Attrition in the Gothenburg H70 birth cohort studies, an 18-year follow-up of the 1930 cohort
- 1Neuropsychiatric Epidemiology Unit, Department of Psychiatry and Neurochemistry, Institute of Neuroscience and Physiology, Sahlgrenska Academy at the University of Gothenburg, Mölndal, Sweden
- 2Centre for Ageing and Health (AgeCap) at the University of Gothenburg, Gothenburg, Sweden
- 3Department of Mood Disorders, Region Västra Götaland, Sahlgrenska University Hospital, Gothenburg, Sweden
- 4Psychiatry, Cognition and Old Age Psychiatry Clinic, Region Västra Götaland, Sahlgrenska University Hospital, Gothenburg, Sweden
- 5Aging Research Center, Department of Neurobiology, Care Sciences and Society, Karolinska Institutet and Stockholm University, Stockholm, Sweden
- 6Region Västra Götaland, Department of Psychiatry, Psychotic Disorders, Sahlgrenska University Hospital, Mölndal, Sweden
Background: Longitudinal studies are essential to understand the ageing process, and risk factors and consequences for disorders, but attrition may cause selection bias and impact generalizability. We describe the 1930 cohort of the Gothenburg H70 Birth Cohort Studies, followed from age 70 to 88, and compare baseline characteristics for those who continue participation with those who die, refuse, and drop out for any reason during follow-up.
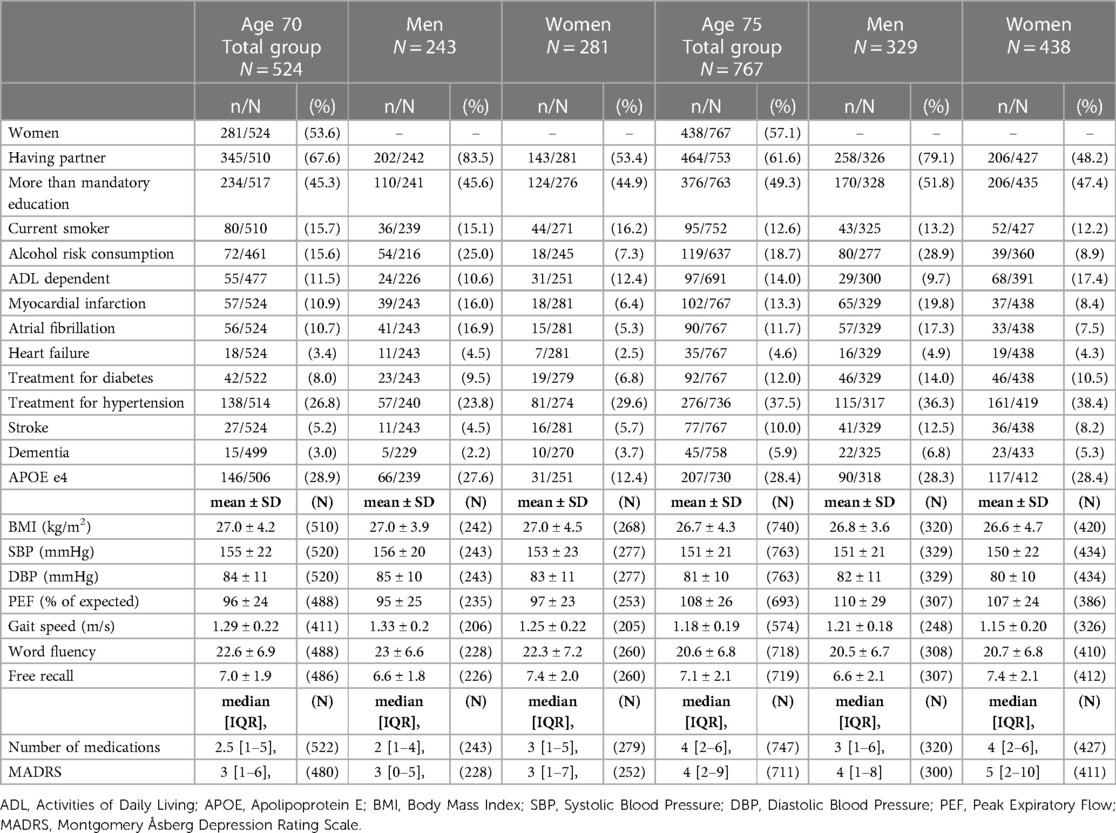
Methods: A population-based sample born 1930 was examined with comprehensive assessments at age 70 (N = 524). The sample was followed up and extended to increase sample size at age 75 (N = 767). Subsequent follow-ups were conducted at ages 79, 85, and 88. Logistic regression was used to analyze baseline characteristics in relation to participation status at follow-up.
Results: Refusal to participate in subsequent examinations was related to lower educational level, higher blood pressure, and lower scores on cognitive tests. Both attrition due to death and total attrition were associated with male sex, lower educational level, smoking, ADL dependency, several diseases, poorer lung function, slower gait speed, lower scores on cognitive tests, depressive symptoms, and a larger number of medications. Attrition due to death was also associated with not having a partner.
Conclusions: It is important to consider different types of attrition when interpreting results from longitudinal studies, as representativeness and results may be differently affected by different types of attrition. Besides reducing barriers to participation, methods such as imputation and weighted analyses can be used to handle selection bias.
1. Introduction
Longitudinal population studies are essential to study ageing processes and incidence, risk factors, and consequences of disorders. However, differences in characteristics between participants and those who drop out can affect representativeness compared to the target population (1) and impact results in association studies (2). In attrition analyses, it is essential to differentiate between various types of attrition, especially to separate attrition due to death and non-death attrition since their impact on representativeness and study results differ (1). Non-death attrition (e.g. refusal to participate and contact failure) may be more important for representativeness than attrition due to death since deaths occur both in the target population and the study cohort (1). All types of attrition may introduce bias and impact effect estimates in association studies, but attrition due to death is especially relevant in longitudinal studies involving older adults where death rates are high (2).
The Gothenburg H70 Birth Cohort Studies (the H70 studies) are multidisciplinary, population-based studies of older adults in Gothenburg, Sweden, aiming to study prevalence, incidence, risk factors, and consequences of physical and mental disorders (3). The H70 studies started in 1971, with baseline examinations of 70-year-olds born 1901-02. Since then, five birth cohorts with baseline at age 70 have been examined longitudinally. Since the start, more than 700 papers have been published using H70 data and the longitudinal design has e.g. enabled the discovery of several risk factors for dementia (4–9) and depression (7, 10). The consecutive recruitment of new birth cohorts of the same age and the use of similar examinations has enabled studies of time trends, and its effect on risk factors and outcomes (11–13).
The aim of this study is to examine if individuals characteristics at age 70 and 75 in the 1930 cohort of the H70 studies, differ between those who participate and those who refuse, die, or drop out for any reason at each follow-up.
2. Methods
All samples from the H70 Studies are systematically selected from the Swedish Population Register based on birth dates to yield representative samples. The five first cross-sectional samples of the 1930-cohort from year 2000–02 to 2018–19 have been described in detail previously (14).
Part of the sample born 1930 (i.e. women born on day 6, 12, 18, 24 and 30 of each month who lived in Gothenburg at the time of the invitation) has been examined previously within the Prospective Population Study of Women (the PPSW study) that started in 1968–69 and was followed-up in 1974–75, 1980–81, and 1992–94 (15). When inviting individuals in year 2000–02 to the first examination of the 1930 cohort within the H70 study, the sample from the PPSW study was extended and included both male and female residents in Gothenburg born on day 3, 6, 12, 18, 21, 24 and 30 of each month (except for women born on day 21, were only those born in January-July were included). At the first follow-up of the H70 1930 cohort in year 2005, the sample was further extended to include male and female residents in Gothenburg born on days 2, 3, 5, 6, 11, 12, 16, 18, 20, 21, 24, 27, or 30 of each month (except for day 27, were only those born in January-May were included).
A letter was first sent to all sampled individuals, who thereafter were contacted by telephone and asked about participation. If they could not visit the outpatient clinic, they were offered home visits. Exclusion criteria included emigration before examination start, inability to speak the Swedish language (language difficulties) and contact failure. The baseline participants were contacted again at each follow-up, except for those who wished not to be contacted further.
2.1. Description of the sample with baseline at age 70
In 2000–02, 775 70-year-olds were invited. Among those, 12 could not participate due to language difficulties, five died before the examination, four could not be contacted, and one emigrated before the examination, leaving an eligible sample of 753 (390 women, 363 men). Of these, 524 (281 women, 243 men) accepted to participate (response rate 70%), while 229 declined participation. A total of 173 participants had previously been examined before age 70 as part of the PPSW study.
2.2. Description of the sample with baseline at age 75
In 2005–07, 1250 75-year-olds were invited. Among those, 24 could not participate due to language difficulties, 11 died before the examination, 17 could not be contacted, and two had emigrated, leaving an eligible sample of 1196 (684 women, 512 men). Of these, 767 (438 women, 329 men) accepted to participate (response rate 64%), while 429 declined participation. A total of 386 participants had previously been examined at age 70 and 116 had been examined before age 70 as part of the PPSW study.
2.3. Data collection procedures
The baseline examinations at age 70 and 75 included semi-structured somatic, psychiatric, dietary (at age 70 only), functional, and social interviews, as well as questions about medications. In addition, physical examinations (e.g., anthropometry, blood pressure, ECG, spirometry, gait speed, and grip strength), and tests of cognition and personality were performed. Biomarkers included blood sampling, genetic analyses, bioimpedance, and computed tomography of the brain (at age 70 only). All examinations are described in detail elsewhere (3). The characteristics examined in the attrition analyses are defined as follows:
Having a partner was defined as being married or cohabitant or having a partner but living separately. Educational level was dichotomised as having mandatory education (corresponding to 7 years) or less vs. more than mandatory education. Smoking was dichotomized as being a current smoker vs. past or never smoker. Alcohol risk consumption was defined according to the NIAAA guidelines as >98 g alcohol/week (16) and was based on self-reported alcohol consumption during the last month. Height and weight were measured, and body mass index (BMI) was calculated.
Blood pressure was measured with a manual sphygmomanometer in the right arm after five minutes' rest in a seated position. Peak Expiratory Flow (PEF) was measured with a Peak Flow Meter in liter per minute and calculated as percent of expected value based on sex, height, and age according the equation suggested by Hankinson et al. (17, 18). Self-selected indoor gait speed (30 meter in 2000 and 20 meter in 2005) with a standing start was measured in meters per second. Activities of daily living (ADL) was assessed according to the Katz Index of Independence in Activities of Daily Living (ADL) (19, 20), using six domains (bathing, dressing, toileting, transferring, continence, and feeding), and the Lawton Instrumental Activities of Daily Living (IADL) scale (21), where four domains were assessed (housekeeping, shopping, mode of transportation, and food preparation). The participants were classified as ADL/IADL dependent if dependent in at least one ADL or IADL domain. The total number of medications was recorded. Myocardial infarction was identified from self-reports, the National Patient Register (NPR) [International Classification of Diseases (ICD) 8-SE codes 410, 412.01, 412.09; ICD9-SE codes 410, 411A, 411C, 412; ICD10-SE codes I21-I23, I24.1, I25.2, I25.6, U98], or presence of major or intermediate Q-waves on ECG [Minnesota code (MC) 1-1-X or 1-2-X, excluding 1-2-6 and 1-2-8] (22). Atrial fibrillation or flutter was identified from close-informant interviews (in 2000), self-reports (in 2005), the NPR (ICD-8-SE code 427.92; ICD-9-SE code 427D; ICD-10-SE code I48), or ECGs (MC 8-3). Heart failure was identified from the NPR (ICD-8-SE code 427.00; ICD-9-SE code 428; ICD-10-SE code I11.0, I13.0, I13.2, I50). Diabetes mellitus was defined as present treatment with insulin or antidiabetic medications. Treatment for hypertension and hypercholesterolemia were defined as self-reported use of antihypertensive or lipid-lowering medication. Stroke was identified from self-reports and close-informant interviews, the NPR (ICD8-SE codes 431, 433, 434; ICD9-SE codes 431, 432, 434, 438; ICD10-SE codes I61-I63, I69.1-I69.4), and hospital medical records. Dementia was based on the Diagnostic and Statistical Manual of Mental Disorders, third edition revised (DSM-III-R), using combined information from neuropsychiatric examinations and close-informant interviews, as described in detail previously (6, 23, 24). The Montgomery-Åsberg Depression Rating Scale (MADRS) (25) was used to assess depressive symptoms and depression severity. Blood was drawn and DNA was extracted according to standard procedures. APOE genotyping was performed by KASPar® PCR SNP genotyping system (LGC Genomics, Hoddesdon, Herts, UK) or by mini-sequencing, as previously described in detail (26). Genotype data for the SNPs rs7412 and rs429358 were used to define ɛ2, ɛ3, and ɛ4 alleles. The cognitive tests included word fluency (name as many animals as possible in one minute), and a free recall test (repeat 12 shown objects after distraction).
2.4. Attrition during follow-up
The baseline participants were classified as participant or drop-out at each follow-up. Those who dropped out were classified as refusals, deceased, or other reasons for attrition, including contact failure, emigration, language difficulties, and technical reasons. Total attrition includes all reasons for attrition. Death dates were obtained from the Swedish Tax Agency.
2.5. Statistical analyses
Logistic regression was used to analyze associations between characteristics at ages 70 and 75 and attrition at each follow-up. Separate analyses were performed for each characteristic (as the predictor variable) in relation to three different types of attrition (as the outcome variable, i.e., refusal, death, and total attrition) compared to participation at each follow-up. Attrition due to death included the cumulative deaths from baseline until the specific examination.
First, unadjusted analyses were performed. Second, adjusted analyses were performed, including sex and education as potential covariates. Third, sensitivity analyses were performed for analyses including cognitive level where individuals with baseline dementia were excluded. No corrections for multiple testing were performed since avoiding type II errors (i.e., to fail to reject a null-hypothesis that is false) were regarded more important than avoiding type I errors (i.e., to reject a null-hypothesis that is actually true). A p-value < 0.05 (two-tailed) was considered statistically significant. Analyses were conducted in SPSS, version 29.0.
2.6. Ethics
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Regional Ethics Committee for Medical Research at the University of Gothenburg. Informed consent was obtained from the participants when possible. In cases where informed consent was not possible to obtain from the participant (e.g., due to dementia), informed consent was obtained from a close relative.
3. Results
Baselines characteristics at age 70 and 75, stratified by sex, are shown in Table 1.
3.1. Follow-up from age 70
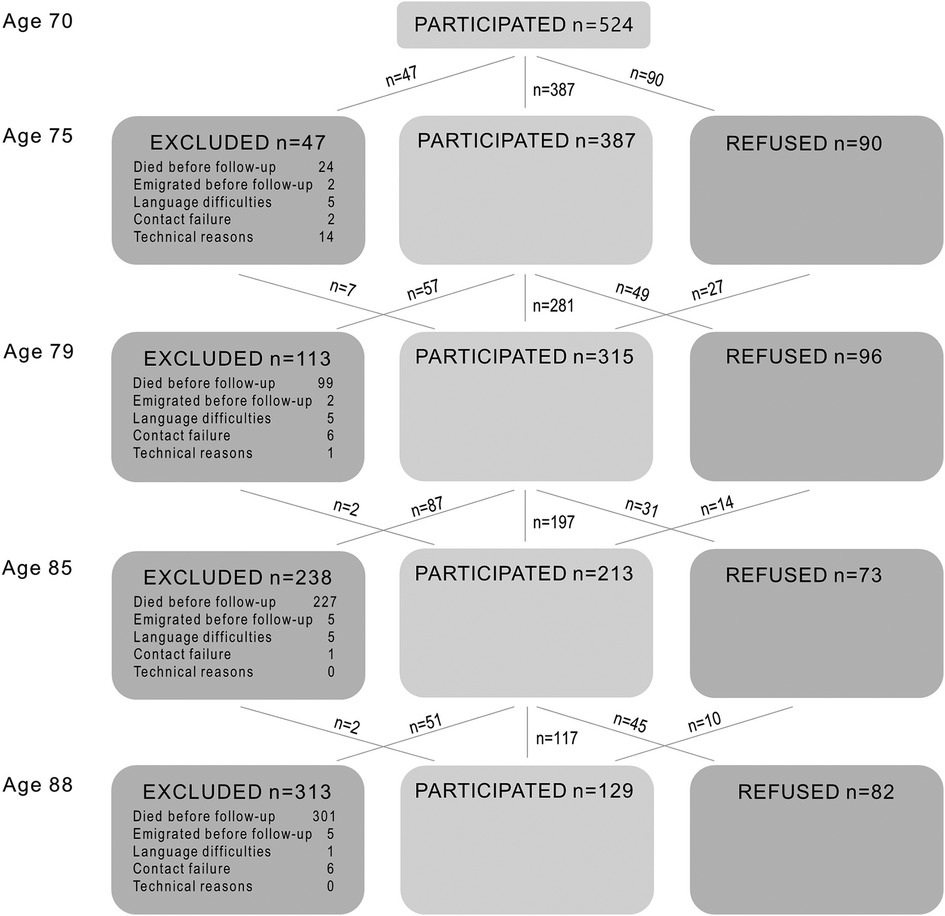
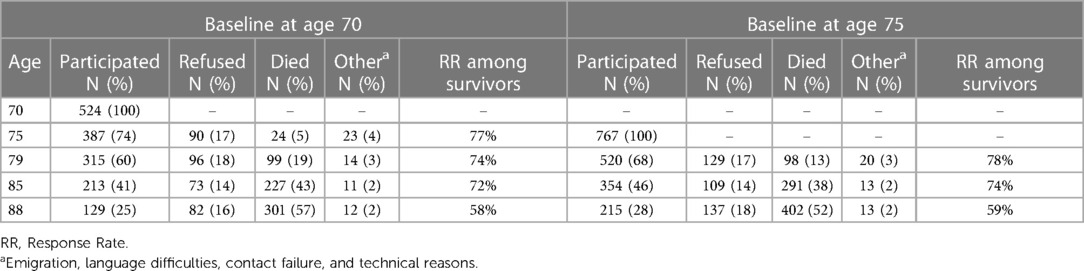
Table 2 shows the number and proportion of individuals who participated and refused participation at each follow-up, died before each follow-up, or dropped out for other reasons (i.e., contact failure, emigration, language difficulties, or technical reasons). In total, 97 individuals participated once, 110 participated twice, 125 participated three times, 84 participated four times, and 108 participated five times. Among the 524 who participated at baseline, 427 (81%) participated in at least one follow-up examination. The response rate among survivors was above 70% at all follow-ups, except at age 88, where the response rate among survivors was 58%. A flow chart of the sample is found in Figure 1.
3.2. Follow-up from age 75
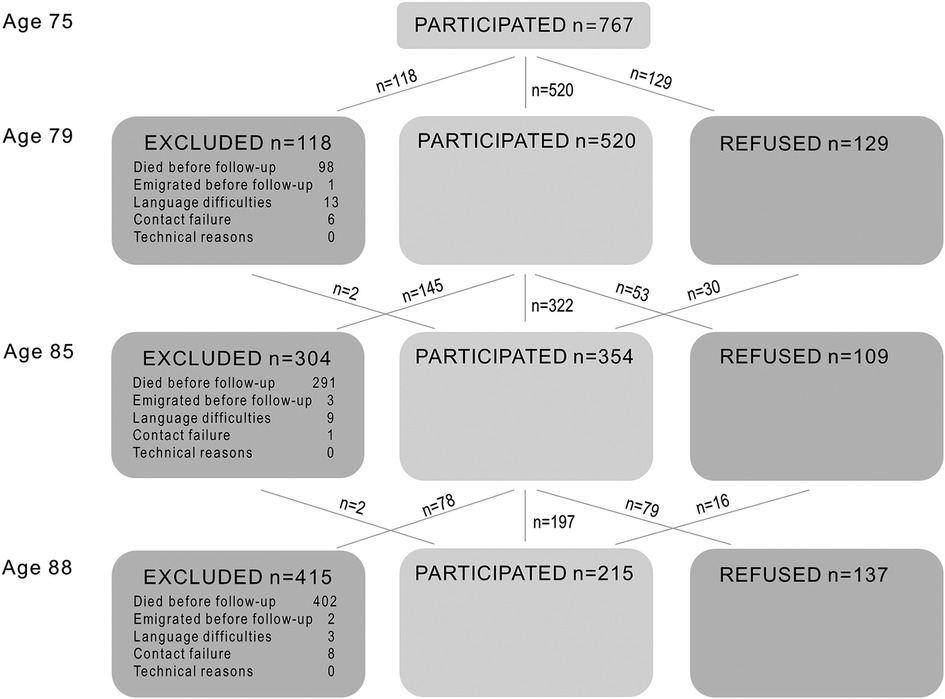
Table 2 shows the number and proportion of individuals who participated and refused at each follow-up, died before each follow-up, or dropped out for other reasons. In total, 208 individuals participated once, 216 participated twice, 156 participated three times, and 187 participated four times. Among the 767 who participated at age 75, 559 (73%) participated in at least one follow-up examination. The response rate among survivors was above 70% for all follow-ups, except at age 88, where the response rate among survivors was 59%. A flow chart of the sample is found in Figure 2.
3.3. Characteristics at age 70 in relation to attrition
Associations are only reported in the text if observed at more than one follow-up. Results for each follow-up examination are given in the tables.
First, we examined characteristics at age 70 in relation to refusal at each follow-up. In both unadjusted (Supplementary Table S1) and adjusted analyses (Table 3), lower educational level was associated with refusal.
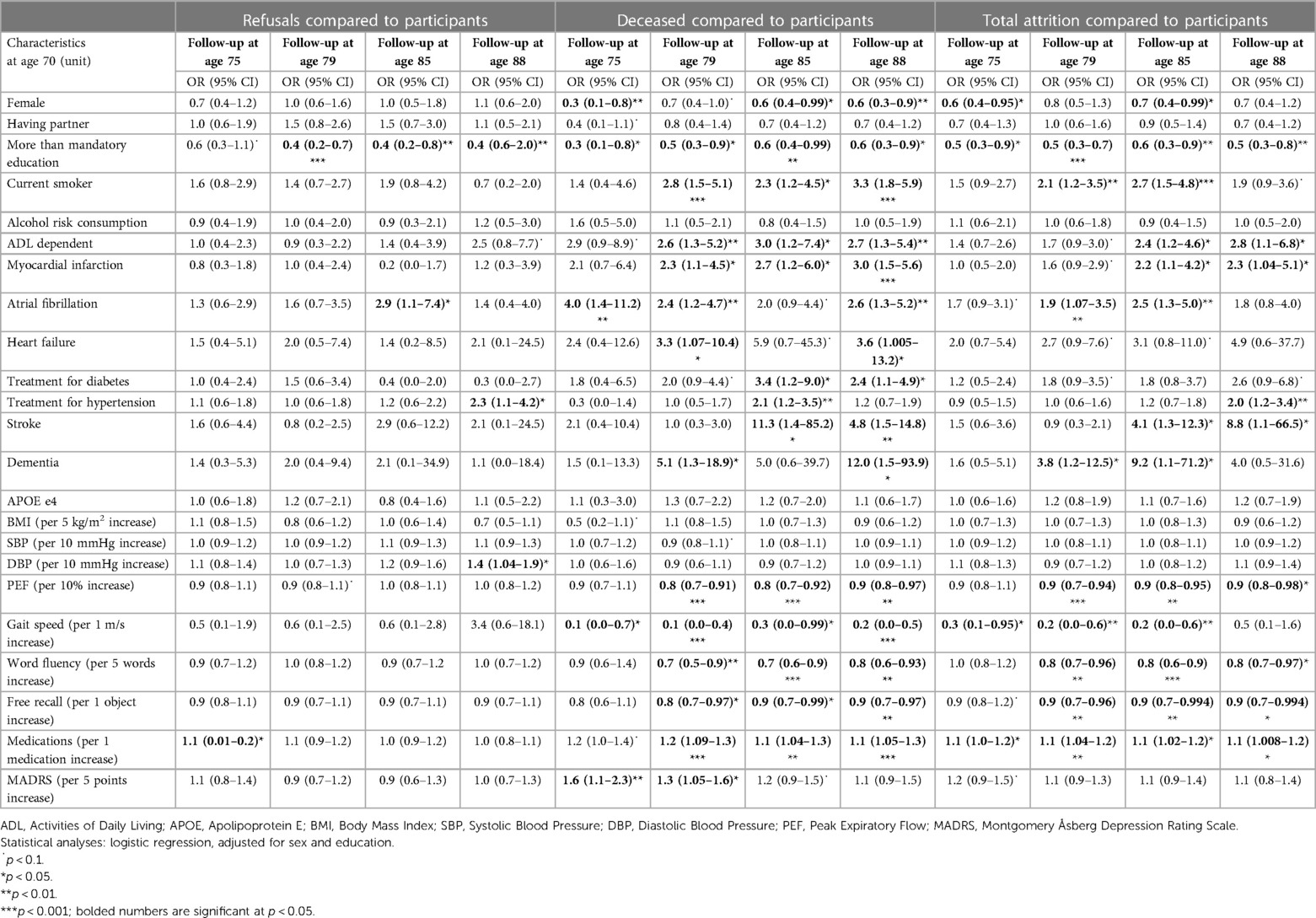
Table 3. Characteristics at age 70 associated with refusal, death, and total attrition during follow-up.
Second, we examined characteristics at age 70 in relation to attrition due to death before each follow-up. In both unadjusted (Supplementary Table S2) and adjusted (Table 3) analyses, male sex, lower educational level, smoking, ADL dependency, myocardial infarction, atrial fibrillation, heart failure, diabetes, stroke, dementia, lower PEF, slower gait speed, lower scores on cognitive tests, larger number of medications, and higher MADRS scores were associated with attrition due to death.
Third, we examined characteristics at age 70 in relation to total attrition before each follow-up. In both unadjusted (Supplementary Table S3) and adjusted analyses (Table 3), lower educational level, smoking, ADL dependency, stroke, dementia, lower PEF, slower gait speed, lower scores on cognitive tests, and larger number of medications were associated with total attrition. In addition, heart failure was associated with total attrition in the unadjusted analyses and male sex, myocardial infarction, and atrial fibrillation were associated with total attrition in the adjusted analyses.
All results including scores on cognitive tests remained when excluding individuals with baseline dementia.
3.4. Characteristics at age 75 in relation to attrition
First, we examined characteristics at age 75 in relation to refusal at each follow-up. In both unadjusted (Supplementary Table S4) and adjusted analyses (Table 4), lower educational level, higher blood pressure, and lower scores on cognitive tests were associated with refusal.
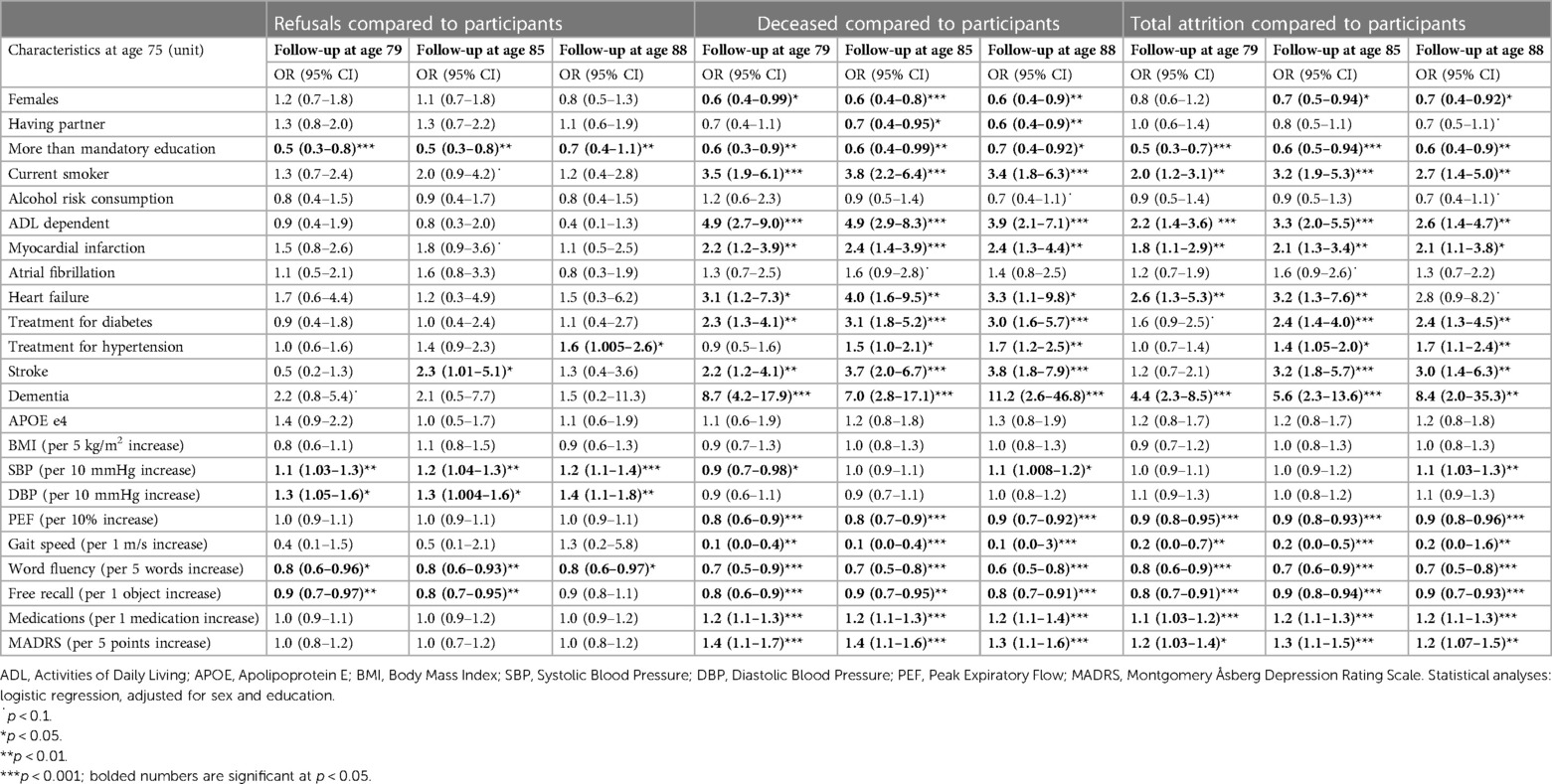
Table 4. Characteristics at age 75 associated with refusal, death, and total attrition during follow-up.
Second, we examined characteristics at age 75 in relation to attrition due to death before each follow-up. In both unadjusted (Supplementary Table S5) and adjusted (Table 4) analyses, male sex, lower educational level, smoking, ADL dependency, myocardial infarction, heart failure, diabetes, hypertension, stroke, dementia, lower PEF, slower gait speed, lower scores on cognitive tests, larger number of medications, and higher MADRS scores were associated with attrition due to death. Lower SBP was associated with attrition due to death before age 79, while higher SBP was associated with attrition due to death before age 88. In addition, not having a partner was associated with attrition due to death in the adjusted analyses.
Third, we examined characteristics at age 75 in relation to total attrition before each follow-up. In both unadjusted (Supplementary Table S6) and adjusted (Table 4) analyses, male sex, lower educational level, smoking, ADL dependency, myocardial infarction, heart failure, diabetes, hypertension, stroke, dementia, lower PEF, slower gait speed, lower scores on cognitive tests, larger number of medications, and higher MADRS score were associated with total attrition.
All results including scores on cognitive tests remained when excluding individuals with baseline dementia.
4. Discussion
This paper describes longitudinal attrition in the 1930 cohort of the Gothenburg H70 Birth Cohort Studies, followed from age 70 or 75 to age 88. Lower educational and cognitive level at baseline were related to attrition due to both refusal and death. In addition, male sex, and a large number of health-related factors were related to attrition due to death. Thus, both non-death attrition and attrition due to death made the sample more selected over time, which is important to consider when evaluating results from longitudinal studies among older adults.
Among the various reasons for attrition, non-death attrition is suggested to be the most important factor in relation to representativeness, since death occurs both in the sample and in the target population (1). We found that lower cognitive and educational level were repeatedly associated with refusal at both short- and long-term follow-up. These results are in line with two previous literature reviews reporting that cognitive impairment (27, 28) and fewer years of education (27) are two of the most important factors for non-death attrition, in addition to high age (27, 28) and lower socio-economic status (27). The Medical Research Council on Cognitive Function and Ageing Study (MRC CFAS) analyzed refusals separately from other types of non-death attrition and found also that those with poorer cognitive ability and fewer years of education were more likely to refuse participation (29). This may impact longitudinal studies on disorders where lower educational and cognitive level at baseline are risk factors or determinants of the outcome, e.g., studies on dementia incidence. Other factors repeatedly studied in relation to non-death attrition are factors related to health and functional status. However, these results are more disparate (27, 28). We found no associations between refusal and indicators for poor baseline health (e.g., number of medications, gait speed, lung function, heart disease, diabetes, depressive symptoms, stroke, dementia, ADL-dependency), with the exception of blood pressure levels where those with higher blood pressure were more likely to refuse subsequent examinations. One reason why most indicators for poor health were not associated with refusal in our study may be that disorders leading to refusal might also have developed after baseline, which is especially important in studies with long follow-up and at high ages. In addition, those with disorders at baseline (when baseline was at age 75) died more often before follow-up and could therefore not refuse. Another reason may be that we offered home visits for those who were too ill to come to the outpatient department, lowering the threshold for participation. Findings regarding the influence of sex on refusal are also disparate. It has been reported that men are less likely to participate, that women are less likely to participate or, as in our study, that sex was not associated with refusal (27).
We found that a large number of social and health related factors were related to attrition due to death. In concordance with MRC CFAS (29), we found that male sex, smoking, ADL dependency, and lower cognitive level were associated with attrition due to death. In addition, we found that number of medications, heart diseases, poorer lung function, and higher MADRS score were associated with attrition due to death. However, although MRC CFAS found that poor self-perceived health was associated with attrition due to death, they did not find any associations with chronic disorders or self-reported depression. One reason for the disparate results may be the shorter follow-up time of two years in the MRC CFAS study, compared to the three to 18-year follow-up in the present study. Regarding blood pressure level, we found that lower SBP at age 75 was associated with attrition due to death at short-term follow-up, while higher SBP at age 75 was associated with attrition due to death at long-term follow-up. One reason may be that high blood pressure is a risk factor for several disorders in the longer perspective, while disorders that have already started to develop may lower blood pressure. One example is that studies on the relation between blood pressure and dementia report that blood pressure declines during the years before dementia onset (4) and is lower in those who already have started to develop the disease (30), while high blood pressure is a risk factor for dementia in the longer perspective (4).
Selective survival during follow-up may introduce bias in association studies if the exposure or outcome is related to survival (2, 31). For example, we found that both dementia and potential risk factors for dementia, such as lower educational level, smoking, and heart diseases were associated with attrition due to death, which may bias the impact of these risk factors on dementia if not accounted for. Thus, studies on risk factors for dementia are influenced by both attrition due to refusal and death.
As mentioned before, non-death attrition is most important for representativeness. If for example low educational level is less common in the sample than the target population at baseline, this selection bias will increase over time if low educational level is also associated with refusal during follow-up. However, also death affect representativeness of the sample in relation to the target population. If low educational level is associated with death, representativeness of the examined sample may actually increase over time, or at least, the increasing selection bias caused by refusal may be reduced. This is however only true if the prevalence of low education is less than half (1). If the prevalence is more than half in the examined sample and the target population, representativeness will instead decrease during follow-up (1). This illustrates the importance of describing and analysing different types of attrition separately, since they may affect representativeness in different directions.
A strength of the present study is the possibility to analyse a large number of characteristics in relation to different types of attrition (i.e., refusal, death, and total attrition) in a longitudinal population-based sample of older adults followed over 18 years. Another strength is the use of different sources of information, including interviews and physical examinations performed by health professionals, and access to high quality register data. However, there are also limitations. First, the number of some characteristics were small, and missing data was more prevalent for some characteristics (gait speed and ADL dependency), leading to lower power and increasing the risk of bias. Second, the ability to communicate in Swedish was an inclusion criterion at baseline, limiting generalisability to the total population in Gothenburg.
5. Conclusions
Since attrition due to death and non-death attrition may impact representativeness and study results differently it is important to consider them separately. We found that the main characteristics associated with attrition due to refusal were lower educational level, higher blood pressure, and lower scores on cognitive tests. This could be handled when planning the study by reducing barriers to participation, but also oversampling individuals more likely to drop-out such as individuals with lower educational level. One further possibility is to compensate for this afterwards by using weighted analyses. Characteristics associated with attrition due to death were male sex, lower educational and cognitive level, and several health-related factors. Therefore, when including these variables in longitudinal analyses, it is important to use models handling the competing risk of death. This is especially important when studying older adults or other groups where death rates are high.
Data availability statement
All data and analyses generated during the current study are available from the corresponding author on reasonable request.
Ethics statement
The studies involving human participants were reviewed and approved by the Regional Ethics Committee for Medical Research at the University of Gothenburg. The patients/participants provided their written informed consent to participate in this study.
Author contributions
LR, HW, and IS had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design LR, HW, and IS Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: LR, HW, and IS Statistical analysis: LR and HW Principal investigator: IS Critical revision of the manuscript for important intellectual content: All authors contributed to the article and approved the submitted version.
Funding
This work was supported by grants from the Swedish state under the agreement between the Swedish government and the county councils, the ALF-agreement [ALF 716681, ALFGBG-81392, ALF GBG-771071, ALFGBG-637271, ALFGBG 147361, ALFGBG-715841]; Stena Foundation; Swedish Research Council [11267, 2005-8460, 2007-7462, 2012-5041, 2015-02830, 2016-01590, 2019-01096, 2013-8717, NEAR 2017-00639, 2019-02075]; Swedish Research Council for Health, Working Life and Welfare [2004-0145, 2006-0596, 2008-1111, 2010-0870, 2013-1202, 2018-00471, 2001-2646, 2003-0234, 2004-0150, 2006-0020, 2008-1229, 2012-1138, AGECAP 2013-2300, 2013-2496]; Konung Gustaf V:s och Drottning Victorias Frimurarestiftelse, Hjärnfonden [FO2014-0207, FO2016-0214, FO2018-0214, FO2019-0163, FO2020-0235]; Alzheimerfonden [AF-554461, AF-647651, AF-743701, AF-844671, AF-930868, AF-940139, AF-842471, AF-737641], Eivind och Elsa K:son Sylvans stiftelse, The Alzheimer's Association Zenith Award [ZEN-01-3151]; The Alzheimer's Association Stephanie B. Overstreet Scholars [IIRG-00-2159]; The Bank of Sweden Tercentenary Foundation; Stiftelsen Söderström-Königska Sjukhemmet; Stiftelsen för Gamla Tjänarinnor; Handlanden Hjalmar Svenssons Forskningsfond; Stiftelsen Demensfonden; Stiftelsen Wilhelm och Martina Lundgrens vetenskapsfond; and the Sahlgrenska Academy Homecoming Fellowship [V2012/294]. The authors had complete freedom to design the study and collect, analyse, and interpret the data and to write the manuscript without influence from any sponsors.
Acknowledgments
The authors would like to thank all participants of the H70 studies in Gothenburg, and the research group members for their contribution to data collection and management. We also acknowledge seminal contributions to this study by the late Dr. Svante Östling.
Conflict of interest
SK has served at scientific advisory boards and/or as consultant for Geras Solutions and Biogen. EJ is currently employed at IQVIA, SE-431 44, Mölndal, Sweden. The other authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fepid.2023.1151519/full#supplementary-material
References
1. Brilleman SL, Pachana NA, Dobson AJ. The impact of attrition on the representativeness of cohort studies of older people. BMC Med Res Methodol. (2010) 10:71. doi: 10.1186/1471-2288-10-71
2. Mayeda ER, Tchetgen Tchetgen EJ, Power MC, Weuve J, Jacqmin-Gadda H, Marden JR, et al. A simulation platform for quantifying survival bias: an application to research on determinants of cognitive decline. Am J Epidemiol. (2016) 184:378–87. doi: 10.1093/aje/kwv451
3. Rydberg Sterner T, Ahlner F, Blennow K, Dahlin-Ivanoff S, Falk H, Havstam Johansson L, et al. The Gothenburg H70 birth cohort study 2014-16: design, methods and study population. Eur J Epidemiol. (2019) 34:191–209. doi: 10.1007/s10654-018-0459-8
4. Skoog I, Lernfelt B, Landahl S, Palmertz B, Andreasson LA, Nilsson L, et al. 15-year Longitudinal study of blood pressure and dementia. Lancet. (1996) 347:1141–5. doi: 10.1016/S0140-6736(96)90608-X
5. Gustafson D, Rothenberg E, Blennow K, Steen B, Skoog I. An 18-year follow-up of overweight and risk of Alzheimer disease. Arch Intern Med. (2003) 163:1524–8. doi: 10.1001/archinte.163.13.1524
6. Rydén L, Zettergren A, Seidu NM, Guo X, Kern S, Blennow K, et al. Atrial fibrillation increases the risk of dementia amongst older adults even in the absence of stroke. J Intern Med. (2019) 286:101–10. doi: 10.1111/joim.12902
7. Gudmundsson P, Olesen PJ, Simoni M, Pantoni L, Östling S, Kern S, et al. White matter lesions and temporal lobe atrophy related to incidence of both dementia and major depression in 70-year-olds followed over 10 years. Eur J Neurol. (2015) 22:781–8.e49-50. doi: 10.1111/ene.12651
8. Jaraj D, Wikkelsø C, Rabiei K, Marlow T, Jensen C, Östling S, et al. Mortality and risk of dementia in normal-pressure hydrocephalus: a population study. Alzheimers Dement. (2017) 13:850–7. doi: 10.1016/j.jalz.2017.01.013
9. Najar J, van der Lee SJ, Joas E, Wetterberg H, Hardy J, Guerreiro R, et al. Polygenic risk scores for Alzheimer's disease are related to dementia risk in APOE ɛ4 negatives. Alzheimers Dement (Amst). (2021) 13:e12142. doi: 10.1002/dad2.12142
10. Skoog I, Waern M, Duberstein P, Blennow K, Zetterberg H, Börjesson-Hanson A, et al. A 9-year prospective population-based study on the association between the APOE*E4 allele and late-life depression in Sweden. Biol Psychiatry. (2015) 78:730–6. doi: 10.1016/j.biopsych.2015.01.006
11. Bäckman K, Joas E, Falk H, Mitnitski A, Rockwood K, Skoog I. Changes in the lethality of frailty over 30 years: evidence from two cohorts of 70-year-olds in Gothenburg Sweden. J Gerontol A Biol Sci Med Sci. (2017) 72:945–50. doi: 10.1093/gerona/glw160
12. Sacuiu S, Gustafson D, Sjögren M, Guo X, Ostling S, Johansson B, et al. Secular changes in cognitive predictors of dementia and mortality in 70-year-olds. Neurology. (2010) 75:779–85. doi: 10.1212/WNL.0b013e3181f0737c
13. Lak VW, Skoog I, Guo X. Secular trends in lung function and its relation to survival in Swedish 75 year olds 1976-2006. Age Ageing. (2012) 41:735–40. doi: 10.1093/ageing/afs098
14. Wetterberg H, Rydén L, Ahlner F, Falk Erhag H, Gudmundsson P, Guo X, et al. Representativeness in population-based studies of older adults: five waves of cross-sectional examinations in the Gothenburg H70 birth cohort study. BMJ Open. (2022) 12:e068165. doi: 10.1136/bmjopen-2022-068165
15. Lissner L, Skoog I, Andersson K, Beckman N, Sundh V, Waern M, et al. Participation bias in longitudinal studies: experience from the population study of women in Gothenburg, Sweden. Scand J Prim Health Care. (2003) 21:242–7. doi: 10.1080/02813430310003309-1693
16. Ahlner F, Falk Erhag H, Johansson L, Mellqvist Fässberg M, Rydberg Sterner T, Samuelsson J, et al. Patterns of alcohol consumption and associated factors in a population-based sample of 70-year-olds: data from the Gothenburg H70 birth cohort study 2014-16. Int J Environ Res Public Health. (2022) 19:8248. doi: 10.3390/ijerph19148248
17. Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. Population. Am J Respir Crit Care Med. (1999) 159:179–87. doi: 10.1164/ajrccm.159.1.9712108
18. Radeos MS, Camargo CA Jr. Predicted peak expiratory flow: differences across formulae in the literature. Am J Emerg Med. (2004) 22:516–21. doi: 10.1016/j.ajem.2004.08.018
19. Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. Gerontologist. (1970) 10:20–30. doi: 10.1093/geront/10.1_Part_1.20
20. Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psycholsocial function. Jama. (1963) 185:914–9. doi: 10.1001/jama.1963.03060120024016
21. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. (1969) 9:179–86. doi: 10.1093/geront/9.3_Part_1.179
22. Ammar KA, Kors JA, Yawn BP, Rodeheffer RJ. Defining unrecognized myocardial infarction: a call for standardized electrocardiographic diagnostic criteria. Am Heart J. (2004) 148:277–84. doi: 10.1016/j.ahj.2004.03.019
23. Guo X, Östling S, Kern S, Johansson L, Skoog I. Increased risk for dementia both before and after stroke: a population-based study in women followed over 44 years. Alzheimers Dement. (2018) 14:1253–60. doi: 10.1016/j.jalz.2018.05.009
24. Skoog I, Nilsson L, Palmertz B, Andreasson LA, Svanborg A. A population-based study of dementia in 85-year-olds. N Engl J Med. (1993) 328:153–8. doi: 10.1056/NEJM199301213280301
25. Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. (1979) 134:382–9. doi: 10.1192/bjp.134.4.382
26. Blennow K, Ricksten A, Prince JA, Brookes AJ, Emahazion T, Wasslavik C, et al. No association between the alpha2-macroglobulin (A2M) deletion and Alzheimer's disease, and no change in A2M mRNA, protein, or protein expression. J Neural Transm (Vienna). (2000) 107:1065–79. doi: 10.1007/s007020070052
27. Bhamra S, Tinker A, Mein G, Ashcroft R, Askham J. The retention of older people in longitudinal studies: a review of the literature. Qual Ageing Older Adults. (2008) 9:27–35. doi: 10.1108/14717794200800025
28. Chatfield MD, Brayne CE, Matthews FE. A systematic literature review of attrition between waves in longitudinal studies in the elderly shows a consistent pattern of dropout between differing studies. J Clin Epidemiol. (2005) 58:13–9. doi: 10.1016/j.jclinepi.2004.05.006
29. Matthews FE, Chatfield M, Freeman C, McCracken C, Brayne C. Attrition and bias in the MRC cognitive function and ageing study: an epidemiological investigation. BMC Public Health. (2004) 4:12. doi: 10.1186/1471-2458-4-12
30. Ribbe M, Kern S, Wetterberg H, Rydén L, Zettergren A, Guo X, et al. Time trends in the relation between blood pressure and dementia in 85-year-olds. J Hypertens. (2021) 39:1964–71. doi: 10.1097/HJH.0000000000002902
Keywords: attrition, population studies, drop out, epidemiogy, representativeness
Citation: Rydén L, Wetterberg H, Ahlner F, Falk Erhag H, Gudmundsson P, Guo X, Joas E, Johansson L, Kern S, Mellqvist Fässberg M, Najar J, Ribbe M, Rydberg Sterner T, Sacuiu S, Samuelsson J, Sigström R, Skoog J, Waern M, Zettergren A and Skoog I (2023) Attrition in the Gothenburg H70 birth cohort studies, an 18-year follow-up of the 1930 cohort. Front. Epidemiol. 3:1151519. doi: 10.3389/fepid.2023.1151519
Received: 26 January 2023; Accepted: 17 April 2023;
Published: 9 May 2023.
Edited by:
Ralph Brinks, University Witten/Herdecke, GermanyReviewed by:
Pengpeng Ye, Chinese Center For Disease Control and Prevention, ChinaZhengyang Zhou, University of North Texas Health Science Center, United States
© 2023 Rydén, Wetterberg, Ahlner, Falk Erhag, Gudmundsson, Guo, Joas, Johansson, Kern, Mellqvist Fässberg, Najar, Ribbe, Rydberg Sterner, Sacuiu, Samuelsson, Sigström, Skoog, Waern, Zettergren and Skoog. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lina Rydén lina.ryden@gu.se
†These authors share first authorship
 Lina Rydén
Lina Rydén Hanna Wetterberg1,2,†
Hanna Wetterberg1,2,†  Felicia Ahlner
Felicia Ahlner Silke Kern
Silke Kern Jenna Najar
Jenna Najar Therese Rydberg Sterner
Therese Rydberg Sterner Robert Sigström
Robert Sigström Johan Skoog
Johan Skoog Margda Waern
Margda Waern Anna Zettergren
Anna Zettergren