- 1The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China
- 2Hangzhou Dunen Medical Laboratory Co., Ltd., Hangzhou, China
Objective: Our study aimed to evaluate the influence of methylenetetrahydrofolate reductase (MTHFR) polymorphism on the clinical features and therapeutic effects in patients with migraine.
Methods: The data of 135 patients with migraine were collected from January 2021 to December 2021. The MTHFR C677T polymorphism was analyzed. The pain intensity was evaluated using a numerical rating scale (NRS) during treatment. The levels of folic acid, homocysteine (Hcy), vitamin B12, interleukin-2 (IL-2), IL-4, and ferritin, and changes of NRS were compared between folic acid and conventional treatment groups stratified by different genotypes of MTHFR in migraine patients.
Results: The levels of Hcy and ferritin in male patients were higher than that in female patients (P < 0.05); Compared with CC and CT genotype groups, the TT genotype group showed significantly higher Hcy levels (P < 0.05) and lower folic acid levels (P < 0.05); In both folic acid and conventional treatment groups, a significant decrease in NRS score was observed in different genotypes post-treatment (P < 0.05). Patients with TT genotype in the folic acid treatment group showed better therapeutic efficacy than conventional treatment group (P < 0.05). There is no significant difference in the therapeutic efficacy in other genotypes between the two groups (P > 0.05).
Conclusion: The MTHFR C677T genotyping may provide a new method to guide and optimize individualized medication for migraine patients.
Introduction
Migraine is a chronic, multifactorial neurovascular disease that is typically characterized by recurring and disabling headache attacks, as well as an impaired autonomic nervous system (1). Symptoms associated with migraine include paroxysmal unilateral throbbing pains, nausea, vomiting, photophobia and phonophobia (2). The incidence of migraine is about 15% worldwide, the prevalence rate is 9.3% in China, and the ratio of males to females is about 1:3 (3, 4).
The pathogenesis of migraine is complex and remains unclear. Migraine is a multifactorial disorder with pathogenesis influenced by dietary, psychological, environmental, and genetic factors. Except for symptomatic treatments, no special drugs are available for migraine. The first-line therapeutic drugs for migraine include triptans, non-steroidal anti-inflammatory drugs, antiemetics, and so on. A combination strategy is commonly used to reduce the degree of the headache and control other symptoms; however, it is related to medication-overuse headaches, adverse reactions, and substantial financial burdens (5, 6), so the treatment discontinuation rate is high. Previous studies reported that 66.7% of patients discontinued their medications (7). Therefore, a significant need exists for other effective, safe, and affordable treatments at present.
Methylenetetrahydrofolate reductase (MTHFR) is a crucial enzyme for homocysteine (Hcy) metabolism and regulates Hcy level in vivo, mainly by affecting folic acid absorption and metabolism (8, 9). MTHFR catalyzes the 5,10-methylenetetrahydrofolate into 5-methyltetrahydrofolate (CH3-THF) to provide the carbon in the metabolism process of Hcy. The MTHFR 677C → T polymorphism reduces MTHFR enzyme activity, resulting in hyperhomocysteinemia (HHcy). HHcy has become a well-established healthy risk factor associated with neurological disorders, cognitive decline, and cardiovascular disease. HHcy may increase neuronal excitability and release many headache mediators and other inflammatory factors; finally, it induces migraine (10–12). Supplementation of folic acid can reduce the level of Hcy, which has been used to prevent and treat other diseases related to Hcy (13, 14). Several clinical studies preliminarily suggested that targeted folic acid supplementation for migraine patients can help prevent the onset and treatment of migraine (10, 15). Some people may respond better to folic acid supplementation, but the conclusions are inconsistent (16). The MTHFR 677C → T variant can decrease the activity of MTHFR, reduce the tetrahydrofolate levels intracellularly, increase the folic acid demand, and counteract the folic acid supplement (9). However, limited studies about the influence of MTHFR C677T polymorphism on migraine's clinical features and effects from different treatments have been carried out, such as folic acid. Thus, this article is aimed to determine the role of MTHFR polymorphism in the treatment of migraine and the optimization of individualized medication for migraine patients.
Materials and methods
Study design
This is a retrospective study using the detection of the MTHFR polymorphism to evaluate the efficacy of patients who received treatments for migraine between January 2021 and December 2021 in the First Affiliated Hospital of Zhejiang University (FAHZJ), a hospital located in the Zhejiang province, China. A total of 135 patients diagnosed with migraine by physicians were enrolled in our hospital. Patients received folic acid (5 mg), or conventional drugs for migraine treatment were eligible. Ethical approval was obtained from the authorizing ethics committee of FAHZJ (IIT20220564A). The data were anonymous, and the requirement for informed consent was waived for our retrospective study.
MTHFR genotyping and laboratory testing
Genomic DNA was prepared from peripheral blood samples by cell lysis assay. For each patient, 2 mL of peripheral venous blood was collected with EDTA as an anticoagulant for testing MTHFR C677T genotypes. A test kit (PCR and microarray method, Shanghai Bio Science and Technology Co., Ltd., China) was used to identify the MTHFR C677T genotypes as follows: CC genotype (heterozygous, fast metabolizer), CT genotype (mutant, intermediate metabolizer) and TT genotype (homozygous mutant, slow metabolizer). The serum analytes measured were folic acid, Hcy, ferritin, vitamin B12, interleukin-2 (IL-2), IL-4, IL-6, IL-10, TNF-α, IFN-γ, and IL-17A.
Efficacy assessment
The treatment duration was 1 month. The pain intensity was evaluated using a numerical rating scale (NRS) ranging from 0 to 10. Higher scores indicated greater pain: mild pain (NRS 1–3), moderate pain (NRS 4–6), and severe pain (NRS 7–10). Furthermore, changes in NRS scores were determined by comparing the NRS scores before and after treatment.
Statistical analysis
Data were statistically processed and analyzed by SPSS version 26.0. Measurement data were presented as mean ± standard deviation (SD) and were compared with t-test or One-Way ANOVA. Enumeration data were presented as percentages. A two-tailed P < 0.05 demonstrated statistically significant differences.
Results
Clinical characteristics
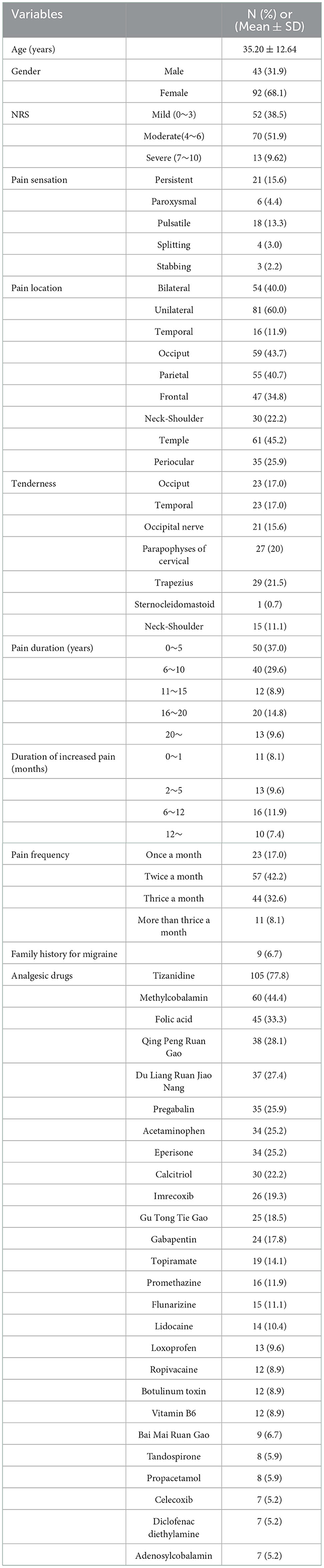
Clinical characteristics are shown in Table 1 and Supplemental Table 1. Among the 135 migraine patients, 43 were males, and 92 were females, ranged from 13 to 69 years old (mean and median age, 35.2 and 34 years old, respectively). Based on gene detection, 35 patients (25.92%) were fast metabolizer (CC genotype), 72 patients (53.33%) were intermediate metabolizer (CT genotype), and 28 patients were (20.74%) slow metabolizer (TT genotype). The conventional drugs used were listed in Table 1 and mainly included non-steroidal anti-inflammatory drugs (acetaminophen, imrecoxib, celecoxib, diclofenac diethylamine), muscle relaxant (tizanidine, eperisone), methylcobalamin, pregabalin, gabapentin, and topiramate.
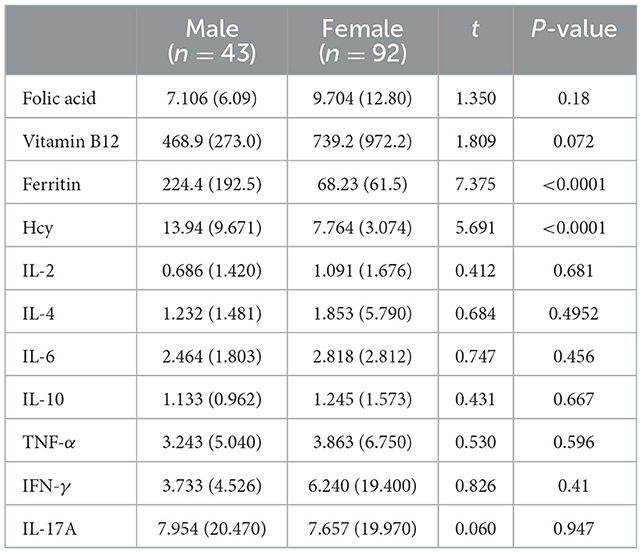
Serum indexes in different genders
Serum indexes are shown in Table 2. Serum levels of Hcy and ferritin were significantly higher in males than those in females (P < 0.05). There was no significant difference between genders on the levels of vitamin B12, IL-2, IL-4, IL-6, IL-10, TNF-α, IFN-γ, and IL-17A (P > 0.05).
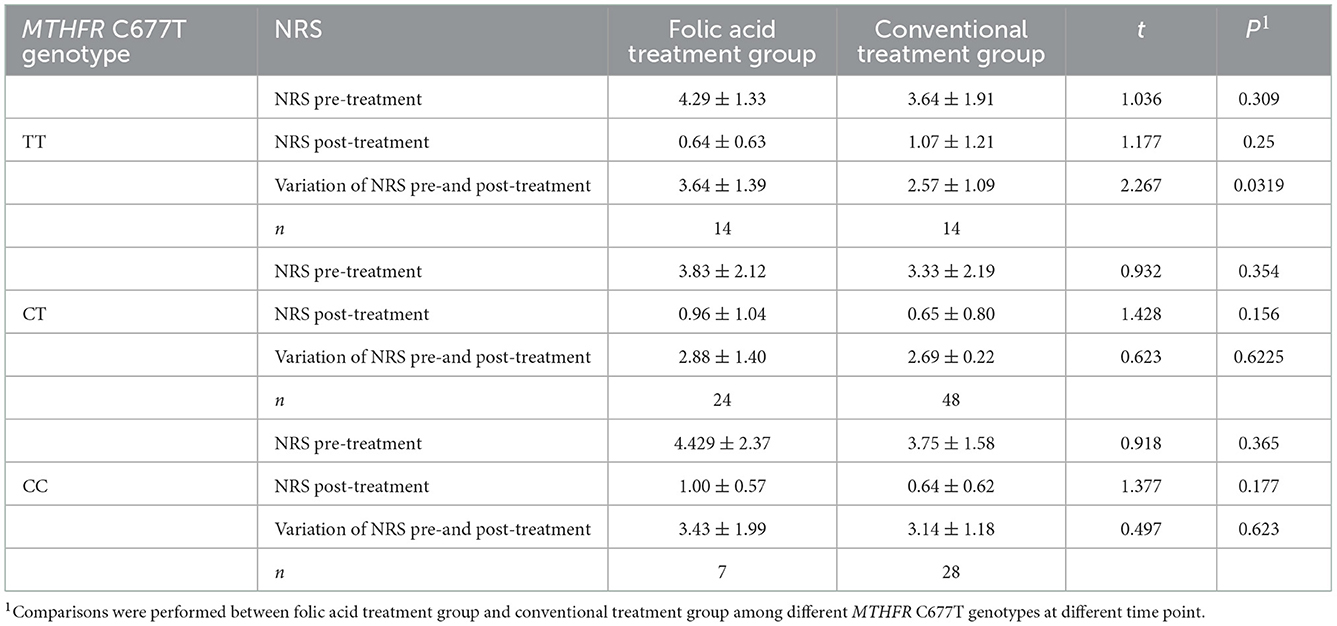
Serum indexes in different genotypes of MTHFR C677T
Summary data are shown in Figure 1 and Table 3. Data analysis showed lower folic acid levels and higher Hcy levels in the TT genotype group (P < 0.05). There was a significant difference in vitamin B12 levels between the CC and CT genotype groups (P < 0.05, Figure 1). No significant difference was found on the levels of ferritin, IL-2, IL-4, IL-6, IL-10, TNF -α, IFN-γ, and IL-17A among the three genotype groups (P > 0.05).
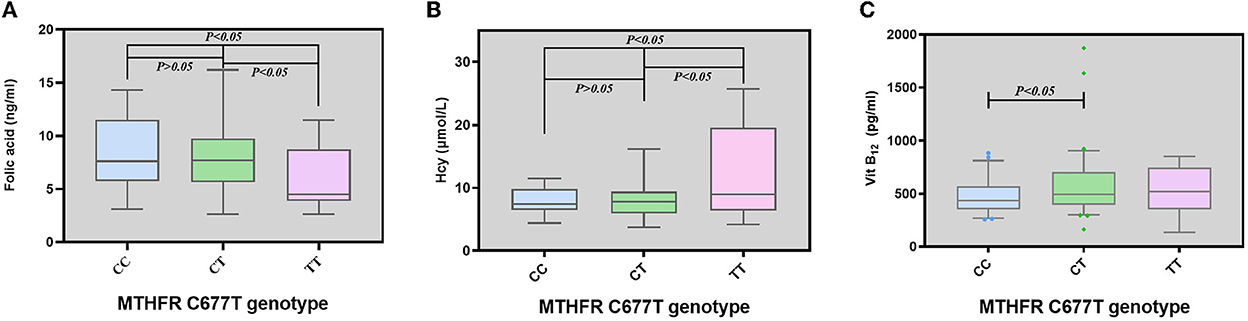
Figure 1. Levels of folic acid, homocysteine, and vitamin B12 among different genotypes of MTHFR in migraine patients. (A) Levels of folic acid among migraine patients with different genotypes of MTHFR. (B) Levels of Hcy among migraine patients with different genotypes of MTHFR. (C) Levels of vitamin B12 among migraine patients with different genotypes of MTHFR. Horizontal lines represent median values, box represent the quartiles, and whiskers represent the range of data.
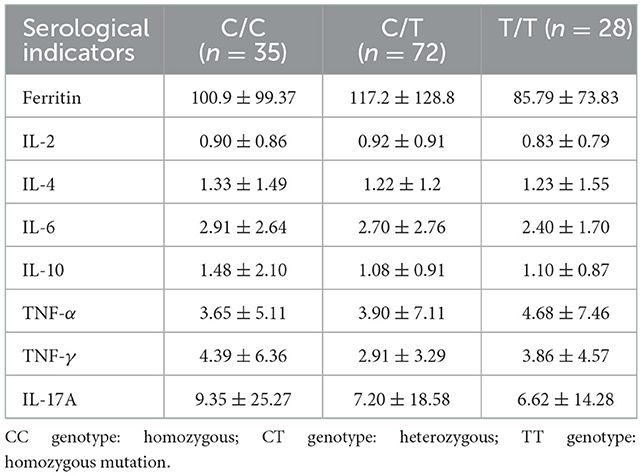
Table 3. Comparison of serological indicators in migraine patients with different MTHFR genotypes (Mean ± SD).
Treatment response by MTHFR C677T genotype
The NRS score variations during treatment are shown in Figure 2 and Table 4. A significant decrease in NRS score was observed post-treatment (P < 0.05). Treatment with folic acid was effective in three genotype groups (P < 0.05). Patients with TT genotype in the folic acid treatment group showed better therapeutic efficacy than conventional treatment group (P < 0.05). There is no significant difference in the therapeutic efficacy in other genotypes between the two groups (P > 0.05).
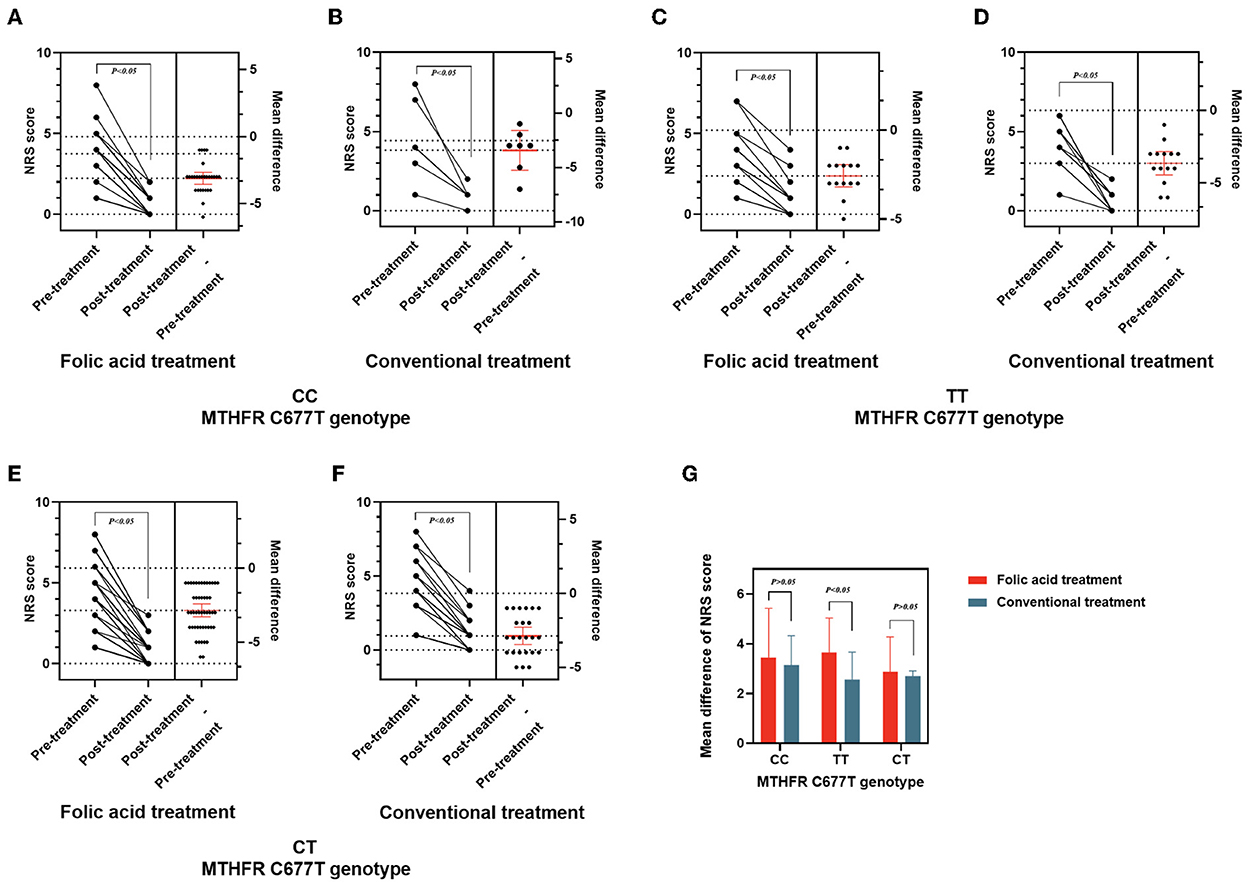
Figure 2. Therapeutic effects for migraine patients with different MTHFR genotypes before and after treatment. (A–F) NRS score and changes of NRS in patients with different genotypes of MTHFR before and after treatment. (G) Mean difference of NRS score between folic acid and conventional treatment groups stratified by different genotypes of MTHFR in migraine patients.
Discussion
Migraine is a neurovascular disorder characterized by recurrent moderate to severe headache, usually near the hemicranial head and often accompanied by vomiting, diarrhea, photophobia, and fear of sound. If one parent has migraine, the children are about 40 percent more likely to have migraine (17). Moreover, while both parents have migraines, the risk of migraine (17) for their children is up to 75%.
The MTHFR enzyme encoded by the MTHFR gene is critical in metabolizing methionine folate. This enzyme reduces 5,10-methylene tetrahydrofolate to 5-methyl tetrahydrofolate (5-MTHF) (8). As a methyl donor, 5-MTHF can maintain the balance of Hcy through the methylation of Hcy in the blood (18). Inadequate consumption of folic acid, or abnormality of the enzymes involved in folic acid metabolism, can lead to decreased levels of folic acid. Thus, the methionine production can be inhibited, resulting in an accumulation of Hcy in the body and HHcy. At the same time, the increased Hcy level contributes to the development of migraine through a series of complex events. A high level of Hcy may impair methylation reactions, which disrupts the normal functions of blood vessels and nerves, inhibit the activity of the cerebral cortex, and decrease local blood flow (19). These reactions can further increase the inflammatory cytokines (such as 5-HT, IL-6, and TNF-α) in cerebral microvascular endothelial cells (20), and finally lead to migraine.
Recently, numerous studies have demonstrated that MTHFR polymorphism is associated with migraine and serum Hcy concentrations (21). The genetic polymorphism of the MTHFR can cause a decrease in MTHFR enzyme activity. Compared with the CC genotype, the CT and the TT genotypes show 65% and 30% of MTHFR enzyme activities, respectively (22). Decreased folic acid levels were observed in patients with the slow metabolism TT genotype. Wang et al. studied the genetic susceptibility of C677T polymorphism to migraine in Asians (23). They suggested that the increase of Hcy may be involved in the pathogenesis of migraine and folic acid, Hcy serum level, and MTHFR polymorphism are related to the occurrence of migraine (23). Some studies showed that the Hcy level in patients with migraine is significantly higher than that of the control group, especially during migraine attacks (24). Our study compared the serum folate and Hcy levels among migraine patients with different genotypes. The result showed that the serum folate levels of patients with slow and intermediate metabolic types were significantly lower than those with fast metabolic types. This result is consistent with the data reported in previous literature about the mechanism of MTHFR enzymes.
The study of Pan et al. showed that (25) the vitamin B12, folic acid, and Hcy levels in the migraine group were negatively correlated, indicating that the elevation of Hcy level may be related to the inducement of migraine and that supplementation of folic acid and vitamin B12 may prevent migraine. Lea et al. (26) suggested that vitamin supplements (2 mg folic acid, 25 mg vitamin B6, and 400 micrograms of vitamin B12 every day) and lower Hcy levels can effectively reduce headache frequency and pain severity in 52 migraine patients with aura. Menon et al. (15) treated 206 migraine patients with vitamin supplements. The results showed that vitamin supplements effectively reduced Hcy levels and headache severity in migraine patients. The C allele of the MTHFR C677T variant has more reductions in Hcy levels and migraine pain severity compared with the TT genotype. Stratified analysis by the genotype of the vitamin treatment group, MTHFR genotype variation affects the therapeutic effect of migraine patients. In our study, migraine patients with CT and TT genotype were divided into a folic acid treatment group and a conventional treatment group. Our results showed that NRS decreased after treatment, with significant differences in numerical values of NRS before and after treatment. The pain and symptoms of migraine patients with the TT genotype were significantly relieved after treatment with folic acid supplementation. Besides, the curative effect of the TT genotype group treated with folic acid supplementation was better than that of conventional treatment group (P < 0.05). Fourteen migraine patients with high Hcy had a noticeable curative effect after taking medicine for 1 month. The doctors used folic acid and methylcobalamin to treat migraine the first time and then adjusted the treatment regimen until the above indexes returned to normal range according to the levels of folic acid, vitamin B12, and Hcy in serum. Meanwhile, the patients should pay attention to eating more foods rich in folic acid in their diet. After treatment, the patients' headache was significantly relieved, suggesting that the MTHFR C677T genotyping has a particular clinical value in guiding the individualized treatment of migraine. Apart from this, it affirms the curative effect of folic acid supplementation on migraine patients with high Hcy.
Some limitations still existe. In our study, 35 patients (25.92%) were fast metabolizer (CC genotype), 72 patients (53.95%) were intermediate metabolizer (CT genotype), and 28 patients were (20.74%) slow metabolizer (TT genotype). The result seems different from the data reported in public databases (27). However, in Chinese populations, geographical and ethnic variations were observed in MTHFR C677T genotypes. In a large sample that pooled the results of epidemiological studies on the distributions of MTHFR C677T genotypes in healthy populations living in Mainland China, the mean frequency of 677TT genotype was 20% (95% confidence interval: 18–23%) (28). The frequency of the 677T allele ranged from 24.0% in Hainan province and 63.1% in Shangdong province. Thus, the polymorphic distribution of MTHFR C677T in our study is within the reported range in previous studies among the Chinese population (28). In addition, this sample size of our study is relatively small, so potential confounders to migraine (such as age distribution, sex percentage, and pain duration) were not further checked via multivariate logistic regression. Therefore, the results of this study also need to be further verified with a well-designed and large sample study. In summary, this study has provided valuable information from real-world clinical practices about individualized medication for migraine treatments.
Conclusion
In conclusion, MTHFR polymorphism may be beneficial to guide and optimize individualized medication for migraine treatments. In the future, the relationship between MTHFR polymorphism and migraine treatment can be further studied in larger sample populations with a well-controlled experimental design, especially for vitamin B supplementation.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the First Affiliated Hospital of Zhejiang University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
Conception and design: JG, YR, and XH. Provision of study materials or patients: XH, NC, and RW. Collection and assembly of data: ZF, KL, and JJ. Data analysis and interpretation: KL. All authors contributed to the writing and final approval of manuscript.
Funding
This study was supported by the project of the Zhejiang Pharmaceutical Association (2019ZYYG02).
Conflict of interest
JJ was employed by Hangzhou Dunen Medical Laboratory Co., Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2022.1074857/full#supplementary-material
References
1. Xuejun S, Bifa F, You W, Daying Z, Yan L, Jisheng H, et al. revision of IASP definition of pain. Chin J Pain Med. (2020) 26:641–4. doi: 10.3969/j.issn.1006-9852.2020.09.001
2. De Felice M, Ossipov MH, Wang R, Dussor G, Lai J, Meng ID, et al. Triptan-induced enhancement of neuronal nitric oxide synthase in trigeminal ganglion dural afferents underlies increased responsiveness to potential migraine triggers. Brain. (2010) 133:2475–88. doi: 10.1093/brain/awq159
3. Shunwei L, Yansheng L. ruozhuo L, Xiangyang Q, Qi W, Xiaosu Y, et al. The Chinese guidelines for the diagnosis and treatment of migraine. Chin J Pain Med. (2011) 17:65–86. doi: 10.3969/j.issn.1006-9852.2011.02.001
4. Vos T, Lim SS, Bisignano C, Cruz J, Mirzaei-Alavijeh M. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019—a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
5. Archibald N, Lipscomb J, McCrory DC, AHRQ. Technical Reviews. Resource Utilization and Costs of Care for Treatment of Chronic Headache. Rockville, MD: Agency for Health Care Policy and Research (US). (1999).
6. Wells RE, O'Connell N, Pierce CR, Estave P, Penzien DB, Loder E, et al. Effectiveness of mindfulness meditation vs headache education for adults with migraine: a randomized clinical trial. JAMA Intern Med. (2021) 181:317–28. doi: 10.1001/jamainternmed.2020.7090
7. Hepp Z, Dodick DW, Varon SF, Chia J, Matthew N, Gillard P, et al. Persistence and switching patterns of oral migraine prophylactic medications among patients with chronic migraine: a retrospective claims analysis. Cephalalgia. (2017) 37:470–85. doi: 10.1177/0333102416678382
8. van der Pol KH, Nijenhuis M, Soree B, de Boer-Veger NJ, Buunk AM, Guchelaar HJ, et al. Dutch pharmacogenetics working group guideline for the gene-drug interaction of ABCG2, HLA-B and Allopurinol, and MTHFR, folic acid and methotrexate. Eur J Hum Genet. (2022) 1–8. doi: 10.1038/s41431-022-01180-0. [Epub ahead of print].
9. Shaik MM, Gan SH. Vitamin supplementation as possible prophylactic treatment against migraine with aura and menstrual migraine. Biomed Res Int. (2015) 469529. doi: 10.1155/2015/469529
10. Askari G, Nasiri M, Mozaffari-Khosravi H, Rezaie M, Bagheri-Bidakhavidi M, Sadeghi O. The effects of folic acid and pyridoxine supplementation on characteristics of migraine attacks in migraine patients with aura: a double-blind, randomized placebo-controlled, clinical trial. Nutrition. (2017) 38:74–9. doi: 10.1016/j.nut.2017.01.007
11. Liu L, Yu Y, He J, Guo L, Li H, Teng J. Effects of MTHFR C677T and A1298C polymorphisms on migraine susceptibility: a meta-analysis of 26 studies. Headache. (2019) 59:891–905. doi: 10.1111/head.13540
12. Tietjen GE, Collins SA. Hypercoagulability and migraine. Headache. (2018) 58:173–83. doi: 10.1111/head.13044
13. Chen H, Liu S, Ge B, Zhou D, Li M, Li W, et al. Effects of folic acid and vitamin b12 supplementation on cognitive impairment and inflammation in patients with alzheimer's disease: a randomized, single-blinded, placebo-controlled trial. J Prev Alzheimers Dis. (2021) 8:249–56. doi: 10.14283/jpad.2021.22
14. Chen H, Liu S, Ji L, Wu T, Ji Y, Zhou Y, et al. Folic acid supplementation mitigates alzheimer's disease by reducing inflammation: a randomized controlled trial. Mediators Inflamm. (2016) 5912146. doi: 10.1155/2016/5912146
15. Menon S, Lea RA, Roy B, Hanna M, Wee S, Haupt LM, et al. Genotypes of the MTHFR C677T and MTRR A66G genes act independently to reduce migraine disability in response to vitamin supplementation. Pharmacogenet Genom. (2012) 22:741–9. doi: 10.1097/FPC.0b013e3283576b6b
16. Di Rosa G, Attinà S, Spanò M, Ingegneri G, Sgrò DL, Pustorino G, et al. Efficacy of folic acid in children with migraine, hyperhomocysteinemia and MTHFR polymorphisms. Headache. (2007) 47:1342–4. doi: 10.1111/j.1526-4610.2007.00932.x
17. Yang Y, Ligthart L, Terwindt GM, Boomsma DI, Rodriguez-Acevedo AJ, Nyholt DR. Genetic epidemiology of migraine and depression. Cephalalgia Int J Headache. (2016) 36:1097–25. doi: 10.1177/0333102416638520
19. Shiyin Z. Change of plasma homocysteine in migraine patients. Clin J Med Officers. (2002) 30:3. doi: 10.3969/j.issn.1671-3826.2002.01.007
20. Feng G, Zhanxiu R, Qiu H, Shanshan S, Meixi J. The contents and correlation studies of HCY and CRP in plasma of migraine in attack stage. J Apoplexy Nervous Dis. (2015) 32:3.
21. Shuowen W. Prevention of folate deficiency with 5-methyl-tetrahydrofolate. Int J Pediatr. (2020) 47:4. doi: 10.3760/cma.j.issn.1673-4408.2020.10.011
22. van der Put NMJ, Gabreels F, Stevens EMB, Smeitink JAM, Trijbels FJM, Eskes T, et al. A second common mutation in the methylenetetrahydrofolate reductase gene: An additional risk factor for neural-tube defects? Am J Hum Genet. (1998) 62:1044–51. doi: 10.1086/301825
23. Min W, Xiaobin C, Jing L. Gang L. MTHFR gene C677T polymorphism and migraine suscepitibility among Asian populations: a meta analysis Chongqing Med. (2020) 49:6. doi: 10.3969/j.issn.1671-8348.2020.12.024
24. Lippi G, Mattiuzzi C, Meschi T, Cervellin G, Borghi L. Homocysteine and migraine. A narrative review. Clin Chim Acta. (2014) 433:5–11. doi: 10.1016/j.cca.2014.02.028
25. Yan P. The clinical significance of change of serum Hcy in patients with migraine. Chin J Tissue Eng Res. (2004) 8:92–3. doi: 10.3321/j.issn:1673-8225.2004.01.047
26. Lea R, Colson N, Quinlan S, Macmillan J, Griffiths L. The effects of vitamin supplementation and MTHFR (C677T) genotype on homocysteine-lowering and migraine disability. Pharmacogenet Genom. (2009) 19:422. doi: 10.1097/FPC.0b013e32832af5a3
27. Sherry ST. Kholodov M, Baker J, Phan L, Smigielski EM, Sirotkin K. dbSNP: the NCBI database of genetic variation. Nucleic Acids Res. (2001) 29:308–11. doi: 10.1093/nar/29.1.308
Keywords: migraine, folic acid, individualized medicine, MTHFR polymorphism, therapeutic efficacy
Citation: Guo J, Hao X, Wang R, Lian K, Jiang J, Chen N, Feng Z and Rao Y (2022) MTHFR polymorphism's influence on the clinical features and therapeutic effects in patients with migraine: An observational study. Front. Neurol. 13:1074857. doi: 10.3389/fneur.2022.1074857
Received: 20 October 2022; Accepted: 08 December 2022;
Published: 23 December 2022.
Edited by:
Shizhang Ling, The First Affiliated Hospital of Wannan Medical College, ChinaCopyright © 2022 Guo, Hao, Wang, Lian, Jiang, Chen, Feng and Rao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuefeng Rao,  raoyf@zju.edu.cn
raoyf@zju.edu.cn
†These authors have contributed equally to this work
 Jianhao Guo1†
Jianhao Guo1† Zhiying Feng
Zhiying Feng Yuefeng Rao
Yuefeng Rao