Behavior of Nutritional Supplements Use in Association With Inflammatory Skin Diseases in Chinese College Students
- 1The Department of Dermatology, Xiangya Hospital, Central South University, Changsha, China
- 2Hunan Key Laboratory of Skin Cancer and Psoriasis, Xiangya Hospital, Central South University, Changsha, China
- 3Hunan Engineering Research Center of Skin Health and Disease, Xiangya Hospital, Central South University, Changsha, China
- 4Department of Dermatology, Tongji Medical College, Union Hospital, Huazhong University of Science and Technology, Wuhan, China
- 5Department of Dermatology, People's Hospital of Xinjiang Uygur Autonomous Region, Urumchi, China
- 6Department of Dermatology, The Affiliated People's Hospital of Inner Mongolia Medical University, Hohhot, China
- 7Department of Dermatology, Xiang'an Hospital, Xiamen University, Xiamen, China
- 8Department of Dermatology, Zhongshan Hospital, Xiamen University, Xiamen, China
- 9Department of Social Medicine and Health Management, Xiangya School of Public Health, Central South University, Changsha, China
- 10Mobile Joint Laboratory, Xiangya Hospital, Central South University, Changsha, China
Objectives: It is understudied how frequently adolescents use nutritional supplements (NS) and whether the corresponding behavior is associated with skin diseases that may cause unpleasant symptoms and disfigurement. The current study aimed to investigate the prevalence of NS use in Chinese college students and its association with inflammatory skin diseases.
Methods: This was a university-based epidemiologic investigation that included 20,138 students who underwent dermatological examinations. A questionnaire survey was conducted to inquire about the use of NS along with related information. Skin diseases were diagnosed by dermatologists during the health examination. Logistic regression models were used for analysis. Adjusted odds ratios (aORs) were presented as the effect size.
Results: Survey responses from a total of 20,138 participants were analyzed. Specifically, 18.3% of the participants reported the use of NS in the past year. The use of vitamin C was most frequently reported, accounting for a proportion of 12.9%, followed by vitamin B and mineral supplements. The use of NS was found to be associated with female sex, Han ethnicity, higher annual household income, and a series of healthy lifestyles such as more physical activity, less second-hand smoke exposure, less alcohol consumption, and higher intake of milk and yogurt (p < 0.001). Participants with chronic urticaria (aOR = 1.3; 95% CI, 1.0–1.7), atopic dermatitis (aOR = 1.4; 95% CI, 1.2–1.6), or acne (aOR = 1.17; 95% CI, 1.04–1.31) were more likely to use NS, especially herbs (aOR = 2.7; 95% CI, 1.2–3.7), followed by vitamin B (aOR = 1.6; 95% CI, 1.2–2.0) and mineral supplements (aOR = 1.4; 95% CI, 1.0–2.0).
Conclusion: College students with inflammatory skin diseases are more likely to use NS.
Introduction
Nutritional supplement (NS) refers to a kind of healthcare product extracted from one or several chemical syntheses, natural plants, or animal ingredients. It usually contains some of the following nutrients: vitamins, minerals, fiber, proteins, etc. (1). NS use is generally popular in the USA, with prevalence rates varying from 21 to 55% reported by several different studies (2). Our previous study revealed that only 0.71% of the participants used NS within 1 month before the survey (3).
Evidence suggests that demographic characteristics, lifestyles, and health characteristics were significantly associated with the overall prevalence of NS use. It is well-known that individuals affected by certain chronic diseases often use complementary and alternative medicines [CAMs, which can be defined as “forms of treatment that are used in addition to (complementary) or instead of (alternative) standard treatments”] as a way to relieve the progression of their diseases, manage comorbidities, and intensify perceived control over their health condition. As a matter of fact, NS is one of the frequently used CAMs.
Atopic dermatitis (AD) is a chronic inflammatory skin condition involving complex interactions between immunologic, hereditary, and environmental influences (4), affecting up to 20% of children and 3% of adults worldwide over the last 30 years (5). Urticaria, manifesting as recurrent itchy wheals and/or angioedema, affects 0.5–1% of the general population (6), and 0.1–0.3% of children (7). Rosacea is a chronic inflammatory disease with multiple skin manifestations, including transient or persistent erythema, papules, pustules, recurrent flushing, telangiectasia, and probably phymatous changes (8). The prevalence of rosacea is estimated to vary from 1 to 22% across different reports (9–11). Acne vulgaris is a chronic inflammatory disease that affects 79–95% of the adolescent population in Western countries (12).
At present, there is a paucity of up-to-date studies reporting the prevalence of NS use among China's college students and elaborating whether NS use is more common among individuals with inflammatory skin diseases.
Methods
Study Design
This was a cross-sectional study performed at five comprehensive universities in China. All newly enrolled students who consented to participate in this study underwent a health examination and responded to an online questionnaire between September and October 2018. More details of the sample and sampling process can be found in our previous studies (13–16).
Questionnaire
A web-based questionnaire survey took place on a single day, organized by the Department of Student Affairs of the university. The participant freshmen completed the questionnaire in separate computer rooms where privacy was guaranteed. During the survey, three investigators were assigned to each room to provide technical support. The questionnaire consisted of 84 questions, including demographic information (ethnicity, original region, household annual income in yuan), disease history (cardiovascular/metabolic diseases, autoimmune diseases, infectious diseases, mental disorders, etc.), and behavior characteristics (cigarette smoking, passive smoking, alcohol drinking, soft drink intake, water intake, exercise, etc.). Within the questionnaire, one self-reported NS use items were asked: “Within the last year, which supplements were frequently used?” six supplements were listed as options for this item, including vitamin B, vitamin C, vitamin E, mineral, protein, and herbal. Participants were instructed to write in supplements they used.
Clinical Evaluation and Diagnosis
The diagnosis of skin diseases and inquiries regarding disease history were performed by certified dermatologists during the health examination. For recurrent skin diseases, only those with current symptoms and lesions were considered cases of point prevalence. Height and weight were measured using standardized methods, which were used then to calculate the body mass index.
Statistical Analysis
Continuous data were presented as mean ± standard deviation, and the between-group differences were tested using analysis of variance. Categorical data were presented as an absolute number in form of percentage (%), and the between-group differences were tested using the Chi-square test. Logistic models were used to estimate the effects of inflammatory skin diseases on the behavior of NS use. Odds ratios (ORs) and 95% confidence intervals (CIs) were estimated from the model. Adjusted odds ratios (aORs) were further estimated by adjusting for covariates [adjustment included level-1 confounders (age, gender, region, ethnicity, and annual household income) and level-2 confounder (daily alcohol drinking, intake of milk and yogurt, passive smoking, sport, sedentary activities)]. Statistical analysis was performed using SPSS 25.0 (IBM SPSS, Chicago, IL), and P < 0.05 was considered statistically significant.
Results
A total of 20,138 students underwent the dermatological examination and completed a specially designed questionnaire after giving consent to this cross-sectional study. Of the participants, 3,703 (18.3%) reported the use of NS in the past year (see Supplementary Table 1 for the use of each type of NS). The use of vitamin C was most frequently reported, accounting for a proportion of 12.9%, followed by vitamin B and mineral supplements.
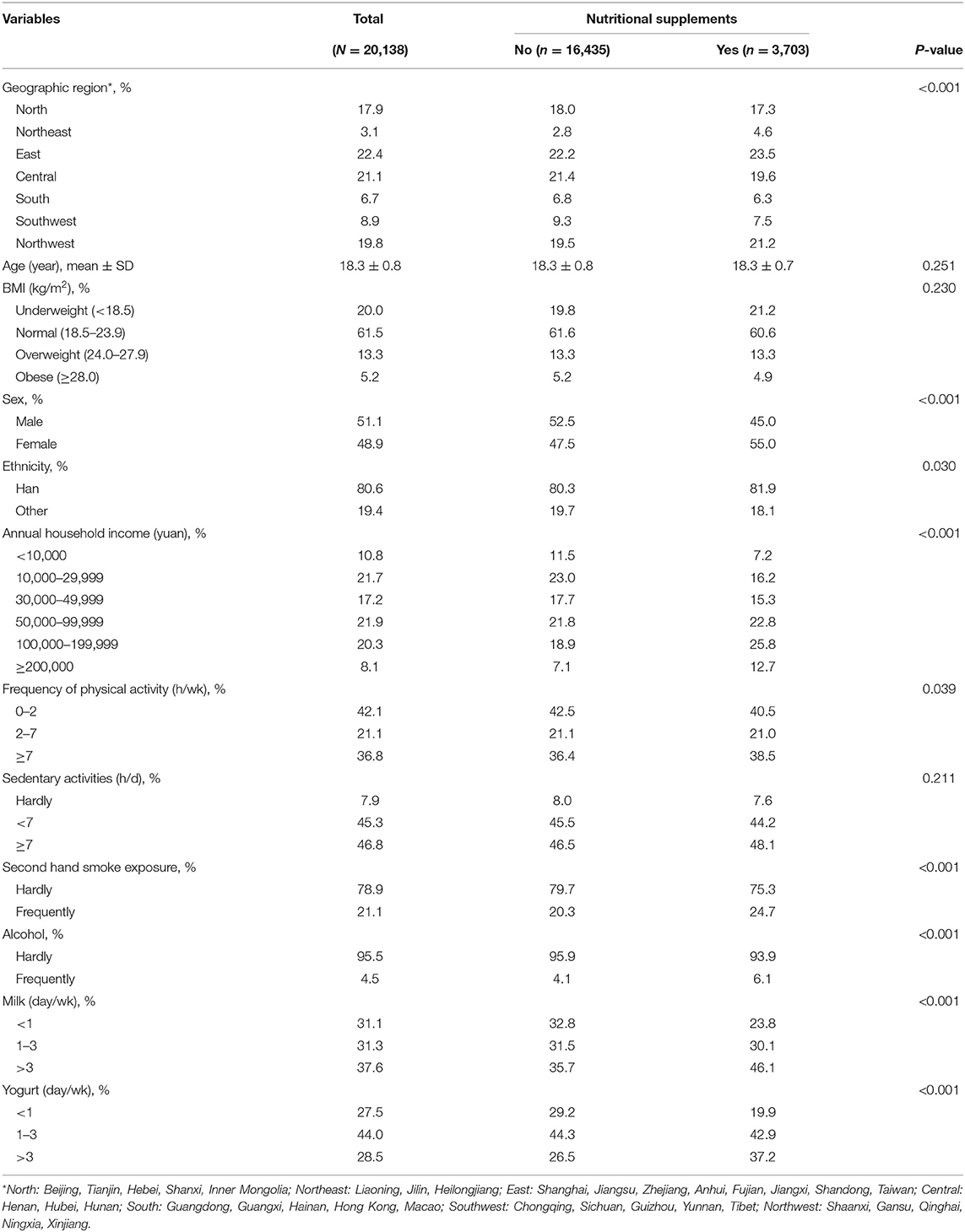
The characteristics of the participants stratified by the prevalence of NS use are shown in Table 1. The use of NS was found to be associated with female sex, Han ethnicity, higher annual household income, and a series of healthy lifestyles including more physical activity, less second-hand smoke exposure, less alcohol consumption, and higher intake of milk and yogurt (P < 0.001).
The association between skin diseases and NS use was examined. As shown in Table 2, participants with inflammatory skin diseases, such as CU (Ptrend = 0.002) and AD (Ptrend = 0.001), were associated with a higher prevalence of NS use, especially vitamin C, followed by vitamin B and mineral supplements. By contrast, the association between acne or rosacea and the prevalence of NS use was statistically insignificant (Ptrend > 0.05).
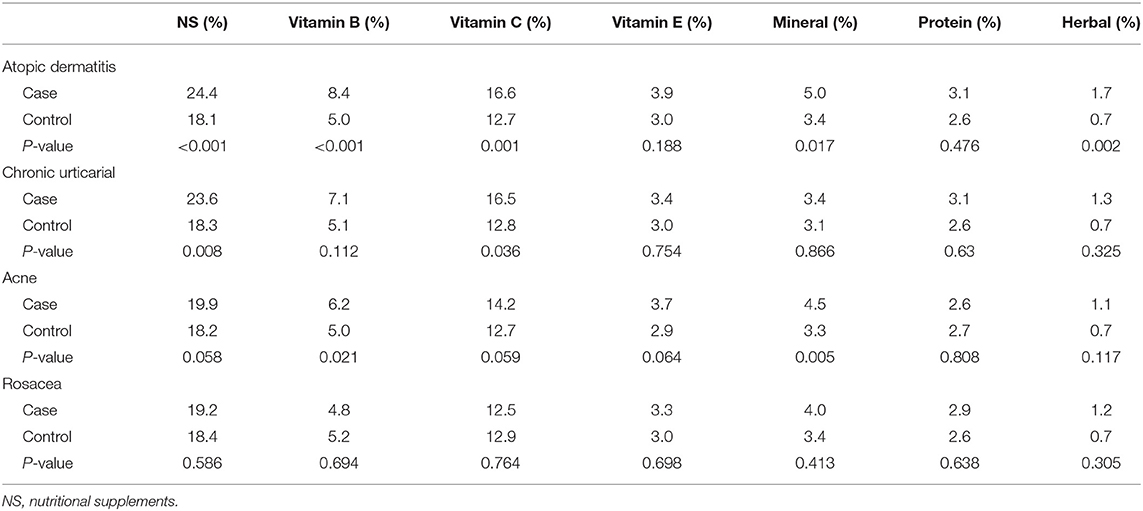
Table 2. Use of nutritional supplements in participants with and without inflammatory skin diseases.
The association of NS use with inflammatory skin diseases was then further adjusted for covariates. As shown in Table 3, the crude and adjusted estimates demonstrated a good consistency. After adjustments for demographic and behavioral factors, the results remained consistent: participants with chronic urticaria (aOR = 1.3; 95% CI, 1.0–1.7), atopic dermatitis (aOR = 1.4; 95% CI, 1.2–1.6), or acne (aOR = 1.17; 95% CI, 1.04–1.31) were more likely to use NS, especially herbs (aOR = 2.7; 95% CI, 1.2–3.7), followed by vitamin B (aOR = 1.6; 95% CI, 1.2–2.0) and mineral supplements (aOR = 1.4; 95% CI, 1.0–2.0).
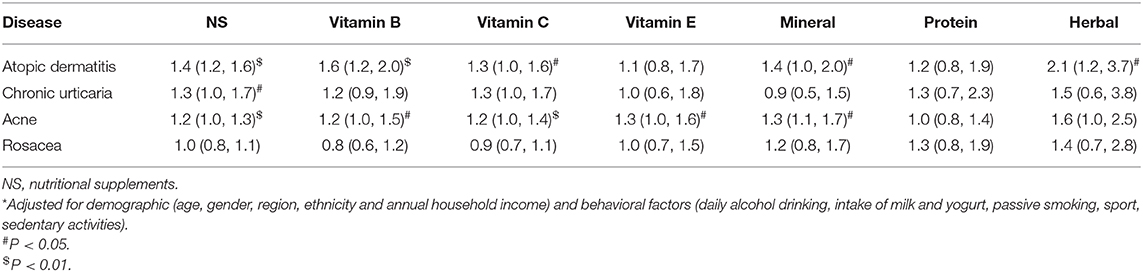
Table 3. Adjusted odds ratios for the association of inflammatory skin diseases and use of nutritional supplements*.
Discussion
This was the first study that provided detailed information on NS use among Chinese college students, and that linked inflammatory skin diseases, especially atopic conditions, acne, and urticaria, with NS use in China.
The overall prevalence of NS use was 18.4% among college students. This finding was higher than other surveys in China (2) but lower than those in other countries (17–22). A lower prevalence was also reported among preschool children in China (2) compared with the USA (23, 24). NS use was more popular in developed countries, which might be attributed to the emphasis of using NS to ensure nutrient adequacy by the Dietary Guidelines (25). However, NS is not recommended for the general population, while acquiring adequate and comprehensive natural nutrients from daily diet is prioritized by the guidelines (26). The most popular NS consumed by college students in our study was vitamin C, followed by vitamin B and mineral supplements, and similar trends were also reported by other studies (27, 28).
Demographic characteristics were found to be associated with the overall prevalence of NS use. Specifically, NS use varies by sex, geography, ethnicity, and annual household income, which serves as a surrogate for one's socioeconomic status; for example, participants with a higher level of annual household income and purchasing power have better accessibility to NS and stronger healthcare consciousness, and as a result, more of them use NS (29).
The current study suggested that NS use was associated with health-related characteristics and might serve as a marker for a range of other health-related behaviors, evidenced by lower prevalence rates of passive smoking and alcohol drinking, higher frequency of sports activity, and higher intake of milk and yogurt, which was similar to the earlier-reported tendency for smoking, BMI, and physical activity; NS users have been characterized as having a positive attitude toward their health. In addition, this study showed that participants suffering from inflammatory skin diseases were more likely to use NS. This result was consistent with the findings of previous research (30, 31). Apart from inflammatory skin diseases, NS use had also been associated with a variety of other diseases (32), such as cancer and cardiac disease. This may be attributable to the fact that people with health problems have stronger health awareness and are more likely to change their lifestyles to improve health conditions (30, 31). Among the various skin diseases, participants with AD reported the highest proportion of NS use. This may be related to the public awareness that certain nutrients can reduce oxidative damage to cells and tissues (33–35) by neutralizing reactive oxygen species (36). In contrast, no association was found between rosacea and NS use. A possible reason is that rosacea is not a well-known skin problem by the public, and many patients would never visit a dermatologist for rosacea owing to subclinical or atypical symptoms or even misdiagnosis (37).
This study has some limitations. First, data was not collected on the amount of NS use. However, with our preliminary result, further study with quantitative measurements of NS on skin diseases are expecting. Second, since our sample was confined to college students with similar educational backgrounds, there might be a selection bias in representing general adolescents across China. Third, our hypothesis that patients with inflammatory diseases are more likely to use NS could not be confirmed owing to the cross-sectional study design.
The strengths of this study are more worth mentioning. First, this was a large-sample and multicenter study. Second, it was the first population-based study that linked inflammatory skin diseases with NS use in China. A comprehensive understanding of the characteristics of NS users can help develop effective public health interventions to reduce unnecessary consumption of NS. Third, this study had a high response rate and high completeness of questionnaires, and the ascertainment of skin diseases was performed by dermatologists, resulting in satisfying quality of evidence.
In summary, by examining the prevalence of NS use, the current study revealed that NS use was more prevalent among China's college students suffering from inflammatory skin diseases. Although there is at least moderate-quality evidence to support the effectiveness of NS for AD patients, the lack of long-term observation makes it challenging to determine whether NS is beneficial in real-world settings. Further research is required to elaborate on the reason or motivation for NS use. Given the fact that individuals with inflammatory skin diseases are more likely to use NS, health practitioners should be prepared to pay attention to the potential benefits and risks of various NS products in the context of inflammatory skin diseases.
Moreover, the public did not have enough understanding and the appropriate attitude about NS because it has only just become known over the past decade; therefore, government regulators and the scientific community should strengthen the supervision of NS industry and NS product marketing, widely publicize NS related information through various publicity channels to avoid false and exaggerated publicity, and then help people gain better understandings of NS.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics Statement
This study was conducted according to the guidelines laid down in the Declaration of Helsinki. All procedures involving study participants were approved by the institutional research Ethics Board of Xiangya Hospital, Central South University (Changsha, China). Written informed consent was obtained from all participants before the investigation.
Author Contributions
YY analyzed the data and drafted the manuscript. LJ, MS, and XC designed the study. JS, JL, JT, XK, BW, SS, and XW acted as study site coordinators. MS, JS, and XC obtained the funding. All authors participated in the field survey and data collection, critically revised the manuscript, and gave final approval to the version submitted for publication.
Funding
This work was supported by the National Key Research and Development Project of China Precision Medicine Initiative (2016YFC0900802) and Central South University (202045005).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank the following dermatologists and investigators who participated in the field survey (in order of family name).
Central South University: Lei Cai, Duling Cao, Qin Cao, Chao Chen, Liping Chen, Menglin Chen, Mengting Chen, Xiang Chen, Qing Deng, Xin Gao, Yihuan Gong, Jia Guo, Yeye Guo, Rui Hu, Xin Hu, Chuchu Huang, Huining Huang, Kai Huang, Xiaoyan Huang, Yuzhou Huang, Danrong Jing, Xinwei Kuang, Li Lei, Jia Li, Jiaorui Li, Jie Li, Keke Li, Peiyao Li, Yajia Li, Yayun Li, Yangfan Li, Dan Liu, Dihui Liu, Fangfen Liu, Nian Liu, Panoan Liu, Runqiu Liu, Hui Lu, Wenhua Lu, Yan Luo, Zhongling Luo, Manyun Mao, Mengping Mao, Yuyan Ouyang, Shiyao Pei, Qunshi Qin, Ke Sha, Lirong Tan, Ling Tang, Ni Tang, Yan Tang, Ben Wang, Yaling Wang, Tianhao Wu, Yun Xie, Siyu Yan, Sha Yan, Bei Yan, Xizhao Yang, Lin Ye, Hu Yuan, Taolin Yu, Yan Yuan, Yi Yu, Rui Zhai, Jianghua Zhang, Jianglin Zhang, Mi Zhang, Xingyu Zhang, Zhibao Zhang, Yaqian Zhao, Kuangbiao Zhong, Lei Zhou, Youyou Zhou, Zhe Zhou, and Susi Zhu.
Huazhong University of Science and Technology: Xiangjie An, Siqi Da, Yaqi Dong, Yangxue Fu, Lixie Gao, Han Han, Biling Jiang, Jiajia Lan, Jun Li, Xiaonan Li, Yan Li, Liquan Liu, Yuchen Lou, Pu Meng, Yingli Nie, Gong Rao, Shanshan Sha, Xingyu Su, Huinan Suo, Rongying Wang, Jun Xie, Yuanxiang Yi, Jia Zhang, Qiao Zhang, Li Zhu, Yanming Zhu.
Xiamen University: Zhiming Cai, Lina Chen, Xiaozhu Fu, Hongjun Jiang, Guihua Luo, Jianbing Xiahou, and Binxiang Zheng.
People's Hospital of Xinjiang Uygur Autonomous Region: Jianxia Chen, Xiaomin Chen, Xinqi Chen, Li Dai, Yanyan Feng, Fanhe Jiang, Lan Jin, Qingyu Ma, Qun Shi, Hongbo Tang, Fang Wang, Zhen Wang, Xiujuan Wu, Kunjie Zhang, and Yu Zhang.
Xinjiang Medical University: Huagui Li, Jianguang Li, and Lei Shi.
Inner Mongolia Medical University: Wei Wang, Rina Wu, Hongjun Xing, and Baogui Yang.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2021.615462/full#supplementary-material
References
1. Radimer K, Bindewald B, Hughes J, Ervin B, Swanson C, Picciano MF. Dietary supplement use by US adults: data from the National Health and Nutrition Examination Survey, 1999-2000. Am J Epidemiol. (2004) 160:339–49. doi: 10.1093/aje/kwh207
2. Gong W, Liu A, Yao Y, Ma Y, Ding C, Song C, et al. Nutrient supplement use among the chinese population: a cross-sectional study of the 2010(-)2012 china nutrition and health surveillance. Nutrients. (2018) 10.:1733 doi: 10.3390/nu10111733
3. Velicer CM, Ulrich CM. Vitamin and mineral supplement use among US adults after cancer diagnosis: a systematic review. J Clin Oncol. (2008) 26:665–73. doi: 10.1200/JCO.2007.13.5905
4. Omata N, Tsukahara H, Ito S, Ohshima Y, Yasutomi M, Yamada A, et al. Increased oxidative stress in childhood atopic dermatitis. Life Sci. (2001) 69:223–8. doi: 10.1016/S0024-3205(01)01124-9
5. Mei-Yen Yong A, Tay YK. Atopic dermatitis: racial and ethnic differences. Dermatol Clin. (2017) 35:395–402. doi: 10.1016/j.det.2017.02.012
6. Shahzad Mustafa S, Sanchez-Borges M. Chronic urticaria: comparisons of US, European, and Asian guidelines. Curr Allergy Asthma Rep. (2018) 18:36. doi: 10.1007/s11882-018-0789-3
7. Kaplan AP. Clinical practice. Chronic urticaria and angioedema. N Engl J Med. (2002) 346:175–9. doi: 10.1056/NEJMcp011186
8. van Zuuren EJ, Fedorowicz Z, Carter B, van der Linden MM, Charland L. Interventions for rosacea. Cochrane Database Syst Rev. (2015) 2015:Cd003262. doi: 10.1002/14651858.CD003262.pub5
9. Elewski BE, Draelos Z, Dréno B, Jansen T, Layton A, Picardo M. Rosacea - global diversity and optimized outcome: proposed international consensus from the Rosacea International Expert Group. J Eur Acad Dermatol Venereol. (2011) 25:188–200. doi: 10.1111/j.1468-3083.2010.03751.x
10. Tan J, Berg M. Rosacea: current state of epidemiology. J Am Acad Dermatol. (2013) 69(6 Suppl. 1):S27–35. doi: 10.1016/j.jaad.2013.04.043
11. McAleer MA, Fitzpatrick P, Powell FC. Papulopustular rosacea: prevalence and relationship to photodamage. J Am Acad Dermatol. (2010) 63:33–9. doi: 10.1016/j.jaad.2009.04.024
12. Cordain L, Lindeberg S, Hurtado M, Hill K, Eaton SB, Brand-Miller J. Acne vulgaris: a disease of Western civilization. Arch Dermatol. (2002) 138:1584–90. doi: 10.1001/archderm.138.12.1584
13. Huang X, Zhang J, Li J, Zhao S, Xiao Y, Huang Y, et al. Daily intake of soft drinks and moderate-to-severe acne vulgaris in chinese adolescents. J Pediatrics. (2019) 204:256–62.e253. doi: 10.1016/j.jpeds.2018.08.034
14. Zhang X, Huang X, Xiao Y, Jing D, Huang Y, Chen L, et al. Daily intake of soft drinks is associated with symptoms of anxiety and depression in Chinese adolescents. Public Health Nutr. (2019) 22:2553–60. doi: 10.1017/S1368980019001009
15. Zuo Z, Wang B, Shen M, Xie H, Li J, Chen X, et al. Skincare habits and rosacea in 3,439 Chinese adolescents: a university-based cross-sectional study. Acta Dermato Venereol. (2020) 100:adv00081. doi: 10.2340/00015555-3442
16. Xiao Y, Huang X, Jing D, Huang Y, Chen L, Zhang X, et al. The prevalence of atopic dermatitis and chronic spontaneous urticaria are associated with parental socioeconomic status in adolescents in China. Acta Dermato Venereol. (2019) 99:321–6. doi: 10.2340/00015555-3104
17. Lieberman HR, Marriott BP, Williams C, Judelson DA, Glickman EL, Geiselman PJ, et al. Patterns of dietary supplement use among college students. Clin Nutr. (2015) 34:976–85. doi: 10.1016/j.clnu.2014.10.010
18. Wiltgren AR, Booth AO, Kaur G, Cicerale S, Lacy KE, Thorpe MG, et al. Micronutrient supplement use and diet quality in university students. Nutrients. (2015) 7:1094–107. doi: 10.3390/nu7021094
19. Hoyte CO, Albert D, Heard KJ. The use of energy drinks, dietary supplements, and prescription medications by United States college students to enhance athletic performance. J Commun Health. (2013) 38:575–80. doi: 10.1007/s10900-013-9653-5
20. Kristiansen M, Levy-Milne R, Barr S, Flint A. Dietary supplement use by varsity athletes at a Canadian university. Int J Sport Nutr Exer Metab. (2005) 15:195–210. doi: 10.1123/ijsnem.15.2.195
21. Spencer EH, Bendich A, Frank E. Vitamin and mineral supplement use among US medical students: a longitudinal study. J Am Dietetic Assoc. (2006) 106:1975–83. doi: 10.1016/j.jada.2006.09.003
22. Marku M, McCarthy BC Jr. Dietary supplement use, knowledge, and perceptions among student pharmacists. Am J Pharm Educ. (2017) 81:6775. doi: 10.5688/ajpe6775
23. Picciano MF, Dwyer JT, Radimer KL, Wilson DH, Fisher KD, Thomas PR, et al. Dietary supplement use among infants, children, and adolescents in the United States, 1999-2002. Arch Pediatrics Adolesc Med. (2007) 161:978–85. doi: 10.1001/archpedi.161.10.978
24. Bailey RL, Gahche JJ, Thomas PR, Dwyer JT. Why US children use dietary supplements. Pediatric Res. (2013) 74:737–41. doi: 10.1038/pr.2013.160
25. Tagtow A, Rahavi E, Bard S, Stoody EE, Casavale K, Mosher A. Coming together to communicate the 2015-2020 dietary guidelines for Americans. J Acad Nutr Dietetics. (2016) 116:209–12. doi: 10.1016/j.jand.2015.12.010
26. Wang SS, Lay S, Yu HN, Shen SR. Dietary Guidelines for Chinese Residents : comments and comparisons. J Zhejiang Univ Sci B. (2016) 17:649–56. doi: 10.1631/jzus.B1600341
27. Kim SH, Keen CL. Patterns of vitamin/mineral supplement usage by adolescents attending athletic high schools in Korea. Int J Sport Nutr. (1999) 9:391–405. doi: 10.1123/ijsn.9.4.391
28. Use of vitamin and mineral supplements in the United States. Nutr Rev. (1990) 48:161–2. doi: 10.1111/j.1753-4887.1990.tb02922.x
29. Dickinson A, MacKay D. Health habits and other characteristics of dietary supplement users: a review. Nutr J. (2014) 13:14. doi: 10.1186/1475-2891-13-14
30. Kofoed CL, Christensen J, Dragsted LO, Tjonneland A, Roswall N. Determinants of dietary supplement use–healthy individuals use dietary supplements. Br J Nutr. (2015) 113:1993–2000. doi: 10.1017/S0007114515001440
31. Satia-Abouta J, Kristal AR, Patterson RE, Littman AJ, Stratton KL, White E. Dietary supplement use and medical conditions: the VITAL study. Am J Prev Med. (2003) 24:43–51. doi: 10.1016/S0749-3797(02)00571-8
32. Bours MJ, Beijer S, Winkels RM, van Duijnhoven FJ, Mols F, Breedveld-Peters JJ, et al. Dietary changes and dietary supplement use, and underlying motives for these habits reported by colorectal cancer survivors of the Patient Reported Outcomes Following Initial Treatment and Long-Term Evaluation of Survivorship (PROFILES) registry. Br J Nutr. (2015) 114:286–96. doi: 10.1017/S0007114515001798
33. Devereux G, Seaton A. Diet as a risk factor for atopy and asthma. J Allergy Clin Immunol. (2005) 115:1109–17; quiz 1118. doi: 10.1016/j.jaci.2004.12.1139
34. Kouda K, Tanaka T, Kouda M, Takeuchi H, Takeuchi A, Nakamura H, et al. Low-energy diet in atopic dermatitis patients: clinical findings and DNA damage. J Physiol Anthropol Appl Human Sci. (2000) 19:225–8. doi: 10.2114/jpa.19.225
35. Shin J, Kim YJ, Kwon O, Kim NI, Cho Y. Associations among plasma vitamin C, epidermal ceramide and clinical severity of atopic dermatitis. Nutr Res Prac. (2016) 10:398–403. doi: 10.4162/nrp.2016.10.4.398
36. Vaughn AR, Foolad N, Maarouf M, Tran KA, Shi VY. Micronutrients in atopic dermatitis: a systematic review. J Alternative Complement Med. (2019) 25:567–77. doi: 10.1089/acm.2018.0363
Keywords: nutritional supplements use, inflammatory skin disease, college students, behavior, NS use
Citation: Yuan Y, Su J, Li J, Tao J, Kang X, Wu B, Shan S, Wang X, Chen X, Shen M and Jiang L (2021) Behavior of Nutritional Supplements Use in Association With Inflammatory Skin Diseases in Chinese College Students. Front. Nutr. 8:615462. doi: 10.3389/fnut.2021.615462
Received: 09 October 2020; Accepted: 13 January 2021;
Published: 17 March 2021.
Edited by:
Nicholas T. Bello, Rutgers, The State University of New Jersey, United StatesReviewed by:
Natalie Caine-Bish, Kent State University, United StatesXiaodong Zheng, Anhui Medical University, China
Copyright © 2021 Yuan, Su, Li, Tao, Kang, Wu, Shan, Wang, Chen, Shen and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liyuan Jiang, jiangliyuan01@hotmail.com
 Yan Yuan
Yan Yuan Juan Su
Juan Su Ji Li
Ji Li Juan Tao4
Juan Tao4  Xiang Chen
Xiang Chen Minxue Shen
Minxue Shen