Are Non-woven Gowns Safe for Dental Professionals? A Preclinical Double-Blind Study
- 1Department of Dental Clinic, Federal Fluminense University School of Dentistry, Niterói, Brazil
- 2Federal Fluminense University School of Dentistry, Niterói, Brazil
- 3Brazilian Army Dental Clinic, Rio de Janeiro, Brazil
With the advent of the coronavirus disease 2019 (COVID-19) pandemic, the risk of dental professional's infection increases exponentially due to aerosol-generating procedures. The protective performance of dental professional gown fabrics is a major challenge against microorganisms and aerosols. Globally, health care workers wear gowns manufactured with non-woven fabrics. However, these professionals may have a false greater sense of protection based on the greater weight of the gown's fabric. This study evaluated whether aerosol generated by dental procedures has the potential to pass through three different non-woven weights (40, 60, and 80 g/m2). Single and folded formats of each weight were analyzed. The positions of the mannequin and the high-speed handpiece were standardized. The non-woven samples were placed over a sheet of sulfite paper and fixed on a marked position of a standardized smooth surface, 10 cm away from the end of the mannequin's head, simulating the dental professional body. For better visualization, the water used in the equipment was tinted with water-soluble red artificial dye. Blind to the nature of the groups, one researcher started the 5 uninterrupted min of aerosol production. The sheets were randomized coded, so that the samples could not be identified by the evaluator. Another researcher, blind to the tests, scanned all sheets and the images were analyzed by ImageJ software. The groups showed significant differences (p < 0.01). Except for the folded 80 g/m2, all groups presented pigmented mean areas ranging from 16.18% (60 g/m2 folded) to 35.68% (40 g/m2 single), suggesting that the one-layer non-woven samples were not effective as barriers for 5 uninterrupted min of aerosol spray. Dental procedures exceeding the studied time may provide different results with the non-woven 80 g/m2 folded. Dental health workers, who are exposed daily to aerosol-generating procedures, should be aware of the exact specification and performance of the fabrics used in the manufacturing of their disposable garments. If the use of an impermeable surgical gown is not possible during aerosol-generating procedures, a plastic garment associated with a disposable gown should be worn, as recommended by the World Health Organization.
Introduction
The coronavirus [severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)] has been showing a high risk of contamination among health care professionals (1). A recent clinical study demonstrated that 29% of 138 hospitalized patients with coronavirus disease 2019 (COVID-19)-infected pneumonia in Wuhan, China, were health care workers (2). The risk of exposure to SARS-CoV-2 is not limited to medical professionals who work in hospitals but also to dental professionals who work in dental schools and private practices. The transmission of SARS-CoV-2 occurs by contact, droplets, and airborne routes (3). Evidence suggests that human-to-human transmission may be occurring during the asymptomatic incubation period, which can be up to 10 days (4). The presence of viral loads in the lower and upper respiratory tract (5), associated with the persistence of viable virus in aerosol for 3 h in the air and until 72 h on surfaces, evidences the risk of contamination of dental workers (6).
The use of infection control universal precautions by dental professionals has been based on the assumption of infectious blood-borne viruses, such as hepatitis B virus, hepatitis C virus, and HIV (7). With the advent of the COVID-19 pandemic, the risk of dental professional's infection increases exponentially due to the amount of procedures that aerosolize the saliva during clinical care (7). Dental high-speed handpieces, ultrasonic scalers, and all instruments that use water sprays and compressed air produce airborne particles. Besides that, dental professionals cannot follow the recommendations of the distance between 1 and 2 m from the patient during dental procedures (8). For these reasons, it is essential for dental professionals to improve strategies to prevent exposure to the COVID-19 virus (9).
The World Health Organization (WHO) reported a guideline for infection prevention of health care workers. The principal recommendation was the use of personal protective equipment (PPE). The long-sleeved disposable gown is one of the PPEs recommended to protect the professional in contact with the patient, especially for aerosol-generating procedures (10, 11). Non-woven fabrics have been used to manufacture medical and dental disposable gowns. This material is made by forming fibrous webs directly from fibers or polymer granules. Materials used in surgical gowns should function as protective barriers against the transfer of microorganisms, particulates, and aqueous fluids to minimize the risk of personnel contamination (12). However, many sellers and most of the users of these protective gowns are not aware of the exact specification and performance requirement of the fabrics used for health workers' garments. In dental practice, the fabric used in the manufacturing of the professional gowns should not only avoid the penetration of microorganisms but also avoid exposure of dental professionals to aerosols containing saliva and blood.
Regarding the lack of literature about the efficiency of the protective non-woven capacity of preventing the penetration of aqueous fluid and aiming to answer the question if non-woven fabrics are safe for use as dental professional gowns, this preclinical blind study aimed to evaluate whether the aerosols and droplets generated by handpieces during dental procedures have the potential to pass through three different non-woven weights.
Materials and Methods
Study Design
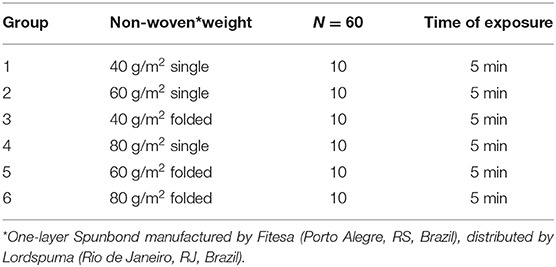
This preclinical double-blind study compared three different weights of non-woven fabric. Polypropylene fibers were used in the composition of all non-woven samples tested in our study. The three weights were tested in single and folded formats, totaling six groups. All groups were exposed to 5 min of aerosol-generating procedures (Table 1).
Test Procedures
The aerosol generated by a dental high-speed handpiece followed the recommendation of a water flow > 30 ml/min for optimal cooling of a #3216 diamond drill (KG Sorensen, Cotia, SP, Brazil), simulating the preparation of a full crown of an upper central incisor on a mannequin attached to a dental chair (7). For better visualization, the water used in the equipment was tinted with water-soluble red artificial dye (Tempemar Comercial de Alimentos LTDA) in the proportion of 10 m/L.
In order to standardize the procedures, the test position was calculated considering the mean of five dental professional heights and their distance from the patient, on a 12-h working position, respecting the principles of ergonomics. Figure 1 shows an example of a 12-h working position. The mannequin was positioned 70 cm from the ground, the samples were placed 10 cm away from the end of the mannequin's head, over a smooth surface, which simulated the dental professional body, and the handpiece was affixed to a stand, aiming to reproduce the same position in all tests. Prior to the tests, the procedure was performed once in order to visualize where the greatest aerosol flow would reach the smooth surface in order to place all samples in the same marked position (EB and EV). Each non-woven sample referring to each group was coded and placed over a sheet of sulfite paper and fixed on the marked position (LS). Blind to the nature of the groups, another researcher (GS), started the 5 uninterrupted min of aerosol production (Figure 2). The same researcher carefully removed the paper sheet and hanged to dry for 48 h. Another researcher (VF), blind to the test, scanned all sheets of paper in 300 DPI (Epson L375–Epson do Brazil LTDA, Barueri, SP, Brazil). However, prior to the analysis, to set up a reference, blank pieces of paper (n = 10) were analyzed by ImageJ v1.53a (Wayne Rasband, National Institutes of Health, USA). Each acquired image was transformed to a 16-bit file, and the auto-threshold reached a mean limit of 230 sensitivity level. All sheets were then analyzed using the same sensitivity level. The pigmented areas (different from white) were measured using the “particles analysis tool.” All obtained measurements were recorded and sent to an SPSS datasheet for statistical analysis. The values of the measured area were compared using Kruskal–Wallis test (SPSS Version 22.0, IBM Corp., Armonk, NY).

Figure 2. Standardized positions of the mannequin, high-speed handpiece, and the sample. Note the aerosols and particles toward the non-woven fabric.
Results
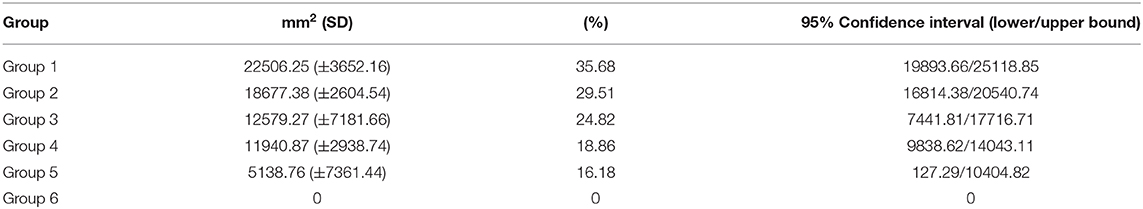
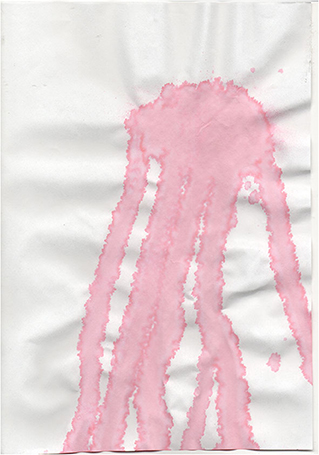
Table 2 shows the mean areas and standard deviations of each group. The groups showed significant differences (Kruskal–Wallis; p < 0.01). Group 6 presented a constant of no pigmented areas, unlike all the other evaluated groups. Except for group 6, all groups presented pigmented areas suggesting that the one-layer non-woven samples were not effective as barriers for 5 uninterrupted min of aerosol production. Dental procedures exceeding the studied time may provide different results with the non-woven 80 g/m2 folded. Figure 3 shows the distribution of pigmented areas. Note that group 6 is the only one that did not present a pigmented area, constituting a barrier against aerosol contamination for a period of 5 min. Figure 4 shows an extreme example of pigmentation after natural drying.
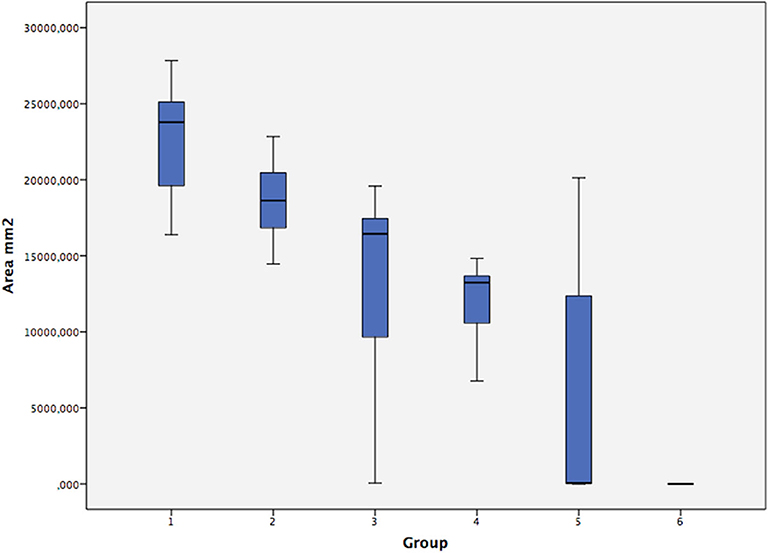
Figure 3. Boxplot showing the confidence limits and means of the sample areas evaluated for each group.
Discussion
This preclinical double-blind study aimed to evaluate whether the aerosols and droplets generated by a high-speed handpiece during a simulation of a dental procedure had the potential to pass through different weights of one-layer non-woven fabrics. Our results showed that except for group 6 (80 g/m2 folded), all groups presented pigmented areas ranging from 16.18 to 35.68%, suggesting that the one-layer non-woven samples were not effective barriers for 5 uninterrupted min of aerosol-generating dental procedures. The protective performance of surgical gown fabrics is a major challenge against microorganisms and aqueous fluids (13). Unfortunately, most of the users of these protective clothing are not aware of the exact specifications and performance requirements of the fabrics used for their protection. Despite the weights of 60 g/m2 (single or folded) and 80 g/m2 (single) may bring the idea of safe protections, our results showed they are non-impermeable, showing to be inefficient as a safe barrier. Although group 6 (80 g/m2 folded) did not show aerosol penetration, it is good to emphasize that 5 min seems to be a minimum working time to prepare one full crown. We recommend longer exposure time tests, simulating other dental procedures that require longer execution times. In addition, the sensibility used in the ImageJ test was 230. A higher sensibility test may present different results.
There is a significant research gap regarding the epidemiology of acute respiratory infection transmission from patients to health care workers during aerosol-generating procedures. This gap is compounded by a lack of precision in the literature with regard to the definition of aerosol-generating procedures (10). Aerosols were defined as particles <50 μm in diameter, and the smaller particles (0.5–10 μm in diameter) have the potential to penetrate the lungs and transmit infections (14). There are potential sources of aerosols and air-borne contamination during dental treatment, such as the use of high-speed handpieces and ultrasonic scalers containing aerosolized saliva and blood and patient respiratory source. It should be emphasized that these contaminated aerosols are not well visible to patients and dental personnel (7). In addition, the tests used to evaluate liquid penetration by impact or spray include the AATCC TM42 and NWSP 80.3. These tests aim to provide materials' certification so that the fabrics can be commercialized. However, the time used for exposure to the liquid (<5 s) by impact or spray in those tests does not simulate the dentist's exposure to aerosols during operatory procedures. In the present study, which did not aim to certificate the investigated products, but to inform the dental workers about the product they are possibly purchasing as PPE, the visual method was chosen to test the samples' wettability. By tinting the water with a red dye, a better visualization of the area (cm2) passing through the non-woven fabric was possible.
Economic advantage has driven the rapid development of non-woven fabrics. There is a large body of literature available for more in-depth discussions of the general non-woven processes and products (15–18), but basically, they should be barrier resistant as well as comfortable to wear. Dental non-woven gowns should resist the penetration of liquids and, at the same time, be sterile, breathable, flexible, and inexpensive (19). In the present study, all samples of different Spunbond weights, single or folded, showed water penetration, with the exception of the 80 g/m2 folded.
The major strength of this manuscript is the analysis of an item of the PPE during the COVID-19 pandemic. This is very important for health care workers, mainly for dental professionals who have the highest risk for SARS-CoV-2 contagiousness. In addition, this study used an innovative methodology, simulating the real exposure of dental professionals during aerosol-generating procedures. However, no suction device was used in this methodology. In most countries, suction tip has been used to suction saliva, not the aerosol. Our study alerted the health care professionals to the risk of being exposed to aerosols and to the false sensation of the greater non-woven weight, the greater protection should be reassessed. Therefore, future studies should focus on breathable, impermeable, and comfortable fabrics, which also offer microorganisms' barriers, ensuring safety for health care workers, especially for those who work in a contaminated environment.
Conclusions
Different weights (single or folded) of one-layer non-woven fabrics did not inhibit aerosol penetration during a simulation of a 5-min aerosol-generating dental procedure, with the exception of the 80 g/m2 folded. Dental procedures exceeding the studied time may provide different results for the non-woven 80g/m2 folded.
Dental health workers, who are exposed daily to aerosol-generating procedures should be aware of the exact specification and performance of the fabrics used in the manufacturing of their disposable garments.
If the use of an impermeable PPE is not possible during aerosol-generating procedures, a plastic garment associated with a disposable PPE should be worn, as recommended by the World Health Organization.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Written informed consent was taken from the individuals pictured.
Author Contributions
EB contributed to the conceptualization, methodology, investigation, project supervision, writing the original draft, and final editing. GS, LS, and EV contributed to the methodology and investigation. CM and VF wrote the original draft and organized the database. VF performed the statistical analysis. All authors contributed to the article and approved the submitted version.
Funding
This work was supported in part by the Coordenação de Aperfeiçoamento de Pessoal de Nivel Superior-Brasil (CAPES)-Finance Code 001.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. An P, Li L, Chaolong W, Huan G, Xingjie H, Qi W. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. medRxiv JAMA. (2020) 323:1915–23. doi: 10.1001/jama.2020.6130
2. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. (2020) 323:1061–9. doi: 10.1001/jama.2020.1585
3. Yu IT, Li Y, Wong TW, Tam W, Chan AT, Lee JH, et al. Evidence of airborne transmission of the severe acute respiratory syndrome virus. N Engl J Med. (2004) 350:1731–9. doi: 10.1056/NEJMoa032867
4. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. (2020) 382:1199–207. doi: 10.1056/NEJMoa2001316
5. Sohrabi C, Alsafi Z, O'Neill N, Khan M, Kerwan A, Al-Jabir A, et al. World health organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. (2020) 76:71–6. doi: 10.1016/j.ijsu.2020.02.034
6. van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. (2020) 382:1564–7. doi: 10.1056/NEJMc2004973
7. Harrel SK, Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. J Am Dent Assoc. (2004) 135:429–37. doi: 10.14219/jada.archive.2004.0207
8. Bahl P, Doolan C, de Silva C, Chughtai AA, Bourouiba L, MacIntyre CR. Airborne or droplet precautions for health workers treating COVID-19? J. Infect. Dis. (2020). doi: 10.1093/infdis/jiaa189. [Epub ahead of print].
9. Sabino-Silva R, Jardim ACG, Siqueira WL. Coronavirus COVID-19 impacts to dentistry and potential salivary diagnosis. Clin Oral Invest. (2020) 24:1619–21. doi: 10.1007/s00784-020-03248-x
10. World Health Organization (WHO). Infection Prevention and Control of Epidemic- and Pandemic-Prone Acute Respiratory Infections in Health Care; WHO Guideline. Geneva: World Health Organisation (2014). Available online at: https://apps.who.int/iris/bitstream/handle/10665/112656/9789241507134_eng.pdf?sequence=1 (accessed March 30, 2020).
11. World Health Organization (WHO). Rational Use of Personal Protective Equipment (PPE) for Coronavirus Disease (COVID-19). Geneva, IL: World Health Organization (2020).
13. Azouni MA, Petre G. Surface-tension-driven flows in a thin layer of a water solution. J Colloid Interf Sci. (2001) 239:509–16. doi: 10.1006/jcis.2001.7568
14. Gralton J, Tovey E, McLaws ML, Rawlinson WD. The role of particle size in aerosolised pathogen transmission: a review. J Infection. (2011) 1:1–13. doi: 10.1016/j.jinf.2010.11.010
15. Albrecht W, Fuchs H, Kittelmann W. Nonwoven Fabrics. Weinheim: Wiley-VCH (2003). p. 9–11. doi: 10.1002/3527603344
16. Russell SJ. Handbook of Nonwovens. Cambridge: Woodhead Publishing (2007). doi: 10.1533/9781845691998
Keywords: COVID-19, Non-woven, biosafety, dental personal protection, aerosol, infection control
Citation: Barboza EP, dos Santos GO, Montez C, Sendra LA, Vieira EO and Ferreira VF (2020) Are Non-woven Gowns Safe for Dental Professionals? A Preclinical Double-Blind Study. Front. Dent. Med. 1:577477. doi: 10.3389/fdmed.2020.577477
Received: 29 June 2020; Accepted: 28 August 2020;
Published: 16 October 2020.
Edited by:
Kristina Bertl, Malmö University, SwedenReviewed by:
Florian Beck, University Dental Clinic Vienna, AustriaGaetano Isola, University of Catania, Italy
Copyright © 2020 Barboza, dos Santos, Montez, Sendra, Vieira and Ferreira. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eliane Porto Barboza, elianeporto.uff@gmail.com
 Eliane Porto Barboza
Eliane Porto Barboza Gustavo Oliveira dos Santos
Gustavo Oliveira dos Santos Caroline Montez
Caroline Montez Luiza Abreu Sendra
Luiza Abreu Sendra Esio Oliveira Vieira
Esio Oliveira Vieira Vinicius Farias Ferreira
Vinicius Farias Ferreira