- 1Department of Neurosurgery, Ningbo Medical Center Lihuili Hospital, Ningbo, China
- 2Department of Radiology, Beijing Hospital, National Center of Gerontology; Institute of Geriatric Medicine, Chinese Academy of Medical Sciences, Beijing, China
- 3Graduate School of Peking Union Medical College, Beijing, China
Objective: Thrombectomy may provide superior results compared to best medical care for acute posterior circulation strokes (PCS). Contact aspiration (CA), stent retriever (SR), and combined SR + CA (SRA) are commonly employed as first-line techniques. However, the optimal strategy and the role of SRA remain uncertain.
Methods: Systematic searching was conducted in three databases (PubMed, Embase, and Cochrane). Network meta-analyzes were performed using random-effects models. The reperfusion and clinical outcomes were compared. Pooled outcomes were presented as odds ratios (OR) with 95% confidence intervals (CI). Rankograms with surface under the cumulative ranking curve (SUCRA) were calculated.
Results: Seventeen studies were included, involving a total of 645 patients who received first-line CA, 850 patients who received SR, and 166 patients who received SRA. Regarding final recanalization outcomes, both first-line SRA (OR = 3.2, 95%CI 1.4–11.0) and CA (OR = 2.1, 95%CI 1.3–3.7) demonstrated superiority over SR in achieving successful reperfusion [modified Thrombolysis In Cerebral Infarction (mTICI) 2b-3], with values of SUCRA 91.1, 58.5, and 0.4%, respectively. In addition, first-line SRA showed an advantage in achieving final mTICI 2c/3 compared to CA (OR = 3.6, 95%CI 0.99–16.0) and SR (OR = 6.4, 95%CI 1.3–35.0), with SUCRA value of 98.0, 44.7, and 7.2%, respectively. Regarding reperfusion outcome after the first pass, SRA also achieved a higher rate of mTICI 3 than SR (OR = 4.1, 95%CI 1.3–14.0), while CA did not (SUCRA 97.4, 4.6, 48.0%). In terms of safety outcomes, first-line CA was associated with a lower incidence of symptomatic intracranial hemorrhage (sICH) compared to SR (OR = 0.38, 95%CI 0.1–1.0), whereas the SRA technique did not (SUCRA 15.6, 78.6, 55.9%). Regarding clinical prognosis, first-line CA achieved a higher proportion of functional independence (modified Rankin Scale (mRS) 0–2) at 90 days than SR (OR = 1.4, 95%CI 1.1–1.9), whereas SRA did not (SUCRA 90.5, 17.4, 42.1%).
Conclusion: For acute PCS, a first-line CA strategy yielded better results in terms of final successful reperfusion and 90-day functional independence compared to SR. As the combined technique, first-line SRA was associated with superior first-pass and final reperfusion outcomes compared to SR. However, no significant difference was observed in functional independence achieved by first-line SRA compared to the other two strategies. Further high-quality studies are warranted.
Introduction
Posterior circulation strokes (PCS), particularly basilar artery occlusion (BAO), are associated with unfavorable clinical outcomes (1, 2). Although two randomized controlled trials (RCTs), the BEST (3) and BASICS (4) trials, did not show significant differences between endovascular therapy and medical therapy for acute PCS, accumulating evidence supported the potential essential role of endovascular thrombectomy. Both BAOCHE (5) and ATTENTION (6) trials, as well as a meta-analysis of the above four RCTs (7, 8), have suggested that endovascular treatment might improve clinical prognosis compared to best medical care. Consequently, endovascular therapy is widely used for acute PCS in clinical practice.
As first-line strategies, all the following three thrombectomy techniques are commonly applied: contact aspiration (CA), stent retriever (SR), as well as a combined technique of SR and CA (SRA). The SR technique was primarily employed in the BEST (3) and BAOCHE (5) trials, while CA was widely used in the BASICS (4) and ATTENTION (6) trials. Previous meta-analyzes have indicated that CA might be superior to SR in terms of reperfusion and clinical outcomes (9, 10). Furthermore, it is worth mentioning that SRA was used for nearly half of the patients in the ATTENTION trials (6). However, there is still an unclear comparison between these three first-line strategies, especially regarding the efficacy and safety of SRA. Therefore, this study was aimed to perform a network meta-analysis.
Methods
The systematic review was reported in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyzes) guidelines (11).
Literature inclusion and risk of bias assessment
Studies reporting reperfusion and clinical outcomes of different first-line strategies for acute PCS were included. A systematic search was conducted in three databases (PubMed, Embase, and Cochrane) for literature published before April 26, 2023. The PubMed search algorithm used was as follows: (((posterior circulation stroke*[Title/Abstract]) OR (basilar artery occlusion [Title/Abstract])) AND (stent*[Title/Abstract])) AND (aspiration*[Title/Abstract]). Exclusion criteria were as follows: (1) secondary review papers; (2) conference abstracts; (3) studies without a comparison between groups; (4) sample size in either group less than 10 cases.
Risk of bias was assessed using the Newcastle Ottawa scale for cohort studies (12). Factors indicating a low risk of bias included well-defined selection criteria, comparable baseline stroke severity, and independent assessment of recanalization and clinical outcomes. Two investigators independently conducted the literature search, selection, and risk of bias assessment. Discrepancies were resolved through discussion and consensus.
Data extraction
The following clinical characteristics were extracted: (1) baseline characteristics: patient number, age, sex, occlusion site, stroke etiology, duration from onset to puncture, National Institutes of Health Stroke Scale (NIHSS) score on admission, intravenous thrombolysis; (2) recanalization outcomes: final successful recanalization [modified Thrombolysis In Cerebral Infarction (mTICI) 2b-3], final excellent reperfusion (mTICI 2c-3), final complete reperfusion (mTICI 3), complete reperfusion after first-pass of maneuvers (first pass effect, FPE), successful reperfusion after first-pass of maneuvers (mFPE), number of passes, new-territory embolic event, rescue therapy, duration from puncture to reperfusion, procedure duration; (3) clinical outcomes: functional independence [modified Rankin Scale (mRS) 0–2] and mortality at 90 days, symptomatic intracranial hemorrhagic event (sICH).
Outcome variables and statistical analysis
The following primary outcomes were compared: final successful reperfusion, FPE, and 90-day functional independence. Secondary outcomes included final excellent reperfusion, final complete reperfusion, mFPE, sICH, and mortality. Random-effect network meta-analyzes were performed using Bayesian Markov chain Monte Carlo modeling. Forest plots were utilized to present pooled estimates, and odds ratios (OR) with 95% confidence intervals (CI) were calculated. Rankograms were constructed, and the surface under the cumulative ranking curve (SUCRA) was calculated to determine treatment ranking probabilities. Heterogeneity between studies was assessed using the I2 statistic, and I2 > 50% indicated moderate to high heterogeneity. Statistical analyzes were conducted using R software (V 3.6.2).
Results
Literature search inclusion and overview
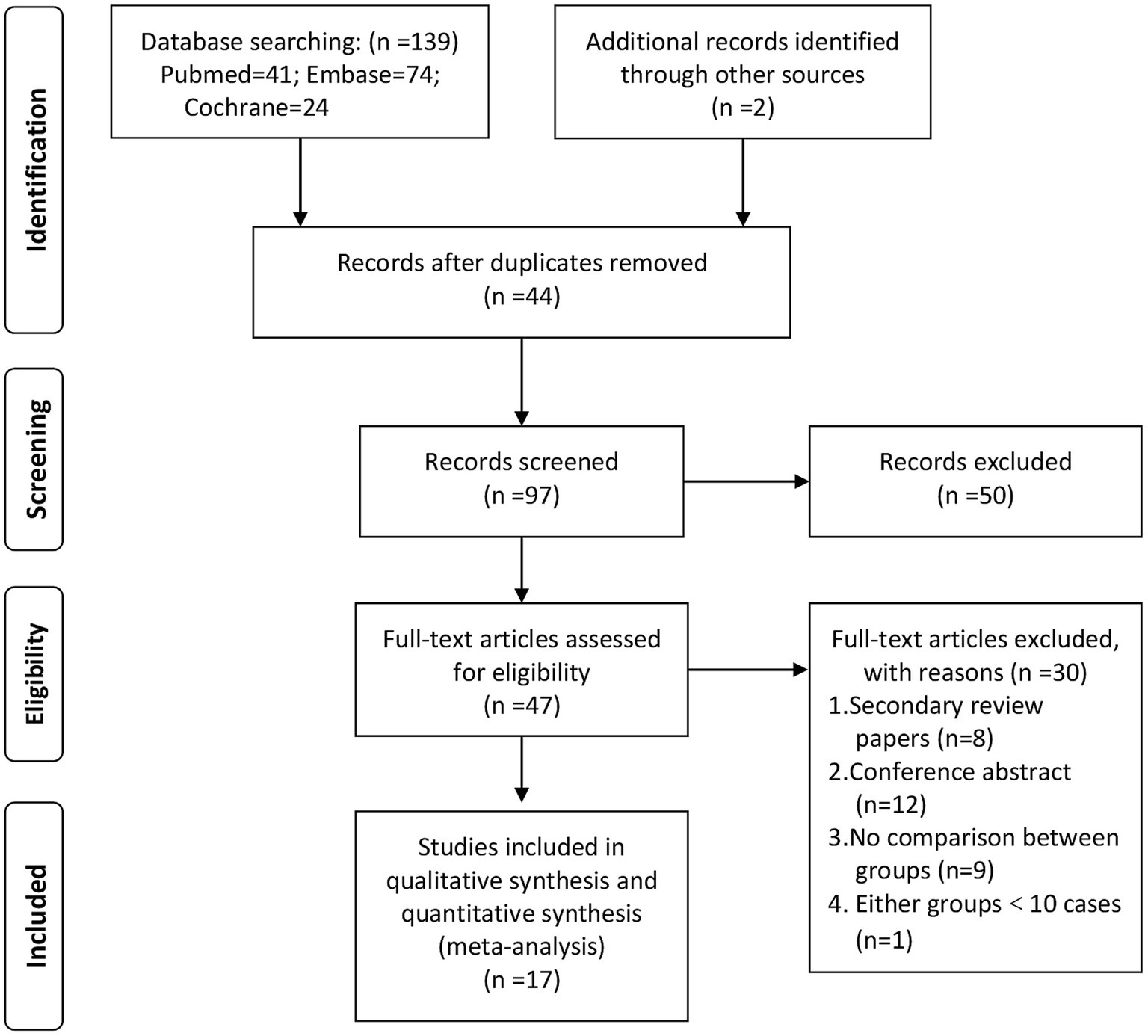
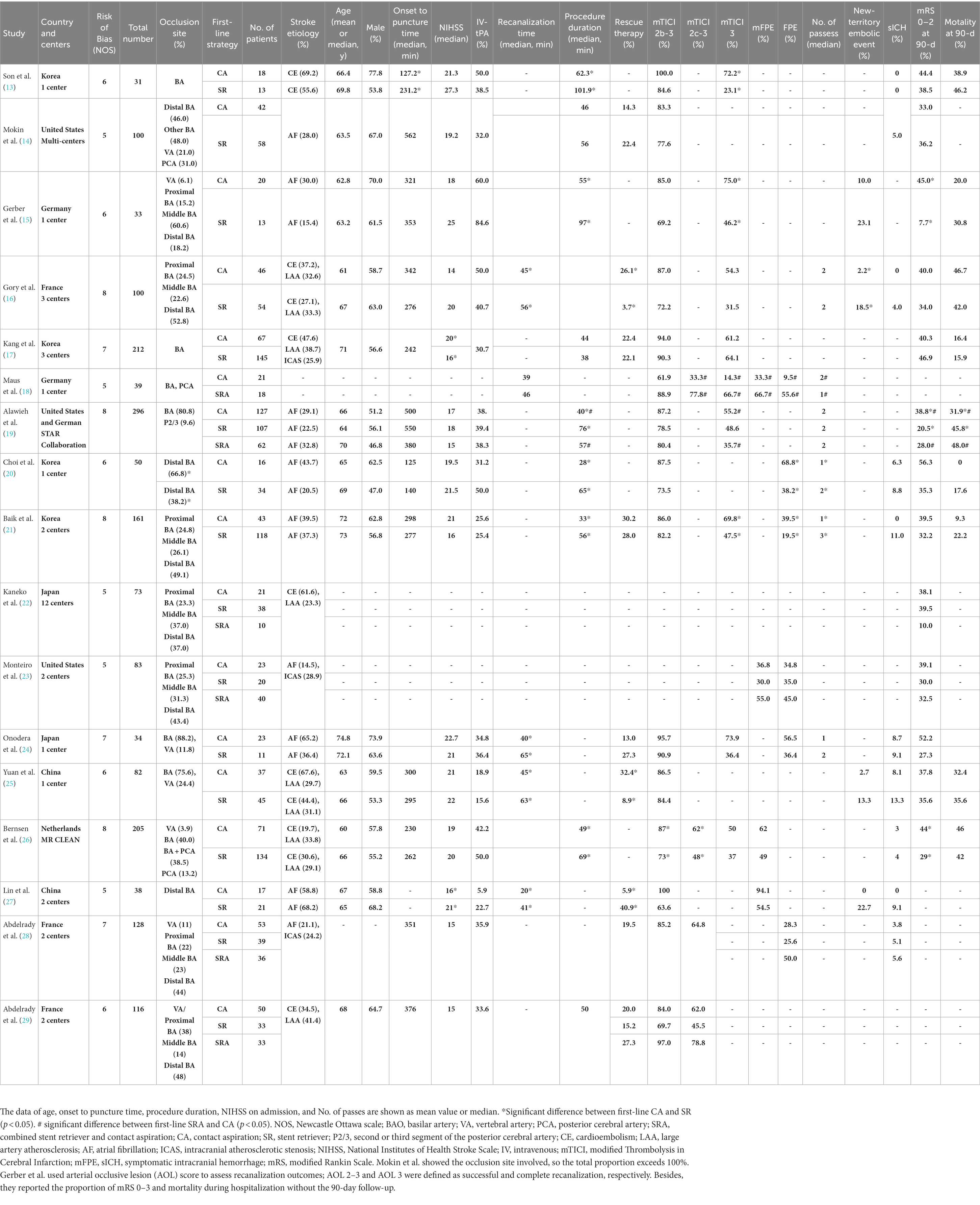
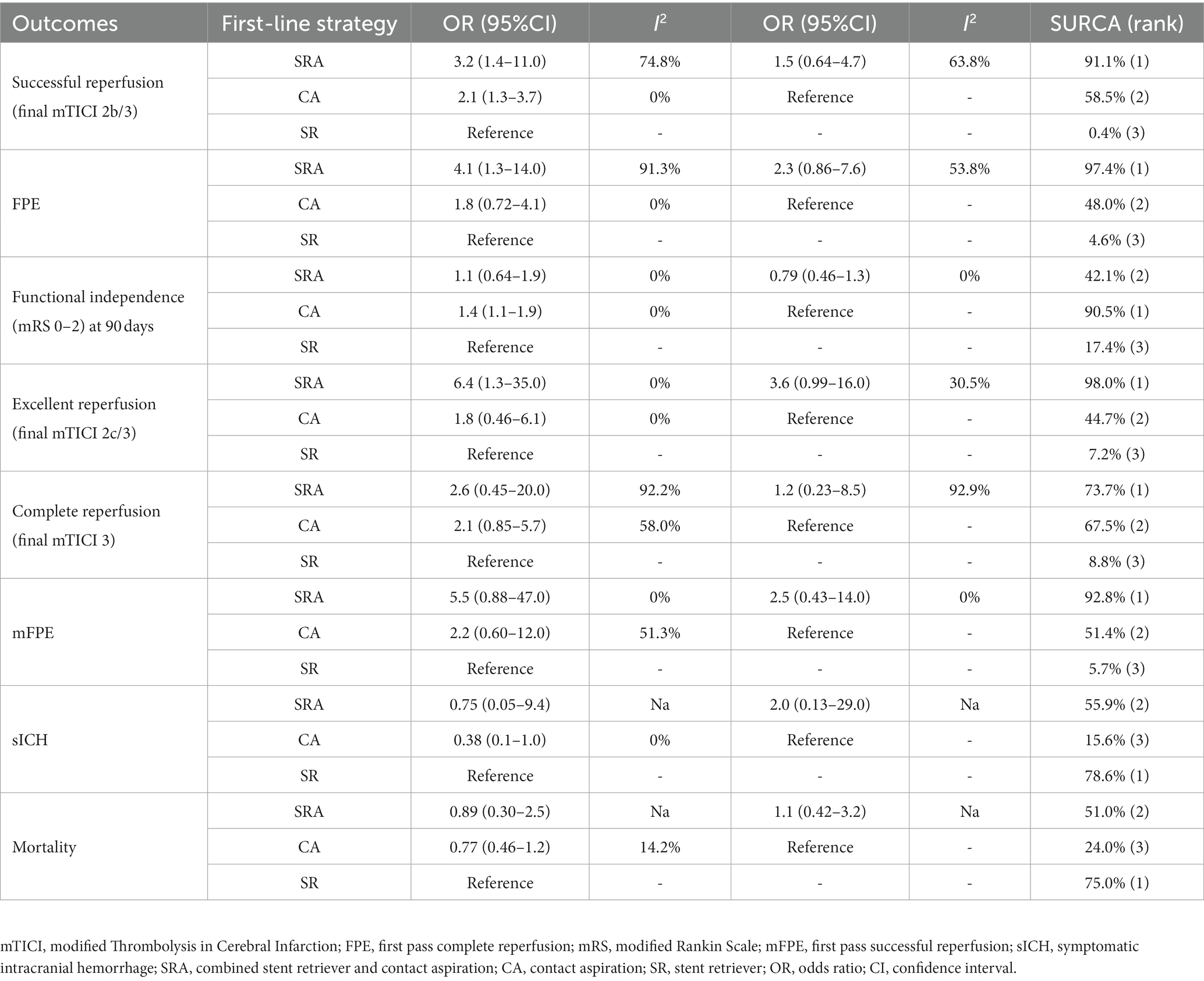
Figure 1 presents the flow diagram for the literature search and selection process. Seventeen observational studies were included in this analysis (13–29). The first-line strategies of CA, SR and SRA were used in 645, 850, and 166 patients, respectively. Table 1 provides an overview of the clinical characteristics of the included studies. Network plots, forest plots, and rankograms are displayed in Figures 2, 3. The pooled estimates and ranking probabilities are summarized in Table 2. The risk of bias assessment and the results of the heterogeneity test are presented in the Supplementary material.
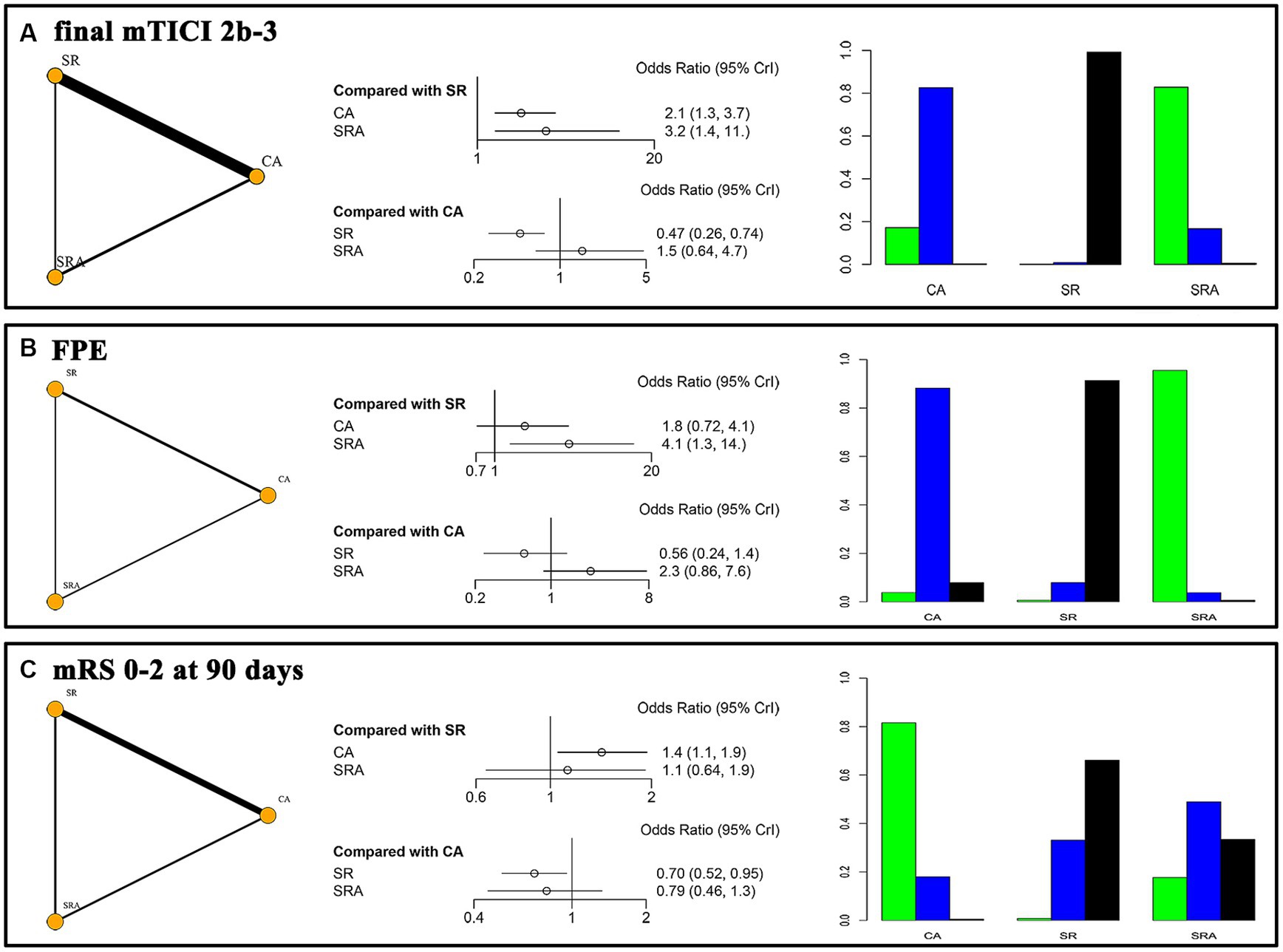
Figure 2. Network plots, forest plots, and rankograms for the primary outcomes. (A) final mTICI 2b/3; (B) FPE, first pass complete reperfusion; (C) mRS 0–2 at 90 days.
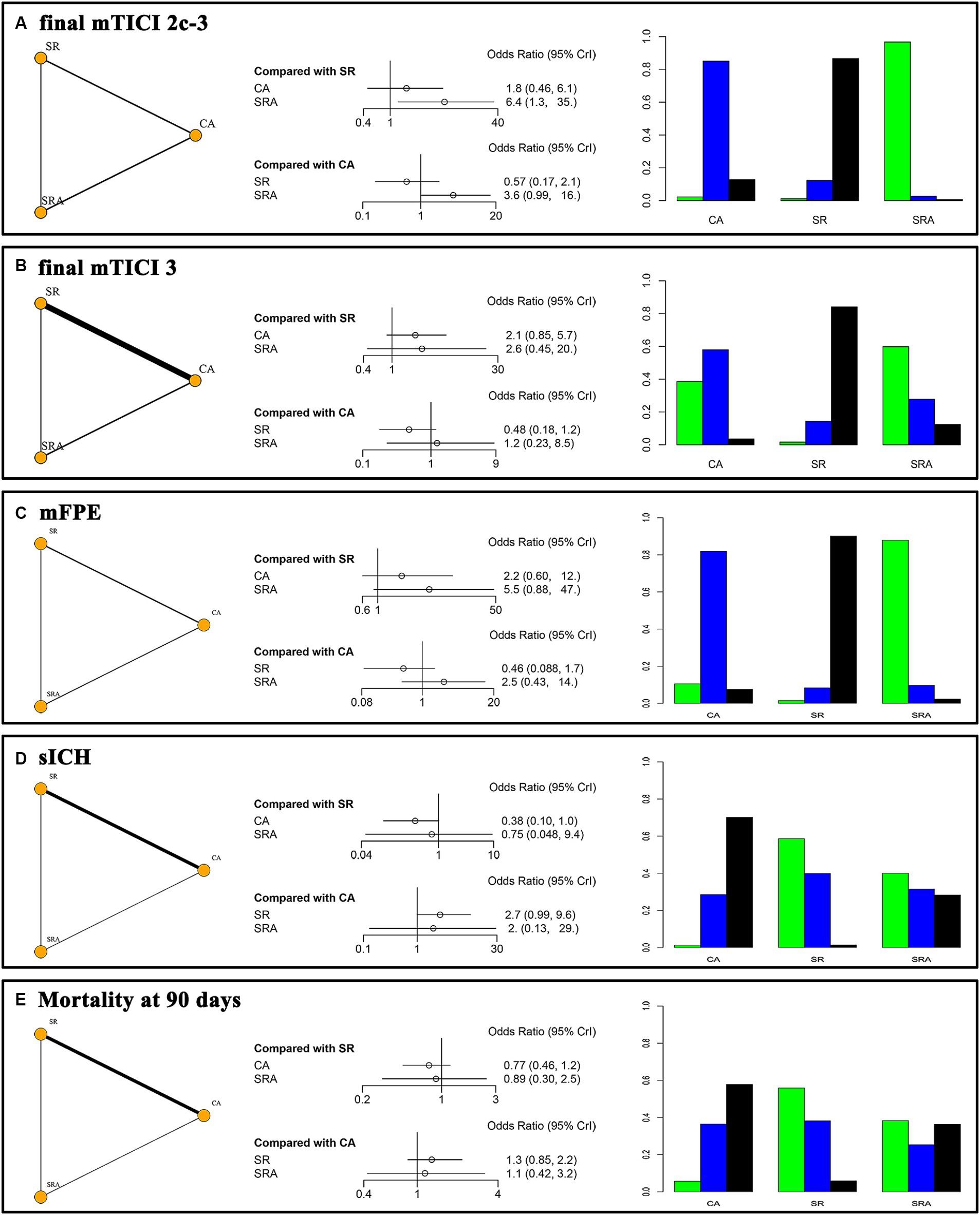
Figure 3. Network plots, forest plots, and rankograms for the secondary outcomes. (A) final mTICI 2c/3; (B) final mTICI 3; (C) mFPE, first pass successful reperfusion; (D) sICH, symptomatic intracranial hemorrhage; (E) mortality at 90 days.
Primary outcomes
Final successful reperfusion and FPE
Both first-line SRA (OR = 3.2, 95% CI 1.4–11.0) and CA (OR = 2.1, 95%CI 1.3–3.7) demonstrated superiority over SR in achieving final mTICI 2b/3 reperfusion. There was no significant difference between first-line SRA and CA (OR = 1.5, 95%CI 0.64–4.7). The SUCRA values for SRA, CA, and SR were 91.1, 58.5, and 0.4%, respectively (Figure 2A). Compared with SR, first-line SRA also showed an advantage in achieving FPE (OR = 4.1, 95%CI 1.3–14.0), while CA did not (OR = 1.8, 95%CI 0.72–4.1). The SUCRA values for SRA, CA, and SR were 97.4, 48.0, and 4.6%, respectively (Figure 2B).
90-day functional independence
Regarding clinical prognosis, the first-line CA strategy was associated with greater functional independence at 90 days compared to SR (OR = 1.4, 95%CI 1.1–1.9). However, there was no significant difference between the SRA technique and either CA (OR = 0.79, 95%CI 0.46–1.3) or SR (OR = 1.1, 95%CI 0.64–1.9). The SUCRA values for SRA, CA, and SR were 42.1, 90.5, and 17.4%, respectively (Figure 2C).
Secondary outcomes
Final excellent, complete reperfusion and mFPE
The first-line SRA strategy demonstrated significantly superior outcomes in achieving final mTICI 2c/3 reperfusion compared to SR (OR = 6.4, 95%CI 1.3–35.0), and it had a better tendency than CA (OR = 3.6, 95%CI 0.99–16.0). The SUCRA values for SRA, CA, and SR were 98.0, 44.7, and 7.2%, respectively (Figure 3A). There were no significant differences among the three first-line strategies regarding achieving final complete reperfusion, with SUCRA values of 73.7, 67.5, and 8.8%, respectively (Figure 3B). Similarly, there were no significant differences in mFPE outcomes among these three techniques, with SUCRA values of 92.8, 51.4, and 5.7%, respectively (Figure 3C).
sICH
The first-line CA strategy was associated with a lower incidence of sICH compared to SR (OR = 0.38, 95%CI 0.1–1.0). However, the SRA technique did not show a significant difference compared to either CA (OR = 2.0, 95%CI 0.13–29.0) or SR (OR = 0.75, 95%CI 0.05–9.4). The SUCRA values for SRA, CA, and SR were 55.9, 15.6, and 78.6%, respectively (Figure 3D).
Mortality
There were no significant differences in mortality at 90 days among the first-line SRA, CA, and SR strategies, with SUCRA values of 51.0, 24.0, and 75.0%, respectively (Figure 3E).
Discussion
This network meta-analysis included 17 observational studies comprising 1,661 cases of acute PCS. The pooled results indicated that the first-line SRA or CA strategies achieved higher rates of final successful reperfusion compared to the SR technique (SUCRA values of 91.1, 58.5, and 0.4%). Additionally, the first-line SRA approach demonstrated advantages in achieving FPE and final excellent reperfusion outcomes compared to the SR technique, while CA did not show such benefits. In terms of the incidence of sICH, the first-line CA strategy had a lower rate compared to SR, whereas no significant difference was observed for SRA (SUCRA values of 15.6, 78.6, and 55.9%). With regard to functional independence at 90 days, the first-line CA strategy appeared to be superior to SR, while SRA did not show a significant difference compared to either CA or SR techniques (SUCRA values of 56.0, 92.0, and 1.9%, respectively).
The present study showed that the first-line CA strategy achieved better final successful reperfusion than SR, which was consistence with the other meta-analysis in for acute PCS (9, 10). However, it was different from the finding in anterior circulation strokes (ACS), for both ASTER (30) and COMPASS trials (31) showing comparable reperfusion outcomes between CA and SR. This discrepancy may be attributed to the straighter characteristics of vertebrobasilar artery. It makes the larger-bore intermediate catheter easier to deliver, and becomes more stable when capture and retriever (32). Besides, SR alone might cause the wiggle of thrombus between the two posterior cerebral arteries, reducing the effectiveness of stentriever. Moreover, CA technique does not require crossing the microguidewire and microcatheter over the thrombus, reducing the risk of vessel perforation and dissection. These factors likely contribute to the efficacy and safety of the CA technique for PCS.
Furthermore, our study favored the first-line SRA strategy in achieving first-pass and final recanalization outcomes compared to SR. On the one hand, the use of an intermediate catheter improved system stability and reduced the difficulty of superselection. On the other hand, the proximal suction of a large-bore catheter could probably improve the reperfusion efficacy of stentriever and reduce the risk of distal embolism. Whereas, this finding was inconsistent with a relevant RCT conducted on ACS, which failed to demonstrate better recanalization outcomes of SRA compared to SR (33). In this RCT study, the use of a balloon-guide catheter was mandatory in SR and SRA groups. Consequently, this difference between PCS and ACS may be attributed to the restricted usage of balloon-guide catheters in PCS cases.
Regarding the comparison between first-line SRA and CA, our study indicated comparable proportions of first-pass and final reperfusion outcomes for PCS. These results differ from the meta-analysis based on ACS (34), which indicated that SRA technique was associated with better recanalization outcomes compared with CA. And this kind of difference could be narrowed due to the advantage of CA in PCS discussed. However, it is worth noting that the first-line SRA strategy appeared to be superior to CA in achieving mFPE (SUCRA 92.8 and 51.4%) and FPE (SUCRA 97.4 and 48.0%). In addition to its better recanalization efficacy, this result might partially be due to the higher incidence of intracranial atherosclerotic stenosis (ICAS) in acute PCS cases. The Angel-ACT registry reported that the underlying ICAS accounted for 54.3% (171/315) of acute PCS patients (35), while only 24.8% (282/1139) in acute ACS (36). And this kind of phenomenon was also observed in the Korean population (37). For patients with underlying ICAS, stent-based strategies showed advantages over CA due to the better integration between thrombectomy devices and clots (38).
The positive correlation between recanalization outcomes and clinical prognosis has been reported (16, 28, 39). However, our meta-analysis did not show a significant difference in functional independence between the first-line SRA strategy and the other two strategies. This could be due to the small sample size of the SRA group. Other factors such as age (17) and baseline NIHSS (17, 23, 39) have also shown predictive value for clinical outcomes, but this information was rarely provided in the included studies.
Limitation
There were several limitations in this study. First, all the included studies were retrospective observational studies with publication and selection bias, potentially leading to unbalanced baseline characteristics among the strategies. Second, the concept of SRA is broad and includes various thrombectomy techniques, such as Solumbra and stent assisted vacuum lock extraction, which may differ in efficacy but were pooled together in our analysis. Third, although the PCS is mainly composed of basilar artery occlusion in this study, the posterior cerebral artery and vertebral artery occlusion were also included, which might increase the heterogeneity. For example, a sub-analysis of the TOPMOST study suggested comparable reperfusion and clinical outcomes between first-line CA and SR for acute P2/3 occlusion (40). Fourth, the safety of the SRA strategy may improve with the use of an intermediate catheter, but this was rarely reported. Only one study provided information on the incidence of symptomatic intracranial hemorrhage, reporting a rate of 5.6% in the SRA group.
Conclusion
Compared to first-line SR, the CA strategy achieved higher rates of final successful reperfusion and 90-day functional independence, as well as a lower incidence of sICH for patients with acute PCS. The reperfusion outcomes after the first pass were comparable between these two strategies. As a combined approach, the recanalization outcomes after the first pass and at the end of the procedure were significantly better than SR, and also showed advantages over CA from the aspect of SUCRA without significant difference. However, the proportion of functional independence and sICH in the first-line SRA group did not exhibit significant differences compared to the other two strategies. Due to the quality limitations of the included studies, these conclusions should be drawn with caution, and further studies are needed.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
GY: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Software, Validation, Writing – original draft. RC: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Writing – original draft. PC: Data curation, Formal analysis, Investigation, Methodology, Software, Writing – review & editing. HW: Funding acquisition, Validation, Writing – review & editing. DW: Validation, Writing – review & editing. MC: Conceptualization, Funding acquisition, Supervision, Validation, Writing – review & editing. ZL: Conceptualization, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the following grants: the project of NINGBO Leading Medical and Health Discipline [2022-F04], the Ningbo Natural Science Foundation [No. 2021 J284], the Ningbo Municipal Bureau of Science and Technology [2021S172], the Ningbo Medical Science and Technology Project [2020Y02].
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2023.1279233/full#supplementary-material
References
1. Schonewille, WJ, Wijman, CA, Michel, P, Rueckert, CM, Weimar, C, Mattle, HP, et al. Treatment and outcomes of acute basilar artery occlusion in the basilar artery international cooperation study (BASICS): a prospective registry study. Lancet Neurol. (2009) 8:724–30. doi: 10.1016/S1474-4422(09)70173-5
2. Mattle, HP, Arnold, M, Lindsberg, PJ, Schonewille, WJ, and Schroth, G. Basilar artery occlusion. Lancet Neurol. (2011) 10:1002–14. doi: 10.1016/S1474-4422(11)70229-0
3. Liu, X, Dai, Q, Ye, R, Zi, W, Liu, Y, Wang, H, et al. BEST trial investigators. Endovascular treatment versus standard medical treatment for vertebrobasilar artery occlusion (BEST): an open-label, randomised controlled trial. Lancet Neurol. (2020) 19:115–22. doi: 10.1016/S1474-4422(19)30395-3
4. Langezaal, LCM, Van der Hoeven, EJR, Mont’Alverne, FJA, Lima, FO, De Carvalho, JJF, Dippel, DWJ, et al. Endovascular therapy for stroke due to basilar-artery occlusion. N Engl J Med. (2021) 384:1910–20. doi: 10.1056/NEJMoa2030297
5. Jovin, TG, Li, C, Wu, L, Wu, C, Chen, J, Jiang, C, et al. BAOCHE investigators. Trial of Thrombectomy 6 to 24 hours after stroke due to basilar-artery occlusion. N Engl J Med. (2022) 387:1373–84. doi: 10.1056/NEJMoa2207576
6. Tao, C, Nogueira, RG, Zhu, Y, Sun, J, Han, H, Yuan, G, et al. ATTENTION investigators. Trial of endovascular treatment of acute basilar-artery occlusion. N Engl J Med. (2022) 387:1361–72. doi: 10.1056/NEJMoa2206317
7. Adusumilli, G, Kobeissi, H, Ghozy, S, Hardy, N, Kallmes, KM, Hutchison, K, et al. Endovascular thrombectomy after acute ischemic stroke of the basilar artery: a meta-analysis of four randomized controlled trials. J Neurointerv Surg. (2022) 2022:019776. doi: 10.1136/jnis-2022-019776
8. Yu, Y, Lou, Y, Cui, R, Miao, Z, Lou, X, and Ma, N. Endovascular treatment versus standard medical treatment for basilar artery occlusion: a meta-analysis of randomized controlled trials. J Neurosurg. (2023) 2023:1–9. doi: 10.3171/2022.12.JNS222490
9. Ye, G, Wen, X, Wang, H, Sun, C, Pan, Z, Chen, M, et al. First-line contact aspiration versus first-line stent retriever for acute posterior circulation strokes: an updated meta-analysis. J Neurointerv Surg. (2022) 14:457–63. doi: 10.1136/neurintsurg-2021-017497
10. Guo, X, Xiong, Y, Huang, X, Pan, Z, Kang, X, Chen, C, et al. Aspiration versus stent retriever for posterior circulation stroke: a meta-analysis. CNS Neurosci Ther. (2023) 29:525–37. doi: 10.1111/cns.14045
11. Moher, D, Shamseer, L, Clarke, M, Ghersi, D, Liberati, A, Petticrew, M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:4053. doi: 10.1186/2046-4053-4-1
12. Higgins, JPT, Thompson, SG, Deeks, JJ, and Altman, DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
13. Son, S, Choi, DS, Oh, MK, Hong, J, Kim, SK, Kang, H, et al. Comparison of solitaire thrombectomy and penumbra suction thrombectomy in patients with acute ischemic stroke caused by basilar artery occlusion. J Neurointerv Surg. (2016) 8:13–8. doi: 10.1136/neurintsurg-2014-011472
14. Mokin, M, Sonig, A, Sivakanthan, S, Ren, Z, Elijovich, L, Arthur, A, et al. Clinical and procedural predictors of outcomes from the endovascular treatment of posterior circulation strokes. Stroke. (2016) 47:782–8. doi: 10.1161/STROKEAHA.115.011598
15. Gerber, JC, Daubner, D, Kaiser, D, Engellandt, K, Haedrich, K, Mueller, A, et al. Efficacy and safety of direct aspiration first pass technique versus stent-retriever thrombectomy in acute basilar artery occlusion-a retrospective single center experience. Neuroradiology. (2017) 59:297–304. doi: 10.1007/s00234-017-1802-6
16. Gory, B, Mazighi, M, Blanc, R, Labreuche, J, Piotin, M, Turjman, F, et al. Mechanical thrombectomy in basilar artery occlusion: influence of reperfusion on clinical outcome and impact of the first-line strategy (ADAPT vs stent retriever). J Neurosurg. (2018) 129:1482–91. doi: 10.3171/2017.7.JNS171043
17. Kang, DH, Jung, C, Yoon, W, Kim, SK, Baek, BH, Kim, JT, et al. Endovascular Thrombectomy for acute basilar artery occlusion: a multicenter retrospective observational study. J Am Heart Assoc. (2018) 7:e009419. doi: 10.1161/JAHA.118.009419
18. Maus, V, Styczen, H, Liman, J, Maier, I, Brehm, A, Tsogkas, I, et al. Intracranial mechanical thrombectomy of large vessel occlusions in the posterior circulation using SAVE. BMC Neurol. (2019) 19:197. doi: 10.1186/s12883-019-1428-x
19. Alawieh, AM, Eid, M, Anadani, M, Sattur, M, Maier, IL, Feng, W, et al. Thrombectomy technique predicts outcome in posterior circulation stroke-insights from the STAR collaboration. Neurosurgery. (2020) 87:982–91. doi: 10.1093/neuros/nyaa179
20. Choi, JW, Han, M, Park, JH, and Jung, WS. Effect of manual aspiration thrombectomy using large-bore aspiration catheter for acute basilar artery occlusion: comparison with a stent retriever system. BMC Neurol. (2020) 20:434. doi: 10.1186/s12883-020-02013-7
21. Baik, SH, Jung, C, Kim, BM, Han, K, and Kim, DJ. Clot Meniscus sign: an angiographic clue for choosing between stent retriever and contact aspiration in acute basilar artery occlusion. AJNR Am J Neuroradiol. (2021) 42:732–7. doi: 10.3174/ajnr.A6988
22. Kaneko, J, Ota, T, Unemoto, K, et al. Endovascular treatment of acute basilar artery occlusion: outcomes, influencing factors and imaging characteristics from the Tama-REgistry of acute thrombectomy (TREAT) study. J Clin Neurosci. (2021) 86:184–9. doi: 10.1016/j.jocn.2020.12.034
23. Monteiro, A, Cortez, GM, Waqas, M, Rai, HH, Baig, AA, Dossani, RH, et al. Comparison of effectiveness and outcomes among different thrombectomy techniques in acute basilar artery occlusion: a dual-center experience. Neurosurg Focus. (2021) 51:E8. doi: 10.3171/2021.4.FOCUS21114
24. Onodera, K, Kurisu, K, Sakurai, J, Wada, H, Takebayashi, S, Kobayashi, T, et al. A direct aspiration first pass technique for vertebra-basilar occlusion: a retrospective comparison to stent retriever. J Stroke Cerebrovasc Dis. (2021) 30:106069. doi: 10.1016/j.jstrokecerebrovasdis.2021.106069
25. Yuan, Z, Yang, Y, Li, J, Luo, Y, Meng, R, Xie, Y, et al. Direct aspiration versus stent-retriever thrombectomy for acute posterior circulation occlusion stroke. Chin J Cerebrovasc Dis. (2021) 18:821–8. doi: 10.3969/j.issn.1672-5921.2021.12.003
26. Bernsen, MLE, Bruggeman, AAE, Brouwer, J, Emmer, BJ, Majoie, CBL, Coutinho, JM, et al. MR CLEAN registry investigators. Aspiration versus stent retriever Thrombectomy for posterior circulation stroke. Stroke. (2022) 53:749–57. doi: 10.1161/STROKEAHA.121.034926
27. Lin, D, Xing, P, Lin, H, Wu, J, Yang, P, Shen, H, et al. Influence of the preferred thrombectomy strategy on vascular recanalization efficiency in the apex of basilar artery occlusion. Chin J Cerebrovasc Dis. (2022) 19:323–30. doi: 10.3969/j.issn.1672-5921.2022.05.005
28. Abdelrady, M, Ognard, J, Cagnazzo, F, Derraz, I, Lefevre, PH, Riquelme, C, et al. RAMBO (revascularization via aspiration or mechanical thrombectomy in basilar occlusion). Frontline thrombectomy strategy and outcome in acute basilar artery occlusion. J Neurointerv Surg. (2023) 15:27–33. doi: 10.1136/neurintsurg-2021-018180
29. Abdelrady, M, Derraz, I, Lefevre, PH, Cagnazzo, F, Gascou, G, Arquizan, C, et al. RAMBO (reperfusion via aspiration or mechanical thrombectomy in basilar occlusion)–investigators group. Negative susceptibility vessel sign might be predictive of complete reperfusion in patients with acute basilar artery occlusion managed with thrombectomy. Eur Radiol. (2023) 33:2593–604. doi: 10.1007/s00330-022-09215-2
30. Lapergue, B, Blanc, R, Gory, B, Labreuche, J, Duhamel, A, Marnat, G, et al. ASTER trial investigators. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion: the ASTER randomized clinical trial. JAMA. (2017) 318:443–52. doi: 10.1001/jama.2017.9644
31. Turk, AS, Siddiqui, A, Fifi, JT, De Leacy, RA, Fiorella, DJ, Gu, E, et al. Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): a multicentre, randomised, open label, blinded outcome, non-inferiority trial. Lancet. (2019) 393:998–1008. doi: 10.1016/S0140-6736(19)30297-1
32. Bernava, G, Rosi, A, Boto, J, Brina, O, Kulcsar, Z, Czarnetzki, C, et al. Direct thromboaspiration efficacy for mechanical thrombectomy is related to the angle of interaction between the aspiration catheter and the clot. J Neurointerv Surg. (2020) 12:396–400. doi: 10.1136/neurintsurg-2019-015113
33. Lapergue, B, Blanc, R, Costalat, V, Desal, H, Saleme, S, Spelle, L, et al. ASTER2 trial investigators. Effect of Thrombectomy with combined contact aspiration and stent retriever vs stent retriever alone on revascularization in patients with acute ischemic stroke and large vessel occlusion: the ASTER2 randomized clinical trial. JAMA. (2021) 326:1158–69. doi: 10.1001/jama.2021.13827
34. Texakalidis, P, Giannopoulos, S, Karasavvidis, T, Rangel-Castilla, L, Rivet, DJ, and Reavey-Cantwell, J. Mechanical Thrombectomy in acute ischemic stroke: a Meta-analysis of stent retrievers vs direct aspiration vs a combined approach. Neurosurgery. (2020) 86:464–77. doi: 10.1093/neuros/nyz258
35. Li, K, Sun, D, Tong, X, Wang, A, Zhang, Y, Ma, G, et al. Incidence, predictors, and impact on outcome of underlying intracranial atherosclerotic disease in acute vertebrobasilar artery occlusion undergoing endovascular therapy: data from ANGEL-ACT registry. Int J Stroke. (2023) 18:856–63. doi: 10.1177/17474930221150111
36. Huo, X, Sun, D, Nguyen, TN, Raynald, R, Jia, B, Tong, X, et al. First-pass effect of mechanical thrombectomy for anterior circulation large vessel occlusion: incidence, predictors, and clinical impact. Insight from the ANGEL-ACT registry. J Neurosurg. (2023) 139:1–8. doi: 10.3171/2023.1.JNS222604
37. Lee, JS, Hong, JM, and Kim, JS. Diagnostic and therapeutic strategies for acute intracranial atherosclerosis-related occlusions. J Stroke. (2017) 19:143–51. doi: 10.5853/jos.2017.00626
38. Kang, DH, Yoon, W, Baek, BH, Kim, SK, Lee, YY, Kim, JT, et al. Front-line thrombectomy for acute large-vessel occlusion with underlying severe intracranial stenosis: stent retriever versus contact aspiration. J Neurosurg. (2019) 132:1202–8. doi: 10.3171/2019.1.JNS182905
39. Mahmoudi, M, Dargazanli, C, Cagnazzo, F, Derraz, I, Arquizan, C, Wacogne, A, et al. Predictors of favorable outcome after endovascular Thrombectomy in MRI: selected patients with acute basilar artery occlusion. AJNR Am J Neuroradiol. (2020) 41:1670–6. doi: 10.3174/ajnr.A6741
40. Meyer, L, Stracke, P, Wallocha, M, Broocks, G, Sporns, P, Piechowiak, EI, et al. Aspiration versus stent retriever Thrombectomy for distal, medium vessel occlusion stroke in the posterior circulation: a subanalysis of the TOPMOST study. Stroke. (2022) 53:2449–57. doi: 10.1161/STROKEAHA.121.037792
Keywords: stroke, posterior circulation, frontline strategy, stent retriever, aspiration, combined technique
Citation: Ye G, Cao R, Chen P, Wang H, Wang D, Chen M and Li Z (2023) Network meta-analysis of first-line thrombectomy strategy for acute posterior circulation strokes: a preliminary evaluation for combined approach. Front. Neurol. 14:1279233. doi: 10.3389/fneur.2023.1279233
Edited by:
Hiroshi Yamagami, Osaka National Hospital (NHO), JapanReviewed by:
Leonard Yeo, National University Health System (Singapore), SingaporeLuis Rafael Moscote-Salazar, Colombian Clinical Research Group in Neurocritical Care, Colombia
Copyright © 2023 Ye, Cao, Chen, Wang, Wang, Chen and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maosong Chen, chenmaosong0416@126.com; Zhenqiang Li, sky13968@163.com
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work
 Gengfan Ye
Gengfan Ye Ruoyao Cao
Ruoyao Cao Pandi Chen1
Pandi Chen1 Hongcai Wang
Hongcai Wang Maosong Chen
Maosong Chen