Telehealth delivery of physical therapist-led interventions for persons with chronic low back pain in underserved communities: lessons from pragmatic clinical trials
- 1Department of Physical Therapy & Athletic Training, University of Utah, Salt Lake City, UT, United States
- 2Department of Orthopaedic Surgery, Duke University School of Medicine, Durham, NC, United States
- 3Duke Clinical Research Institute, Duke University School of Medicine, Durham, NC, United States
- 4Department of Population Health Sciences, Duke University School of Medicine, Durham, NC, United States
In this perspective, we present our experience developing and conducting two pragmatic clinical trials investigating physical therapist-led telehealth strategies for persons with chronic low back pain. Both trials, the BeatPain Utah and AIM-Back trials, are part of pragmatic clinical trial collaboratories and are being conducted with persons from communities that experience pain management disparities. Practice guidelines recommend nonpharmacologic care, and advise against opioid therapy, for the primary care management of persons with chronic low back pain. Gaps between these recommendations and actual practice patterns are pervasive, particularly for persons from racial or ethnic minoritized communities, those with fewer economic resources, and those living in rural areas including Veterans. Access barriers to evidence-based nonpharmacologic care, which is often provided by physical therapists, have contributed to these evidence-practice gaps. Telehealth delivery has created new opportunities to overcome access barriers for nonpharmacologic pain care. As a relatively new delivery mode however, telehealth delivery of physical therapy comes with additional challenges related to technology, intervention adaptations and cultural competence. The purpose of this article is to describe the challenges encountered when implementing telehealth physical therapy programs for persons with chronic low back pain in historically underserved communities. We also discuss strategies developed to overcome barriers in an effort to improve access to telehealth physical therapy and reduce pain management disparities. Inclusion of diverse and under-represented communities in pragmatic clinical trials is a critical consideration for improving disparities, but the unique circumstances present in these communities must be considered when developing implementation strategies.
Introduction
Chronic low back pain (cLBP) is among the most common reasons for healthcare visits (1, 2) and results in greater financial costs and loss of quality of life than any other chronic health condition (3, 4). The burden of cLBP falls disproportionately on persons in underserved communities. Persons with few socioeconomic resources, living in rural communities, who are Veterans, or part of racial/ethnic minoritized groups are at greater risk of experiencing chronic pain, especially chronic pain that results in substantial restriction of daily activities and the ability to work (5).
Disparities related to cLBP are evident in access to evidence-based care. Guidelines advocate first-line nonpharmacologic care emphasizing active coping strategies including physical activity, patient education, and exercise many of which are provided by physical therapists (PTs) (6). Guidelines advise against low-value services that promote passive coping including rest and opioid therapy (6–8). Practice patterns, however, reveal persistent evidence-practice gaps with over-utilization of opioids and underuse of nonpharmacologic therapy (9). Gaps are particularly notable for persons from racial or ethnic minoritized communities, those with fewer economic resources, living in rural areas and Veterans receiving care outside of large, urban Veteran's Administration (VA) facilities. Persons in these communities are less likely to receive nonpharmacologic interventions and are often more likely to receive opioids for cLBP (10–13).
Persistent evidence-practice gaps for persons with cLBP has motivated interest in pragmatic clinical trials (PCTs) to increase use of nonpharmacologic interventions. PCTs are designed to examine effectiveness of interventions under real-world circumstances (14). As such, PCTs should include diverse, heterogeneous patient populations that accentuate generalizability. Prior to COVID, PT-led telehealth delivery of nonpharmacologic interventions was discussed as a strategy to overcome access barriers, but was studied sparingly (15, 16). Research interest increased substantially with COVID (17). however, most studies have not included patients from communities that experience pain management disparities (18).
The authors of this paper are conducting PCTs examining PT-led telehealth interventions for persons with cLBP who are from communities that experience disparities. Our purpose is to describe the challenges experienced conducting PCTs evaluating PT-led telehealth interventions for persons with cLBP in underserved communities; and discuss strategies to overcome these challenges in order to reduce pain management disparities.
Pragmatic clinical trials being conducted in underserved communities
The authors are conducting two PCTs examining PT-led telehealth interventions in communities that experience disparities. The Improving Veteran Access to Integrated Management of Back Pain (AIM-Back) trial is examining two care pathways for LBP in multiple VA Medical Center sites (19). Veterans are more likely to experience chronic pain (20), and to be impacted by multiple chronic health conditions and psychological distress than non-Veterans (21, 22). Veterans who receive care in the VA Health System are more likely to live in rural communities, be from racial/ethnic minoritized communities, and have income below the federal poverty level relative to Veterans who receive care outside the VA (23, 24). The AIM-Back trial recruited VA sites that include smaller clinics without an existing relationship to an academic institution or a VA Center for Innovation site, resulting in 19 geographically-distinct clinics of which 10 are community-based clinics not connected to a larger VA facility. This approach enhanced the inclusion under-represented populations by engaging VA sites typically left out of clinical research.
BeatPain Utah is evaluating two strategies to provide telehealth PT for adults with cLBP who receive care in Community Health Centers (CHCs) in Utah (25). CHCs are federally-funded, non-profit organizations providing primary care in areas with high prevalence of medically underserved individuals (26). Nationally, about 1 in 12 Americans, including 1 in 5 residents of rural communities, receive primary care in a CHC, a majority of whom are members of racial/ethnic minoritized groups and have a household income below the federal poverty level (27, 28). The prevalence of chronic pain is 40%–60% among adult CHC patients (29, 30). In Utah, half of the state's 60 CHC clinics operate in rural or frontier counties, with 49% of patients served identifying their ethnicity as Hispanic/Latino, 39% best served in a language other than English, 45% are uninsured, and 59% have a household income below the federal poverty level (31).
Use of physical therapist-Led telehealth interventions in AIM-Back and BeatPain Utah PCTs
The goal of the AIM-Back trial is to compare the effectiveness of two pathways to improve access to nonpharmacologic pain care. One pathway uses a local pain navigator to assists veterans to navigate non-pharmacological care options within their VA system. The alternative pathway involves integrated sequenced care that provides an in-person PT visit followed by weekly telehealth sessions for 6 weeks; creating a hybrid approach. Telehealth sessions use two-way video or by phone and focus on physical activity counseling. After 6 weeks Veterans return to in-person PT and complete a risk stratification screening (32). Veterans at medium or high-risk for prolonged disability receive an additional 6 weeks of phone-based, telehealth PT including psychological and behavioral activation components such as pain coping skills and behavioral techniques.
The goal of the BeatPain trial is to compare the effectiveness of two strategies to provide telehealth PT using brief or extended delivery. Both strategies are completely remote with no in-person contact. The two strategies provide either 2 or 12 telehealth sessions in treatment phase I. At the conclusion of phase I all patients are evaluated. Those initially receiving 2 sessions are provided 10 additional sessions if they are determined to be non-responders to the initial 2 sessions. Those receiving 12 sessions do not receive additional treatment. Patients are referred to BeatPain PTs by primary care providers in participating CHCs using an electronic referral process. Telehealth sessions are provided in English or Spanish based on patient preference and use synchronous video or phone-based communication.
Both BeatPain and AIM-Back deliver care to patients in underserved communities typically omitted from clinical trials. Both studies are using telehealth to provide PT care that involves physical activity, exercise, education and psychologically-informed strategies. Both studies gathered input from community members and have learned lessons as the trials proceeded. We grouped issues encountered into four areas to characterize challenges encountered in providing PT-led telehealth interventions. These issues are outlined in Table 1 and described below.
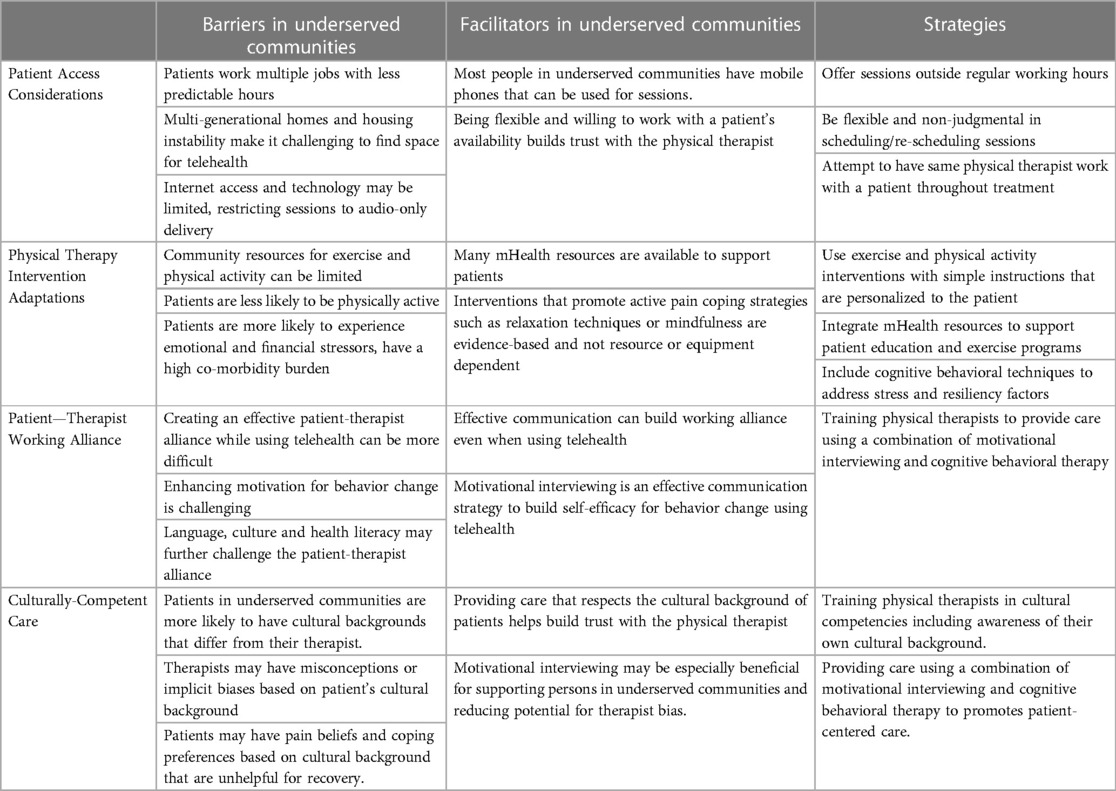
Table 1. Overview of barriers and facilitators encountered in the development and implementation of physical therapist-led telehealth interventions and the strategies used to deliver telehealth interventions in the BeatPain and AIM-Back pragmatic clinical trials.
Patient access considerations
Telehealth overcomes barriers related to geographic proximity and transportation, but does not eliminate other access barriers contributing to disparities. Persons in underserved communities are more likely to have multiple persons living in the same household, experience housing instability, and are more likely to hold multiple jobs with irregular work hours (33); creating challenges in finding time and space for telehealth sessions. The ability to offer services outside traditional working hours and scheduling flexibility can be essential for telehealth access. If other people are present it is important to ask and document the patient's approval for another person to be present.
The digital divide, which relates to digital literacy and availability of technology for telehealth (34), can pose additional access barriers. Adults in rural and racial/ethnic minoritized communities are less likely to own a tablet or traditional computer (35). Access to broadband internet is a barrier in rural communities, where about a quarter of residents find high speed internet access a major problem, a figure that increases to 31% for non-white residents in rural communities (35). Low digital literacy impacts access when persons lack experience setting up web cameras, accessing software, downloading apps (36), and the overall cognitive load of learning new tasks with unfamiliar technologies (37). Collectively these factors make it more likely that persons in underserved communities will rely on their phone for audio-only telehealth instead of 2-way video communication (38). While audio-only telehealth was common during COVID, using the phone instead of video communication has been associated with lower patient satisfaction (39), and may be particularly challenging for providing PT interventions.
In the BeatPain study we addressed access by ensuring PTs are available during early evening and morning hours. We adopted a flexible work schedule for PTs and hired people available at different times. The PT training emphasizes the need for flexibility, recognizing that participants' time limitations may require shorter sessions. Sessions may need to be rescheduled with short notice so PTs keep times open during the week to permit timely rescheduling. It is important that these circumstances be accommodated in a patient-centered, non-judgmental manner. Every effort is made to have the same PT provide care for a BeatPain participant throughout the study as provider consistency can help reduce missed appointments (40).
The AIM-Back study facilitated access by taking advantage of resources available through the VA health system; a leader in expanding telehealth access. Veterans and providers can use VA Video Connect, a secure videoconferencing app, for telehealth sessions on a smartphone, tablet, or computer. However, approximately 15% of Veterans do not have internet access (41), and many, including rural or low income Veterans, lack access to necessary technology or connectivity. As such, AIM-Back telehealth providers educate Veterans on possible services offered by the VA to improve telehealth access including Digital Divide Consults that help Veterans obtain services necessary for telehealth, including lending internet-connected tablets and eliminating data charges for Veterans using the VA Video Connect app. Accessing Telehealth through Local Area Stations (ATLAS) provides Veterans with private space in their local community to use for video appointments (42).
Physical therapy intervention adaptation
Exercise is an evidence-based strategy for persons with cLBP and a core component of PT practice (43). Persons in underserved communities are less likely to have access to spaces conducive to physical activity, and are less likely to be physically active (44–46). Veterans and persons in rural communities are more likely to have co-morbidities including mental health conditions, diabetes, and obesity that can pose additional challenges for exercise (46–48). These factors must be considered in developing PT-led telehealth interventions. Additionally, emotional and financial stressors are risk factors for high impact cLBP and are prevalent among Veterans and persons in low income communities (49, 50). Addressing these stressors through coping strategies such as relaxation techniques, sleep quality, mindfulness and countering negative cognitions around pain may be less familiar to PTs (51), but these techniques can be effective in offsetting the impact of cLBP on daily life (52), can be effectively delivered by PTs (53, 54), and are amenable to telehealth delivery.
The BeatPain and AIM-Back studies considered these factors when developing their telehealth PT protocols. Emphasis is placed in both studies on simple exercise activities such as walking that can be explained to participants even when care is audio-only. Exercise programs are supplemented with Mobile Health (mHealth) applications for asynchronous instruction including videos or written performance descriptions. BeatPain uses Medbridge (Medbridge, Inc., Bellevue, WA) to create personalized programs that include videos, audio, handouts and pictures that patients can access asynchronously through a mobile app, or emailed or texted to a patient. AIM-Back provides Veterans with informational packets that include all prescribed exercises with picture demonstrations and detailed text describing technique, frequency, and intensity. Materials for the psychologically-informed components include education materials on behavioral interventions and handouts to increase engagement from Veterans and encourage active participation in treatment. These materials are also made available digitally, through the MyHealtheVet portal or email. Both AIM-Back and BeatPain PT integrate cognitive and behavioral strategies that focus on reducing maladaptive cognitions about pain including kinesiophobia and catastrophizing that may reduce engagement in physical activity (55). Strategies to reduce these cognitions include education, reframing, goal setting and graded exposure, problem-solving, activity pacing and relaxation techniques (e.g., visualization, mindfulness, pain journaling, etc.). These strategies were also supported by supplemental print materials and videos available to participants.
Patient—therapist working alliance
The working alliance, or therapeutic bond, between patient and PT is an integral component of engagement and behavioral change, and predicts outcomes of in-person PT care (56, 57). Developing an effective working alliance can be challenging when care is provided using telehealth as patient surveys suggest the care may be perceived as less personal (58, 59), particularly with audio-only delivery (60). Surveys of PTs providing telehealth highlight concerns about developing rapport without the ability to touch, or perhaps see, their patient (61). Concepts contributing to effective patient-PT working alliances include attention to the patient's needs, understanding their narrative through active listening, providing a safe therapeutic space for patients to set meaningful goals and build autonomy (60, 62). These concepts can be effectively developed using telehealth, but likely require additional skills for PTs whose experience has primarily involved in-person delivery.
In BeatPain, PTs are trained to integrate motivation and problem-solving (MAPS). MAPS is an approach to enhance patients' intrinsic motivation for behavior change that combines motivational interviewing (MI) and cognitive behavioral practices (63), that has been found effective for engaging patients in behavior changes for smoking cessation and substance use (64–66). MAPs was considered apposite for BeatPain because it uses MI, a patient-centered communication strategy that facilitates active listening and is well-suited to audio-only delivery (67, 68). Problem-solving techniques used with MAPS are intended to enhance intrinsic motivation for change by guiding patients to develop personalized goals and build self-efficacy; an important factor for limiting the functional impact of LBP (69). MAPS emphasizes expressions of empathy for PTs through active, nonjudgmental listening about the patient's perspective and goals (65). Expressing empathy in the context of telehealth can be challenging, but is important for developing an effective patient-PT working alliance (70, 71). Additional efforts to enhance empathy included minimizing distractions and background noise during sessions and encouraging picture-in-picture functions during video telehealth sessions when possible to allow eye contact.
Similar strategies were used in the AIM-Back study. Telehealth providers had flexibility in scheduling sessions and determining call durations which helped establish rapport and allowed Veterans to share their pain-related narratives without time constraints. This arrangement facilitated a more comprehensive and nuanced understanding of the Veterans’ experiences, fostering a stronger patient-PT working alliance. AIM-Back telehealth providers were also trained to use MI in their interactions with Veterans. Through the use of MI techniques emphasizing open-ended questions, affirmations, reflections, and summarizations, Veterans were guided in defining and evaluating personalized, values-based goals over the course of care. This approach was used to foster Veterans' intrinsic motivation to actively engage with home-based exercise and pain coping programs, potentially enhancing adherence.
Culturally-competent care
Culture, which includes shared beliefs and behaviors, communication styles, views of roles and relationships, values, and traditions (72); impacts a person's pain experience (73). Culturally competent care effectively provides services that meet the social, cultural, and linguistic needs of patients (74), and is essential for reducing health disparities (75). Cultural competence applies to racial/ethnic minoritized communities and other communities that experience disparities including persons from low income, rural and Veteran communities (75). Culturally competent care is not achieved by merely having providers with similar backgrounds as their patients. Providers need to be aware of their own cultural perspective because ineffective communication, stereotyping or biased care can arise when cultural differences between patient and provider are unrecognized (76).
With respect to cLBP, cultural factors can impact when and how an individual chooses to seek care, their beliefs about the likely cause of pain, locus of control, self-efficacy, preferred coping strategies and receptivity to particular interventions (77, 78). For example, a core component of evidence-based PT for cLBP is helping patients adopt active coping for self-management, but some cultural perspectives may favor more passive strategies (e.g., rest, prayer, etc.) (79). Cultural considerations can also impact patients' trust in healthcare, their willingness to participate in PT, or enroll in clinical research studies (80). Helping potential participants understand clinical research and develop strong interpersonal connections with a PT may be especially important to build trust with persons in underserved communities (81). In the BeatPain study, participants considering enrollment have the opportunity to consult the study's web page or connect with a PT who can answer additional questions about participation.
Many BeatPain participants are persons of Hispanic/Latino ethnicity. Persons of Hispanic ethnicity living in the U.S represent an array of cultural sub-groups based on region of origin, degree of acculturation, socioeconomic status and other factors (82). Some similarities among persons of Hispanic ethnicity have been identified (83–85), and tend to be reflected in patients participating in the BeatPain study. These include approaching chronic pain with greater stoicism and a focus on continuing in social roles, particularly familial roles. BeatPain also serves people in rural communities who are more likely to use passive pain coping strategies such as heat/cold application, medication, etc. (12). Integrating MAPS and MI into BeatPain protocols has facilitated the delivery of culturally competent PT care. This may reflect MI's emphasis on open questions and reflective summaries that communicate respect for the patient's perspective on the causes and consequences of pain. The non-judgmental, patient-centered MI approach may reduce risks of misconceptions or implicit bias on the part of PTs (86). The goal-setting and problem-solving aspect of MAPS helps PTs center on activities of importance to the patient such as familial responsibilities. BeatPain PTs receive additional training in culturally competent care to help them examine their own cultural background and understand how it may interact with their patient's background to impact care (87), and to help PTs consider major cultural issues they may encounter (88). Initial training includes about 2 h for cultural competence and 10 h for MAPS. Ongoing training involves weekly meetings to discuss cases and quarterly peer-practice sessions.
The AIM-Back study serves Veterans, a community with unique experiences and a distinct culture that encompasses persons whose cultural background is further informed by gender, race, ethnicity etc. (24). During the design phase of AIM-Back, a partner engagement process with the Veteran community was incorporated to provide opportunities for patients, caregivers, clinicians, and administrative leaders to voice their views on the planning, implementation, and evaluation of the proposed care pathways. Attention was paid to gaining diverse input based on Veterans' race/ethnicity, gender and deployment experiences (89).
Discussion
Although cLBP disproportionately impacts persons in minoritized, low income, Veteran and rural communities, clinical trials historically focus recruitment on urban, academic medical centers serving persons with greater economic resources and less diversity (90). Inclusion of patients from underserved communities is critical for all research, particularly for PCTs that recruit participants as part of routine care. Thus, PCTs risk reproducing and reinforcing disparities if they focus on urban, academic healthcare systems and fail to make intentional efforts to include persons from communities that experience disparities (91, 92).
Access to evidence-based, nonpharmacologic care is a likely contributor to pain prevalence and outcome disparities. Telehealth is an attractive strategy to mitigate access barriers in communities where nonpharmacologic providers are often unavailable. Data emerging from the COVID pandemic, however, raise concerns that the communities with the greatest need for improved access may not realize the benefits of telehealth without intentional efforts. Several studies suggest that persons from racial/ethnic minorized and/or rural communities, and those with lower income may be less likely to use telehealth (93–96).
Communities that experience disparities have been referred to as “evidence vacuums” because they are generally omitted from clinical research (92). Interventions found effective in urban, academic settings cannot be presumed effective for persons in underserved communities. Although clinical trials support equivalence between telehealth and in-person PT (97), these trials have not focused on patients in underserved communities (92). Emphasis on telehealth as a strategy to overcome disparities could paradoxically have the opposite effect if the challenges for providing care to persons in underserved communities are not reflected in research (98). This concern motivated the BeatPain and AIM-Back studies to partner with CHCs and mostly non-academic VA facilities respectively. This paper describes the important step of tailoring the PT interventions to meet the unique needs of patients served in these settings. While these PCTs are ongoing, we believe our experiences can inform future efforts to use telehealth to make effective nonpharmacologic pain care accessible for persons with cLBP in underserved communities.
Conclusion
In order to address disparities in health and health care, pragmatic clinical trials should include patients in communities that are historically under-represented in research. Inclusion of settings and participants who are familiar with pragmatic research requires careful attention to unique challenges when developing interventions and implementation strategies.
Data availability statement
The original contributions presented in the study are included in the article/supplementary Materials, further inquiries can be directed to the corresponding author.
Author contributions
JF: Conceptualization, Funding acquisition, Supervision, Writing – original draft, Writing – review & editing. IF: Conceptualization, Writing – original draft, Writing – review & editing. SG: Supervision, Writing – review & editing. LV: Writing – original draft, Writing – review & editing. TC: Writing – review & editing. CB: Writing – review & editing. AG: Conceptualization, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article.
This work is supported through cooperative agreements UH3-AT009790 from the National Center for Complementary and Integrative Health (NCCIH) and UH3-NR019943 from the National Institute of Nursing Research (NINR) and the National Institutes of Health (NIH). This work also received logistical and technical support from the PRISM Resource Coordinating Centre under award number U24AT010961 from the NIH through the NIH HEAL Initiative.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Finley CR, Chan DS, Garrison S, Korownyk C, Kolber MR, Campbell S, et al. What are the most common conditions in primary care? Can Fam Phys. (2018) 64:832–40. 30429181.
3. Dieleman JL, Cao J, Chapin A, Chen C, Li Z, Liu A, et al. US Health care spending by payer and health condition, 1996–2016. JAMA. (2020) 323:863–84. doi: 10.1001/jama.2020.0734
4. Vos T, Allen C, Arora M, Collaborators GDaIIaP. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet. (2017) 390:1211–59. doi: 10.1016/S0140-6736(17)32154-2
5. Pitcher MH, Von Korff M, Bushnell MC, Porter L. Prevalence and profile of high-impact chronic pain in the United States. J Pain. (2019) 20:146–60. doi: 10.1016/j.jpain.2018.07.006
6. Skelly AC, Chou R, Dettori JR, Turner JA, Friedly JL, Rundell SD, et al. Noninvasive Nonpharmacological Treatment for Chronic Pain: A Systematic Review. Comparative Effectiveness Review No. 209. (Prepared by the Pacific Northwest Evidence-based Practice Center under Contract No. 290-2015-00009-I.) AHRQ Publication No 18-EHC013-EF. Rockville, MD: Agency for Healthcare Research and Quality (2018).
7. Rosenberg JM, Bilka BM, Wilson SM, Spevak C. Opioid therapy for chronic pain: overview of the 2017 US department of veterans affairs and US department of defense clinical practice guideline. Pain Med. (2018) 19:928–41. doi: 10.1093/pm/pnx203
8. Pangarkar SS, Kang DG, Sandbrink F, Bevevino A, Tillisch K, Konitzer L, et al. VA/Dod clinical practice guideline: diagnosis and treatment of low back pain. J Gen Intern Med. (2019) 34:2620–9. doi: 10.1007/s11606-019-05086-4
9. Kamper SJ, Logan G, Copsey B, Thompson J, Machado GC, Abdel-Shaheed C, et al. What is usual care for low back pain? A systematic review of health care provided to patients with low back pain in family practice and emergency departments. Pain. (2020) 161:694–702. doi: 10.1097/j.pain.0000000000001751
10. Atkins N, Mukhida K. The relationship between patients’ income and education and their access to pharmacological chronic pain management: a scoping review. Can J Pain. (2022) 6:142–70. doi: 10.1080/24740527.2022.2104699
11. Mannes ZL, Stohl M, Fink DS, Olfson M, Keyes KM, Martins SS, et al. Non-pharmacological treatment for chronic pain in US veterans treated within the veterans health administration: implications for expansion in US healthcare systems. J Gen Intern Med. (2022) 37:3937–46. doi: 10.1007/s11606-021-07370-8
12. Eaton LH, Langford DJ, Meins AR, Rue T, Tauben DJ, Doorenbos AZ. Use of self-management interventions for chronic pain management: a comparison between rural and nonrural residents. Pain Manag Nurs. (2018) 19:8–13. doi: 10.1016/j.pmn.2017.09.004
13. Turner BJ, Rodriguez N, Valerio MA, Liang Y, Winkler P, Jackson L. Less exercise and more drugs: how a low-income population manages chronic pain. Arch Phys Med Rehabil. (2017) 98:2111–7. doi: 10.1016/j.apmr.2017.02.016
14. Rowbotham MC, Gilron I, Glazer C, Rice ASC, Smith BH, Stewart WF, et al. Can pragmatic trials help us better understand chronic pain and improve treatment? Pain. (2013) 154:643–6. doi: 10.1016/j.pain.2013.02.034
15. Cottrell MA, Galea OA, O'Leary SP, Hill AJ, Russell TG. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clinical Rehabil. (2017) 31:625–38. doi: 10.1177/0269215516645148
16. Salisbury C, Montgomery AA, Hollinghurst S, Hopper C, Bishop A, Franchini A, et al. Effectiveness of PhysioDirect telephone assessment and advice services for patients with musculoskeletal problems: pragmatic randomised controlled trial. Br Med J. (2013) 346:f43. doi: 10.1136/bmj.f43
17. Hohenschurz-Schmidt D, Kleykamp BA, Draper-Rodi J, Vollert J, Chan J, Ferguson M, et al. Pragmatic trials of pain therapies: a systematic review of methods. Pain. (2022) 163:21–46. doi: 10.1097/j.pain.0000000000002317
18. Brandt HM, Young VM, Campbell DA, Choi SK, Seel JS, Friedman DB. Federally qualified health Centers’ capacity and readiness for research collaborations: implications for clinical-academic-community partnerships. Clin Transl Sci. (2015) 8:391–3. doi: 10.1111/cts.12272
19. George SZ, Coffman CJ, Allen KD, Lentz TA, Choate A, Goode AP, et al. Improving veteran access to integrated management of back pain (AIM-back): protocol for an embedded pragmatic cluster-randomized trial. Pain Med. (2020) 21:S62–s72. doi: 10.1093/pm/pnaa348
20. Nahin RL. Severe pain in veterans: the effect of age and sex, and comparisons with the general population. J Pain. (2017) 18:247–54. doi: 10.1016/j.jpain.2016.10.021
21. Kramarow EA, Pastor PN. The health of male veterans and nonveterans aged 25–64: united States, 2007–2010. NCHS Data Brief. (2012) 101:1–8. 23101789.
22. Bloeser K, Lipkowitz-Eaton J. Disproportionate multimorbidity among veterans in middle age. J Public Health. (2022) 44:28–35. doi: 10.1093/pubmed/fdab149
23. Meffert BN, Morabito DM, Sawicki DA, Hausman C, Southwick SM, Pietrzak RH, et al. US Veterans who do and do not utilize veterans affairs health care services: demographic, military, medical, and psychosocial characteristics. Prim Care Companion CNS Disord. (2019) 21:18m02350. doi: 10.4088/PCC.18m02350
24. McClendon J, Essien UR, Youk A, Ibrahim SA, Vina E, Kwoh CK, et al. Cumulative disadvantage and disparities in depression and pain among veterans with osteoarthritis: the role of perceived discrimination. Arthritis Care Res. (2021) 73:11–7. doi: 10.1002/acr.24481
25. Fritz JM, Del Fiol G, Gibson B, Wetter DW, Solis V, Bennett E, et al. Beatpain Utah: study protocol for a pragmatic randomised trial examining telehealth strategies to provide non-pharmacologic pain care for persons with chronic low back pain receiving care in federally qualified health centers. BMJ Open. (2022) 12:e067732. doi: 10.1136/bmjopen-2022-067732
26. Rural Health Information Hub. Federally Qualified Health Centers (FQHCs) and the Health Center Program. Federally Qualified Health Centers (FQHCs) and the Health Center Program Overview—Rural Health Information Hub. (Updated 2021). (accessed August 31, 2023).
27. Health Resources and Service Administration. National Health Center Program Uniform Data System (UDS) Awardee Data, National Health Center Program Uniform Data System (UDS) Awardee Data (hrsa.gov), (Updated 2021). (accessed August 10, 2023).
28. Chang CH, Bynum JPW, Lurie JD. Geographic expansion of federally qualified health centers 2007–2014. J Rural Health. (2019) 35:385–94. doi: 10.1111/jrh.12330
29. Anderson D, Wang S, Zlateva I. Comprehensive assessment of chronic pain management in primary care: a first phase of a quality improvement initiative at a multisite community health center. Qual Prim Care. (2012) 20:421–33. 23540822.23540822
30. Smith LJ, Johnson-Lawrence V, Andrews M, Parker S. Opportunity for interprofessional collaborative care—findings from a sample of federally qualified health center patients in the midwest. Public Health. (2017) 151:131–6. doi: 10.1016/j.puhe.2017.07.009
31. Association for Utah Community Health. Utah Community Health Centers 2021/2022 Overview. Available online at: https://auch.org/2022overview (accessed September 10, 2023).
32. Hill JC, Dunn KM, Lewis M, Mullis R, Main CJ, Foster NE, et al. A primary care back pain screening tool: identifying patient subgroups for initial treatment. Arthritis Rheum. (2008) 59:632–41. doi: 10.1002/art.23563
33. Bailey KA, Spletzer JR. A new measure of multiple jobholding in the U.S. Economy. In: Goertz C, editors. Washington, D.C.: U.S. Census Bureau Center for Economic Studies (2020). p. 1–3.
34. Price-Haywood EG, Arnold C, Harden-Barrios J, Davis T. Stop the divide: facilitators and barriers to uptake of digital health interventions among socially disadvantaged populations. Ochsner J. (2023) 23:34–42. doi: 10.31486/toj.22.0101
35. Pew Research Center. Digital Divide. Available online at: https://www.pewresearch.org/topic/internet-technology/technology-policy-issues/digital-divide/ (2021). (accessed September 8, 2023).
36. Alkureishi MA, Choo ZY, Rahman A, Ho K, Benning-Shorb J, Lenti G, et al. Digitally disconnected: qualitative study of patient perspectives on the digital divide and potential solutions. JMIR Hum Factors. (2021) 8:e33364. doi: 10.2196/33364
37. Antonio MG, Williamson A, Kameswaran V, Beals A, Ankrah E, Goulet S, et al. Targeting patients’ cognitive load for telehealth video visits through student-delivered helping sessions at a United States federally qualified health center: equity-focused, mixed methods pilot intervention study. J Med Internet Res. (2023) 25:e42586. doi: 10.2196/42586
38. Eberly LA, Kallan MJ, Julien HM, Haynes N, Khatana SAM, Nathan AS, et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. (2020) 3:e2031640. doi: 10.1001/jamanetworkopen.2020.31640
39. Chen K, Lodaria K, Jackson HB. Patient satisfaction with telehealth vs. in-person visits during COVID-19 at a large, public healthcare system. J Eval Clin Pract. (2022) 28:986–90. doi: 10.1111/jep.13770
40. Ruggeri K, Folke T, Benzerga A, Verra S, Büttner C, Steinbeck V, et al. Nudging New York: adaptive models and the limits of behavioral interventions to reduce no-shows and health inequalities. BMC Health Serv Res. (2020) 20:363. doi: 10.1186/s12913-020-05097-6
41. O’Shea AMJ, Baum A, Haraldsson B, Shahnazi A, Augustine MR, Mulligan K, et al. Association of adequacy of broadband internet service with access to primary care in the veterans health administration before and during the COVID-19 pandemic. JAMA Network Open. (2022) 5:e2236524–e2236524. doi: 10.1001/jamanetworkopen.2022.36524
42. U.S. Department of Veterans Affairs. Briding the Digital Divide. Available online at: https://telehealth.va.gov/digital-divide (accessed September 8, 2023).
43. George SZ, Fritz JM, Silfies SP, Schneider MJ, Beneciuk JM, Lentz TA, et al. Interventions for the management of acute and chronic low back pain: revision 2021. J Orthop Sports Phys Ther. (2021) 51:Cpg1–cpg60. doi: 10.2519/jospt.2021.0304
44. D'Alonzo KT, Saimbert MK. Hispanic women and physical activity: an integrative review. Annu Rev Nurs Res. (2013) 31:209–34. doi: 10.1891/0739-6686.31.209
45. Murillo R, Reesor LM, Hernandez DC, Obasi EM. Neighborhood walkability and aerobic physical activity among latinos. Am J Health Behav. (2019) 43:802–11. doi: 10.5993/AJHB.43.4.13
46. Okobi OE, Ajayi OO, Okobi TJ, Anaya IC, Fasehun OO, Diala CS, et al. The burden of obesity in the rural adult population of America. Cureus. (2021) 13:e15770. doi: 10.7759/cureus.15770
47. Early NK, Buckley K, Entsuah N, Fairman KA. Association of cardiovascular disease and military veteran status with impairments in physical and psychological functioning: retrospective cross-sectional analysis of US national survey data. J Cardiovasc Pharmacol Ther. (2022) 27:10742484221091015. doi: 10.1177/10742484221091015
48. Rubio JM, Markowitz JC, Alegría A, Pérez-Fuentes G, Liu SM, Lin KH, et al. Epidemiology of chronic and nonchronic major depressive disorder: results from the national epidemiologic survey on alcohol and related conditions. Depress Anxiety. (2011) 28:622–31. doi: 10.1002/da.20864
49. Baria AM, Pangarkar S, Abrams G, Miaskowski C. Adaption of the biopsychosocial model of chronic noncancer pain in veterans. Pain Med. (2019) 20:14–27. doi: 10.1093/pm/pny058
50. Weissman JD, Russell D, Taylor J. The relationship between financial stressors, chronic pain, and high-impact chronic pain: findings from the 2019 national health interview survey. Public Health Rep. (2023) 138(3):438–46. doi: 10.1177/00333549221091786
51. Foster NE, Delitto A. Embedding psychosocial perspectives within clinical management of low back pain: integration of psychosocially informed management principles into physical therapist practice--challenges and opportunities. Phys Ther. (2011) 91:790–803. doi: 10.2522/ptj.20100326
52. Roberts KE, Beckenkamp PR, Ferreira ML, Duncan GE, Calais-Ferreira L, Gatt JM, et al. Positive lifestyle behaviours and emotional health factors are associated with low back pain resilience. Eur Spine J. (2022) 31:3616–26. doi: 10.1007/s00586-022-07404-7
53. Archer KR, Devin CJ, Vanston SW, Koyama T, Phillips SE, George SZ, et al. Cognitive-behavioral-based physical therapy for patients with chronic pain undergoing lumbar spine surgery: a randomized controlled trial. J Pain. (2016) 17:76–89. doi: 10.1016/j.jpain.2015.09.013
54. Bryant C, Lewis P, Bennell KL, Ahamed Y, Crough D, Jull GA, et al. Can physical therapists deliver a pain coping skills program? An examination of training processes and outcomes. Phys Ther. (2014) 94:1443–54. doi: 10.2522/ptj.20130444
55. Marshall PWM, Schabrun S, Knox MF. Physical activity and the mediating effect of fear, depression, anxiety, and catastrophizing on pain related disability in people with chronic low back pain. PLoS One. (2017) 12:e0180788. doi: 10.1371/journal.pone.0180788
56. Flückiger C, Del Re AC, Wampold BE, Horvath AO. The alliance in adult psychotherapy: a meta-analytic synthesis. Psychother. (2018) 55:316–40. doi: 10.1037/pst0000172
57. Alodaibi F, Beneciuk J, Holmes R, Kareha S, Hayes D, Fritz J. The relationship of therapeutic alliance to patient characteristics and functional outcome during an episode of physical therapy care for patients with low back pain: an observational study. Phys Ther. (2021) 101:pzab026. doi: 10.1093/ptj/pzab026
58. Fritz JM, Minick KI, Brennan G, McGee T, Lane E, Skolasky RL, et al. Outcomes of telehealth physical therapy provided using real-time, videoconferencing for patients with chronic low back pain: a longitudinal observational study. Arch Phys Med Rehabil. (2022) 103:1924–34. doi: 10.1016/j.apmr.2022.04.016
59. Skolasky RL, Kimball ER, Galyean P, Minick KI, Brennan G, McGee T, et al. Identifying perceptions, experiences, and recommendations of telehealth physical therapy for patients with chronic low back pain: a mixed methods survey. Arch Phys Med Rehabil. (2022) 103:1935–43. doi: 10.1016/j.apmr.2022.06.006
60. Wallace LM, Falla D, Rushton A, Heneghan NR. Group and individual telehealth for chronic musculoskeletal pain: a scoping review. Musculoskel Care. (2022) 20:245–58. doi: 10.1002/msc.1594
61. Lawford BJ, Delany C, Bennell KL, Hinman RS. "I was really pleasantly surprised": firsthand experience and shifts in physical therapist perceptions of telephone-delivered exercise therapy for knee osteoarthritis-a qualitative study. Arthritis Care Res. (2019) 71:545–57. doi: 10.1002/acr.23618
62. Søndenå P, Dalusio-King G, Hebron C. Conceptualisation of the therapeutic alliance in physiotherapy: is it adequate? Musculoskelet Sci Pract. (2020) 46:102131. doi: 10.1016/j.msksp.2020.102131
63. McClure J, Westbrook E, Curry S, Wetter D. Proactive, motivationally enhanced smoking cessation counseling among women with elevated cervical cancer risk. Nicotine Tob Res. (2005) 7:881–9. doi: 10.1080/14622200500266080
64. Correa-Fernández V, Díaz-Toro EC, Reitzel LR, Guo L, Chen M, Li Y, et al. Combined treatment for at-risk drinking and smoking cessation among Puerto Ricans: a randomized clinical trial. Addict Behav. (2017) 65:185–92. doi: 10.1016/j.addbeh.2016.10.009
65. Vidrine JI, Reitzel LR, Figueroa PY, Velasquez MM, Mazas CA, Cinciripini PM, et al. Motivation and problem solving (MAPS): motivationally based skills training for treating substance use. Cogn Behav Pract. (2013) 20:501–16. doi: 10.1016/j.cbpra.2011.11.001
66. Vinci C, Lam C, Schlechter CR, Shono Y, Vidrine JI, Wetter DW. Increasing treatment enrollment among smokers who are not motivated to quit: a randomized clinical trial. Trans Behavior Med. (2022) 12:ibab114. doi: 10.1093/tbm/ibab114
67. Jiang S, Wu L, Gao X. Beyond face-to-face individual counseling: a systematic review on alternative modes of motivational interviewing in substance abuse treatment and prevention. Addict Behav. (2017) 73:216–35. doi: 10.1016/j.addbeh.2017.05.023
68. Patel ML, Wakayama LN, Bass MB, Breland JY. Motivational interviewing in eHealth and telehealth interventions for weight loss: a systematic review. Prev Med. (2019) 126:105738. doi: 10.1016/j.ypmed.2019.05.026
69. Puschmann AK, Drießlein D, Beck H, Arampatzis A, Moreno Catalá M, Schiltenwolf M, et al. Stress and self-efficacy as long-term predictors for chronic low back pain: a prospective longitudinal study. J Pain Res. (2020) 13:613–21. doi: 10.2147/JPR.S223893
70. Unsgaard-Tøndel M, Søderstrøm S. Building therapeutic alliances with patients in treatment for low back pain: a focus group study. Physiother Res Int. (2022) 27:e1932. doi: 10.1002/pri.1932
71. Duffy LV, Evans R, Bennett V, Hady JM, Palaniappan P. Therapeutic relational connection in telehealth: concept analysis. J Med Internet Res. (2023) 25:e43303. doi: 10.2196/43303
72. Carrillo JE, Green AR, Betancourt JR. Cross-cultural primary care: a patient-based approach. Ann Intern Med. (1999) 130:829–34. doi: 10.7326/0003-4819-130-10-199905180-00017
73. Reis FJJ, Nijs J, Parker R, Sharma S, Wideman TH. Culture and musculoskeletal pain: strategies, challenges, and future directions to develop culturally sensitive physical therapy care. Braz J Phys Ther. (2022) 26:100442. doi: 10.1016/j.bjpt.2022.100442
74. Betancourt JR, Green AR, Carrillo JE. Cultural Competence in Health Care: Emerging Frameworks and Practical Approaches. New York, NY: The Commonwealth Fund (2002).
75. Butler M, McCreedy E, Schwer N, Burgess D, Call K, Przedworski J, et al. AHRQ Comparative Effectiveness Reviews, Improving Cultural Competence to Reduce Health Disparities. Rockville (MD): Agency for Healthcare Research and Quality (US) (2016).
76. Betancourt JR. Cross cultural medical education: conceptual approaches and frameworks for evaluation. Acad Med. (2003) 78:560–9. doi: 10.1097/00001888-200306000-00004
77. Orhan C, Van Looveren E, Cagnie B, Mukhtar NB, Lenoir D, Meeus M. Are pain beliefs, cognitions, and behaviors influenced by race, ethnicity, and culture in patients with chronic musculoskeletal pain: a systematic review. Pain Physician. (2018) 21:541–58. 30508984.30508984
78. Sharma S, Ferreira-Valente A, Abbott JH, Pais-Ribeiro J, Jensen MP. Group differences between countries and between languages in pain-related beliefs, coping, and catastrophizing in chronic pain: a systematic review. Pain Med. (2020) 21:1847–62. doi: 10.1093/pm/pnz373
79. Meints SM, Cortes A, Morais CA, Edwards RR. Racial and ethnic differences in the experience and treatment of noncancer pain. Pain Manag. (2019) 9:317–34. doi: 10.2217/pmt-2018-0030
80. Letzen JE, Mathur VA, Janevic MR, Burton MD, Hood AM, Morais CA, et al. Confronting racism in all forms of pain research: reframing study designs. J Pain. (2022) 23:893–912. doi: 10.1016/j.jpain.2022.01.010
81. Joyce C, Keysor J, Stevans J, Ready K, Roseen EJ, Saper RB. Beyond the pain: a qualitative study exploring the physical therapy experience in patients with chronic low back pain. Physiother Theory Pract. (2023) 39:803–13. doi: 10.1080/09593985.2022.2029650
82. Nahin RL, Pain prevalence, chronicity and impact within subpopulations based on both hispanic ancestry and race: United States, 2010–2017. J Pain. (2021) 22: 826–51. doi: 10.1016/j.jpain.2021.02.006
83. Campbell LC, Andrews N, Scipio C, Flores B, Feliu MH, Keefe FJ. Pain coping in latino populations. J Pain. (2009) 10:1012–9. doi: 10.1016/j.jpain.2009.03.004
84. Chou L, Ranger TA, Peiris W, Cicuttini FM, Urquhart DM, Sullivan K, et al. Patients’ perceived needs for medical services for non-specific low back pain: a systematic scoping review. PLoS One. (2018) 13:e0204885. doi: 10.1371/journal.pone.0204885
85. Hollingshead NA, Ashburn-Nardo L, Stewart JC, Hirsh AT. The pain experience of hispanic Americans: a critical literature review and conceptual model. J Pain. (2016) 17:513–28. doi: 10.1016/j.jpain.2015.10.022
86. Anastas TM, Miller MM, Hollingshead NA, Stewart JC, Rand KL, Hirsh AT. The unique and interactive effects of patient race, patient socioeconomic status, and provider attitudes on chronic pain care decisions. Ann Behav Med. (2020) 54:771–82. doi: 10.1093/abm/kaaa016
87. Hays PA. Addressing Cultural Complexities in Practice: A Framework for Clinicians and Counselors. Washington, DC: American Psychological Association (2001).
88. Betancourt JR, Green AR, Carrillo JE. The Patient’s Culture and Effective Communication, (2021).
89. Ballengee LA, King HA, Simon C, Lentz TA, Allen KD, Stanwyck C, et al. Partner engagement for planning and development of non-pharmacological care pathways in the AIM-back trial. Clin Trials. (2023) 20(5):463–72. doi: 10.1177/17407745231178789
90. National Academies of Sciences, Engineering, and Medicine. Improving Representation in Clinical Trials and Research: Building Research Equity for Women and Underrepresented Groups. Washington, DC: National Academies Press (2022).
91. Ali J, Davis AF, Burgess DJ, Rhon DI, Vining R, Young-McCaughan S, et al. Justice and equity in pragmatic clinical trials: considerations for pain research within integrated health systems. Learn Health Syst. (2022) 6:e10291. doi: 10.1002/lrh2.10291
92. Quiñones AR, Mitchell SL, Jackson JD, Aranda MP, Dilworth-Anderson P, McCarthy EP, et al. Achieving health equity in embedded pragmatic trials for people living with dementia and their family caregivers. J Am Geriatr Soc. (2020) 68(Suppl 2):S8–s13. doi: 10.1111/jgs.16614
93. Tong L, George B, Crotty BH, Somai M, Taylor BW, Osinski K, et al. Telemedicine and health disparities: association between patient characteristics and telemedicine, in-person, telephone and message-based care during the COVID-19 pandemic. IPEM Transl. (2022) 3:100010. doi: 10.1016/j.ipemt.2022.100010
94. Chu C, Cram P, Pang A, Stamenova V, Tadrous M, Bhatia RS. Rural telemedicine use before and during the COVID-19 pandemic: repeated cross-sectional study. J Med Internet Res. (2021) 23:e26960. doi: 10.2196/26960
95. Khatana SAM, Yang L, Eberly LA, Julien HM, Adusumalli S, Groeneveld PW. Predictors of telemedicine use during the COVID-19 pandemic in the United States-an analysis of a national electronic medical record database. PLoS One. (2022) 17:e0269535. doi: 10.1371/journal.pone.0269535
96. Tauben DJ, Langford DJ, Sturgeon JA, Rundell SD, Towle C, Bockman C, et al. Optimizing telehealth pain care after COVID-19. Pain. (2020) 161:2437–45. doi: 10.1097/j.pain.0000000000002048
97. Seron P, Oliveros MJ, Gutierrez-Arias R, Fuentes-Aspe R, Torres-Castro R, Merino-Osorio C, et al. Effectiveness of telerehabilitation in physical therapy: a rapid overview. Phys Ther. (2021) 101:pzab053. doi: 10.1093/ptj/pzab053
Keywords: pragmatic clinical trials, telehealth, health equity, chronic pain, physical therapy
Citation: Fritz JM, Ford I, George SZ, Vinci de Vanegas L, Cope T, Burke CA and Goode AP (2024) Telehealth delivery of physical therapist-led interventions for persons with chronic low back pain in underserved communities: lessons from pragmatic clinical trials. Front. Pain Res. 5:1324096. doi: 10.3389/fpain.2024.1324096
Received: 18 October 2023; Accepted: 8 April 2024;
Published: 19 April 2024.
Edited by:
Aliaa Rehan Youssef, Cairo University, EgyptReviewed by:
Ruth Chimenti, The University of Iowa, United States© 2024 Fritz, Ford, George, Vinci de Vanegas, Cope, Burke and Goode. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Julie M. Fritz julie.fritz@utah.edu
 Julie M. Fritz
Julie M. Fritz Isaac Ford1
Isaac Ford1  Colleen A. Burke
Colleen A. Burke Adam P. Goode
Adam P. Goode