Hybrid total arch replacement via ministernotomy for Stanford type A aortic dissection
- 1Department of Cardiovascular Surgery, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 2Department of Otorhinolaryngology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
Background: Type A aortic dissection (TAAD) is a cardiovascular emergency condition with high mortality rate. Hybrid total aortic arch replacement using endovascular graft for the descending aorta repair results in favorable outcomes and has been recommended as an alternative procedure for the higher-risk category patients. Our institution started applying the upper ministernotomy incision technique for the hybrid procedures back in 2018.
Methods: We collected patients who underwent hybrid total arch replacement (HTAR) via ministernotomy (96) and total arch replacement with frozen elephant trunk (TAR + FET) procedures (99), between 2018 and 2021. The baseline information, intraoperative and postoperative characteristics have been compared. Kaplan-Meier analysis was used for survival evaluation. Cox regression were applied to identify the independent predictor of mortality.
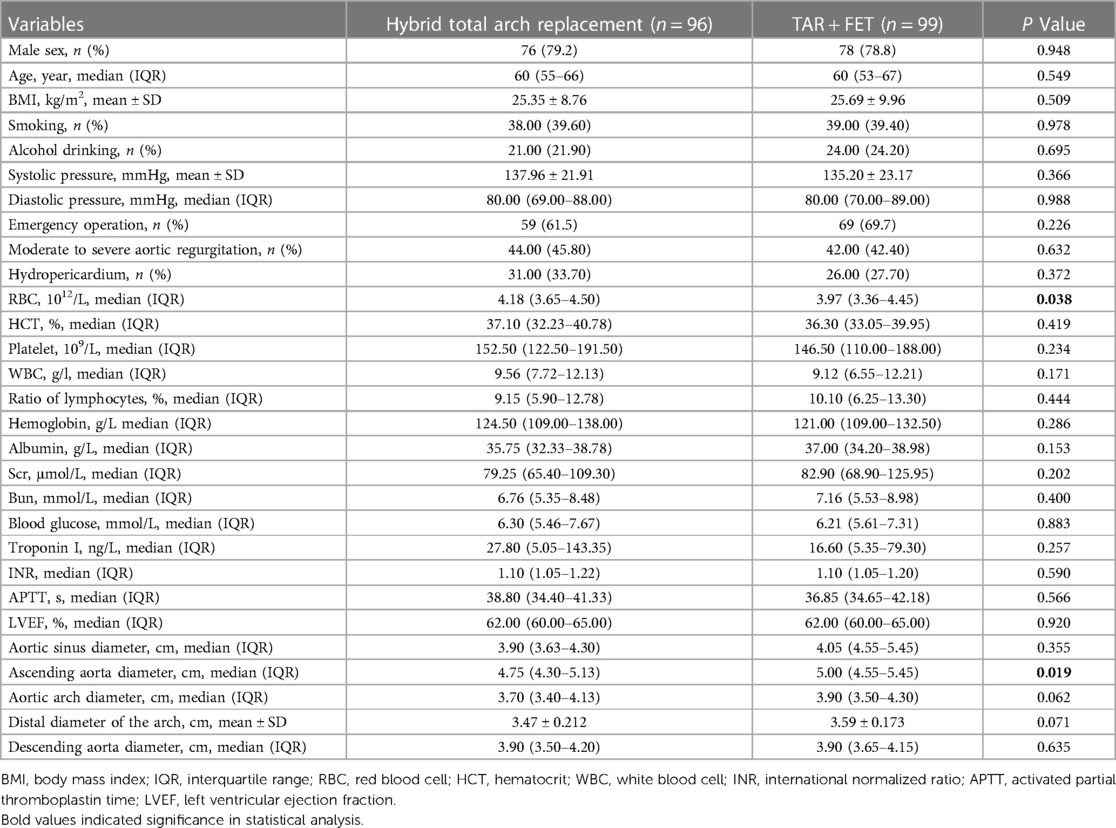
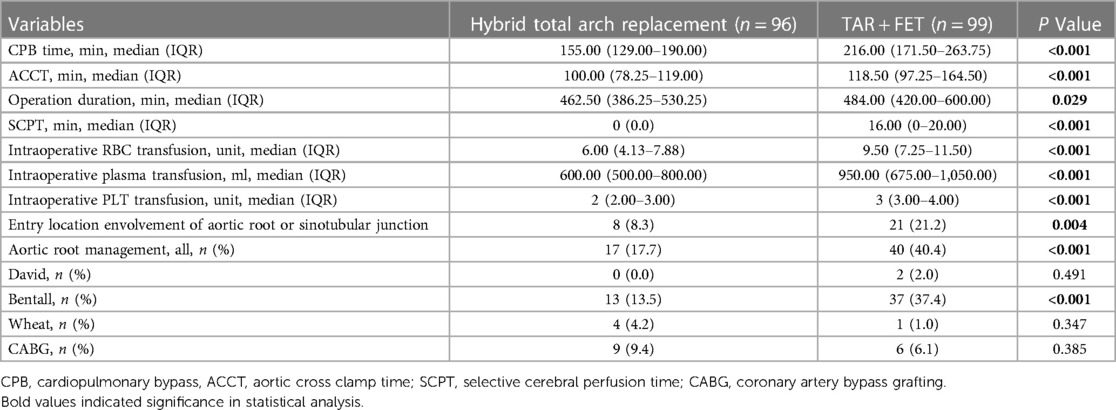
Results: The baseline characteristics between the two patient groups were compared and found similar, except that RBC counts were higher (p = 0.038) and the ascending aorta diameter was smaller (P = 0.019) in the “HTAR” group relative to the “TAR + FET” group. The cardiopulmonary bypass time (P < 0.001), the aortic cross clamp time (P < 0.001), the operation duration (P = .029), ICU (P = 0.037) and postoperative hospital stay (P = 0.002) were shorter in the “HTAR” group. The “HTAR” group exhibited also significantly lower levels of intraoperative transfusion (all <0.001) characteristics than the “TAR + FET” group. The hospital mortality and 1-year mortality revealed similar patterns in both groups.
Conclusion: HTAR via ministernotomy have similar short term prognosis, and also reduced the ICU and postoperative hospital stay. In all, The application of the ministernotomy technique in HTAR was safe and technically feasible and may benefit individual patients as well as hospitals in general.
Introduction
Type A aortic dissection (TAAD) is a devastating disease with a high degree of mortality if not intervened promptly (1). TAAD, with its rapid progression, requires a multidisciplinary diagnosis in combination with a proper and timely surgical intervention. A poor prognosis for the disease is mostly associated with the aortic rupture and organ malperfusion (2, 3). Timely surgical reconstruction of aortic aneurysm and its dissection are the mainstays of the TAAD therapy. Total arch replacement with frozen elephant trunk (TAR + FET) has achieved desirable long-term outcomes and been widely used for TAAD treatment in China (4, 5). Nonetheless, the operative mortality of the disease remained high, owing to the inevitably large surgical invasions and long operation times (6).
While endovascular total arch repair is a new technique of limited utility (7), hybrid total arch replacement (HTAR) currently represents a more practical and extensive therapeutic strategy for TAAD (8). Initially, short and long-term outcomes of HTAR were reported by single-center clinical studies (9, 10), however, the small sample size in those studies has led to different experiences and conclusions. Subsequently, various institutions have successively utilized HART as one of the TAAD main treatments, and some even attempted to further improve the technique (8, 11).
Having benefited from the implementation and improvement of the TAAD repair procedures and the cerebral protection methods, surgeons have advocated for utilization of a minimally-invasive approach involving an upper ministernotomy, which had been used in cardiac surgery for nearly two decades (12), especially in aortic valve surgery, and, according to numerous studies, provided satisfactory outcomes (13, 14). Utilization of upper ministernotomy for the HTAR procedure has been initiated also at our institution. This study was aimed at determining if the use of upper ministernotomy for HTAR is safe for patients, as compared to the conventional TAR + FET intervention, and further advisable.
Patients and method
Study populations
We retrospectively included 195 patients who underwent surgery at Union Hospital between December 2018 and December 2021. All patients initially experienced sudden chest/back pain and were diagnosed with Stanford type A aortic dissection on the basis of computed tomography angiography (CTA). The morphology of the patients’ heart valves was assessed by using transthoracic echocardiography. Patients with intramural hematoma (IHM), aortic aneurysm, penetrating aortic ulcer (PAU), or Stanford type B aortic dissection (TBAD) were excluded from this study (Figure 1). All the patients included in this study underwent aortic dissection repair surgery. The patients were divided into two study groups based on the surgical method used in their treatment: 96 (49.2%) patients who underwent hybrid total arch repair via upper ministernotomy, and 99 (50.7%) who received a conventional TAR with FET. The “TAR + FET” group included only patients above age 50. At our center, Stanford Type A aortic dissection repair surgery is being performed by three staff chief physicians with similar surgical skills and experience. We collected medical history and examined clinical information, including test results, surgical records as well as the follow-up information for each patient enrolled in the study by using the Union Hosptial Records System. This study was approved by the ethics committee of Wuhan Union Hospital, Huazhong University of Science and Technology (UHCT22975) and complied with the World Medical Association Code of Ethics (Declaration of Helsinki) adopted in 1975.
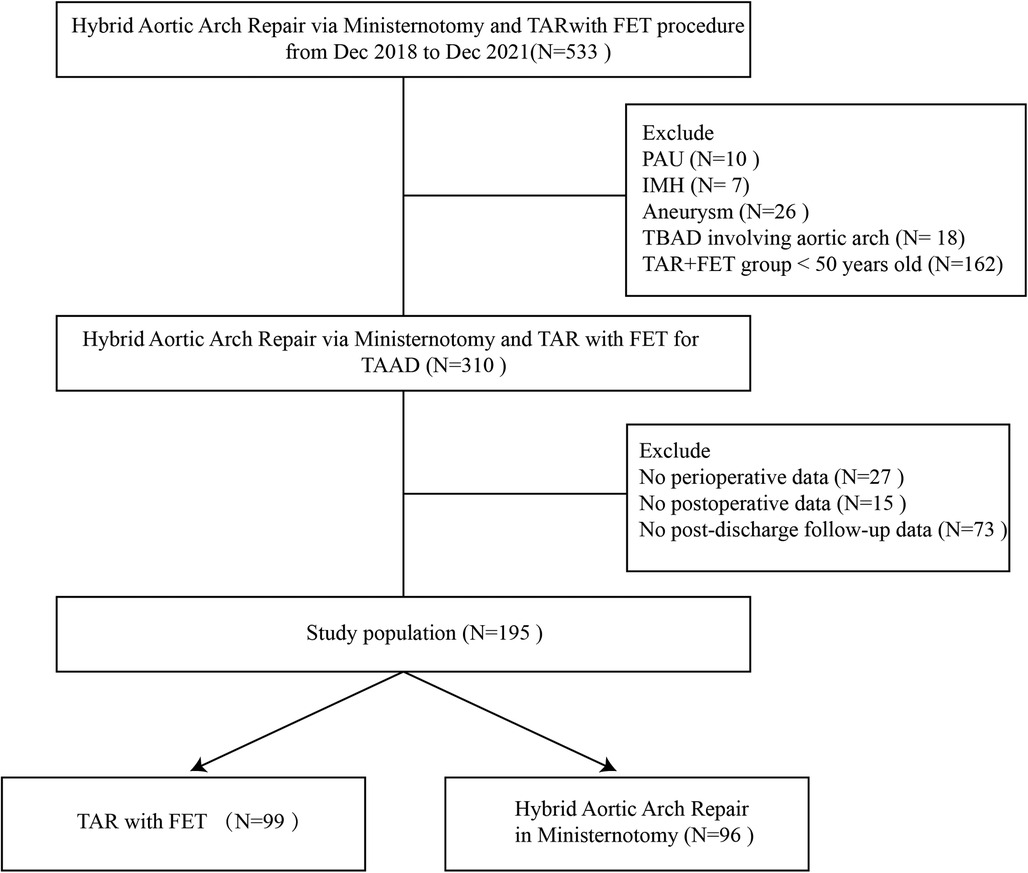
Figure 1. Flow diagram of the study cohort. Inclusion and exclusion criteria and population of this study. Five hundred thirty-three patients who underwent HTAR or TAR with FET procedure for TAAD from Dec 2018 to December 2021 were included. PAU, penetrating aortic ulcer; IMH, Intramural hematoma; TAAD, type A aortic dissection; TBAD, Stanford type B aortic dissection; FET, frozen elephant trunk.
Surgical indication
In our hospital, hybrid total arch repair (HTAR) via ministernotomy and TAR + FET are currently the standard treatment options for Stanford type A aortic dissection. HTAR via ministernotomy is the most commonly used treatment of this disorder in the following circumstances: (i). in patients of old age (above 50) with multiple comorbid conditions who are at higher risk of hypothermic circulatory arrest (HCA); (ii) in patients with routine distal FET anastomosis that is a challenging condition when massive intimal tears or dissected pseudoluminas affect the distal portion of the descending aorta; (iii) in patients with high aesthetic wound requirements as HTAR via ministernotomy can shorten the period of wound healing.
Surgical techniques
“TAR + FET” group
After induction of general anesthesia, the right axillary artery was cannulated for cardiopulmonary bypass (CPB) and ACP, and a standard median sternotomy was performed. Then CPB was carried out through the right axillary artery and right atrium, while the cooling process was initiated. When the patient was cooled down to 33°C or the heart suffered from a ventricular fibrillation, the ascending aorta was clamped. At this time, the surgical procedures in the aortic root were carried out. Then, the patient was continuously cooled down to about 25°C, at which circulatory arrest would be performed. The bilateral ACP was initiated through the left common carotid artery during the circulatory arrest. Meanwhile, the left subclavian, left common carotid and innominate arteries were clamped. The stented elephant trunk was inserted into the true lumen of the descending aorta, which was anastomosed to the distal end of the four-branched graft (Maquet M00202175728APO). As required, air was removed from the descending aorta after anastomosis. Blood perfusion of the lower body was initiated by the infusion limb of the four-branched graft. The left subclavian artery was anastomosed to one limb of the vascular graft. As a result, CPB gradually resumed to normal flow, and the rewarming started. The left common carotid artery was anastomosed end-to-end with the innominate artery. Anastomosis of the proximal end was carried out during the rewarming step. When the lung was reventilated, the ascending aorta was reopened to resume the cardiac perfusion.
When the patients were cooled down to the temperatures below 28°C, a PH steady-state blood gas management was used, while an alpha steady-state blood gas management was applied when the temperature was above 28°C. The whole process of cooling and rewarming was carried out at a slow and uniform rate, in a step-by-step process. Following the operation, CPB was stopped when the blood gas analysis results were satisfactory.
“Hybrid total arch repair via ministernotomy” group
Our small-incision hybrid aortic repair is a single-stage procedure that was performed in a hybrid operating room and consisted of two phases: an open repair and an endovascular repair phase. The operation involved hybrid aortic arch repair without MHCA. In the open repair phase, a midline ministernotomy incision was made from the suprasternal fossa to the third intercostal (about 12–16 cm) (Figure 2A). Then the right femoral artery and the right atrium were used for cardiopulmonary bypass, and cooled to 32°C−28°C. The aortic cross-clamp placement was proximal to the opening of the anonymous artery and followed by the aortic root repair. Subsequently, a bilateral cerebral perfusion was initiated through the left common carotid artery and innominate artery catheterization. Meanwhile, the left subclavian carotid and innominate arteries were clamped. The aortic cross-clamp was used between the opening of the anonymous artery and the left common carotid artery. The aortic arch was transected proximal to the left common carotid artery. The distal end of the graft was then sutured end-to-end to the aortic arch, proximal to the left common carotid. An antegrade perfusion of the lower body was initiated by the branch of the artificial vessel, followed by rewarming and proximal anastomosis of the artificial vessel trunk (Figure 2B). The vessels in the parietal region were sequentially anastomosed with the left common artery, left subclavian artery, and anonymous artery. CPB was discontinued and wound hemostasis was achieved after protamine was administered to neutralize heparin. This is followed by endoluminal repair on digital subtraction angiography (DSA) (Figure 2C).
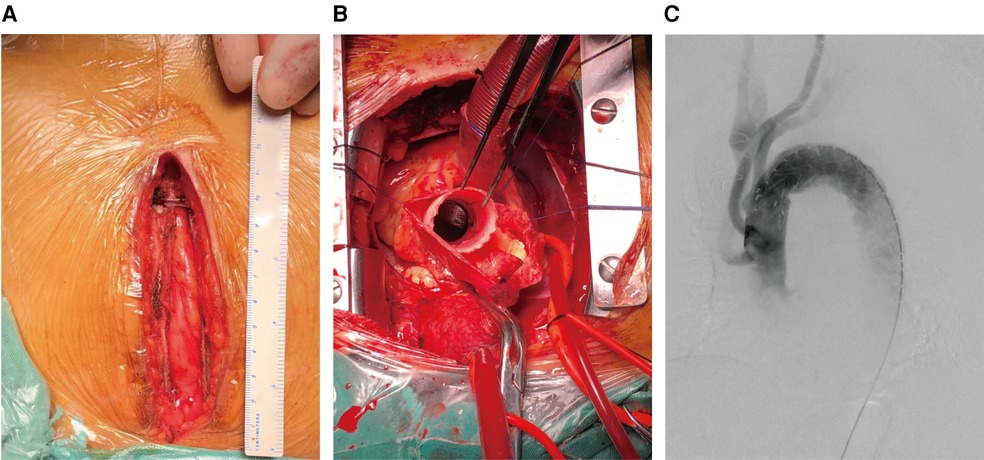
Figure 2. Incision of upper ministernotomy and HTAR technique. (A) Upper ministernotomy incision. (B) Intra-operative surgical filed of view: proximity of tetrafurcate vascular prosthesis graft was anastomosed to the sinotubular junction (aortic root has been repaired). (C) Endovascular portion: a stent graft implantation to exclude the entire lesioned aortic arch.
In the endovascular repair phase, the proximal stent was anchored to the artificial vessel to complete the arch repair. Angiography showed that there was no endoleak or contrast agent inside the false lumen of the thoracic aorta. A computed tomography performed prior to discharge showed aortic remodeling with complete thrombosis of the false lumen of the stented thoracic aorta. A postoperative transfer of the patients was made first to the intensive care unit (ICU) and then to a general ward, depending on the state of their recovery. After discharge, patients were advised to undergo a total aortic CTA examination in 3 months and 12 months after surgery, and annually thereafter.
Outcome criteria
The primary outcome was a 1-year survival rate. The secondary outcome included such postoperative criteria as in-hospital mortality, postoperative complications, tracheotomy, extracorporeal membrane oxygenation (CRRT) secondary insertion pipe, tracheal intubation time, ICU stay, and postoperative hospital stay.
Statistical analysis
Statistical analysis was performed by SPSS 25.0 software. Descriptive statistics was presented as frequency and percentage for categorical variables. For continuous variables, data was reported as mean ± SD or median with interquartile range after normal distribution testing. The non-normal distribution of the data necessitated the use of non-parametric tests. The Kaplan Meier survival estimate was calculated using Kaplan Meier analysis and Kaplan Meier curves were plotted. Cox univariable and multivariable regression analyses were performed and screened to show predictors of mortality. The variables used have been established in previous literature as predictors of the total arch replacement outcome.
Results
Baseline characteristics
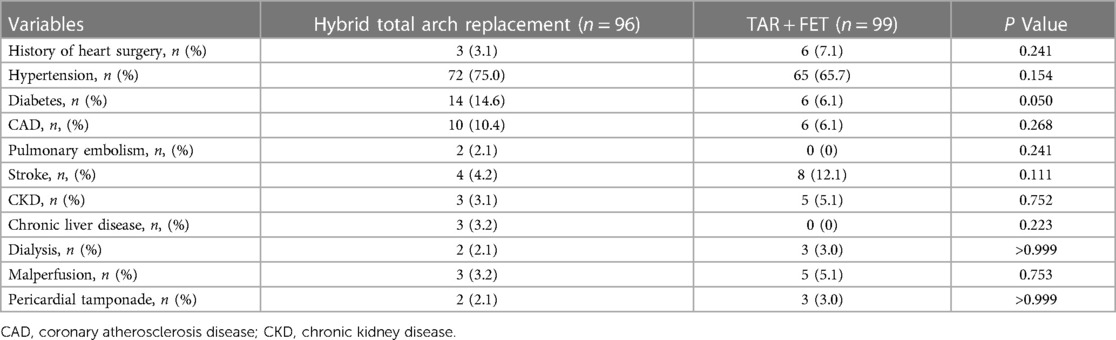
The median age of patients in the “hybrid total arch replacement (HTAR) via ministernotomy” group was 60 (IQR:55–66) with 76 (79.2%) patients being males, whereas the median age of the patients in the “TAR + FET” group was 60 (IQR:53–67) with 78 (78.8%) being males. A moderate to severe aortic regurgitation occurred in 44 (45.8%) patients in HTAR and 42 (42.4%) in TAR + FET groups, respectively. RBC was statistically different between the two groups (4.18 vs. 3.97, p = 0.038). In addition, the results of the patients’ echocardiography analysis have shown that the ascending aorta diameter in the “HTAR via ministernotomy” group was smaller than that in the “TAR + FET” group (4.75 vs. 5.0, P = 0.019). Apart from the above, the baseline characteristics of both groups were identical, which is evident from Table 1. As shown in Table 2, there were no significant differences in coronary atherosclerosis disease (P = 0.268), hypertension (P = 0.154), or diabetes (P = 0.050) between the “HTAR via ministernotomy” and the “TAR + FET” groups. Moreover, there was no statistically significant difference between the two groups in terms of comorbidities.
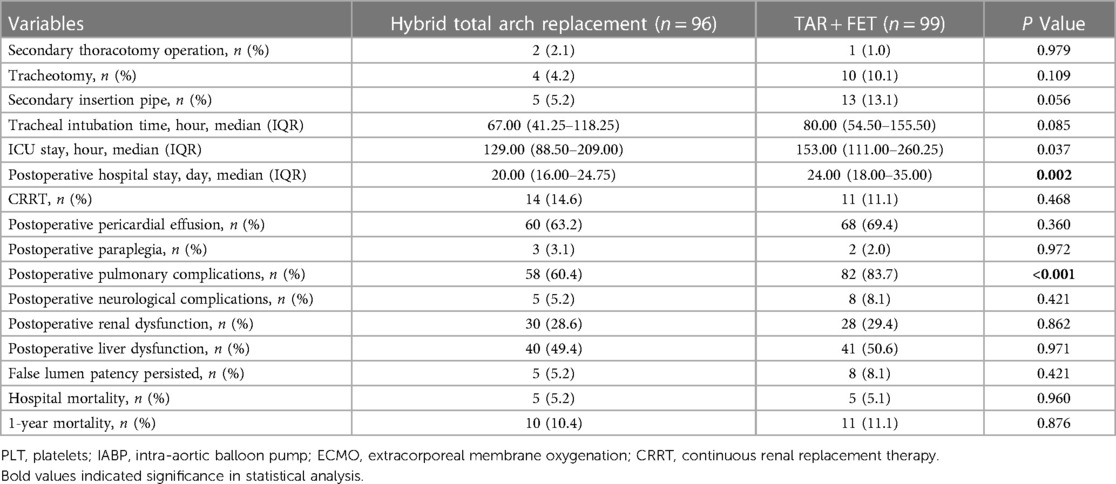
Intraoperative data
Intraoperative data are detailed in Table 2. The CPB time (155 vs. 216 min, P < 0.001), the aortic cross clamp time (ACCT) (100 vs. 118.5 min, P < 0.001) and the operation duration (462.5 vs. 484.0 min, P = .029) times were shorter in the “HTAR via ministernotomy” group than in the “TAR + FET” group (Table 3). Besides, the “HTAR via ministernotomy” group exhibited also significantly lower values in intraoperative blood transfusion: RBC (6 vs. 9.5 units, P < 0.001), plasma (600 vs. 950 ml, P < 0.001), PLT (2 vs. 3 units, P < 0.001) compared with the “TAR + FET” group. Besides, the “HTAR via ministernotomy” and the “TAR + FET” groups revealed a difference with regard to the simultaneous surgical aortic root management by Bentall operation (13.5% vs. 37.4%, P < 0.001).
Short-term postoperative outcomes
There were no significant differences in the outcomes of post-surgical continued treatment such as ECMO, secondary thoracotomy operation, tracheotomy, tracheal intubation time, secondary insertion pipe, and CRRT (P > 0.05). However, the length of the patients’ ICU stay (129 vs. 153 h, P = 0.037) and the length of postoperative hospital stay (20 vs. 24 days, P = 0.002) were shorter for the “HTAR via ministernotomy” group relative to the “TAR + FET” group. As far as the postoperative complications are concerned, no difference between the groups was noted, as from the 12 patients who died during the immediate postoperative period, 6 were from the “HTAR via ministernotomy” group and 6 from the “TAR + FET” group (6.3% vs. 6.1%, P = 0.941), while no patients exhibited a postoperative stent endoleak or stent displacement. The percentage of postoperative pulmonary complications, however, was lower in the “HTAR via ministernotomy” group than in the “TAR + FET” group (60.4% vs. 83.7%, P < 0.001). Nonetheless, there were no significant differences in postoperative pericardial effusion (P = 0.360), postoperative neurological complications (P = 0.421), and postoperative renal or liver dysfunctions (P = 0.539).
Survival analysis
All patients were followed up until October 10th, 2022, and the median follow up time was 29.0 (16.5–40.7) months for the “TAR + FET” group and 20.8 (10.3–27.3) months for the “HTAR via ministernotomy” group, respectively. In Kaplan–Meier survival analysis, no significant differences were found between the “HTAR via ministernotomy” group and the “TAR + FET” group (p = 0.29) (Figure 3). Separate analyses of hospital mortality (5.2% vs. 5.1%, p = 0.960) and 1-year mortality (10.4% vs. 11.1%, p = 0.876) revealed similar patterns (Table 4). The variables were selected according to the previous studies and the baseline variables that have a significant bias between the two groups for univariable Cox analysis (Figure 4A). On the basis of Cox multivariable regression analysis, we found that the application of ministernotomy for HTAR was safe [HR 0.671 (0.331–1.444); p = 0.307] (Figure 4B). Furthermore, older age [HR 1.072 (1.030–1.115); p = 0.001], cardiopulmonary bypass time [HR 1.008(1.005–1.012); p < 0.001] and Scr [HR 1.002 (1.001–1.003); p = 0.001] represented significant independent predictors of mortality in both univariable and multivariable models. The Schoenfeld residuals analysis was performed and showed no significance (Figure 4C).
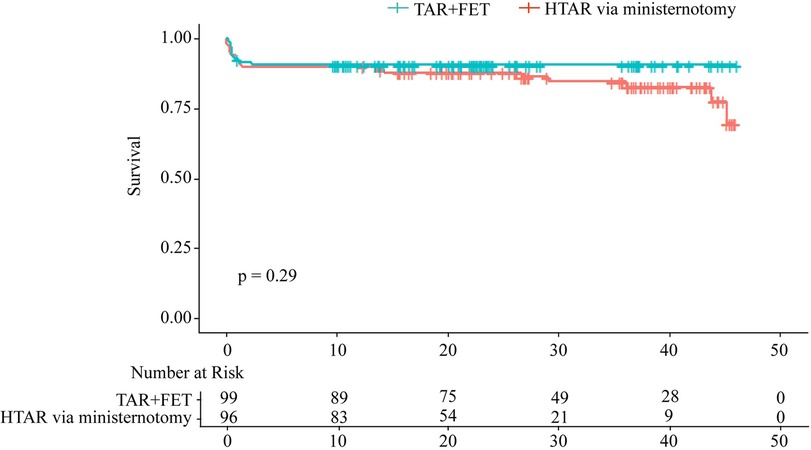
Figure 3. Kaplan–Meier analysis for overall survival stratified by HTAR via ministernotomy and TAR + FET, and log-rank test showed no significant difference between two group (P = 0.29).
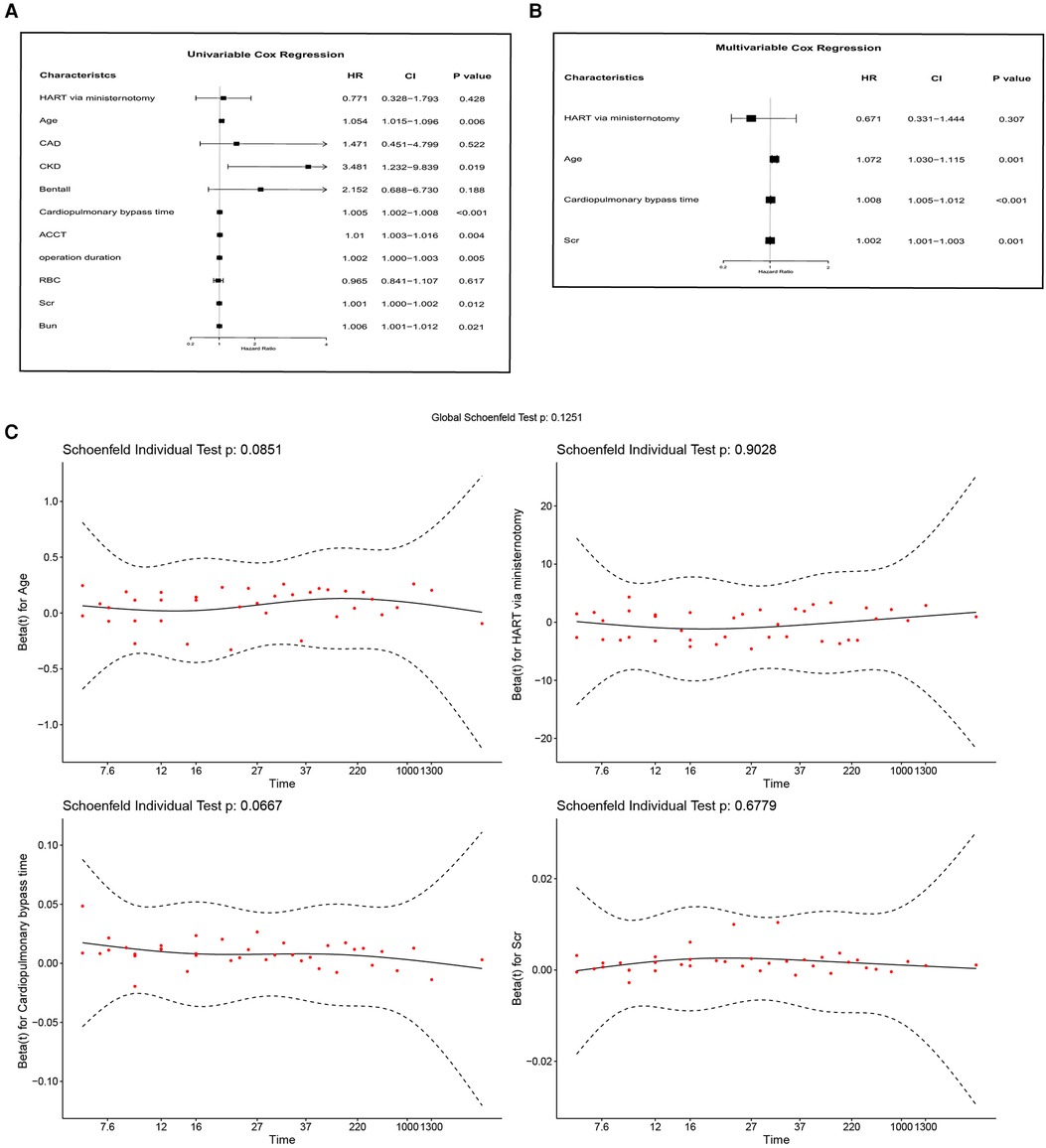
Figure 4. Cox proportional hazards regression models. (A) Univariable Cox regression analysis; (B) multivariable Cox regression analysis. (C) Schoenfeld residuals analysis. HR, hazard ratio; CI, confidence interval.
Conclusion
HTAR via ministernotomy have similar short term prognosis, and also reduced the ICU and postoperative hospital stay. In all, The application of the ministernotomy technique in HTAR was safe and technically feasible and may benefit individual patients as well as hospitals in general.
Discussion
This retrospective study on acute TAAD patients has led to the following findings: primarily, the application of the ministernotomy for HTAR was safe and technically feasible compared with the traditional aortic repair. Second, the differences in intraoperative variables have indicated that the HTAR via ministernotomy procedure has shortened duration of the operation, CPB, and ACC, as well as reduced the intraoperatively needed blood transfusion volume of RBC, plasma, and PLT. More importantly, the ministernotomy for HTAR procedure per se was not an independent risk factor for the patient mortality. However, older age, the cardiopulmonary bypass time, and the Scr level remained independent risk factors after adjusting for covariates.
As the technology improving the sensitivity of diagnostic for TAAD advances, more and more patients receive timely surgical interventions before the aortic rupture occurs. A prompt surgical treatment along with improved surgical techniques and perioperative patient care make the TAAD disease increasingly curable. Despite the advances in all the above fields, the operative and perioperative morbidity and mortality for TAAD remains high. In this regard, the goal of clinical TAAD treatment has not only been to improve the patients’ survival, but also to obtain a better long-term prognosis for those patients. Since the traditional total aortic repair surgery was still a highly-invasive and risky procedure, the endovascular treatment of the thoracic aortic disease is emerging as a less invasive alternative to open surgery (15, 16). With the steadily increasing use of EAVR, it has been the mainstay of the descending aortic disease treatment (17, 18). Since the HTAR approach was first implemented in 2000 by J.A. Macierewicz et al. (19), many cardiovascular centers applied it for over a decade and their data show that HTAR has achieved desirable early and long-term clinical outcomes (9, 20). Our method of HTAR via upper ministernotomy procedure has similar indications as the conventional HTAR approach. Our data also indicated a favorable outcome after adjusting for age, which is the factor of the greatest bias from the TAR group (10). A meta-analysis of 38 studies reported that the hospital mortality associated with HTAR for TAAD was 5.5% lower than that in the case of traditional total arch repair (11). While a 12-year retrospective study involving the HTAR treatment of 209 patients in China demonstrated an early mortality rate of 10.0% (9), our study's early mortality associated with HTAR via ministernotomy was only 5.2%, (5.1% in the “TAR + FET” group), and a 1-year mortality was 10.4% (11.1% for the “TAR + FET” group). The rate of early mortality associated with our ministernotomy for HTAR technique was similar to that resulting from the conventional invasion of HTAR procedure. The two procedures compared in our study significantly differed in such characteristics, as post-operative in-hospital time (20 vs. 24; p = 0.002) and post-operative pulmonary complications (60.4% vs. 83.7%; p < 0.001). Except for the comparable short-term outcomes, the two groups exhibited significant differences in intraoperative variables, in line with the previous studies demonstrating that the HTAR procedure decreased the time of CPB, ACC, as well as the operation duration time (20). Besides, the use of HTAR via ministernotomy reduced the intraoperatively needed blood transfusion volume.
It is noteworthy that “HTAR” reported by some earlier studies was referred to as a “TAR with FET” procedure. Actually, TAR with FET that is also called Sun's procedure, has been widely used for the TAAD treatment in China for over 20 years (21). In our institution HTAR has been utilized as an alternative option for TAR with FET, especially for the high-risk patient category. In this case, there was a notable discrepancy in patients’ age between the two groups. We excluded patients under the age of 50 from the “TAR with FET” treatment group also because the indication age for the HTAR treatment in our institution was 50 years of age and over. Patients’ age has been previously reported as an independent predictor for mortality and used as such also in our study [HR 1.072 (1.030–1.115); p = 0.001]. This, to some extent, decreased the risk of potential bias. Besides, our results were consistent with those of an earlier study, reporting that, after propensity-score matching (PSM), the early mortality and post-operational complication rates in the “HTAR” group were not significantly different from the “TAR + FET” group (10).
The upper ministernotomy approach was first implemented for aortic valve operations in 1996, and since 1997 its use was extended to more complex cardiac surgery procedures (13, 22, 23). A surgical department from Italy with 11 years of experience in applying upper ministernotomy for the ascending aorta procedures, has found that this technique can reduce the postoperative bleeding and thereby the number of transfused RBC units in patients, as well as reduce their hospital stay (14). These outcomes were similar to those of our study and demonstrated that the utilization of upper ministernotomy provides substantial clinical advantages (24, 25). Both the satisfactory clinical outcomes and patients’ requests facilitated application of ministernotomy for HTAR. To date the usage of this technique has been limited to a few large cardiovascular centers. More time is obviously needed for this technique to be widely and more commonly used in complex cardiac surgeries. A center in China has applied upper ministernotomy for the conventional TAR with FET procedure, but their results showed no difference in ICU and total hospital stay (26). Besides, they selected low-risk patients for this minimally-invasive surgery, and this made the above study different from ours. Our purpose thus was to further decrease the risk of infection and improve the poor surgical wound healing, since the HTAR procedure was indicated for the high-risk category patients. To our delight, our study revealed that the use of HTAR via ministernotomy has led to less post-operative pulmonary complications, which would mainly involve a pulmonary infection and excessive or moderate pleural effusions. In conclusion, practicing upper ministernotomy for HTAR in our institution proved safe and feasible, alleviated both patients’ and hospital's burden and provided a minimal invasiveness to the surgical process.
Study limitations
There are few limitations to this study. First, this was a single-center based retrospective observational study, which can only provide a limited clinical and statistical information. A multi-center study with larger sample size may be needed. Second, we didn't include a perfect control group because, since 2018, almost all the patients with HTAR indication received surgery using the upper ministernotomy approach at our institution. However, the data of HTAR via ministernotomy in this study was discussed and compared with previous studies of conventional invasion of HTAR procedure obove. Third, since the use of this approach in our institution has not been long enough, the data on the long-term outcomes of this study are not yet available, and the patients from our study should still be followed up in the future.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Wuhan Union Hospital, Huazhong University of Science and Technology (UHCT22975). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because Retrospective study have no intervention on human or need any coordination.
Author contributions
XL, XYL, JL, and HL contributed to conception and design of the study. JS, FL, PL, CD, XH, LW, JL, and HL Performed development of surgery methodology. XL, XYL, HY, YY, QZ, and KW organized the database. XL, XYL, and HY performed the statistical analysis. XL and XYL wrote the first draft of the manuscript. HY, QZ, KW, JS, JWL, and HL performed review and revision of the paper. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
TAAD, type A aortic dissection; HTAR, hybrid total arch replacement; TAR, total arch replacement; FET, frozen elephant trunk; CTA, computed tomography angiography; IHM, intramural hematoma; PAU, penetrating aortic ulcer; TBAD, Stanford type B aortic dissection; HCA, hypothermic circulatory arrest; DSA, digital subtraction angiography; ICU, intensive care unit; ACCT, aortic cross clamp time; PSM, propensity-score matching; BMI, body mass index; IQR, interquartile range; RBC, red blood cell; HCT, Hematocrit; WBC, white blood cell; INR, international normalized ratio; APTT, activated partial thromboplastin time; LVEF, left ventricular ejection fraction; CAD, coronary atherosclerosis disease; CKD, chronic kidney disease; CPB, cardiopulmonary bypass; SCPT, selective cerebral perfusion time; CABG, coronary artery bypass grafting; PLT, platelets; IABP, intra-aortic balloon pump; ECMO, extracorporeal membrane oxygenation; CRRT, continuous renal replacement therapy; HR, hazard ratio; CI, confidence interval.
References
1. Blakeslee-Carter J, Menon AJ, Novak Z, Spangler EL, Beck AW, McFarland GE. Association of mental health disorders and aortic dissection. Ann Vasc Surg. (2021) 77:217–25. doi: 10.1016/j.avsg.2021.05.054
2. Harris KM, Nienaber CA, Peterson MD, Woznicki EM, Braverman AC, Trimarchi S, et al. Early mortality in type a acute aortic dissection: insights from the international registry of acute aortic dissection. Jama Cardiol. (2022) 7(10):1009–15. doi: 10.1001/jamacardio.2022.2718
3. Howard DP, Fau BA, Fau FJ, Fau PJ, Fau SL, Rothwell PM. Population-based study of incidence and outcome of acute aortic dissection and premorbid risk factor control: 10-year results from the Oxford Vascular Study. Circulation. (2013) 127(20):2031–7. doi: 10.1161/CIRCULATIONAHA.112.000483
4. Ma WG, Zhang W, Zhu JM, Ziganshin BA, Zhi AH, Zheng J, et al. Long-term outcomes of frozen elephant trunk for type a aortic dissection in patients with marfan syndrome. J Thorac Cardiovasc Surg. (2017) 154(4):1175–89. doi: 10.1016/j.jtcvs.2017.04.088
5. Hirano K, Tokui T, Nakamura B, Inoue R, Inagaki M, Hirano R, et al. Impact of the frozen elephant trunk technique on total aortic arch replacement. Ann Vasc Surg. (2020) 65:206–16. doi: 10.1016/j.avsg.2019.10.075
6. Kawajiri H, Khasawneh MA, Pochettino A, Oderich GS. Techniques and outcomes of total aortic arch repair with frozen elephant trunk for DeBakey I dissections. J Cardiovasc Surg. (2020) 61(4):392–401. doi: 10.23736/S0021-9509.20.11359-4
7. Horton JD, Kölbel T, Haulon S, Khoynezhad A, Green RM, Borger MA, et al. Endovascular repair of type a aortic dissection: current experience and technical considerations. Semin Thorac Cardiovasc Surg. (2016) 28(2):312–7. doi: 10.1053/j.semtcvs.2015.12.004
8. Rudarakanchana N, Jenkins MA-O. Hybrid and total endovascular repair of the aortic arch. Br J Surg. (2018) 105(4):315–27. doi: 10.1002/bjs.10713
9. Zhang B, Sun X, Liu Y, Dun Y, Liang S, Yu C, et al. Hybrid technique on the total arch replacement for type a aortic dissection: 12-year clinical and radiographical outcomes from a single center. Front Cardiovasc Med. (2022) 9:820653. doi: 10.3389/fcvm.2022.820653
10. Zhang L, Yu C, Yang X, Sun X, Qiu J, Jiang W, et al. Hybrid and frozen elephant trunk for total arch replacement in DeBakey type I dissection. J Thorac Cardiovasc Surg. (2019) 158(5):1285–92. doi: 10.1016/j.jtcvs.2019.01.020
11. Smith HN, Boodhwani M, Ouzounian M, Saczkowski R, Gregory AJ, Herget EJ, et al. Classification and outcomes of extended arch repair for acute type a aortic dissection: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg. (2017) 24(3):450–59. doi: 10.1093/icvts/ivw355
12. Goyal A, Chhabra L, Parekh A, Bhyan P, Khalid N. Minimally Invasive Aortic Valve Surgery. In: StatPearls. Treasure Island (FL): StatPearls Publishing (2023).
13. Byrne JG, Karavas AN, Cohn LH, Adams DH. Minimal access aortic root, valve, and complex ascending aortic surgery. Curr Cardiol Rep. (2000) 2(6):549–57. doi: 10.1007/s11886-000-0041-2
14. Totaro P, Carlini S, Pozzi M, Pagani F, Zattera G, D'Armini AM, et al. Minimally invasive approach for complex cardiac surgery procedures. Ann Thorac Surg. (2009) 88(2):462–6. doi: 10.1016/j.athoracsur.2009.04.060
15. Greenberg RK, Fau OS, Fau WE, Fau HF, Fau LS, Svensson LG, et al. Endovascular repair of thoracic aortic lesions with the zenith TX1 and TX2 thoracic grafts: intermediate-term results. J Vasc Surg. (2005) 41(4):589–96. doi: 10.1016/j.jvs.2005.01.043
16. Drews JD, Patel HJ, Williams DM, Dasika NL, Deeb GM. The impact of acute renal failure on early and late outcomes after thoracic aortic endovascular repair. Ann Thorac Surg. (2014) 97(6):2027–33. doi: 10.1016/j.athoracsur.2014.02.045
17. Riambau V, Böckler D, Brunkwall J, Cao P, Chiesa R, Coppi G, et al. Editor's choice - management of descending thoracic aorta diseases: clinical practice guidelines of the European society for vascular surgery (ESVS). Ann Thorac Surg. (2017) 53(1):4–52. doi: 10.1016/j.ejvs.2016.06.005
18. Fiorucci B, Kölbel T, Rohlffs F, Heidemann F, Carpenter SW, Debus ES, et al. The role of thoracic endovascular repair in elective, symptomatic and ruptured thoracic aortic diseases. Eur J Cardiothorac Surg. (2019) 56(1):197–203. doi: 10.1093/ejcts/ezy482
19. Macierewicz JA, Jameel MM, Whitaker SC, Ludman CN, Davidson IR, Hopkinson BR, et al. Endovascular repair of perisplanchnic abdominal aortic aneurysm with visceral vessel transposition. J Endovasc Ther. (2000) 7(5):410–4. doi: 10.1177/152660280000700510
20. Xie E, Wu J, Qiu J, Dai L, Qiu J, Luo Q, et al. Early outcomes of three total arch replacement strategies for DeBakey type I aortic dissection. Front Cardiovasc Med. (2021) 15(8):638420. doi: 10.3389/fcvm.2021.638420
21. Ma WG, Zheng J, Sb D, Lu W, Sun K, Rd Q, et al. Sun's procedure of total arch replacement using a tetrafurcated graft with stented elephant trunk implantation: analysis of early outcome in 398 patients with acute type a aortic dissection. Ann Cardiothorac Surg. (2013) 2(5):621–8. doi: 10.3978/j.issn.2225-319X.2013.09.06
22. Cosgrove DM 3rd, Sabik JF. Minimally invasive approach for aortic valve operations. Ann Thorac Surg. (1996) 62(2):596–7.8694642
23. Svensson LG. Minimal-access “J” or “j” sternotomy for valvular, aortic, and coronary operations or reoperations. Ann Thorac Surg. (1997) 64(5):1501–3. doi: 10.1016/S0003-4975(97)00927-2
24. Bonacchi M, Prifti E, Giunti G, Frati G, Sani G. Does ministernotomy improve postoperative outcome in aortic valve operation? A prospective randomized study. Ann Thorac Surg. (2002) 73(2):460–5. doi: 10.1016/s0003-4975(01)03402-6
25. Masiello P, Coscioni E, Panza A, Triumbari F, Preziosi G, Di Benedetto G. Surgical results of aortic valve replacement via partial upper sternotomy: comparison with median sternotomy. Cardiovasc Surg. (2000) 10(4):333–8. doi: 10.1016/s0967-2109(02)00026-1
Keywords: Stanford type A aortic dissection, total arch repair, hybrid total arch repair, frozen elephant trunk, ministernotomy
Citation: Liu X, Liu X, Yu H, Yang Y, Shi J, Zheng Q, Wang K, Liu F, Li P, Deng C, Hu X, Wu L, Li H and Liu J (2023) Hybrid total arch replacement via ministernotomy for Stanford type A aortic dissection. Front. Cardiovasc. Med. 10:1231905. doi: 10.3389/fcvm.2023.1231905
Received: 31 May 2023; Accepted: 2 October 2023;
Published: 18 October 2023.
Edited by:
Wolf-Hans Eilenberg, Medical University of Vienna, AustriaReviewed by:
Faizus Sazzad, National University of Singapore, SingaporeJia Hu, Sichuan University, China
Elisa Mikus, Maria Cecilia Hospital, Italy
© 2023 Liu, Liu, Yu, Yang, Shi, Zheng, Wang, Liu, Li, Deng, Hu, Wu, Li and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huadong Li lihuadong@hust.edu.cn Junwei Liu junweiliu@hust.edu.cn
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work and share last authorship
 Xing Liu
Xing Liu Xinyi Liu1,†
Xinyi Liu1,†  Yuehang Yang
Yuehang Yang Qiang Zheng
Qiang Zheng Kan Wang
Kan Wang Huadong Li
Huadong Li