- 1Act to End NTDs | East Program, RTI International, Addis Ababa, Ethiopia
- 2Neglected Tropical Diseases Team, Disease Prevention and Control Directorate, Federal Ministry of Health, Addis Ababa, Ethiopia
- 3Biruck Kebede Beyene, Programme Director, World Vision, Ebril, Iraq
- 4Health Promotion and Disease Prevention Core Process, Beneshangul-Gumuz Regional Health Bureau, Assosa, Ethiopia
- 5Disease Prevention and Control Case Team, Tigray Regional Health Bureau, Mekelle, Ethiopia
- 6Act to End NTDs | East Program, RTI International, Washington, DC, United States
- 7Morbidity Management and Disability Prevention (MMDP) Project, Helen Keller International, Washington, DC, United States
Background: The World Health Organization (WHO) recommends that countries ensure morbidity management and disability prevention (MMDP) services are available to all lymphedema and hydrocele patients in lymphatic filariasis (LF)-endemic areas. The first step in ensuring the availability of MMDP services is to understand the number and distribution of people with lymphedema and hydrocele. We examined the burden of lymphoedema and hydrocoele using different patient estimation approaches employed in endemic districts of the Beneshangul-Gumuz and Tigray regions of Ethiopia.
Methodology/principal findings: In Approach I, trained health extension workers (HEWs) conducted the patient estimates during a door-to-door pre-mass drug administration (MDA) census. Validation of a sample of the data collected was integrated with a post-MDA coverage survey. In Approach II, trained HEWs conducted a stand-alone patient estimation, and clinical officers validated all suspected patients. In 15 districts, 753,557 individuals were surveyed. A total of 1,645 lymphedema (1:1.6 male-to-female ratio) and 517 hydrocele cases were identified. The prevalence of lymphedema and hydrocele was 40 per 10,000 in the adult population and 25 per 10,000 in the adult male population, with wide variation across districts. Validation in Approach I showed that 94% of the lymphedema cases and 77% of hydrocele cases were correctly identified by the HEWs, while 60% and 53% were correctly identified in Approach II.
Conclusion/significance: Patient estimation is important for planning, prioritization, targeting interventions, and monitoring progress in LF-endemic areas. Trained HEWs can correctly identify most cases using a standardized patient estimate job aid and questionnaire, even when cascade training is used. For the purposes of LF elimination, these results are sufficient and at a low cost per district. Ethiopia’s LF program could integrate patient estimations into MDA activities in the remaining LF-endemic districts with minimal cost and effort.
Introduction
Lymphatic filariasis (LF) is a mosquito-borne parasitic infection targeted for elimination as a public health problem by the World Health Organization (WHO). Two key strategies are recommended by the WHO for elimination: stopping the spread of infection through large-scale annual treatment in areas where infection is present; and alleviating the suffering caused by LF-related clinical manifestations through morbidity management and disability prevention (MMDP) activities (1). Globally, 50 countries still require mass drug administration (MDA) to interrupt transmission (2). In 2019, only 58 countries reported estimates of the number of patients by implementation unit (IU) (2).
The two most common LF-related clinical manifestations are lymphedema (swelling of the leg, breast, or arm), which is estimated to affect 16.7 million people globally, and hydrocele (scrotal swelling), which affects 19.4 million men globally (3). These conditions are usually observed from puberty onwards, with increasing prevalence with age (4, 5). In many areas where bancroftian filariasis is endemic, lymphedema of the leg is more common in women than in men (6). Both lymphedema and hydrocele patients are affected by acute dermatolymphangioadenitis (ADLA), also called ‘acute attacks’, which are episodes of fever, pain, and swelling that develop due to secondary bacterial infections and lead to more severe disease (7). There is no definite diagnostic test to prove that lymphedema or hydrocele is caused by LF; instead, the WHO recommends that national LF programs ensure that MMDP services are available for anyone with lymphedema or hydrocele, regardless of the cause, in areas where LF is endemic (7). In the dossier documenting evidence of elimination of LF as a public health problem, the WHO requires data on the estimated number of patients with lymphedema and hydrocele by implementation unit (8). In Ethiopia, 83 districts require MDA for LF, and there are likely to be lymphedema and hydrocele patients in other districts as well.
Patient estimation methodologies
The first step in scaling up MMDP services is to understand the estimated number and distribution of people with lymphedema and hydrocele in order to plan and prioritize services (7, 8). Currently, there is no gold standard methodology recommended for estimating the number of patients. Instead, the WHO recommends a variety of methods, including house-to-house surveys, population-based surveys, and key informant interviews, to estimate the number of patients in each implementation unit (7).
Each methodology has its own strengths and weaknesses. Mathieu et al. found that questionnaire-based surveys underestimate morbidity prevalence compared to information collected through clinical examination due to the potential stigma around disclosing the conditions (9). Other studies have found substantial over-reporting of morbidity by key informants or community health workers after validation through clinical examination by medical doctors (10, 11). Data collected through population-based surveys, while useful in reducing costs through integration with other activities, provide point estimates of patient numbers only. National programs have found line listings from house-to-house surveys more valuable in planning services and reaching patients. This paper examines different approaches to LF patient estimation employed in endemic districts of the Beneshangul-Gumuz and Tigray regions of Ethiopia.
Methods
Study area and population
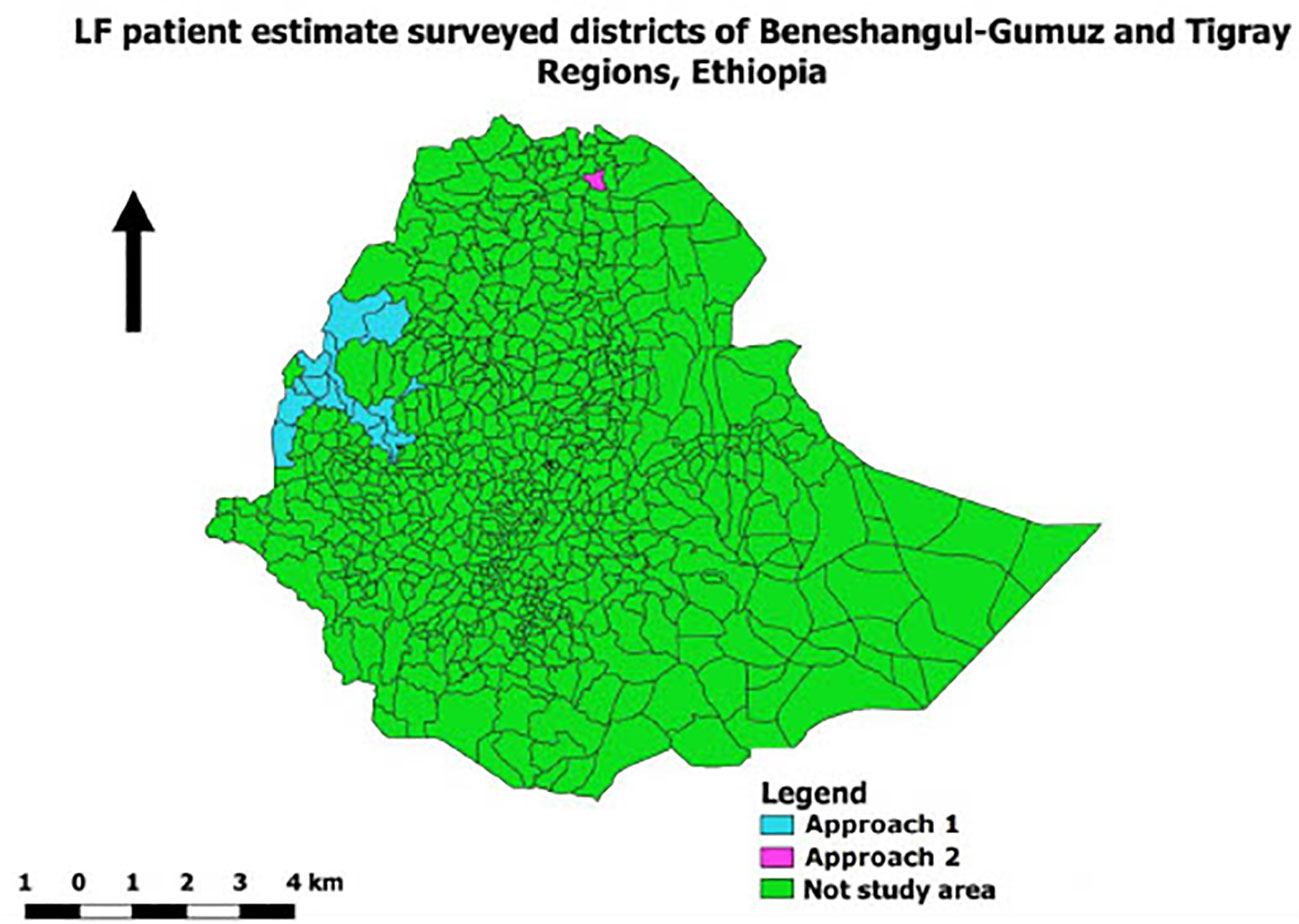
The patient estimations were conducted in 15 districts endemic to LF in the regions of Beneshangul-Gumuz (14 districts) and Tigray (1 district), Ethiopia (Figure 1). Prevalence of filarial antigenemia varied between 1% and 29% as per the LF mapping completed between 2008 and 2014. The population of these districts is estimated at 688,755 (Beneshangul-Gumuz 556,550 and Tigray 132,205). The total population in each district was targeted for inclusion in the study, including two refugee camps, Sherkole and Tongo, in Beneshangul-Gumuz. Of the 15 districts, 1 (Homosha) in Beneshangul-Gumuz is co-endemic with podoconiosis.
Study period
The patient estimation survey was conducted between December 2015 (Beneshangul-Gumuz) and April 2016 (Tigray) over a period of 2 weeks in each region.
Study design and sampling
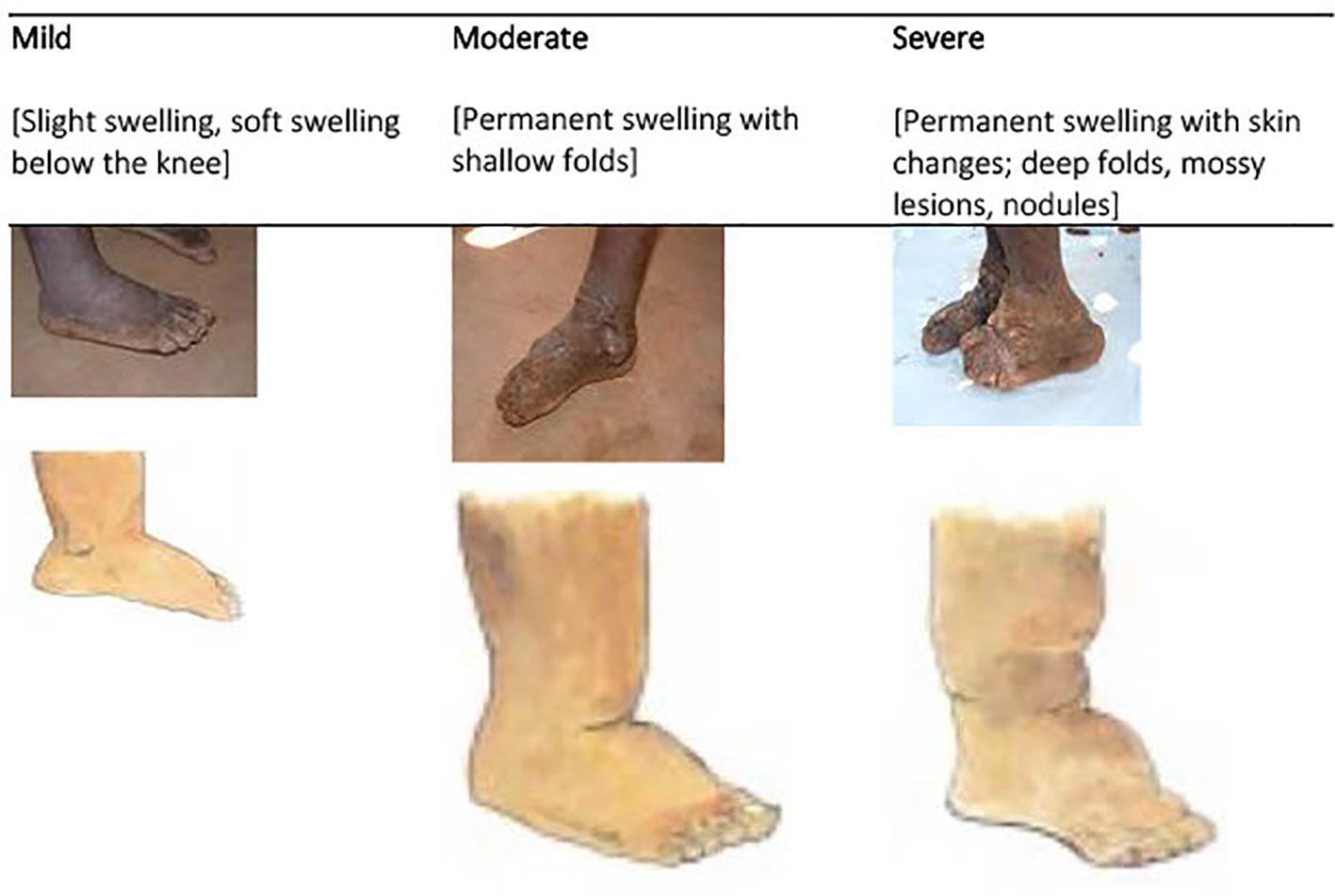
Two different approaches were used to estimate the number of patients with lymphedema or hydrocele (Table 1). In Approach I, patient estimates and validation were integrated with the existing activities of the LF pre-MDA census and coverage survey, respectively. In Approach II, a standalone method was used to conduct the patient estimates and validation. In both approaches, the study used a semi-structured questionnaire-based, cross-sectional study design conducted by the HEWs in their community catchment areas or villages. The HEWs were female trained government employees recruited from the communities they served to expand access to basic health promotion, disease prevention, and selected curative health services (12). For LF, HEWs routinely provide social mobilization and census updates before mass drug administration, provide training to community drug distributors, and supervise mass drug administration. Clinical workers are health officers and/or nurses who provide training to health extension workers and supervise mass drug administration during the MDA week.
Approach I: data collection by HEWs during pre-MDA census
In 14 districts in the Beneshangul-Gumuz region, patient estimation data was integrated into ongoing LF-onchocerciasis MDA activities.
1a. Training
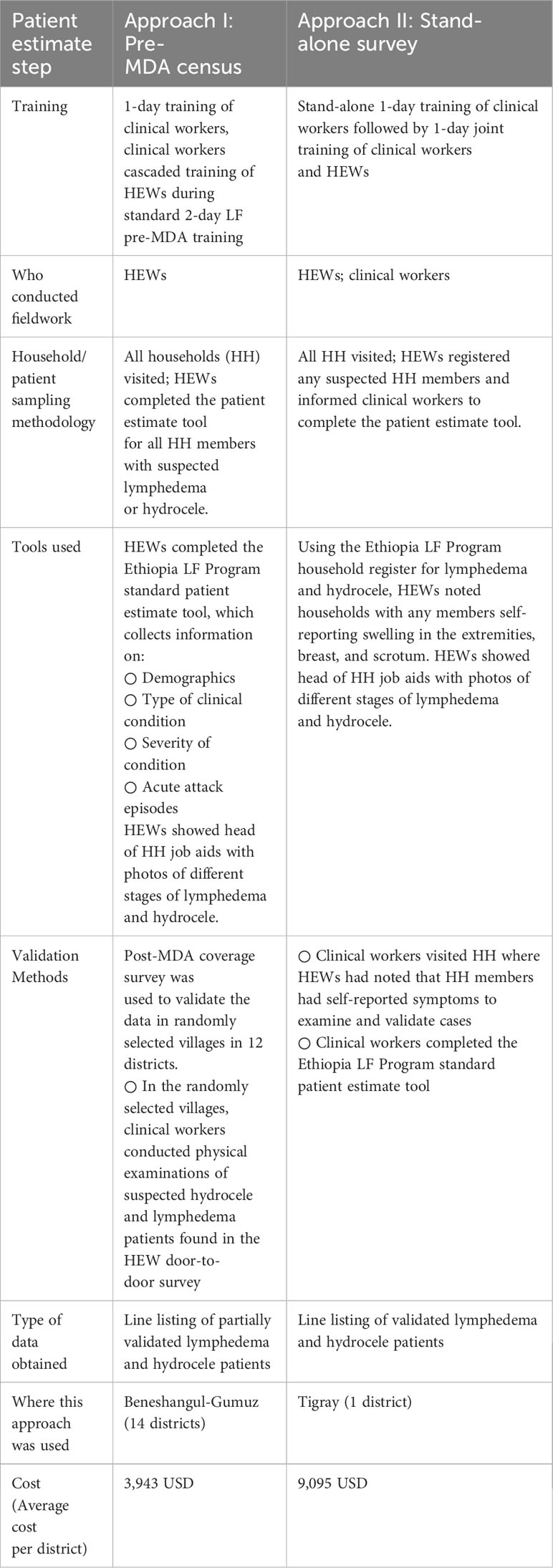
As part of a two-day MDA training of trainers for regional, zonal, and district NTD focal persons and health center staff, sessions were included on the need for patient estimates, case detection, clinical symptoms, lymphedema staging, lymphedema management, and patient estimate data collection tools. The survey team from the Federal Ministry of Health (FMOH), Research Triangle Institute (RTI) International, and National Podoconiosis Action Network (NaPAN) led practical training on clinical diagnosis and disease staging, using a simplified staging system, based on a modified Dreyer scale in which stage 1 ‘mild’ included slight swelling below the knee, either reversible or irreversible; stage 2 ‘moderate’ included permanent swelling with shallow folds; and stage 3 ‘severe’ included permanent swelling with skin changes, deep folds, mossy lesions, or nodules (Figure 2) (13). Acute attacks were defined as painful inflammation of the foot and/or leg with swollen lymph nodes and fever.
A cascade training approach was used to train HEWs in their respective districts integrated with LF/onchocerciasis MDA training.
1b. Fieldwork
Using a job aid with clinical photos, HEWs registered people with lymphedema and/or hydrocele in their respective villages over a period of 10 days through house-to-house visits integrated with the pre-MDA census. The head of the household was asked for consent and whether they had any family members with lymphedema and hydrocele. Each individual with suspected lymphedema or hydrocele completed a 10-15-minute questionnaire in the Amharic or Tigrigna language, collecting information on age, sex, occupation, onset of clinical signs, disease stage, and number of acute attacks in the past 6 months. The data collection tools were adapted from a previous LF and podoconiosis patient estimate study in Amhara and Southern Nations, Nationalities and Peoples regions, Ethiopia (13).
1c. Validation methods
While conducting a post-LF-onchocerciasis MDA coverage survey in Beneshangul-Gumuz, trained clinical personnel confirmed any cases reported by HEWs in the randomly selected villages. A survey team deployed in the randomly selected villages to perform the coverage survey while a clinical officer visited the suspected patients identified in that village during the initial patient estimation exercise to physically examine the patients to confirm the clinical diagnosis.
Approach II: data collection by HEWs during separate house-to-house survey
In one district in the Tigray region, patient estimation data was collected through a stand-alone activity.
2a. Training
The survey team from FMOH, RTI, and NaPAN conducted a one-day training for clinical workers followed by a one-day training for clinical workers and HEWs that used the same training materials as in Beneshangul-Gumuz.
2b. Fieldwork
HEWs conducted house-to-house visits in Tigray to complete the patient estimation. The head of the household was asked if any members had lymphedema or hydrocele, using the same job aids as in the first approach. HEWs filled out a lymphedema and hydrocele register and notified clinical workers if any household self-reported a patient case. Clinical workers then visited households to fill out the standard Ethiopia LF patient estimate tool and returned them to the district NTD focal person, who reviewed for completeness.
2c. Validation methods
Clinical workers validated the suspected cases reported by HEWs by visiting the respective households to physically examine suspected patients.
Data entry and analysis
Data were entered, cleaned, and analyzed using SPSS v.23.0. The overall frequency of lymphedema and hydrocele were calculated by district. Only those 15 years and older were included in the data analysis. The prevalence estimates of lymphedema and hydrocele were calculated as the ratio of the number of patients with lymphedema or hydrocele to the total adult population (male population only for hydrocele) in the surveyed districts. For Beneshengal-Gumuz, where only some patients were validated, prevalence estimates were calculated using suspected patients. For Tigray, estimates were calculated using validated patients only. Adult population denominators, i.e., those 15 years and older, were calculated from the latest 2007 national census using the annual regional total population growth rates and adult population rates for 2016 (12 districts of Beneshengal-Gumuz and 1 district of Tigray) and 2017 (2 districts of Beneshengal-Gumuz).
Descriptive statistical analysis was performed to examine the frequency distribution of the demographic and disease information included in the study. The age of patients and the number of years with lymphedema and hydrocele were presented as median and range, while all other categorical variables (sex, education, occupation, marital status, type, and stage of lymphedema) were presented as frequencies and percentages.
The association of stage of lymphedema with age, sex, education, occupation, marital status, and acute attacks of respondents was assessed using the Chi-square test for independence. This test compares two variables to determine whether their distributions are different from each other. A p-value of less than 0.05 was considered significant in the determination of the association between the variables. During statistical analysis, variables were categorized as follows. For lymphedema stage, two categories were made: mild or moderate lymphedema and severe lymphedema. For age, 15-34, 35-54, 55-74, and 74+ age groups were used. For education status, two categories were made: illiterate and literate. For occupation, the farmers were compared with all other occupation categories. For marital status, married patients were compared with other marital groups.
For Beneshangul-Gumuz data, chi-squared tests were conducted to assess the presence of an association between any reported acute attacks in lymphedema patients and stage of lymphedema, age, sex, education, occupation, and marital status, as well as between these variables and the frequency of acute attacks (using the median value to group answers in categories of <=4 and >4). The same tests were also conducted to assess the presence of association between any reported acute attacks in hydrocele patients and age, education, occupation, and marital status, as well as between the same variables and frequency of acute attacks (using median value to group answers in categories of <=3 and >3). For Tigray data, given the small number of hydrocele patients (17), analysis was done for both lymphedema and hydrocele patients together.
Suspected patients identified during the initial patient estimation and those confirmed during the validation step were compared to calculate the proportion of cases accurately identified by HEWs.
Ethical consideration
The Beneshangul-Gumuz and Tigray Regional Health Bureaus approved implementation of the study before it was conducted. Prior to data collection, verbal consent was obtained from heads of households. Only those who provided consent were registered, interviewed, and examined. Individuals identified as having lymphedema and hydrocele were provided health education, advised how to take care of their hygiene for early-stage lymphedema, and advised to visit the nearest hospital to receive healthcare for advanced-stage lymphedema and surgical services for hydrocele.
Results
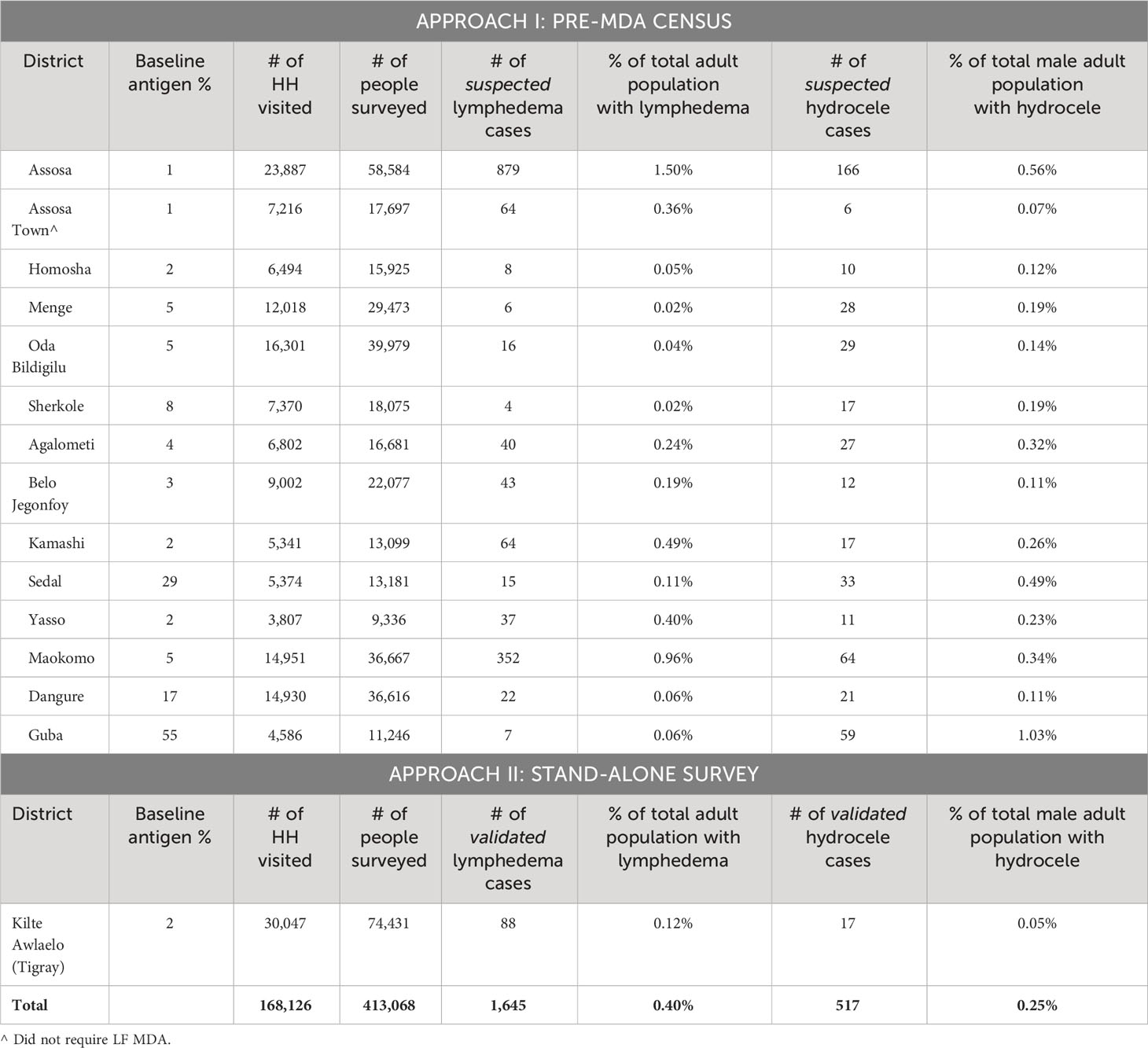
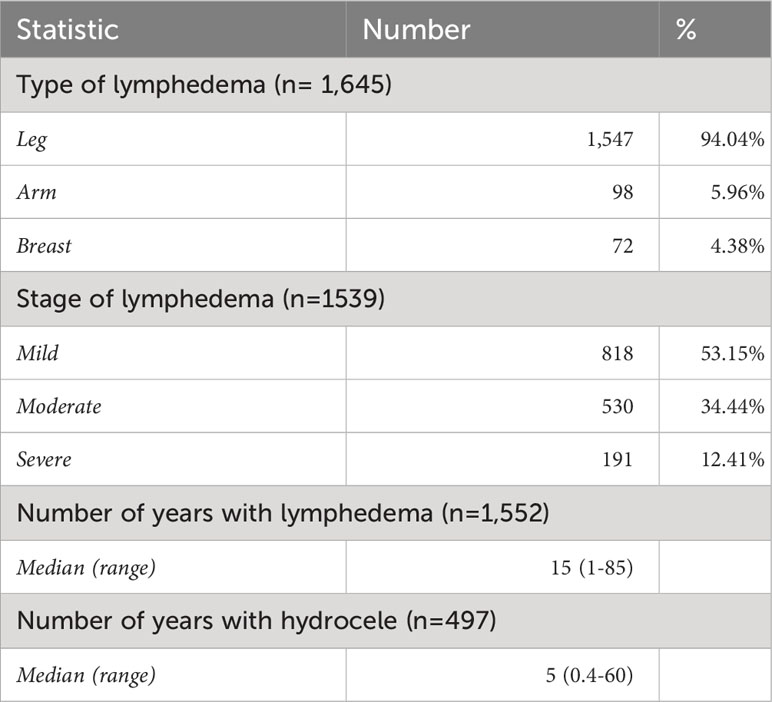
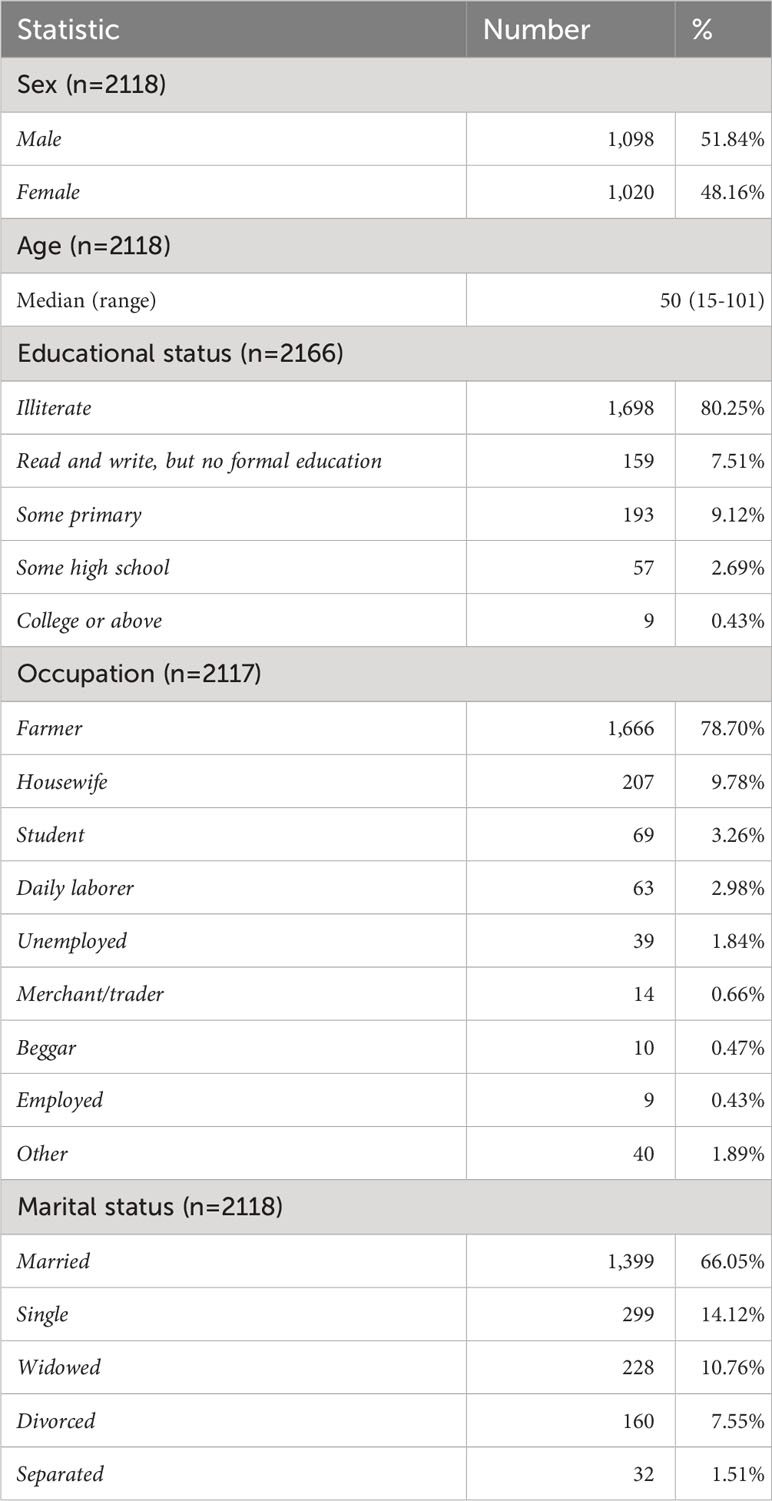
A total of 168,126 households were visited and 753,557 individuals (413,068 adults) were surveyed in 15 districts; with 1,645 cases of lymphedema and 517 cases of hydrocele identified (Table 2). In Beneshangul-Gumuz, since only a portion of the patients were validated (123 adults), results include all suspected adult patients, i.e., those 15 years and older. The results do not include 90 children, 30 with lymphedema and 63 with hydrocele, originally included as suspected patients. In Tigray, since full information including age and sex was only collected on validated patients, the results include all validated adult patients. Overall, the percentage of the adult population with lymphedema was estimated at 0.4% and the percentage of the adult male population with hydrocele was estimated at 0.25%. Of the 1,645 lymphedema patients, 1,547 (94%) had lymphedema of the leg, 98 (5.96%) had arm lymphedema, and 72 (4.4%) had breast lymphedema (Table 3). The median number of years with disease for lymphedema patients was 15 years (range: 1-85), and for hydrocele patients, it was 5 years (range 0.4-60). The median age of patients was 50 years (range: 15-101) (Table 4). Overall, 52% of respondents were male. Of the 1645 lymphedema patients, 625 (38%) were male and 1,020 (62%) were female, with a male-to-female ratio of 1:1.6. The vast majority of the patients were illiterate (80.25%), most were farmers (78.70%), and the majority were married (66.05%).
Lymphedema stage
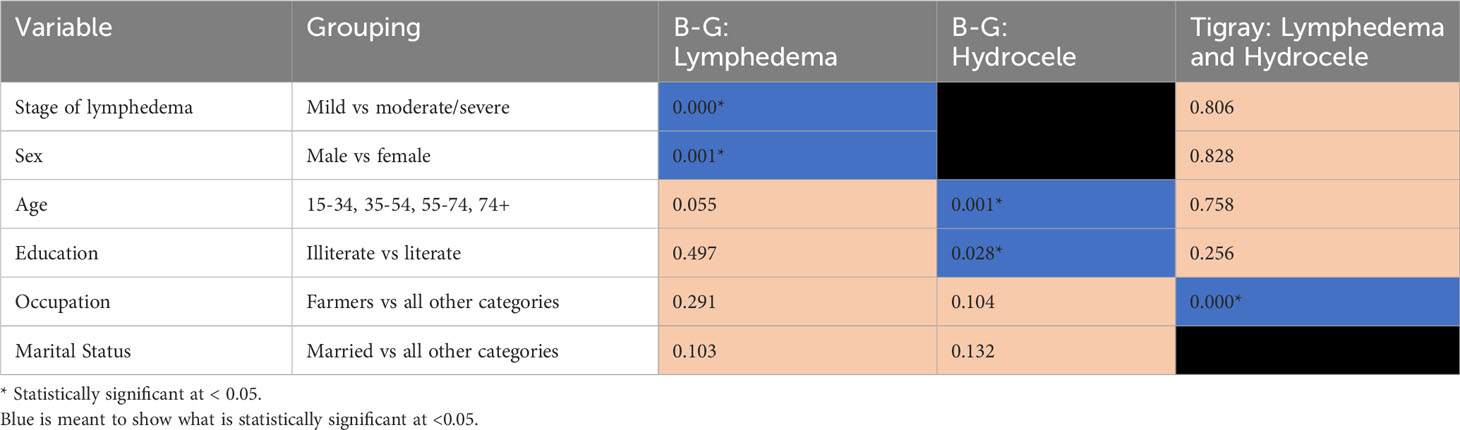
Stage of lymphedema disease was collected from 1,539 lymphedema patients, of whom 818 (53%) were identified as having mild lymphedema, 530 (34%) moderate, and 191 (12%) severe (Table 3). The proportions of male and female cases for each stage were similar, with slightly more than half of mild, moderate, and severe cases being female: 60.6%, 61.7%, and 59.2%, respectively. In Beneshangul-Gumuz, comparing those with mild or moderate lymphedema to those with severe lymphedema, a statistically significant association was only found between stage and occupation (X2 = 15.025, p=0.000). In Tigray, a statistically significant association was only found between stage and sex (X2 = 4.656, p=0.031).
Validation results
a. Approach I
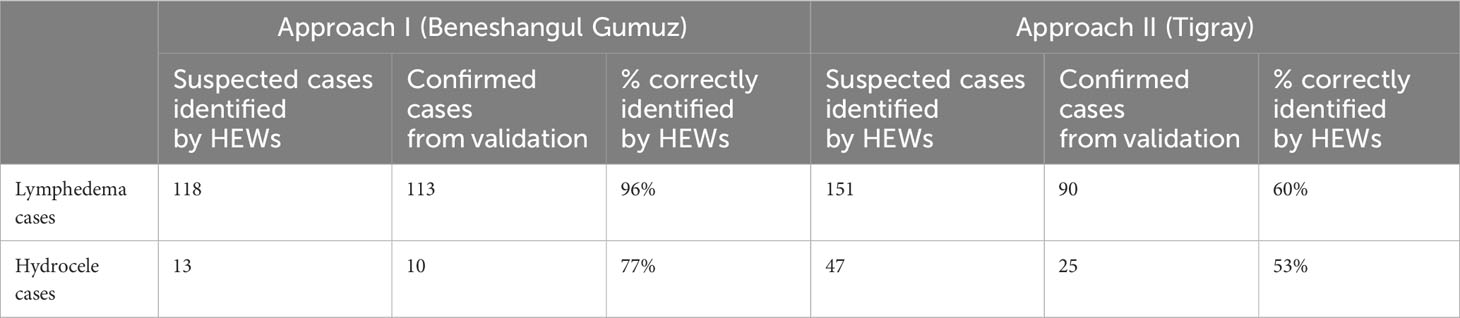
During the validation process, of the 131 patients assessed, the clinical workers validated 123 (94%) had lymphedema or hydrocele (Table 5). The result showed that 113 of 118 (96%) lymphedema patients, and 10 of 13 (77%) hydrocele patients were correctly identified by HEWs. Validation was not done on stage of disease. In addition to the 123 validated patients, the validation team also identified four hydrocele patients and one lymphedema patient who were not originally registered by HEWs.
b. Approach II
In the Tigray region, all suspected lymphedema and hydrocele patients were validated by the trained clinical workers after the HEWs registered the suspected patients. Among 151 lymphedema patients and 47 hydrocele patients registered by HEWs, clinical workers confirmed 90 (60%) had lymphedema and 25 (53%) had hydrocele (Table 5).
Acute attacks
From the 1,688 patients answering questions about acute attacks, 922 (55%) reported experiencing acute attacks in the 6 months prior to the survey, with 40.2% of male patients and 59.8% of female patients reporting at least one acute attack. Of the 818 patients who reported a specific number of acute attacks, the median number of acute attacks reported was four (range: 1-80).
In Beneshangul-Gumuz, there were significant associations between any reported acute attack in lymphedema patients with stages of lymphedema (X2 = 22.855, p=0) and sex (X2 = 10.796, p=0.001) (Table 6 and Supplementary Material). Furthermore, in Beneshangul-Gumuz, there were significant associations between any reported acute attack in hydrocele patients with age (X2 = 15.662, p=0.001) and education (X2 = 4.858, p=0.028). In Tigray, a statistically significant association was found with any reported acute attack in both lymphedema and hydrocele patients and occupation (X2 = 23.213, p=0).
Discussion
Results from this assessment were comparable with previous patient estimates in Ethiopia and other LF-endemic countries. The present study revealed that the prevalence of lymphedema was 40 per 10,000 in the adult population, ranging from 2 to 150 per 10,000 among districts, which lies within the range of results from Malawi (17.7 per 10,000 adults) and Ghana (76.9 per 10,000 adults) (14). It is markedly lower than a study conducted in LF- and podoconiosis-endemic districts of Ethiopia (147 per 10,000 adult population) (13), which is to be expected given that only one of the districts in this study was co-endemic for podoconiosis.
The prevalence of hydrocele in this study was 25 per 10,000 in the adult male population, ranging from 5 to 103 per 10,000 among districts, which is equivalent to 13 patients per 10,000 adults. Previous studies conducted in Ethiopia, Malawi, and Ghana found a wide range of hydrocele prevalence per 10,000 adults, at 4.4, 33, and 70.5, respectively (13, 14).
This assessment found a greater burden of lymphedema cases in the female population compared to the male population, with a male-to-female ratio of 1:1.6, similar to other studies in Ethiopia, Nigeria, and India (4, 5). This study also identified 54%, 34%, and 12% of patients as having mild, moderate, and severe lymphedema, respectively. This finding is consistent with the previous Ethiopia study in 20 LF and podoconiosis co-endemic districts, which reported that 58% of patients had mild lymphedema, 34% moderate, and 9% severe (13), as well as a 2016 India study, which identified 67% of patients in early stages, 22% in moderate, and 10% in advanced stages (4). The study identified variation in the prevalence of lymphedema and hydrocele among districts of Beneshangul Gumuz regions. The highest prevalence of lymphedema, 1.5%, was observed in the Assosa district, whereas the lowest prevalence, 0.02%, was observed in the Mengae and Sharkole districts. It is unclear why there was a higher lymphedema prevalence in the Assosa district. This could be due to a higher concentration of lymphedema patients around the urban center and tertiary referral hospital, but this is speculation. The highest prevalence of hydrocele, 1.03%, was observed in the Guba district, whereas the lowest prevalence, 0.05% was observed in Kilte. The higher hydrocele prevalence in the Guba district might be related to the baseline prevalence, which was 55%.
Analysis of associations between the demographic variables and LF patients or acute attacks can provide valuable insights to program managers and/or clinical health workers to understand the impact of these variables on the disease so that health workers can provide targeted interventions such as health education, counseling, and treatment. In Beneshangul-Gumuz, the stage of lymphedema was associated with occupation. Most lymphedema patients were farmers, and the increased risk of lymphedema in farmers may be due to poor sanitation and hygiene practices and access to healthcare. Targeted interventions are needed, including health education, self-care and personal hygiene practices, and the provision of access to healthcare.
Acute attack data was difficult to parse out. The range of acute attacks was quite wide, with 3.1% of patients reporting over 10 acute attacks in the previous 6 months. There is potential that the definition of acute attack used was simplified to ‘fever’ by the HEWs and, thus, patients overreported acute attacks. When looking at associations, there was no pattern to what was significantly associated with acute attacks for lymphedema patients in Beneshangul-Gumuz, hydrocele patients in Beneshangul-Gumuz, or all patients in Tigray.
This study builds on a previous methodology used in other regions of Ethiopia by adding validation of suspected patients by clinical workers. The validation showed that the HEWs correctly identified most patients, even when cascade training was implemented. The validation result of Approach I indicated that 97% of lymphedema and 77% of hydrocele cases were correctly identified by HEWs, while Approach II indicated that 60% of lymphedema and 53% of hydrocele cases were correctly identified. The reasons for lower validation scores in Approach II are unclear but perhaps have something to do with the fact that when HEWs fill out the entire questionnaire, as in Approach I, they are more accurate in the reporting. One limitation of this study is that information on differential diagnosis of patients not correctly identified by HEWs was not collected. Not having to use clinical workers to accurately identify cases can help ease the potential burden on the health system. For the purposes of LF elimination – which requires an estimated number of patients so that national programs can plan and budget for MMDP activities – these results are sufficient and at a low cost per district. Sufficient quality data was able to be collected using Approach I, which was a third of the cost of the stand-alone survey piloted in Approach II.
In addition, we showed that integrating patient estimates into ongoing NTD activities, such as the pre-MDA census, was feasible and did not result in poorer quality estimates. However, this integration does incur an additional time burden to HEWs for taking consent, registering suspected patients, and observing lymphedema stages. Given the restrictions on funding for patient estimates in many LF-endemic countries, this is encouraging as a way forward to complete patient estimates for planning and budgeting MMDP activities. We found that a house-to-house morbidity census not only helps to identify patients at a community level but creates awareness in the health-seeking behavior of patients and their families. Anecdotal reports from the districts found that many patients and families asked during the patient interviews whether hydrocele surgery service was available in their catchment area. Clinical workers were also trained on lymphedema management so that they could immediately respond to questions from the identified patients and inform the local health system so that it could provide the necessary health services.
HEWs, female government-salaried community health workers, were involved as primary patient identifiers in their respective communities. Given their experience in health matters and the trust bestowed on them by the community, they are well positioned to identify these patients. While a potential limitation to using HEWs is the reluctance of men with hydrocele to disclose the condition to women, especially those from the same community (13), showing the job aid to family members helped in part to overcome any shyness felt by the HEWs themselves as well as patients. However, given the stigma associated with hydrocele (15), it is likely some hydrocele patients were not identified through this approach. The prevalence of hydrocele was lower than reported in other studies, and a 2016 hydrocele surgery camp in Assosa included 56 patients who only were identified when they self- referred to the camp. In order to overcome this barrier, stronger community sensitization about LF, the consequences if left untreated, and treatment availability ahead of patient identification could be useful.
One limitation of this study was a lack of statistical analysis to compare the agreement of different approaches employed during the burden assessment in the two regions. This was because, during data collection, the questionnaires were completed only for lymphedema and hydrocele cases, and this didn’t allow us to conduct an analysis of agreement between the two approaches. The other reason was that the populations were of markedly different sizes in the two approaches.
The two pillars of elimination of LF are interruption of transmission through MDA and ensuring access to MMDP services for those affected individuals. Knowing the burden of LF morbidity is the first step to ensuring quality services for lymphedema and hydrocele patients, and reporting it by implementation unit is a dossier requirement. Patient estimation is important for planning and prioritizing interventions and monitoring progress in endemic areas. In Ethiopia, as of 2019, 51% of districts requiring LF mass drug administration have conducted patient estimates. Given the results of this study, the country LF program could use LF or other MDA activities as an opportunity to integrate patient estimations into the remaining LF-endemic districts with minimal cost and effort.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Tigray and Beneshangul-Gumuz RHB. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
BM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. FK: Conceptualization, Investigation, Methodology, Writing – original draft. BK: Conceptualization, Methodology, Writing – original draft, Formal analysis, Supervision. AM: Conceptualization, Formal analysis, Methodology, Validation, Writing – original draft, Investigation, Visualization. BB: Methodology, Supervision, Writing – review & editing. SAb: Methodology, Writing – review & editing, Conceptualization, Validation. BT: Methodology, Validation, Investigation, Writing – original draft. AO: Validation, Writing – original draft, Supervision. SAl: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. SB: Conceptualization, Methodology, Supervision, Writing – review & editing. CB: Investigation, Methodology, Supervision, Writing – original draft. ET: Writing – review & editing. MB: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. SM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. These activities were made possible by the generous support of the American people through the United States Agency for International Development (USAID). The content is the responsibility of the authors and does not necessarily reflect the views of USAID or the United States Government. The activities were conducted under the Morbidity Management and Disability Prevention (MMDP) Project, which is led by Helen Keller International in partnership with RTI International and the African Filariasis Morbidity Project.
Acknowledgments
The study authors would like to thank NaPAN for providing technical support during the training of supervisors, clinical officers, and health extension workers. The Beneshangul-Gumuz and Tigray Regional Health Bureau coordinated the overall patient estimate process starting from the planning process, training, patient identification, and validation. The authors would also like to thank the patients, HEWs, clinical workers, and regional and district NTD focal persons who took part in these activities.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fitd.2023.1286274/full#supplementary-material
References
1. World Health Organization. Lymphatic filariasis: Progress report 2000–2009 and strategic plan 2010– 2020. Geneva:World Health Organization (2010).
2. World Health Organization. Global programme to eliminate lymphatic filariasis: progress report, 2019. Wkly Epidemiol Rec Relevépidémiologique Hebd (2020) 95:509–24.
3. Ramaiah KD, Ottesen EA. Progress and impact of 13 years of the global programme to eliminate lymphatic filariasis on reducing the burden of filarial disease. PloS Negl Trop Dis (2014). 8(11):e3319. doi: 10.1371/journal.pntd.0003319
4. Walsh V, Little K, Wiegand R, Rout J, Fox LAM. Evaluating the burden of lymphedema due to lymphatic filariasis in 2005 in Khurda district, Odisha state, India. PloS Negl Trop Dis (2016) 10:1–12. doi: 10.1371/journal.pntd.0004917
5. Christiana O, Olajumoke M, Oyetunde S. Lymphatic filariasis and associated morbidities in rural communities of Ogun State, Southwestern Nigeria. Travel Med Infect Dis (2013) 12:95–101. doi: 10.1016/j.tmaid.2013.02.006
6. Allotey P, Gyapong M. The gender agenda in the control of tropical diseases : a review of current evidence (2005). Available at: http://www.who.int/iris/handle/10665/69067.
7. World Health Organization. Lymphatic Filariasis: Managing Morbidity and Preventing Disability: An Aide Memoire for National Programme Managers. Geneva:World Health Organization (2013).
8. World Health Organization. Validation of Elimination of Lymphatic Filariasis as a Public Health Problem. Geneva:World Health Organization (2017).
9. Mathieu E, Amann J, Eigege A, Richards F, Sodahlon Y. Collecting baseline information for national morbidity alleviation programs: different methods to estimate lymphatic filariasis morbidity prevalence. Am J Trop Med Hyg (2008) 78:153–8. doi: 10.4269/ajtmh.2008.78.153
10. Addiss DG, Louis-Charles J, Roberts J, Leconte F, Wendt JM, Milord MD, et al. Feasibility and effectiveness of basic lymphedema management in Leogane, Haiti, an area endemic for bancroftian filariasis. PloS Negl Trop Dis (2010) 4:e668. doi: 10.1371/journal.pntd.0000668
11. Leang R, Socheat D, Bin B, Bunkea T, Odermatt P. Assessment of disease and infection of lymphatic filariasis in Northeastern Cambodia. Trop Med Int Health (2004) 9:1115–20. doi: 10.1111/j.1365-3156.2004.01311.x
12. Tilahun H, Fekadu B, Abdisa H, Canavan M, Linnander E, Bradley EH, et al. Ethiopia’s health extension workers use of work time on duty: time and motion study. Health Policy Plan. (2017) 32:320–8.
13. Kebede B, Martindale S, Mengistu B, Kebede B, Mengiste A, H/Kiros F, et al. Integrated morbidity mapping of lymphatic filariasis and podoconiosis cases in 20 co-endemic districts of Ethiopia. PloS Negl Trop Dis (2018) 12:1–16. doi: 10.1371/journal.pntd.0006491
14. Stanton MC, Mkwanda SZ, Debrah AY, Batsa L, Biritwum N-K, Hoerauf A, et al. Developing a community-led SMS reporting tool for the rapid assessment of lymphatic filariasis morbidity burden: case studies from Malawi and Ghana. BMC Infect Dis (2015) 15:214. doi: 10.1186/s12879-015-0946-4
Keywords: lymphedema, lymphatic filariasis, morbidity, patient estimate, hydrocele
Citation: Mengistu B, Kebede F, Negash BK, Miheret A, Beyene BK, Abetew S, Tedla BG, Oucha AK, Alene S, Backers S, Burgert C, Toubali E, Brady M and McPherson S (2024) Comparing different lymphatic filariasis patient estimate approaches and results in Ethiopia. Front. Trop. Dis 4:1286274. doi: 10.3389/fitd.2023.1286274
Received: 31 August 2023; Accepted: 01 December 2023;
Published: 05 February 2024.
Edited by:
Anders Seim, Health and Development International, United StatesReviewed by:
Charles D. Mackenzie, Task Force for Global Health, United StatesEmmanuel Abraham Mpolya, Nelson Mandela African Institution of Science and Technology, Tanzania
Copyright © 2024 Mengistu, Kebede, Negash, Miheret, Beyene, Abetew, Tedla, Oucha, Alene, Backers, Burgert, Toubali, Brady and McPherson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Scott McPherson, smcpherson@rti.org
 Belete Mengistu1
Belete Mengistu1 Solomon Abetew
Solomon Abetew Shigute Alene
Shigute Alene Scott McPherson
Scott McPherson