Better oral hygiene is associated with a reduced risk of cataract: A nationwide cohort study
- 1Department of Oral and Maxillofacial Surgery, Mokdong Hospital, College of Medicine, Ewha Womans University, Seoul, South Korea
- 2Department of Neurology, Seoul Hospital, College of Medicine, Ewha Womans University, Seoul, South Korea
Objective: To investigate the association of oral health status and oral hygiene behaviors with cataract occurrence longitudinally.
Materials and methods: Based on the National Health Screening cohort database of Korea, participants who underwent oral health screening by dentists in 2003 were included. Cataract was defined as two or more claims of disease classification for the International Classification of Diseases-10 (E10.34, E11.34, E12.34, E13.34, E14.34, H25, and H26) with cataract specific treatment or surgery procedure claim codes. The occurrence of cataract was analyzed with Cox proportional hazard model according to the presence of periodontitis and oral health examination findings, including missing teeth, caries, tooth brushing, and dental scaling.
Results: Overall, 103,619 subjects were included. During a median follow-up of 12.2 years, cataract developed in 12,114 (11.7%) participants. Poor oral health status such as the presence of periodontitis (adjusted hazard ratio [HR] 1.08, 95% CI [confidence interval] 0.99–1.17, p = 0.088) and increased number of missing teeth (adjusted HR = 1.74, 95% CI = 1.55–1.96, p < 0.001) was associated with the increased cataract risk. Better oral hygiene behaviors such as increased frequency of tooth brushing (adjusted HR = 0.84, 95% CI = 0.79–0.88, p < 0.001) and performed dental scaling within 1 year (adjusted HR = 0.90, 95% CI = 0.86–0.94, p < 0.001) were negatively associated with cataract occurrence.
Conclusion: Periodontitis and increased number of missing teeth may increase the risk of cataract. However, maintaining good oral hygiene through tooth brushing and dental scaling may reduce the risk of future cataract occurrence. Further studies should be performed to confirm the association between chronic oral inflammation and cataract.
Introduction
Poor oral health conditions such as periodontitis, dental caries, or multiple tooth loss are common conditions in humans (1, 2). Poor oral health not only adversely affects oral health itself but also shows a systematic association with or triggers the occurrence of various diseases (3, 4). For example, periodontitis not only causes local inflammation in the oral cavity but also triggers systemic inflammatory consequences. Furthermore, missing tooth and caries are associated with the risk of various systemic diseases, such as diabetes, cardiovascular disease, certain cancers, and neurodegenerative diseases (1, 4–8).
Cataract is a cloudy area of the crystalline lens inside the eye, leading to a decrease in vision. Cataracts affect approximately 95 million people worldwide and remain the major cause of blindness in middle-income and low-income countries (9). The potential risk factors for cataract are aging, dyslipidemia, diabetes mellitus, and hypertension (10). Inflammatory reaction and cascade play an important role in cataract development at a cellular level (9, 11). Because oral health conditions such as periodontitis, tooth loss, and dental caries are closely related to this systemic inflammation, oral health may be linked to cataract occurrence (12–14). Moreover, a decreased inflammatory reaction following good oral hygiene or behavior can reduce the risk of cataract occurrence (12). However, few related studies have described the association of oral health status with cataract.
We hypothesized that poor oral health would be related to the increased risk of cataract occurrence, and better oral hygiene behavior would be related with a reduced risk of cataract occurrence. Therefore, this study aimed to investigate the association of oral health examination estimates with cataract development longitudinally in a nationwide cohort database.
Materials and methods
Data source
The National Health Insurance Service-National Health Screening (NHIS-HEALS) cohort database of Korea was used in this study. The NHIS is administered and supported by the Korean government. As the sole insurance provider in Korea, it covers nearly 97% of Koreans. The remaining 3% of the population is supported by the Medical Aid program, which is administered by the NHIS (15). Subscribers of the NHIS are recommended to receive standardized health screening every 1–2 years. The NIHS-HEALS cohort consists of a database of approximately 510,000 random individuals aged 40–79 years and who participated in health screenings, representing 10% of the total population (16). The cohort database contains individual health screening information, including weight, height, blood pressure, and laboratory tests. It also includes the claims database of diagnosis, prescription, and treatment as well as demographic and socioeconomic information. During health screening, questionnaires on lifestyle, which include oral hygiene behaviors such as frequency of tooth brushing or dental visit within a year, are collected. It also includes oral health examination by a dentist, who examined dental problems such as the number of dental caries or missing teeth. This study was approved by the human subjects ethics board of Ewha Womans University College of Medicine (2020-08-018).
Study population
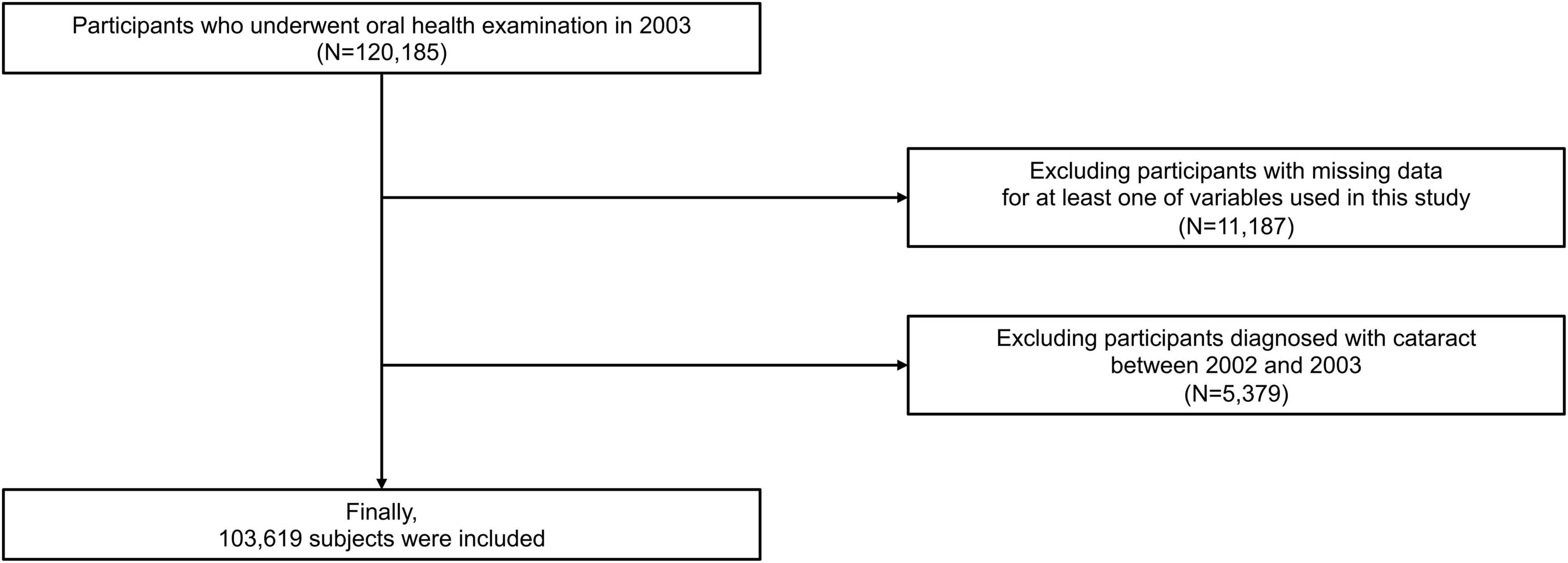
From the NHIS-HEALS database, subjects who underwent oral health screening in 2003 were included (n = 120,185). Participants (n = 11,187) were excluded when data on at least one variable of interest were missing. Participants (n = 5,379) with a history of cataract (International Classification of Diseases (ICD)-10 codes E10.34, E11.34, E12.34, E13.34, E14.34, H25, and H26) between January 2002 and December 2003 were excluded. Thus, 103,619 participants were analyzed in this study (Figure 1).
Definition and variables
The date of oral health examination was set as the index date. The following baseline characteristics on the index date were collected: age, sex, household income, and body mass index. Information on smoking habits (non-smoker, former smoker, and current smoker), alcohol consumption (frequency per week), and regular physical exercise (frequency per week) was obtained using questionnaires. Comorbidities were identified via the following criteria: between January 2002 and index date. Hypertension was defined in patients when they satisfied one of the following criteria: (1) at least one claim of diagnostic codes (ICD-10 I10–15) with the prescription of an antihypertensive agent, (2) two or more claims of diagnostic codes (ICD-10 I10–15), (3) systolic/diastolic blood pressure ≥140/90 mmHg, or 4) self-reported hypertension in the questionnaire. Diabetes mellitus was defined in patients when they met one of the following criteria: (1) at least one claim of diagnostic codes (ICD-10 E11–14) with the prescription of an antidiabetic agent, (2) two or more claims of diagnostic codes (ICD-10 E11–14), (3) fasting serum glucose level ≥7.0 mmol/L, or (4) self-reported diabetes mellitus in the questionnaire. Dyslipidemia was defined when patients satisfied one of the following criteria: (1) at least one claim of diagnostic codes (ICD-10 E78) with the prescription of a dyslipidemia-related agent, (2) two or more claims of diagnostic codes (ICD-10 E78), and (3) total cholesterol ≥240 mg/dl. Atrial fibrillation was defined as two or more claims of diagnostic code (ICD-10 I48). Renal disease was defined as two or more claims of diagnostic codes (ICD-10 N17-19, I12-13, E082, E102, E112, and E132) or estimated glomerular filtration rate of less than 60 ml/min/1.73 m2.
The presence of periodontitis was defined according to the following criteria between January 2002 and the index date: (1) two or more claims of ICD-10 codes K052–054 (acute periodontitis [K052], chronic periodontitis [K053], and periodontitis [K054]) with at least one claim of related treatment codes (Supplementary Table 1) or (2) positive checking of a periodontal pocket by a dentist upon oral health examination. The number of missing tooth and dental caries was assessed by a dentist upon oral health examination. The number of dental caries was classified as 0, 1–5, and ≥6 and the number of missing teeth was categorized as 0, 1–7, 8–14, and ≥15 without considering the cause (1, 17). Oral hygiene behaviors were collected as self-reported data during oral health examination: the frequency of tooth brushing per day, dental visit for any reason within the previous year, and dental scaling within the previous year were included.
Study outcomes
The main outcome was cataract occurrence. Cataract was defined as two or more claims of disease classification for ICD-10 codes (E10.34, E11.34, E12.34, E13.34, E14.34, H25, and H26) with cataract-specific treatment or surgical procedure claim codes. The Korean Electronic Data Interchange codes for cataract treatment were (1) phacoemulsification (S5119), (2) extracapsular or intracapsular cataract extraction (S5111), (3) secondary intraocular lens implantation (S5116), and (4) primary intraocular lens implantation (S5117). Subjects with at least one claim of the following claim codes was not considered as cataract development to exclude false-positive cases: (1) retained magnetic intraocular foreign body (H446), (2) retained nonmagnetic intraocular foreign body (H447), (3) trabeculectomy (S5043), (4) microscopic trabeculotomy (S5047), (5) glaucoma implant insertion (S5049), (6) limited vitrectomy (S5122), and (7) complete vitrectomy (S5121). The follow-up period was from the index date to the occurrence of cataract, the death of a subject, or December 2015, whichever occurred first.
Statistical analysis
A chi-square test and an independent t-test were, respectively, used for categorical and continuous variables to compare the baseline characteristics of groups. Categorical and continuous variables were expressed as numbers (percentages) and means ± standard deviations (SDs), respectively. Kaplan–Meier survival curves were used to evaluate the association of oral health status and oral hygiene behaviors with the incident cataract risk, and a log-rank test was performed to compare the survival curves. The number of cataract cases was divided by the sum of person-years to estimate cataract incidence. Cox’s proportional hazard regression was performed to determine the hazard ratio (HR) with 95% confidence interval (CI) to determine the risk for cataract development in relation to oral health status and oral hygiene behaviors. A multivariable regression model was constructed with adjustment for age, sex, body mass index, household income, alcohol consumption, smoking status, regular physical activity, comorbidities (hypertension, diabetes mellitus, dyslipidemia, atrial fibrillation, and renal disease). The oral health parameters were adjusted in multivariable analysis separately because of multicollinearity. Schoenfeld’s residuals were used to test the assumption of the proportionality of hazards. No violation of the proportional hazard assumption was observed. Data were statistically analyzed using the SAS software (version 9.2, SAS Institute, Cary, NC), and all values were considered statistically significant when p < 0.05.
Results
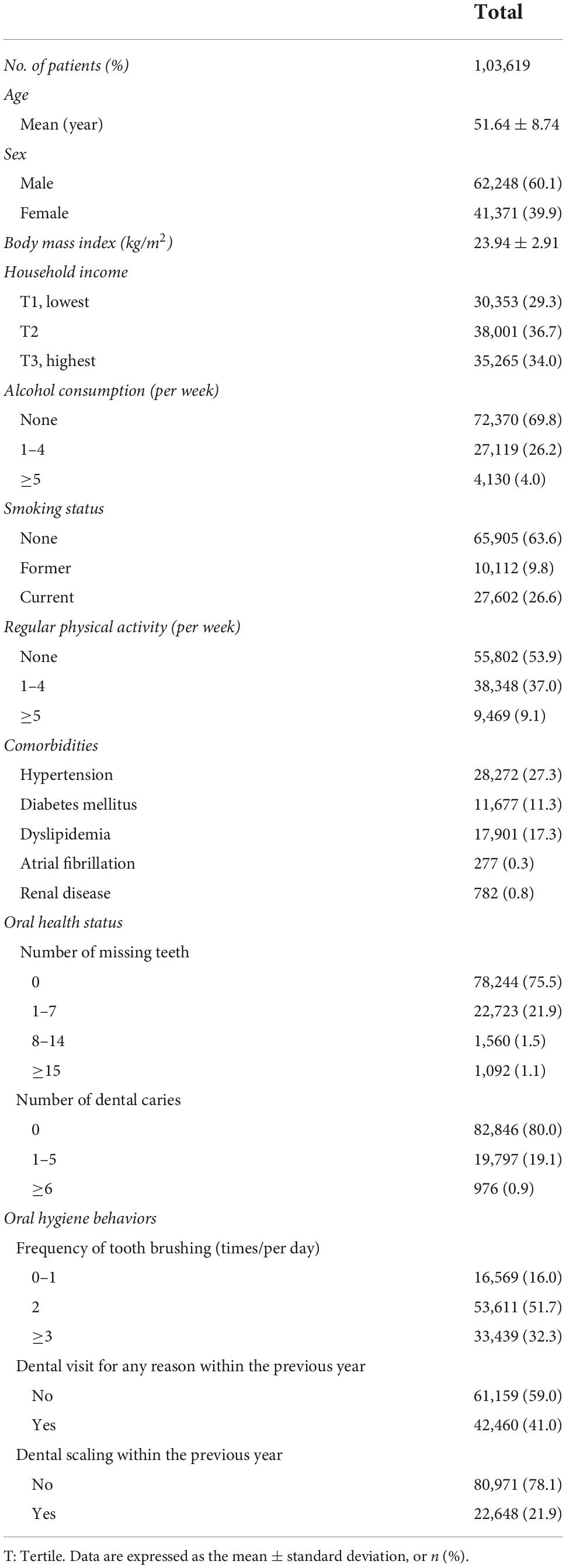
Among 103,619 participants, the included participants had an average age of 51.64 ± 8.74 years, and 60.1% of them were male. Among them, 1,092 (1.1%) participants had more than 15 missing teeth, 976 (0.9%) participants had 6 or more caries, and 33,439 (32.3%) participants brushed their teeth more than thrice a day (Table 1). Comparative analysis of the baseline characteristics is shown in Supplementary Table 2.
During the median follow-up of 12.2 years (interquartile range of 12.1–12.5 years), cataract developed in 12,114 (11.7%) participants. Figure 2 shows the Kaplan–Meier survival curves free from cataract according to oral health status and oral hygiene behaviors. The risk for incident cataract was higher when the participants had periodontitis and a higher number of missing teeth (p < 0.001). Better oral hygiene behaviors, namely, increased frequency of daily tooth brushing and a history of dental scaling within the previous year, were also associated with a reduced occurrence of cataract (p < 0.001). However, a history of dental visit for any reason was not a factor that increased or decreased the risk for cataract (p = 0.739).
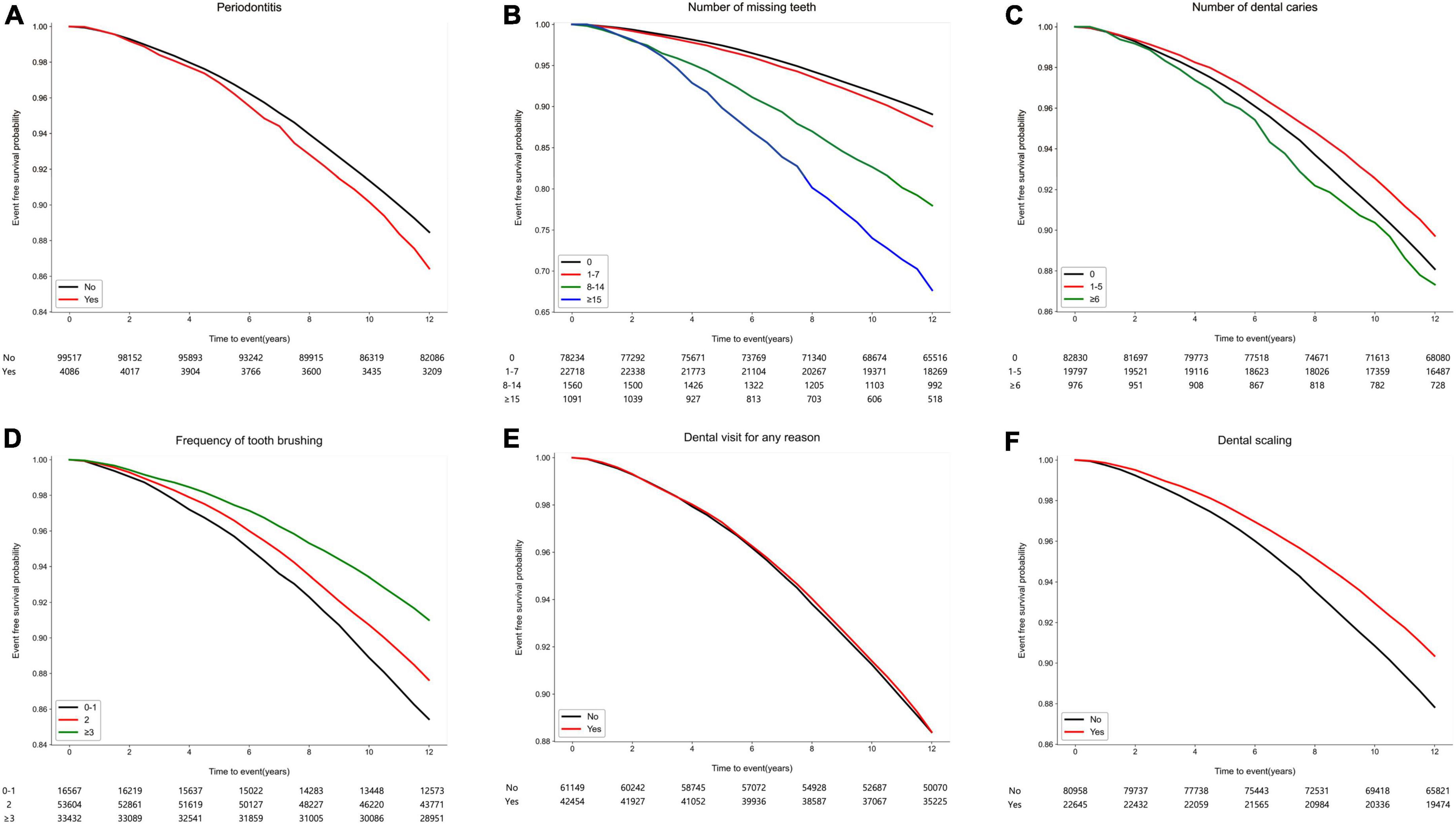
Figure 2. Kaplan–Meier survival curves free from cataract according to oral health status and oral hygiene behaviors. (A) Periodontitis (p < 0.001). (B) Number of missing teeth (p < 0.001). (C) Number of dental caries (p < 0.001). (D) Frequency of tooth brushing (times/per day) (p < 0.001). (E) Dental visit for any reason within the previous year (p = 0.739). (F) Dental scaling within the previous year (p < 0.001).
Although periodontitis was positively correlated with the occurrence of incident cataract in univariable analysis (Supplementary Table 3), the significance of this correlation decreased in multivariable analysis (adjusted HR = 1.08, 95% CI = 0.99–1.17, p = 0.088) (Table 2). The number of missing teeth was associated with an increased risk for cataract occurrence. The following adjusted HRs (in reference to the subject with no missing teeth) were obtained: 1.31 (95% CI = 1.17–1.47, p < 0.001) for participants with 8–14 missing teeth, and 1.74 (95% CI = 1.55–1.96, p < 0.001) for participants with more than 15 missing teeth. Furthermore, the increased frequency of tooth brushing was negatively correlated with cataract occurrence. In reference to the participants who brushed their teeth less than once a day, the subjects who brushed their teeth twice a day (adjusted HR = 0.94, 95% CI = 0.89–0.98, p = 0.008) and more than thrice a day (adjusted HR = 0.84, 95% CI = 0.79–0.88, p < 0.001) had a decreased risk for incident cataract. Moreover, those who received dental scaling within one year showed a significantly lower risk for cataract (adjusted HR = 0.90, 95% CI = 0.86–0.94, p < 0.001). In contrast, the number of dental caries was not a factor associated with the increased risk for cataract. In addition, dental visit history for any reason was not a factor reducing the risk for cataract.
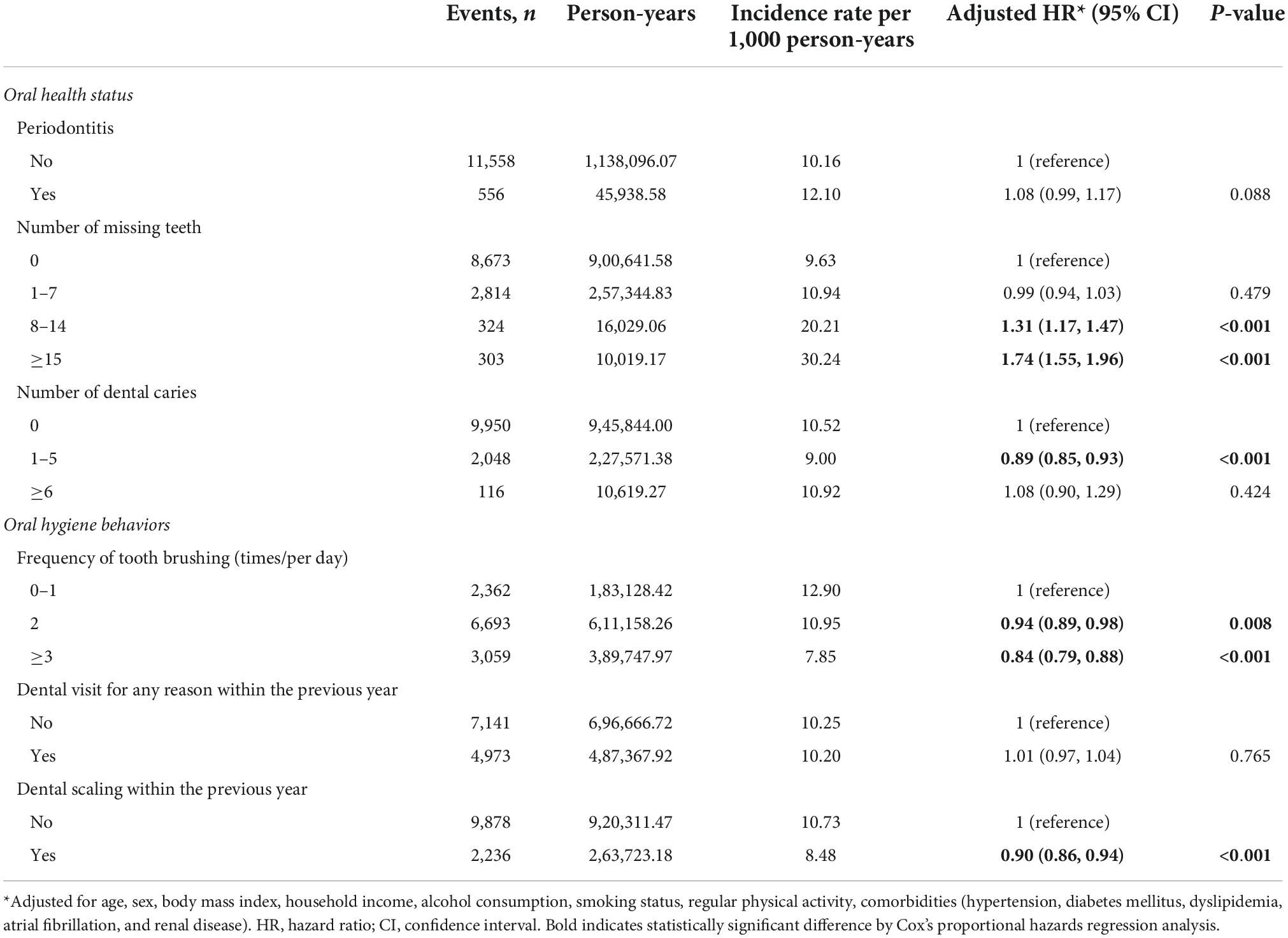
Table 2. The risk for occurrence of cataract according to oral health status and oral hygiene behaviors.
Discussion
The key findings of our study demonstrated that poor oral health status such as the presence of periodontitis and an increased number of missing teeth was associated with an increased risk of cataract occurrence. Conversely, better oral hygiene behaviors such as higher frequency of tooth brushing and a history of dental scaling were associated with a decreased risk of cataract occurrence. Recent evidence has indicated that chronic oral inflammation and infection lead to systemic inflammatory consequences and are associated with various systemic diseases. Periodontitis, a common oral inflammatory disease, increases the risk for cardiovascular diseases and diabetes (18–20). Tooth loss, an indicator of poor oral health status, is also associated with the increased risk for cardiovascular diseases (17, 21) and hypertension (22, 23). Conversely, an increased frequency of tooth brushing, a behavior that lowers oral inflammation, reduces the risk for stroke, (7) atrial fibrillation, and heart failure (1). In contrast to these reports, studies have rarely reported the association of oral health with cataract. Previous studies also suggested the potential relationship between periodontitis and eye diseases (24, 25). The development and progression of ocular diseases, such as glaucoma (26), age-related macular degeneration (27), and diabetic retinopathy (28), are likely affected by periodontitis. Moreover, limited evidence supports the effect of periodontitis or oral hygiene on cataract occurrence. In a retrospective study that evaluated the risk for cataract in subjects with and without periodontitis by referring to the national health insurance research database of Taiwan, subjects with periodontitis have a higher risk for cataract development than those without periodontitis (29). Considering these previous and our research results, our findings were meaningful because they showed that tooth loss, frequent tooth brushing, and dental scaling were associated with the risk of cataract occurrence. Furthermore, our results suggested that the control of periodontitis and chronic oral inflammation through prophylactic dental scaling and good oral hygiene behaviors could reduce the risk of future cataract occurrence.
Although the direct causal relationship between poor oral health and cataract occurrence could not be determined in our study, the following hypotheses might explain the association. In poor oral hygiene or oral disease status, a systemic inflammatory reaction induced by oral inflammatory conditions may elicit the excessive production of reactive oxygen species, such as superoxide, hydroxyl anions, and hydrogen peroxide in oral or periodontal tissues, as supported by clinical and animal studies (30–33). These reactive oxygen species can diffuse into the bloodstream (33, 34). This condition can cause the oxidation of various molecules in the blood; in turn, it can lead to circulating oxidative stress, which can progressively damage other organs (35, 36). Oxidative stress is an important factor in cataractogenesis in experimental animals and cultured lens models (37, 38). Therefore, increased oxidative stress levels due to chronic oral inflammation may negatively affect cataract development.
In our study, periodontitis showed positive tendency for association with cataract in multivariable analysis, although there was an association in univariable analysis. This may be because the association of other factors, i.e. vascular risk factors, with cataract development was greater than that of periodontitis. The results may be attributed to the nature of the included population, such as general population or ethnicity. Moreover, periodontitis was defined using the frequently used definition in most studies. Although this definition has a high diagnostic accuracy for periodontitis, periodontitis may have been already treated because treatment-related claim codes are considered; therefore, the risk for cataract may be relatively low. Nevertheless, our findings were meaningful because they suggested the possible link between periodontitis and the risk of cataract occurrence.
In the present study, the increased number of dental caries was not a factor associated with the increased risk of cataract. Since dental caries is a biofilm-mediated disease similar to periodontitis, a local inflammatory response through dental caries likely results in systemic inflammation via mechanisms similar to periodontitis (39, 40). However, dental caries unlikely triggers inflammatory responses of surrounding tissues until bacteria penetrate the root canal system of the teeth. Only advanced dental caries causes apical periodontitis, which is characterized by periodontal tissue destruction. Thus, the number of dental caries, including advanced and incipient ones, unlikely affects the increased risk of cataract.
This study has several limitations. First, residual confounding factors might exist and affect cataract development. Ultraviolet sunlight exposure, known to be positively correlated with cataracts (41, 42), was not included in the analyses because of the lack of information on sunlight exposure in the cohort database. Second, results of other races/ethnics might vary because study subjects only included Koreans. Third, no information of the detailed attachment loss was found in the NIHS-HEALS cohort database, and severity of periodontitis could not be investigated. Fourth, response bias such as social–desirability bias might occur because oral health behaviors were based on the self-reported questionnaire. However, this study has the following strengths. Large-scale long-term-tracked nationally representative data were used to elucidate the effect of oral health status and oral hygiene behaviors on cataract occurrence. Our results provided significant evidence supporting the benefits of maintaining good oral health for cataract prevention.
Conclusion
Periodontitis and increased number of missing teeth may be associated with the increased risk of cataract. However, maintaining good oral hygiene through tooth brushing and dental scaling may reduce the risk of future cataract occurrence. Further studies should be performed to confirm the association between chronic oral inflammation and cataract.
Data availability statement
The datasets presented in this article are not readily available because the data used in this study are available in the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) database, but restrictions apply to the public availability of these data used under the license for the current study. Requests for access to the NHIS data can be made through the National Health Insurance Sharing Service homepage (http://nhiss.nhis.or.kr/bd/ab/bdaba021eng.do). For access to the database, a completed application form, research proposal, and application for approval from the institutional review board should be submitted to the inquiry committee of research support in the NHIS for review. Requests to access the datasets should be directed to http://nhiss.nhis.or.kr/bd/ab/bdaba021eng.do.
Ethics statement
This study was approved by the human subjects Ethics Board of Ewha Womans University College of Medicine (2020-08-018). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
J-HP contributed to data interpretation and drafted the manuscript. HL and J-WK contributed to data analysis and interpretation. T-JS contributed to conception, design, data acquisition, interpretation, and critically revised the manuscript. All authors gave final approval and agreed to be accountable for all aspects of the work.
Funding
This project was supported by a grant from the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Education (2021R1F1A1048113 to T-JS). This work was supported by Institute of Information & communications Technology Planning & Evaluation (IITP) grant funded by the Korea government (MSIT) (No.2022-0-00621 to T-JS, Development of artificial intelligence technology that provides dialog-based multi-modal explainability). This project was supported by a grant from the National Research Foundation of Korea funded by the Korean government (2020R1A2C4001842 to J-WK). The funding source had no role in the design, conduct, or reporting of the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.1036785/full#supplementary-material
References
1. Lee K, Lee JS, Kim J, Lee H, Chang Y, Woo HG, et al. Oral health and gastrointestinal cancer: a nationwide cohort study. J Clin Periodontol. (2020) 47:796–808. doi: 10.1111/jcpe.13304
2. Chang Y, Lee JS, Lee KJ, Woo HG, Song TJ. Improved oral hygiene is associated with decreased risk of new-onset diabetes: a nationwide population-based cohort study. Diabetologia. (2020) 63:924–33. doi: 10.1007/s00125-020-05112-9
3. Park MS, Jeon J, Song TJ, Kim J. Association of periodontitis with microvascular complications of diabetes mellitus: a nationwide cohort study. J Diabetes Complications. (2022) 36:108107. doi: 10.1016/j.jdiacomp.2021.108107
4. Song TJ, Chang Y, Jeon J, Kim J. Oral health and longitudinal changes in fasting glucose levels: a nationwide cohort study. PLoS One. (2021) 16:e0253769. doi: 10.1371/journal.pone.0253769
5. Song TJ, Kim JW, Kim J. Oral health and changes in lipid profile: a nationwide cohort study. J Clin Periodontol. (2020) 47:1437–45. doi: 10.1111/jcpe.13373
6. Woo HG, Chang Y, Lee JS, Song TJ. Association of tooth loss with new-onset Parkinson’s disease: a nationwide population-based cohort study. Parkinsons Dis. (2020) 2020:4760512. doi: 10.1155/2020/4760512
7. Chang Y, Woo HG, Lee JS, Song TJ. Better oral hygiene is associated with lower risk of stroke. J Periodontol. (2021) 92:87–94. doi: 10.1002/JPER.20-0053
8. Kim J, Kim HJ, Jeon J, Song TJ. Association between oral health and cardiovascular outcomes in patients with hypertension: a nationwide cohort study. J Hypertens. (2022) 40:374–81. doi: 10.1097/hjh.0000000000003022
9. Liu Y-C, Wilkins M, Kim T, Malyugin B, Mehta JS. Cataracts. Lancet. (2017) 390:600–12. doi: 10.1016/s0140-6736(17)30544-5
10. Rim THT, Kim M-H, Kim WC, Kim T-I, Kim EK. Cataract subtype risk factors identified from the Korea National Health and Nutrition Examination survey 2008–2010. BMC Ophthalmol. (2014) 14:4. doi: 10.1186/1471-2415-14-4
12. Kapila YL. Oral health’s inextricable connection to systemic health: Special populations bring to bear multimodal relationships and factors connecting periodontal disease to systemic diseases and conditions. Periodontol. (2021) 87:11–6. doi: 10.1111/prd.12398
13. Tomofuji T, Irie K, Sanbe T, Azuma T, Ekuni D, Tamaki N, et al. Periodontitis and increase in circulating oxidative stress. Jpn Dent Sci Rev. (2009) 45:46–51. doi: 10.1016/j.jdsr.2008.12.002
14. Wang Y, Andrukhov O, Rausch-Fan X. Oxidative stress and antioxidant system in periodontitis. Front Physiol. (2017) 8:910. doi: 10.3389/fphys.2017.00910
15. Park JH, Kwoen MJ, Lee JR, Kim KS, Lee HJ, Kim JW, et al. Gradual, but not sudden, dose-dependent increase of ONJ risk with bisphosphonate exposure: a nationwide cohort study in women with osteoporosis. Front Endocrinol. (2021) 12:774820. doi: 10.3389/fendo.2021.774820
16. Seong SC, Kim YY, Park SK, Khang YH, Kim HC, Park JH, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open. (2017) 7:e016640. doi: 10.1136/bmjopen-2017-016640
17. Park SY, Kim SH, Kang SH, Yoon CH, Lee HJ, Yun PY, et al. Improved oral hygiene care attenuates the cardiovascular risk of oral health disease: a population-based study from Korea. Eur Heart J. (2019) 40:1138–45. doi: 10.1093/eurheartj/ehy836
18. Geismar K, Stoltze K, Sigurd B, Gyntelberg F, Holmstrup P. Periodontal disease and coronary heart disease. J Periodontol. (2006) 77:1547–54. doi: 10.1902/jop.2006.050405
19. Bengtsson VW, Persson GR, Berglund JS, Renvert S. Periodontitis related to cardiovascular events and mortality: a long-time longitudinal study. Clin Oral Investig. (2021) 25:4085–95. doi: 10.1007/s00784-020-03739-x
20. Chang Y, Woo HG, Park J, Lee JS, Song T-J. Improved oral hygiene care is associated with decreased risk of occurrence for atrial fibrillation and heart failure: a nationwide population-based cohort study. Eur J Prev Cardiol. (2020) 27:1835–45. doi: 10.1177/2047487319886018
21. Joshipura KJ, Hung HC, Rimm EB, Willett WC, Ascherio A. Periodontal disease, tooth loss, and incidence of ischemic stroke. Stroke. (2003) 34:47–52. doi: 10.1161/01.str.0000052974.79428.0c
22. Taguchi A, Sanada M, Suei Y, Ohtsuka M, Lee K, Tanimoto K, et al. Tooth loss is associated with an increased risk of hypertension in postmenopausal women. Hypertension. (2004) 43:1297–300. doi: 10.1161/01.HYP.0000128335.45571.ce
23. Woo HG, Chang Y, Lee JS, Song TJ. Tooth loss is associated with an increased risk of hypertension: a nationwide population-based cohort study. PLoS One. (2021) 16:e0253257. doi: 10.1371/journal.pone.0253257
24. Pockpa ZAD, Struillou X, Coulibaly NT, Weber M, Soueidan A, Badran Z. Potential relationship between periodontal diseases and eye diseases. Med Hypotheses. (2017) 99:63–6. doi: 10.1016/j.mehy.2016.12.011
25. Chau SF, Lee CY, Huang JY, Chou MC, Chen HC, Yang SF. The existence of periodontal disease and subsequent ocular diseases: a population-based cohort study. Medicina. (2020) 56:621. doi: 10.3390/medicina56110621
26. Sun KT, Shen TC, Chen SC, Chang CL, Li CH, Li X, et al. Periodontitis and the subsequent risk of glaucoma: results from the real-world practice. Sci Rep. (2020) 10:17568. doi: 10.1038/s41598-020-74589-6
27. Sun KT, Hsia NY, Chen SC, Lin CL, Chen IA, Wu IT, et al. Risk of age-related macular degeneration in patients with periodontitis: a nationwide population-based cohort study. Retina. (2020) 40:2312–8. doi: 10.1097/IAE.0000000000002750
28. Veena HR, Natesh S, Patil SR. Association between diabetic retinopathy and chronic periodontitis-a cross-sectional study. Med Sci. (2018) 6:104. doi: 10.3390/medsci6040104
29. Yeh LJ, Shen TC, Sun KT, Lin CL, Hsia NY. Periodontitis and subsequent risk of cataract: results from real-world practice. Front Med. (2022) 9:721119. doi: 10.3389/fmed.2022.721119
30. Tsai CC, Chen HS, Chen SL, Ho YP, Ho KY, Wu YM, et al. Lipid peroxidation: a possible role in the induction and progression of chronic periodontitis. J Periodontal Res. (2005) 40:378–84. doi: 10.1111/j.1600-0765.2005.00818.x
31. Tomofuji T, Azuma T, Kusano H, Sanbe T, Ekuni D, Tamaki N, et al. Oxidative damage of periodontal tissue in the rat periodontitis model: effects of a high-cholesterol diet. FEBS Lett. (2006) 580:3601–4. doi: 10.1016/j.febslet.2006.05.041
32. Ekuni D, Tomofuji T, Tamaki N, Sanbe T, Azuma T, Yamanaka R, et al. Mechanical stimulation of gingiva reduces plasma 8-OHdG level in rat periodontitis. Arch Oral Biol. (2008) 53:324–9. doi: 10.1016/j.archoralbio.2007.10.005
33. Akalin FA, Baltacioğlu E, Alver A, Karabulut E. Lipid peroxidation levels and total oxidant status in serum, saliva and gingival crevicular fluid in patients with chronic periodontitis. J Clin Periodontol. (2007) 34:558–65. doi: 10.1111/j.1600-051X.2007.01091.x
34. Sobaniec H, Sobaniec-Lotowska ME. Morphological examinations of hard tissues of periodontium and evaluation of selected processes of lipid peroxidation in blood serum of rats in the course of experimental periodontitis. Med Sci Monit. (2000) 6:875–81.
35. Tomofuji T, Ekuni D, Yamanaka R, Kusano H, Azuma T, Sanbe T, et al. Chronic administration of lipopolysaccharide and proteases induces periodontal inflammation and hepatic steatosis in rats. J Periodontol. (2007) 78:1999–2006. doi: 10.1902/jop.2007.070056
36. Ekuni D, Tomofuji T, Sanbe T, Irie K, Azuma T, Maruyama T, et al. Periodontitis-induced lipid peroxidation in rat descending aorta is involved in the initiation of atherosclerosis. J Periodontal Res. (2009) 44:434–42. doi: 10.1111/j.1600-0765.2008.01122.x
37. Truscott RJ. Age-related nuclear cataract-oxidation is the key. Exp Eye Res. (2005) 80:709–25. doi: 10.1016/j.exer.2004.12.007
38. Gupta SK, Trivedi D, Srivastava S, Joshi S, Halder N, Verma SD. Lycopene attenuates oxidative stress induced experimental cataract development: an in vitro and in vivo study. Nutrition. (2003) 19:794–9. doi: 10.1016/s0899-9007(03)00140-0
39. Scannapieco FA. The oral microbiome: its role in health and in oral and systemic infections. Clin Microbiol Newsl. (2013) 35:163–9. doi: 10.1016/j.clinmicnews.2013.09.003
40. Sabharwal A, Stellrecht E, Scannapieco FA. Associations between dental caries and systemic diseases: a scoping review. BMC Oral Health. (2021) 21:472. doi: 10.1186/s12903-021-01803-w
41. Sharma S, Lang C, Khadka J, Inacio MC. Association of age-related cataract with skin cancer in an Australian population. Invest Ophthalmol Vis Sci. (2020) 61:48. doi: 10.1167/iovs.61.5.48
Keywords: periodontitis, oral hygiene, cataract, epidemiology, oral inflammation
Citation: Park J-H, Lee H, Kim J-W and Song T-J (2023) Better oral hygiene is associated with a reduced risk of cataract: A nationwide cohort study. Front. Med. 9:1036785. doi: 10.3389/fmed.2022.1036785
Received: 05 September 2022; Accepted: 02 November 2022;
Published: 03 January 2023.
Edited by:
Dario Rusciano, Consultant, Catania, ItalyReviewed by:
Mitiku Hambisa, University of New South Wales, AustraliaMihajlo Petrovski, Goce Delcev University, North Macedonia
Copyright © 2023 Park, Lee, Kim and Song. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tae-Jin Song, knstar@ewha.ac.kr
 Jung-Hyun Park
Jung-Hyun Park Heajung Lee
Heajung Lee Jin-Woo Kim
Jin-Woo Kim Tae-Jin Song
Tae-Jin Song