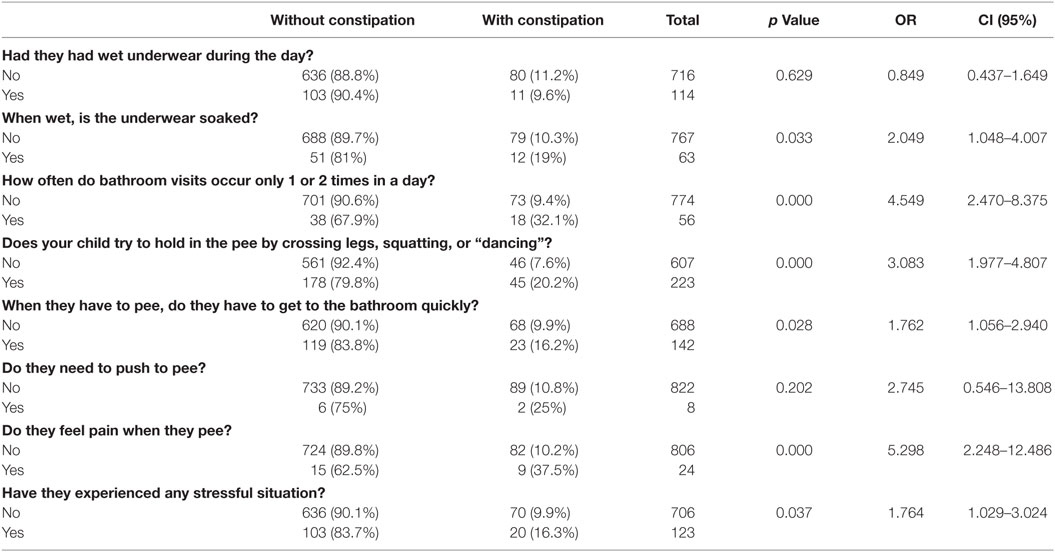
Table 2. Presence of urinary symptoms, according to DVSS in constipated and non-constipated children.
The final score of the DVSS, after eliminating questions about intestinal rhythm, which compares constipated and non-constipated children, is described in Table 4. It is noted that constipated children, according to the Rome III criteria, possess a worse DVSS (p < 0.001).
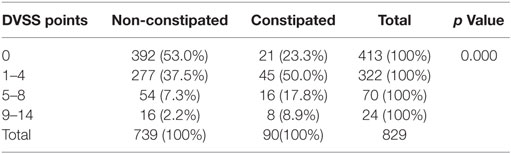
Table 4. Final score obtained in DVSS, without constipation questions, for constipated and non-constipated children.
Regarding the presence of nocturnal enuresis, 12.6% of children and adolescents had constipation in association with this symptom (Table 5). However, this relationship was not statistically significant (p = 0.483). Still, 89.8% of non-constipated children were not enuretic, as well.
Discussion
Our study shows that LUTD is associated with constipation in children. Although this association is well reported in the literature, there are surprisingly few studies on this topic with population samples. In our sample, 27% of constipated children have LUTD, with a 6.782 times greater chance of having voiding dysfunction compared with those who are not constipated.
One study has shown that 6.3% of school-age children have daytime urinary incontinence (14) and that some risk factors may be attributed to daytime urinary incontinence such as encopresis, nocturnal enuresis, and social concerns (15). As for constipation, a systematic review study (16) has shown that the prevalence of constipation among children ranged between 0.7 and 29.6%, with a median of 12%. Another study has reported that 36% of Brazilian children in public schools are constipated, with no differences among boys and girls (17).
In order to determine the prevalence of dysfunctional voiding symptoms and abnormal bowel habits, Chung et al. (18) found in their study that the prevalence of both abnormal voiding and bowel habits is 46.4 and 31.3%, respectively, among Korean children on a nationwide basis. Curiously, 18.4% of Korean children had both abnormal voiding and bowel habits. Only, 5.6% of children had nocturnal enuresis.
Surprisingly, although the relationship between constipation and LUT dysfunction is well established and well known, few articles address this issue. Those who have addressed the issue have only used convenience samples and additionally have not used a Rome III criteria questionnaire to evaluate the degree of constipation.
The study by Hadjizadeh and colleagues (19) classifies a convenience sample of children with functional constipation in which modified DVSS is applied (without the questions related to constipation). It found that 63.5% of constipated children had voiding dysfunction according to the DVSS. However, Rome III criteria were not used to determine the presence of constipation in the children studied. Bolat and colleagues (20) conducted a population-based study in Turkey in order to identify risk factors associated with daytime urinary incontinence. They applied DVSS to obtain the information relating to urinary and bowel habits of children, noting that constipated children are 2.6 times more likely to have daytime urinary incontinence. In that study, the Rome III criteria were not used.
It is important to use the criteria of Rome III to diagnose constipation in children, given the objective of standardizing the definitions of gastrointestinal disorders such as constipation (21). The application of this criterion in population samples is observed in the literature (22, 23), and yet there are few studies employing the Rome III criteria in correlation studies with LUTD.
One important finding in our study, which to the best of our knowledge has not been reported in the literature, was that children with more severe constipation symptoms had more intense urinary symptoms. Koff et al. (6) showed that voiding and defecatory symptoms, such as infrequent urination and fecal retention, are associated with vesicoureteral reflux and urinary tract infection, suggesting a worse clinical picture when BBD is active. However, when diagnosing constipation and LUTD by using the Rome III and DVSS, as was done in our study, it is possible to measure the impact of constipation on LUTS.
Although the relationship between LUTD and constipation is well known, the most common urinary symptoms in constipated children were not well elucidated until now. BBD, according to ICCS, is defined as a combination of functional bladder and bowel disturbances (24). The definition, however, does not embrace the whole spectrum of LUT dysfunction. We know that LUT dysfunction presentation is diverse, and each symptom may suggest various meanings. Our study shows that symptoms which represent delaying of micturition such as holding maneuvers and reducing the number of micturitions per day are independently associated with constipation. The degree of continence required to control urination and defecation depends on the proper use of the striated musculature of adjacent structures as well as the perception of stimuli coming from both the bladder (25) and the rectum. The relationship between the concomitant establishment of LUTD and constipation can be explained by considering the innervation of the structures involved in urinary and digestive tracts of the sacral region. Once the bladder and rectum have a common embryological origin, the motor neurons responsible for the innervation of these structures come from the existing nerve endings in S2 and S4. Furthermore, the external sphincters, both anal and urethral, also have common innervation via the pudendal nerve (26). Other explanations for the emergence of BBD include contraction of the anal sphincter during defecatory urgency may cause contraction of the urethral sphincter and reflexively inhibit bladder function; the reverse can also happen with contraction of the urethral sphincter during urinary urgency, inhibiting the defecatory function; a rectum full of feces can itself alter bladder function (27).
Loening-Baucke (28) demonstrated in a study that the treatment of constipation can improve urinary symptoms and, therefore, constipated children with voiding dysfunction have fewer recurrent episodes of urinary tract infection. Moreover, it is known that events that affect the child’s life, such as stress, trauma, or change in routine, can be the cause of voluntary retention of feces, accounting for the relationship between constipation and stressful events (29). In our study, the association between stressful events and constipation is apparent.
Voluntary retention of feces may be present in children with LUTD given that, just as some children perform holding maneuvers to hold in urine, in a similar way, these children also end up prolonging the trip to the bathroom to evacuate. Voluntary retention of feces is a major cause of functional constipation and can be triggered by previous episodes of painful removal of hardened and large amounts of feces (30). According to Morais and Tahan (31), before the urge to defecate, the child contracts the external sphincter of the anus and the gluteal muscles in order to prevent the elimination of feces and to succeed in retaining them. Retention maneuvers can also be used in LUTD, especially in OAB, due to involuntary detrusor contractions that manifest in children as urinary urgency; therefore, the contraction of the urethral external sphincter can promote relaxation of the detrusor by relieving the symptoms of OAB (32), which cause children normally to adopt postures such as crossing legs and squatting in order to suppress or relieve the involuntary bladder contractions (33).
Thus, the feces are retained, assisted by voluntary restraining. They lose liquid while remaining in the rectum and over time become more desiccated, which complicates their evacuation and leads to a clogged toilet. Furthermore, evacuation of dry and hardened feces becomes more troublesome, which causes a portion of the fecal mass not to be expelled during defecation and remain in the rectal ampoule. Stagnant feces accumulate in the ampoule to the point of belatedly stimulating the defecation reflex, which inadvertently causes the child to present fecal incontinence events.
This study showed no association between nocturnal enuresis and constipation, as did the study of Sarici et al. (34) which did not observe a significant association between constipation and enuresis, present in 13.2% of enuretic children in the study.
There are some limitations of this study. We did not evaluate the constipation by digital rectal examination or by rectal diameter on ultrasound. Also, we did not evaluate the dietary habits that could have some influence in the intestinal rhythm. Furthermore, this is a cross-sectional study and, therefore, we cannot establish any causal relationship.
Conclusion
Constipated children were 6.8 times more likely to have LUTD than those not constipated. Among the urinary symptoms, infrequent voiding and holding maneuvers are independent factors of urinary expressions in constipated children. Children with more severe constipation have more prominent urinary symptoms. The presence of enuresis was not associated with constipation.
Author Contributions
All authors listed have made substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Loening-Baucke V. Encopresis and soiling. Pediatr Clin North Am (1996) 43:279–98. doi:10.1016/S0031-3955(05)70406-5
2. Biggs WS, Dery WH. Evaluation and treatment of constipation in infants and children. Am Fam Physician (2006) 73:469–77.
3. Feldman AS, Bauer SB. Diagnosis and management of dysfunctional voiding. Curr Opin Pediatr (2006) 18(2):139–47.
4. Vaz GT, Vasconcelos MM, Oliveira EA, Ferreira AL, Magalhaes PG, Silva FM, et al. Prevalence of lower urinary tract symptoms in school-age children. Pediatr Nephrol (2012) 27(4):597–603. doi:10.1007/s00467-011-2028-1
5. Averbeck MA, Madersbacher H. Constipation and LUTS – how do they affect each other? Int Braz J Urol (2001) 37(1):16–28. doi:10.1590/S1677-55382011000100003
6. Koff SA, Wagner TT, Jayanthi VR. The relationship among dysfunctional elimination syndromes, primary vesicoureteral reflux and urinary tract infections in children. J Urol (1998) 160(3):1019–22. doi:10.1016/S0022-5347(01)62686-7
7. Von Gontard A, Niemczyk J, Weber M, Equit M. Specific behavioral comorbidity in a large sample of children with functional incontinence: report of 1,001 cases. Neurourol Urodyn (2014) 34(8):763–8. doi:10.1002/nau.22651
8. Veiga ML, Lordelo P, Farias T, Barroso C, Bonfim J, Barroso U Jr. Constipation in children with isolated overactive bladders. J Pediatr Urol (2013) 6(6):945–9. doi:10.1016/j.jpurol.2013.01.013
9. Burgers R, Jong TPVM, Visser M, Di Lorenzo C, Dijkgraaf MGW, Benninga MA. Functional defecation disorders in children with lower urinary tract symptoms. J Urol (2013) 189(5):1886–91. doi:10.1016/j.juro.2012.10.064
10. Hogdes SJ, Anthony EY. Occult megarectum – a commonly unrecognized cause of enuresis. Urology (2012) 79(2):421–4. doi:10.1016/j.urology.2011.10.015
11. Farhat W, Bagli DJ, Capolicchio G, O’Reilly S, Merguerian PA, Khoury A, et al. The dysfunctional voiding scoring system: quantitative standardization of dysfunctional voiding symptoms in children. J Urol (2000) 164(3 Pt 2):1011–5. doi:10.1097/00005392-200009020-00023
12. Calado AA, Araújo EM, Barroso U Jr, Netto JM, Filho MZ, Macedo A Jr, et al. Cross-cultural adaption of the dysfunctional voiding score symptom (DVSS) questionnaire for Brazilian children. Int Braz J Urol (2010) 36:458–63.
13. Rasquin A, Di Lorenzo C, Forbes D, Guiraldes E, Hyams JS, Staiano A, et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology (2006) 130:1527–37. doi:10.1053/j.gastro.2005.08.063
14. Kajiwara M, Inoue K, Usui A, Kurihara M, Usui T. The micturition habits and prevalence of daytime urinary incontinence in Japanese primary school children. J Urol (2004) 171(1):403–7. doi:10.1097/01.ju.0000101907.87169.06
15. Sureshkumar P, Jones M, Cumming R, Craig J. A population based study of 2,856 school-age children with urinary incontinence. J Urol (2009) 181(2):808–15. doi:10.1016/j.juro.2008.10.044
16. Mugie SM, Benninga MA, Lorenzo CD. Epidemiology of constipation in children and adults: a systematic review. Best Pract Res Clin Gastroenterol (2011) 25(1):3–18. doi:10.1016/j.bpg.2010.12.010
17. de Araújo Sant’Anna AM, Calçado AC. Constipation in school-aged children at public schools in Rio de Janeiro, Brazil. J Pediatr Gastroenterol Nutr (1999) 29(2):190–3. doi:10.1097/00005176-199908000-00016
18. Chung JM, Lee SD, Kang DI, Kwon DD, Kim KS, Kim SY, et al. An epidemiologic study of voiding and bowel habits in Korean children: a nationwide multicenter study. Urology (2010) 76(1):215–9. doi:10.1016/j.urology.2009.12.022
19. Hadjizadeh N, Motamed F, Abdollahzade S, Rafiei S. Association of voiding dysfunction with functional constipation. Indian Pediatr (2009) 46:1093–5.
20. Bolat D, Acar IC, Zumrutbas AE, Eskicorapci S, Sancak EB, Zencir M, et al. Prevalence of daytime urinary incontinence and related risk factors in primary school children in Turkey. Korean J Urol (2014) 55(3):213–8. doi:10.4111/kju.2014.55.3.213
21. Rasquin-Weber A, Hyman PE, Cucchiara S, Fleischer DR, Hyams JS, Milla PJ, et al. Childhood functional gastrointestinal disorders. Gut (1999) 45:II60–8. doi:10.1136/gut.45.2008.ii60
22. Rajindrajith S, Devanarayana N, Adhikari C, Pannala W, Beninga MA. Constipation in children: an epidemiological study in Sri Lanka using Rome III criteria. Arch Dis Child (2012) 97:43–5. doi:10.1136/adc.2009.173716
23. Tam YH, Li AM, So HK, Shit KY, Pang KK, Wong YS, et al. Socioenviromental factors associated with constipation in Hon Kong children and Rome III criteria. J Pediatr Gastroenterol Nutr (2012) 55(1):56–61. doi:10.1097/MPG.0b013e31824741ce
24. Austin PF, Bauer S, Bower W, Chase J, Franco I, Hoebeke P, et al. The standardization of terminology of bladder function in children and adolescents: update report from the Standardization Committee of the International Children’s Continence Society (ICCS). J Urol (2014) 191(6):1863–65.e13. doi:10.1016/j.juro.2014.01.110
25. Clayden G, Wright A. Constipation and incontinence in childhood: two sides of the same coin? Arch Dis Child (2007) 92(6):472–4. doi:10.1136/adc.2007.115659
26. Charach G, Greenstein A, Rabinovich P, Groskopf I, Weintraub M. Alleviating constipation in the elderly improves lower urinary tract symptoms. Gerontology (2001) 47:72–6. doi:10.1159/000052776
27. Burgers R, Liem O, Canon S, Mousa H, Benninga MA, Di Lorenzo C, et al. Effect of rectal distention on lower urinary tract function in children. J Urol (2010) 184:1680–5. doi:10.1016/j.juro.2010.03.120
28. Loening-Baucke V. Urinary incontinence and urinary tract infection and their resolution with treatment of chronic constipation of childhood. Pediactrics (1997) 100(2):228–32.
29. Chase JW, Homsy Y, Siggaard C, Sit F, Bower WF. Functional constipation in children. J Urol (2004) 171(6 Pt 2):2641–3. doi:10.1097/01.ju.0000109743.12526.42
30. Benninga MA, Voskuijl WP, Taminiau JA. Childhood constipation: is there new light in the tunnel? J Pediatr Gastroenterol Nutr (2004) 39:448–64.
32. Franco I. Overactive bladder in children. Part 1: pathophysiology. J Urol (2007) 178(3):761–8. doi:10.1016/j.juro.2007.05.076
33. Leclair MD, Yves H. Non-neurogenic elimination disorders in children. J Pedriatr Urol (2010) 6:338–45. doi:10.1016/j.jpurol.2010.01.006
Keywords: constipation, incontinence, children, lower urinary tract dysfunction
Citation: Sampaio C, Sousa AS, Fraga LGA, Veiga ML, Bastos Netto JM and Barroso U Jr. (2016) Constipation and Lower Urinary Tract Dysfunction in Children and Adolescents: A Population-Based Study. Front. Pediatr. 4:101. doi: 10.3389/fped.2016.00101
Received: 13 June 2016; Accepted: 06 September 2016;
Published: 03 October 2016
Edited by:
Ricardo González, Auf der Bult Kinder- und Jugendkrankenhaus, GermanyReviewed by:
Maya Horst, University of Zurich, SwitzerlandMaría José Martínez-Urrutia, Children’s Hospital La Paz, Spain
Copyright: © 2016 Sampaio, Sousa, Fraga, Veiga, Bastos Netto and Barroso. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ubirajara Barroso Jr., ubarroso@uol.com.br
 Clara Sampaio
Clara Sampaio Ariane Sampaio Sousa
Ariane Sampaio Sousa Luis Gustavo A. Fraga
Luis Gustavo A. Fraga Maria Luiza Veiga1,2
Maria Luiza Veiga1,2
 Ubirajara Barroso Jr.
Ubirajara Barroso Jr.